Abstract
Sciatic hernia is a rare condition with diverse clinical manifestations. We report a case of sciatic hernia causing sciatica, in which the diagnosis made on CT was subsequently confirmed on MRI including magnetic resonance neurography. The salient clinical and imaging features and a brief review are presented.
Sciatic hernia is a rare condition that can lead to bowel obstruction, sciatica, pelvic pain, back pain or ureteric obstruction [1, 2]. Clinical diagnosis of this condition is difficult. Ultrasonography and CT are the imaging modalities commonly used to diagnose sciatic hernia, although MRI can be used in cases in which entrapment of the sciatic nerve is suspected. Magnetic resonance neurography (MRN) provides high-resolution images to demonstrate entrapment of the nerve and morphological changes in the nerve [3]. Colour Doppler can be useful in surgical planning, as it can provide information regarding bowel viability.
Case report
A 55-year-old woman presented with swelling in the left gluteal region and pain in the left lower limb of two years' duration. A detailed clinical history also revealed that she had an abscess in the left gluteal region following an intramuscular injection one year previously; however, at presentation there was no clinical feature suggestive of abscess. Physical examination revealed non-tender soft swelling in the left lumbar region with associated atrophy of gluteal muscles. To diagnose the nature of the gluteal mass, a CT scan of the pelvis and gluteal region was performed. The CT scan revealed herniation of the sigmoid colon through the greater sciatic foramen reaching up to the skin surface and atrophy of the gluteal muscles. Other major pelvic organs including the uterus, ureter and urinary bladder were normally located (Figure 1). As there was atrophy of the left gluteal muscles, and because the patient had symptoms of sciatica, entrapment of the sciatic nerve by sciatic hernia was suspected. MRI of the pelvis and upper thigh with MRN was performed to confirm entrapment of the sciatic nerve. MRN was used for high-resolution imaging of the sciatic nerve and was performed on a 1.5 T scanner (Sonata, Siemens, Erlangen, Germany) using a pelvis phase-array coil. Sequence parameters included 4 mm section thickness, 0 mm intersection gap, 18–24 cm field of view, 256 × 256 matrix, and an 8- to 10 min imaging time per sequence. The patient underwent axial T1 weighted spin echo (580/11/2–3 [TR/TE/excitations]) and axial and oblique coronal short tau inversion recovery (STIR, 5000/27/2–3; inversion time, 130 ms) sequences. Coronal oblique images were taken parallel to the course of the sciatic nerve. MRI revealed thickening and increased signal in the left sciatic nerve on STIR coronal oblique images (Figure 2). Lateral deviation and entrapment of the nerve by hernia was also noted along with atrophy of the left gluteal muscles.
Figure 1.
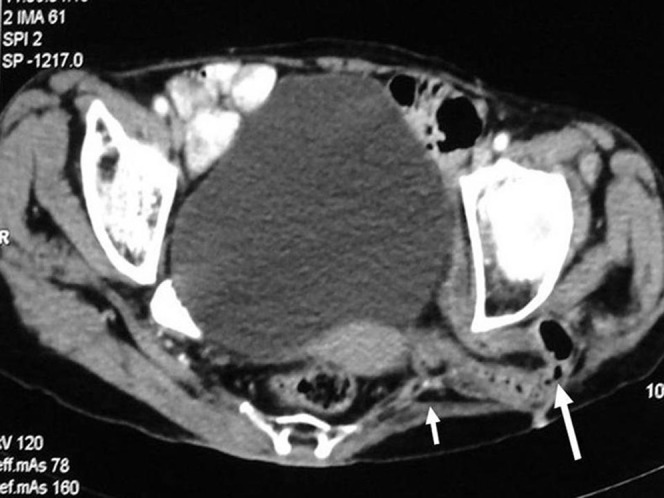
CT scan of the pelvis. The long arrow shows herniation of the sigmoid colon through the greater sciatic foramen. The short arrow shows atrophy of the left gluteal muscles.
Figure 2.
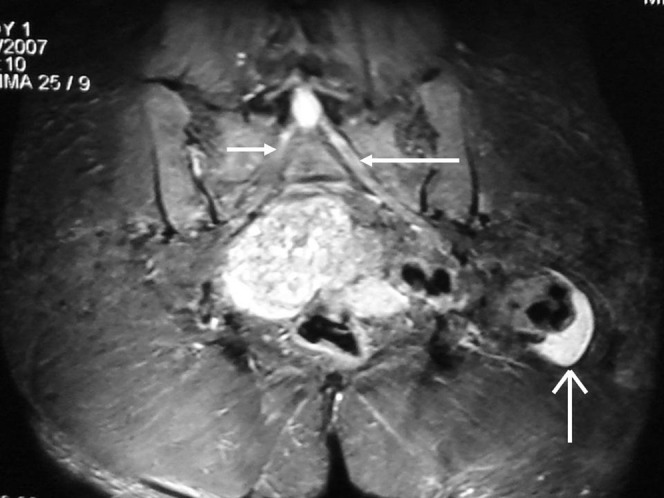
MRI coronal oblique STIR sequence image. The long arrow shows thickening and increased signal of the left sciatic nerve. The short arrow shows the normal right sciatic nerve. The thin white arrow in the lower part of the figure shows the herniated sac causing entrapment of the left sciatic nerve.
Discussion
Sciatic hernia is a rare condition, defined as protrusion of the peritoneal sac and its contents through the greater or lesser sciatic foramen. It is described in both adults and children. In adults, females are more commonly affected [1, 4]. Small bowel, omentum, ureter, ovary, fallopian tube, colon, bladder or Meckel's diverticulum may form the contents of the herniated sac [2, 5, 6]. Various presentations of sciatic hernia could be symptoms of bowel obstruction, ureteric obstruction, pelvic pain, lower back pain or sciatica [2, 5, 6]. Sciatica occurs as a result of compression of the sciatic nerve by the herniated sac [2, 7]. Ureteric obstruction can occur if a ureter is included in the herniated tissue.
Sciatic hernia can also lead to abscess formation in the gluteal region, particularly after perforation of a strangulated bowel [7]. In our patient, there was a history of abscess development in the left gluteal region after an intramuscular injection in the region.
Ultrasonography may be useful in establishing the diagnosis of sciatic hernia by revealing bowel loops and peristalsis. Colour Doppler study could provide information about the viability of the herniated bowel, which is important for surgical planning. The CT scan plays an important role in diagnosing sciatic hernia, although MRI is the modality of choice to evaluate the sciatic nerve in cases of sciatic hernia [8, 9]. MRN has been accepted as a clinical tool for high-resolution imaging of peripheral nerves and to diagnose peripheral neuropathy and plexopathy [3, 10, 11]. The MRN protocol uses high-resolution T1 weighted MRI sequences to delineate anatomic detail and fat-suppressed T2 weighted or STIR sequences to detect abnormal nerve signal intensity [9, 12]. Diffuse or focal enlargement of a nerve is definite evidence of abnormality, as is diffuse or focal marked hyperintensity on T2 weighted or STIR images [11, 12]. An altered fascicular pattern is another finding indicative of an abnormal nerve [11, 12]. At present, there is limited utility for gadolinium-based intravenous contrast material in peripheral nerve imaging [12]. The contrast material is used primarily in the evaluation of peripheral nerve tumours, neoplastic infiltration, and in studies of idiopathic inflammatory disorders [12]. We did not use gadolinium in imaging this case. Demonstration of the location and involvement of the sciatic nerve by MRI and MRN is important before surgery, especially if a laparoscopic approach is planned, to prevent inadvertent injury to the nerve.
Symptomatic sciatic hernia should be surgically treated as soon as possible, as the risk of strangulation of the bowel is high. A transabdominal or transgluteal approach may be used [13, 14]. A transabdominal approach is recommended in patients who present with bowel obstruction, especially when incarceration or strangulation is suspected; a transgluteal approach may be used when the herniated segments appear viable and reducible [13, 14].
In conclusion, sciatic hernia is rare, and entrapment of the sciatic nerve is unusual. Although CT scans can demonstrate hernia, MRI and MRN may be considered useful tools to image the sciatic nerve in patients with sciatic hernia.
References
- 1.Weintraub JL, Pappas GM, Romano WJ, Kirsch MJ, Spencer W. Percutaneous reduction of ureterosciatic hernia: case report. AJR Am J Roentgenol 2000;175:181–2 [DOI] [PubMed] [Google Scholar]
- 2.Skipworth RJE, Smith GHM, Stewart KJ, Anderson DN. The tip of the iceberg: a giant pelvic atypical lipoma presenting as a sciatic hernia. World J Surg Oncol 2006;4:33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Filler SG, Haynes J, Jordan SE, Prager J, Villablanca JP, Farahani K, et al. Sciatica of non disc origin and piriformis syndrome: diagnosis by magnetic resonance neurography and interventional magnetic resonance imaging with outcome study of resulting treatment. J Neurosurg Spine 2005;2:99–115 [DOI] [PubMed] [Google Scholar]
- 4.Rommel FM, Boline GB, Huffnagle HW. Ureterosciatic hernia: an anatomical radiographic correlation. J Urol 1993;150:1232–4 [DOI] [PubMed] [Google Scholar]
- 5.Touloupidis S, Kalaitzis C, Schneider A, Patris E, Kolias Ureterosciatic hernia with compression of the sciatic nerve. Int Urol Nephrol 2006;38:457–8 [DOI] [PubMed] [Google Scholar]
- 6.Yu PC, Ko SF, Lee TY, Ng SH, Huang CC, Wan YL. Small bowel obstruction due to incarcerated sciatic hernia: ultrasound diagnosis. Br J Radiol 2002;75:381–3 [DOI] [PubMed] [Google Scholar]
- 7.Servant CT. An unusual cause of sciatica: a case report. Spine 1998;23:2134–6 [DOI] [PubMed] [Google Scholar]
- 8.Rosenberg ZS, Cavalcanti CFA. Entrapment neuropathies of the lower extremity. In: Stoller DW, editor. Magnetic resonance imaging in orthopaedics and sports medicine. Philadelphia: Lippincott Williams & Wilkins, 2007:1051–5 [Google Scholar]
- 9.Moore KR, Tsuruda JS, Dailey AT. The value of MR neurography for evaluating extraspinal neuropathic leg pain: a pictorial essay. Am J Neuroradiol 2001;22:786–94 [PMC free article] [PubMed] [Google Scholar]
- 10.Bendszus M, Wessig C, Reiners K, Bartsch AJ, Solymosi L, Koltzenberg M. MR imaging in the differential diagnosis of neurogenic foot drop. Am J Neuroradiol 2003;24:1283–9 [PMC free article] [PubMed] [Google Scholar]
- 11.Bowen BC. Peripheral nerve imaging and the magic angle. Am J Neuroradiol 2004;25:352–4 [PMC free article] [PubMed] [Google Scholar]
- 12.Maravilla KR, Bowen BC. Imaging of the peripheral nervous system: evaluation of peripheral neuropathy and plexopathy. Am J Neuroradiol 1998;19:1011–23 [PMC free article] [PubMed] [Google Scholar]
- 13.Ivanov NT, Losanoff JE, Kjossev KT. Recurrent sciatic hernia treated by prosthetic mesh reinforcement of the pelvic floor. Br J Surg 1994;81:447. [DOI] [PubMed] [Google Scholar]
- 14.Hayashi N, Suwa T, Kimura F, Okuno A, Ishizuka M, Kakizaki S, et al. Radiographic diagnosis and surgical repair of a sciatic hernia: report of a case. Surg Today 1995;25:1066–8 [DOI] [PubMed] [Google Scholar]


