Abstract
Speech recognition reporting was introduced in our institution to address the significant delay between report dictation and the appearance of a typed report on the Picture Archiving and Communication System (PACS). We report our experience of a “total” implementation of a speech recognition reporting (SRR) system, which became the sole means of radiology reporting from day 1 of introduction. Prospectively gathered Radiology Information System (RIS) data were examined to determine the monthly mean reporting times and completion times for all studies from January 2004 to February 2006 (11 months before introduction of SRR and 15 months after introduction). Studies were grouped for analysis according to referral source (casualty, general practice, inpatient or outpatient). A large, sustained reduction in time to completion was noted in all referral groups at both hospital sites within our institution (6.79 ± 0.92 days pre-SRR and 2.20 ± 0.78 days post-SRR, independent two-sample Student’s t-test, p<10−11). Workflow was maintained following the introduction of SRR: numbers of reports per month and mean times to report were unchanged. SRR eliminated the delays associated with report transcription and subsequent authorisation, dramatically reducing report turnaround times. Resistance to change has perhaps led to suboptimal implementation of SRR in some other institutions, such that benefits have not been fully realised. Our experience demonstrates the dramatic impact that a well-planned, organisation-wide implementation of SRR can have on radiology service delivery.
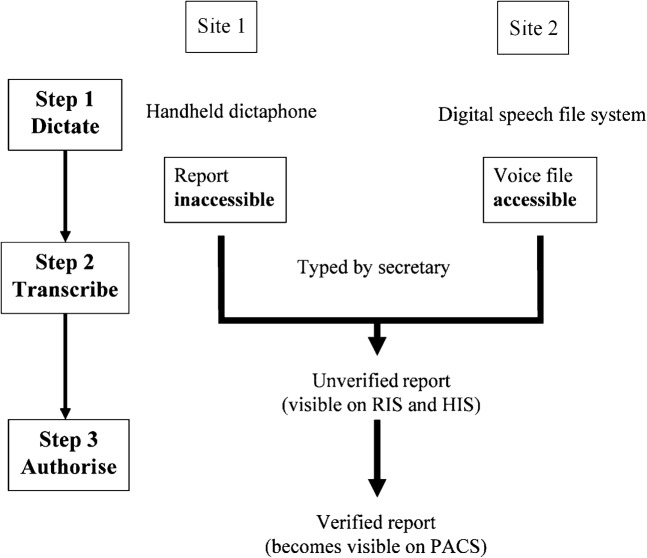
Our hospital trust consists of two sites, which between them perform more than 230,000 radiology examinations a year. A trust-wide Picture Archiving and Communication System (PACS) was established in 2003. Before the introduction of speech recognition reporting (SRR), reports were dictated and subsequently typed onto the Radiology Information System (RIS) as “unverified reports” by secretarial staff. Reports were effectively inaccessible until transcribed by the secretary, often several days after they had been dictated onto tape. Figure 1 outlines the process at both hospital sites. Frequent interruptions by clinicians requesting verbal reports for urgent studies (many of which had already been dictated) were disrupting reporting sessions and further reducing efficiency. Speech recognition reporting was introduced to address the significant delay between dictation and the appearance of a typed report on PACS.
Figure 1.
Original workflow. PACS was the “final resting place” for the imaging report, yet it was the system first accessed by clinicians seeking the report. Often the reports were “held up” at Step 2 or 3.
Despite evidence of benefit, in terms of reduced report turnaround times [1–6], much of the literature about SRR in radiology focuses on the issues of transcription error rates and the increased workload placed on the reporting radiologist [7–11]. We report our experience of a “total” (where SRR immediately became the sole means of reporting) implementation of SRR, emphasising the importance of a carefully managed transition for a successful outcome.
Methods and materials
CentricityTM PACS (GE Healthcare Diagnostic Imaging, Slough, UK), software release 3.0.2, was in use for the duration of the study. Powerscribe® for Radiology (Dictaphone Healthcare Solutions, Nuance Communications, Burlington, MA), software release 3.0, was introduced in December 2004.
Prospectively gathered data were extracted from the RIS database (CRIS®; Healthcare Software Systems, Mansfield, UK) to establish the monthly mean reporting times (time from exam acquisition to report dictation by a radiologist) and completion times (total time from exam acquisition to verification of the final report by a radiologist) for all studies. All departmental activity was included: plain radiographs, CT, ultrasound, MRI, nuclear medicine, fluoroscopy and interventional fluoroscopy (vascular and non-vascular). Data were collected for the period January 2004 to February 2006, representing a period of 11 months prior to the introduction of SRR and 15 months post introduction. Studies were grouped for analysis according to referral source (casualty, general practice, inpatient or outpatient).
Results
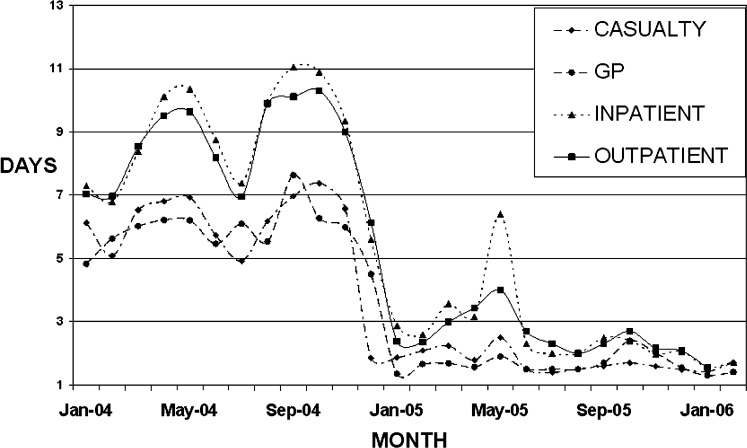
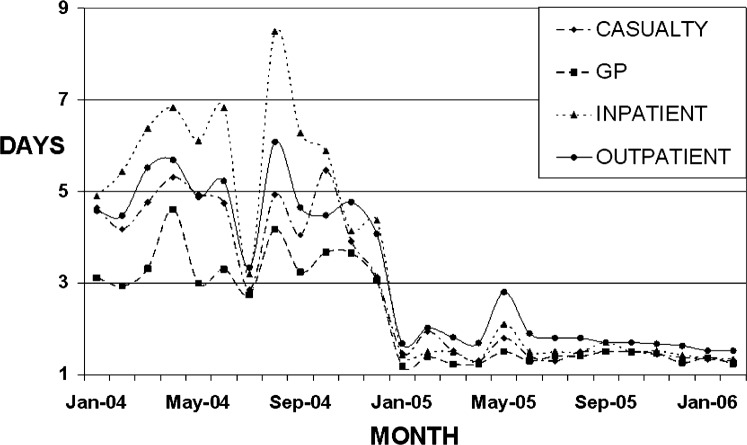
A large, sustained reduction in time to report completion was noted in all referral groups at both trust sites (Tables 1 and 2, Figures 2 and 3).
Table 1. Reporting data prea and postb introduction of speech recognition reporting (Site 1).
| Mean studies per month |
Mean time to report (days) |
Mean time to complete (days) |
||||
| Pre (SD) | Post (SD) | Pre (SD) | Post (SD) | Pre (SD) | Post (SD) | |
| Casualty | 2040 (159) | 2271 (146) | 2.00 (0.39) | 1.75 (0.30) | 6.29 (0.78) | 1.76 (0.32) |
| GP | 1056 (56) | 1077 (105) | 1.78 (0.35) | 1.65 (0.28) | 6.00 (0.70) | 1.84 (0.79) |
| Inpatient | 2850 (140) | 2741 (198) | 2.90 (0.78) | 2.67 (1.12) | 9.10 (1.50) | 2.90 (1.39) |
| Outpatient | 4094 (306) | 4196 (380) | 2.83 (0.65) | 2.45 (0.61) | 8.72 (1.29) | 2.75 (1.14) |
aJanuary 2004 to November 2004.
bDecember 2004 to February 2006.
Table 2. Reporting data prea and postb introduction of speech recognition reporting (Site 2).
| Mean studies per month |
Mean time to report (days) |
Mean time to complete (days) |
||||
| Pre (SD) | Post (SD) | Pre (SD) | Post (SD) | Pre (SD) | Post (SD) | |
| Casualty | 901 (58) | 941 (76) | 1.38 (0.11) | 1.48 (0.18) | 4.52 (0.74) | 1.60 (0.46) |
| GP | 832 (54) | 815 (111) | 1.27 (0.11) | 1.36 (0.12) | 3.44 (0.56) | 1.44 (0.45) |
| Inpatient | 2827 (167) | 3003 (333) | 1.44 (0.26) | 1.52 (0.19) | 5.84 (1.43) | 1.66 (0.76) |
| Outpatient | 2786 (197) | 2585 (218) | 1.63 (0.11) | 1.79 (0.31) | 4.87 (0.74) | 1.92 (0.66) |
aJanuary 2004 to November 2004.
bDecember 2004 to February 2006.
Figure 2.
Time to report completion (Site 1). The baseline has been set at 1. The Radiology Information System in use during the study period recorded completion times in integers. All reports completed in ≤1 day are therefore allocated a completion time of 1 day.
Figure 3.
Time to report completion (Site 2). The baseline has been set at one. The Radiology Information System in use during the study period recorded completion times in integers. All reports completed in less than one day are therefore allocated a completion time of one day.
It should be noted that the RIS in place during the period of the study recorded report completion times in whole days. The lowest reporting time entry is therefore 1 day and the baseline on the graphs has been set appropriately (in reality, the majority of films are reported in less than 24 h).
An independent two-sample Student’s t-test was used to compare the overall mean number of studies per month, mean time to report and mean time to completion pre and post introduction of SRR. There was no significant difference in the mean number of studies per month (17 387 ± 793 pre-SRR and 17 657 ± 911 post/SRR, p = 0.45) or the mean time to report (2.11 ± 0.35 days pre-SRR and 2.00 ± 0.42 days post-SRR, p = 0.50). The decrease in mean time to completion was statistically significant (6.79 ± 0.92 days pre-SRR and 2.20 ± 0.78 days post-SRR, p<10−11).
Discussion
Since December 2004, all radiology reporting in the trust has been carried out using SRR. Our data show the impact of speech recognition reporting on report completion times at both sites and from all referral sources. The lag-time of one month before a full reduction in report completion times was achieved at Site 1 was actually due to a large backlog of reports dictated onto tape in November being transcribed during early December, rather than a consequence of a learning curve associated with the transition to speech recognition. SRR eliminated the delays associated with report transcription and subsequent verification/authorisation. A substantial improvement in the quality of service to referring clinicians, and consequently patients, has been achieved: inpatient or emergency studies can be available on PACS before the patient returns to the ward. Outpatients are frequently booked to attend clinics on the same visit as an imaging procedure, as reports are usually available by the time of the clinic appointment.
A “total” (where SRR immediately becomes the only means of reporting) rather than piecemeal approach to implementation avoids the inherent inefficiencies in maintaining two streams of practice and allows any cost-savings to be realised fully. Our SRR transition was implemented following a period of consultation involving radiologists, radiographers, the information technology department, secretarial staff and management. An inclusive approach at an early stage encouraged acceptance and the subsequent success of the new system [12]. Extensive pre-launch testing and trouble-shooting was conducted on a stand-alone computer and PACS using dummy studies, which included historical examinations on the same test patients. All possible reporting scenarios were simulated and the testing was performed by a multidisciplinary team including a radiologist, engineers from the PACS, RIS and speech recognition vendors, and hospital IT personnel. Training for all users was conducted in the week before the implementation date. Application specialists were available on-site to give support and to deal with “teething problems” for several days during implementation. The period before Christmas was selected for the transition because a seasonal reduction in outpatient workload was anticipated.
The SRR software is fully integrated with the RIS and PACS, and direct access to the system from within the PACS software means that additional viewing screens are not required. Reporting is carried out from PACS worklists searchable by site, modality, body part, date and reporting status. In practice, most are reported by modality from “unreported” worklists or “recent exams”. Selecting a study populates patient information (and clinical details) on the screen and automatically attaches it to the voice dictation file, eliminating the need for manual or verbal entry of demographic data. Indeed, the radiologist has no direct contact with the RIS; the workstations display only the PACS platform and the embedded SRR system. Full system integration, opening both images and dictation following a single mouse-click, is vital to derive maximum benefit from SRR. The transient increase in report completion times in May or June 2005 was due to a system upgrade that caused an unforeseen integration problem. (The upgraded software had been tested on a higher specification platform than that extant in the Imaging Department; thus, integration problems between the upgraded SRR, RIS and PACS had not been pre-empted.) Efficient communication and interaction between the various system providers is clearly vital when systems are so closely integrated.
Some radiologists remain sceptical of the benefits of SRR, despite evidence of improvements in report turnaround times. Manufacturers claim an accuracy in excess of 95% for the majority of users, but reported error rates for speech recognition systems in radiology vary from 4% to 28% [9–11]. The majority of these errors do not result in clinically relevant misinterpretation, but proofreading of dictated text is required (in the same way that proofreading of reports transcribed by secretaries is necessary). In our experience, the majority of reports require little or no alteration. The facility to update and adapt the vocabulary reduces the number of corrections necessary.
It has been suggested that SRR causes “secretarial” workload to be transferred to the radiologist, reducing productivity [7, 8]. This may be valid if transcriptionists are efficient and invariably accurate. Within our large city-hospital practice, however, recruitment and retention of sufficient numbers of well-trained radiological secretaries was not possible. Checking and authorising inaccurate reports at a later date, when the images might need to be re-examined to make sense of the report, is time-consuming; all our radiologists check and authorise reports immediately after dictation. The facility to check and authorise reports whilst the images are still displayed represents an important advantage of the SRR system. In the UK, The Royal College of Radiologists guidelines suggest that reports should be proofread and authorised at the time of transcription and whilst viewing the relevant images [13]. Some departments have addressed this by removing the authorisation step altogether for plain film reporting, which saves time but introduces scope for error. Reducing the number of workflow steps places the radiologist in control of the entire process and the short time invested in proofreading and making brief corrections to the speech recognition text is offset by significant reduction in interruptions from clinical staff seeking reports on studies that have been dictated but not typed or authorised. User-generated standardised report templates and macros for more complex imaging reports (e.g. cardiac MRI) and for normal examinations also speed up the reporting process.
Conclusions
Despite the obvious advantages of speech recognition systems integrated with PACS and RIS, resistance to change has led to partial introduction of SRR alongside traditional reporting and transcription methods in some institutions. This is likely to result in suboptimal implementation of SRR and risks inconsistency in the various report databases. Furthermore, close integration of the SRR with pre-existing systems is vital for success: reporting from PACS worklists with an embedded SRR allows the radiologist to continue to work efficiently. Overall, our experience demonstrates the dramatic, positive impact that a well-planned, organisation-wide implementation of SRR can have on radiology service delivery.
References
- 1.Rosenthal DI, Chew FS, Dupuy DE, Kattapuram SV, Palmer WE, Yap RM, et al. Computer-based speech recognition as a replacement for medical transcription. AJR Am J Roentgenol 1998;170:23–5 [DOI] [PubMed] [Google Scholar]
- 2.Marquez LO. Improving medical imaging report turnaround times. Radiol Manage 2005;27:34–7 [PubMed] [Google Scholar]
- 3.Sferrella SM. Success with voice recognition. Radiol Manage 2003;25:42–9 [PubMed] [Google Scholar]
- 4.Wheeler S, Cassimus GC. Selecting and implementing a voice recognition system. Radiol Manage 1999;21:37–42 [PubMed] [Google Scholar]
- 5.Kauppinen T, Koivikko MP, Ahovuo J. Improvement of report workflow and productivity using speech recognition — a follow-up study. J Digit Imaging 2008;21:378–82 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ramaswamy MR, Chaljub G, Esch O, Fanning DD, van Sonnenberg E. Continuous speech recognition in MR imaging reporting: advantages, disadvantages, and impact. AJR Am J Roentgenol 2000;174:617–22 [DOI] [PubMed] [Google Scholar]
- 7.Bhan SN, Coblentz CL, Norman GR, Ali SH. Effect of voice recognition on radiologist reporting time. Can Assoc Radiol J 2008;59:203–9 [PubMed] [Google Scholar]
- 8.Gale B, Safriel Y, Lukban A, Kalowitz J, Fleischer J, Gordon D. Radiology report production times: voice recognition vs. transcription. Radiol Manage 2001;23:18–22 [PubMed] [Google Scholar]
- 9.Pezzullo JA, Tung GA, Rogg JM, Davis LM, Brody JM, Mayo-Smith WW. Voice recognition dictation: radiologist as transcriptionist. J Digit Imaging 2008;21:384–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quint LE, Quint DJ, Myles JD. Frequency and spectrum of errors in final radiology reports generated with automatic speech recognition technology. J Am Coll Radiol 2008;5:1196–9 [DOI] [PubMed] [Google Scholar]
- 11.Rana DS, Hurst G, Shepstone L, Pilling J, Cockburn J, Crawford M. Voice recognition for radiology reporting: is it good enough? Clin Radiol 2005;60:1205–12 [DOI] [PubMed] [Google Scholar]
- 12.Bramson RT, Bramson RA. Overcoming obstacles to work-changing technology such as PACS and voice-recognition. AJR Am J Roentgenol 2005;184:1727–30 [DOI] [PubMed] [Google Scholar]
- 13.Board ofFacultyofClinicalRadiology , The RoyalCollegeofRadiologists Risk Management in Clinical Radiology. London: The Royal College of Radiologists, 2002 [Google Scholar]