Abstract
We present a case of subacute left testicular pain and enlargement. Scrotal Doppler ultrasound revealed an enlarged left testicle with symmetrical intra-testicular colour flow bilaterally. Contrast-enhanced MRI demonstrated incomplete testicular torsion which was verified at surgery. To our knowledge, this is the first report on the use of contrast-enhanced MRI in the diagnosis of incomplete testicular torsion.
Incomplete testicular torsion is difficult to diagnose because of its subacute presentation with non-specific symptoms and signs. Decreased intra-testicular vascularity might be the only imaging finding, and subtle decreases in intra-testicular blood flow are often difficult to detect on colour Doppler ultrasound (CDUS). There is a high false-negative rate for the diagnosis of incomplete torsion on CDUS [1]. Suggestive findings include asymmetry of flow and resistive indices with decreased or reversed diastolic flow in the affected testis [2, 3].
MRI has been evaluated for the diagnosis of a wide variety of scrotal and testicular pathology, including testicular masses, testicular trauma and epididymo-orchitis [4–8]. However, there are no reports in the literature on the use of contrast-enhanced MRI in the pre-operative diagnosis of incomplete testicular torsion.
Case report
A 30-year-old man was referred to a urologist for evaluation of subacute left testicular pain and swelling of six weeks in duration. Physical examination revealed a healthy afebrile male with an enlarged but minimally tender left testis with normal lie and no palpable masses. There was no epididymal tenderness and the contralateral testis was normal. A cremasteric reflex was present bilaterally. There was no evidence of hernia, hydrocele or varicocele. Urinalysis was unremarkable and laboratory investigations revealed a normal white blood cell count and negative results for tumour markers including AFP, hCG and LDH.
Scrotal colour-flow Doppler ultrasound revealed an enlarged but homogenous left testis, with normal echogenicity, no focal lesion and symmetrical intra-testicular colour flow bilaterally (Figure 1). The cause of the patient's symptoms was not evident on ultrasound and thus an MRI was performed. The MRI showed that the left testis (4.2 × 3.9 × 3.2 cm) was enlarged in comparison to the right (3.6 × 2.2 × 2.1 cm), but both testes were homogeneous on pre-contrast T1- and T2-weighted images and no focal intra-testicular lesion was identified. The epididymides were also normal in appearance. Following the administration of gadolinium, enhancement of the left testis was markedly decreased in comparison to that of the right, and an obvious twisting of the left spermatic cord was seen (Figure 2).
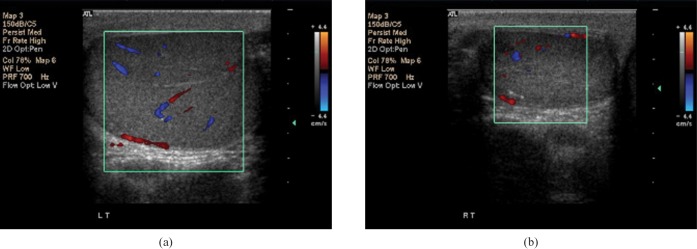
Figure 1.
Doppler ultrasound demonstrating (a) an enlarged left testis (4.9 × 3.5 × 2.6 cm) with homogenous echotexture and no focal intra-testicular lesion. Colour flow was present and appeared symmetrical to that of (b) the normal sized (3.6 × 2.2 × 2.1 cm) right testis.
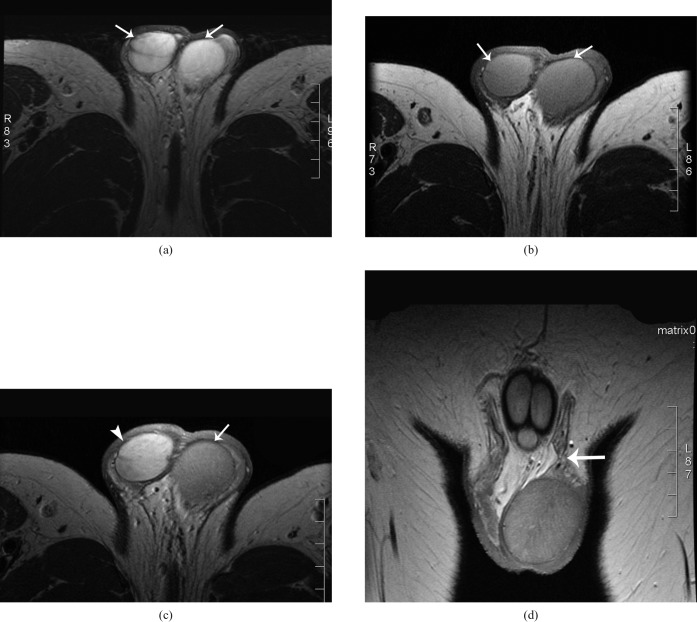
Figure 2.
(a) Axial T2- and (b) T1-weighted MR images demonstrating homogenous high T2 and homogenous intermediate T1 signal intensity in both testes (arrows). (c) Axial T1-weighted MRI image following administration of IV gadolinium showing decreased enhancement of the left testis (arrow) compared to the right (arrowhead). (d) Coronal T1-weighted MRI image demonstrating torsion of left spermatic cord (arrow).
Surgical exploration confirmed the presence of a bilateral bell-clapper deformity and a swollen, but viable, left testis with incomplete torsion of the left spermatic cord. Bilateral orchidopexy was performed and the patient's symptoms resolved post-operatively.
Discussion
It has been established that CDUS is the best imaging modality for the initial evaluation of scrotal or testicular pathology [9–12]. Further, CDUS is the most commonly employed initial imaging modality in the evaluation of patients with suspected testicular torsion. However, the gold standard in the diagnosis of testicular torsion remains surgical exploration.
Incomplete testicular torsion is extremely challenging to diagnose pre-operatively, but must be considered in the differential diagnosis for subacute testicular pain and/or swelling.
The importance of looking for rotated cord structures on grey-scale ultrasound has been suggested in studies in the paediatric population [13, 14]. Arce et al [14] showed that rotated cord structures were visualised with grey-scale ultrasound in all of 6 patients with surgically proven testicular torsion, despite the presence of intra-testicular colour flow on CDUS, suggesting a diagnosis of incomplete testicular torsion.
A retrospective study of dynamic contrast-enhanced MRI in the evaluation of testicular torsion in 39 patients yielded a sensitivity of 100%, a specificity of 93% and a negative predictive value of 96%. The authors concluded that MRI had little value in the evaluation of intermittent torsion, but did not explore its use in suspected incomplete torsion [7].
Trambert et al [8] were the first to suggest that the demonstration of torsion knot and whirlpool patterns on non-contrast MRI, resulting from twisting of the spermatic cord, yielded 100% accuracy in the diagnosis of incomplete testicular torsion in patients with subacute scrotal pain.
There are no studies in the literature on the use of MRI in the diagnosis of incomplete testicular torsion that evaluate contrast enhancement patterns. In this case report, we clearly demonstrate that gadolinium contrast enhancement on MRI may be reduced even in incomplete testicular torsion in which symmetrical bilateral colour flow is seen on CDUS. We also show that direct visualisation of rotated cord structures is possible, and could provide additional support for a diagnosis of incomplete testicular torsion. Another suggestive finding is increased testicular size caused by the obstruction of venous outflow.
Serra et al [15] performed a cost-analysis of MRI in the management of clinically and sonographically inconclusive scrotal lesions. This group showed that MRI improved the management plan in over 50% of such patients, resulting in cost savings of $543–730 USD per patient. Few of these patients had a diagnosis of testicular torsion, but this study does support the use of MRI in the evaluation of indeterminate scrotal pathology.
Conclusion
In conclusion, contrast-enhanced MRI was able to make the diagnosis of incomplete testicular torsion when clinical and ultrasound findings were equivocal.
References
- 1.Sanelli PC, Burke BJ, Lee L. Color and spectral Doppler sonography of partial torsion of the spermatic cord. AJR Am J Roentgenol 1999;172:49–51 [DOI] [PubMed] [Google Scholar]
- 2.Dogra VS, Sessions A, Mevorach RA, Rubens DJ. Reversal of diastolic plateau in partial testicular torsion. J Clin Ultrasound 2001;29:105–8 [DOI] [PubMed] [Google Scholar]
- 3.Dogra VS, Bhatt S, Rubens DJ. Sonographic evaluation of testicular torsion. Ultrasound Clin 2006;1:55–66 [Google Scholar]
- 4.Baker LL, Hajek PC, Brukhard TK, Dicapua L, Landa HM, Leopold GR, et al. MR imaging of the scrotum: pathologic conditions. Radiology 1987;163:93–8 [DOI] [PubMed] [Google Scholar]
- 5.Seidenwurm D, Smathers RL, Ko RK, Carrol CL, Bassett J, Hoffman AR. Testes and scrotum: MR imaging at 1.5 T. Radiology 1987;164:393–8 [DOI] [PubMed] [Google Scholar]
- 6.Thurnher S, Hricak H, Carroll PR, Pobiel RS, Filly RA. Imaging the testis: comparison between MR imaging and US. Radiology 1988;167:631–6 [DOI] [PubMed] [Google Scholar]
- 7.Terai A, Yoshimura K, Ichioka K, Ueda N, Utsunomiya N, Kohei N, et al. Dynamic contrast-enhanced subtraction magnetic resonance imaging in diagnostics of testicular torsion. Urology 2006;67:1278–82 [DOI] [PubMed] [Google Scholar]
- 8.Trambert MA, Mattrey RF, Levine D, Berthoty DP. Subacute scrotal pain: evaluation of torsion versus epididymitis with MR imaging. Radiology 1990;175:53–6 [DOI] [PubMed] [Google Scholar]
- 9.Hricak H, Filly RA. Sonography of the scrotum. Invest Radiol 1983;18:112–21 [DOI] [PubMed] [Google Scholar]
- 10.Carroll BA, Gross DM. High-frequency scrotal sonography. AJR Am J Roentgenol 1983;140:511–5 [DOI] [PubMed] [Google Scholar]
- 11.Leopold GR, Woo VL, Scheible FW, Nachtsheim D, Gosink BB. High resolution ultrasonography of scrotal pathology. Radiology 1979;131:719–22 [DOI] [PubMed] [Google Scholar]
- 12.Bree RL, Hoang DL. Scrotal ultrasound. Radiol Clin North Am 1996;34:1183–205 [PubMed] [Google Scholar]
- 13.Baud C, Veyrac C, Couture A, Ferran JL. Spiral twist of the spermatic cord: a reliable sign of testicular torsion. Pediatr Radiol 1998;28:950–4 [DOI] [PubMed] [Google Scholar]
- 14.Arce JD, Cortés M, Vargas JC. Sonographic diagnosis of acute spermatic cord torsion. Pediatr Radiol 2002;32:485–91 [DOI] [PubMed] [Google Scholar]
- 15.Serra AD, Hricak H, Coakley FV, Kim B, Dudley A, Morey A, et al. Inconclusive clinical and ultrasound evaluation of the scrotum: impact of magnetic resonance imaging on patient management and cost. Urology 1998;51:1018–21 [DOI] [PubMed] [Google Scholar]