Abstract
The aim of this study was to investigate the movement, and the factors that influence such movement, of pancreatic lesions and to provide a reference for determination of planning target volume (PTV) during stereotactic radiotherapy. We implanted 19 gold markers into the inner pancreatic tumours of 16 pancreatic carcinoma patients percutaneously under B-ultrasonographic guidance. The marked motion of pancreatic lesions in the x (right–left), y (superoinferior) and z (anteroposterior) directions was measured using an X-ray simulator system. Based on the statistical analysis of the detected movements, we investigated the relevant influencing factors of pancreatic lesions with multinomial linear regression. Data showed that the mean motion amplitudes of pancreatic lesions were 0.16 cm ± 0.06 (range 0.1–0.3 cm) in the x direction, 0.25 cm ± 0.12 (range 0.1–0.4 cm) in the y direction and 0.88 cm ± 0.24 (0.5–1.6 cm) in the z direction. Motion amplitude was not correlated with the height, weight or age of the patients nor with the location or size of the tumour. The motion of pancreatic lesions was mainly influenced by the respiratory motion and has maximal amplitude in the z direction. Therefore, motion in the z direction should be given a priority consideration while determining the PTV.
Pancreatic carcinoma is a kind of malignant tumour that develops rapidly and has poor prognosis. Approximately 80% of patients have lost the opportunity of surgical removal at the time of their diagnosis [1]. Radiotherapy or combination therapies such as concomitant radiochemotherapy are employed as primary treatments. Stereotactic radiotherapy technology requires that physiological movements (e.g. respiratory motion, cardiac impulse, etc.) of thoracic and abdominal malignancies be taken into account in the formulation of the planning target volume (PTV) margin for uncertainty. Therefore, an analysis of the distance of displacement of pancreatic lesions may be of interest in further establishing the pattern of motion, as well as the factors that intensify such motion, and provide clinically useful information in determining the extent of the margin for uncertainty during irradiation of such lesions.
Methods and materials
Patient information
Patients were included from among those who received CyberKnife® radiosurgery treatment using the Synchrony® (Accuracy Incorporated, Sunnyvale, CA) respiratory tracking system for pancreatic carcinoma between 2006 and 2008, and the first step was to insert the gold markers into or near the tumour. Those with acute or chronic respiratory diseases, abnormal cardiac function, ascites and abdominal cavity infection were excluded from the study. The 16 patients, 10 men and 6 women, were of a median age 59.5 years (range 43–86 years), height 162.5 cm (range 145–180 cm) and weight 58.7 kg (range 37–75 kg). The lesions, average volume 68.69 ml (range 13.5–148.0 ml), were located in the body of pancreas in 5 cases and in the head of pancreas in 11.
Equipment and measurements
Under B-ultrasound guidance, one or two gold markers 5 mm long and 0.8 mm diameter were implanted percutaneously into the pancreatic tumour. The total number of markers for the 16 patients was 19. When the locations were confirmed by abdominal CT 1 week later, the recorded motion amplitudes were measured by an X-ray simulator system and the movement data were recorded in millimetres. Before measurement, patients were asked to lie down, relax, keep their hands under their head and, in particular, to relax their abdominal muscles. The measurements began when the patient's breathing had stabilised. We measured the motion of the markers in the z (anteroposterior) and x (right–left) directions when the gantry of the simulator system was set to 0°, and in the y (superoinferior) direction when that angle was set to 90°. We recorded maximum movement of the gold markers in each direction through five to eight respiratory cycles as detected by the simulator system. In three patients, two gold markers were implanted into the pancreatic tumour. In these cases, only one of the markers was tracked for measurement, as the motion patterns of the two markers were determined to be identical.
Statistical analysis
The means in pairs, with different factors in three directions, were analysed using SPSS13.0 software (SPSS Incorporated, Chicago, IL) for the t-test, and the potential influencing factors were analysed by the multiple linear regression model.
Results
Implantation of gold markers
Gold markers were implanted percutaneously under B-ultrasound guidance and their position was confirmed with CT (Figures 1 and 2).
Figure 1.

The location of gold markers under B-ultrasound image.
Figure 2.
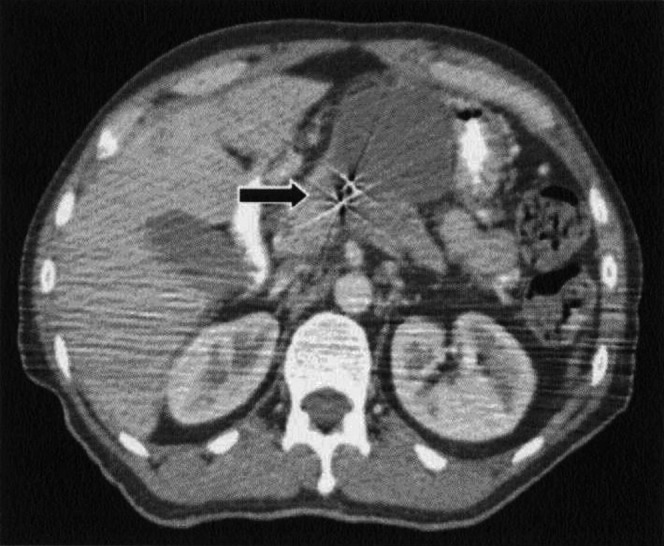
The location of gold markers under CT image.
Means and standard deviations of fiducial movements
During measurements, we found that the movement patterns of the markers were in accord with respiratory movement, and the markers always returned to the starting point of each co-ordinate direction at the end of a respiratory cycle. The mean motion amplitude of pancreatic lesions were 0.88 cm ±0.24 (range 0.5–1.6 cm) in the z direction; 0.16 cm ± 0.06 (range 0.1–0.3 cm) in the x direction; and 0.25 cm ±0.12 (0.1–0.4 cm) in the y direction. The analyses of potential factors of influence are shown in Tables 1–4.
Table 2. Multiple linear regressions analysis of influencing factors for motion in the x direction.
| Factor | β | SE | t | p |
| Age (years) | 0.001 | 0.002 | 0.447 | 0.664 |
| Height (cm) | 0.001 | 0.003 | 0.500 | 0.627 |
| Weight (kg) | −0.001 | 0.002 | −0.306 | 0.765 |
| Lesion size (ml) | 0.000 | 0.001 | 0.825 | 0.427 |
Table 1. Comparison results of different factors.
| Content | Number | z | t | p | x | t | p | y | t | p |
| Gender | 0.523 | 0.609 | 0.298 | 0.770 | 0.435 | 0.670 | ||||
| Male | 10 | 0.90±0.29 | 0.16±0.07 | 0.26±0.13 | ||||||
| Female | 6 | 0.83±0.12 | 0.15±0.05 | 0.23±0.10 | ||||||
| Age (years) | 0.458 | 0.654 | −0.843 | 0.414 | 0.642 | 0.531 | ||||
| ≤60 | 9 | 0.90±0.31 | 0.14±0.05 | 0.27±0.11 | ||||||
| >60 | 7 | 0.84±0.11 | 0.17±0.08 | 0.23±0.13 | ||||||
| Height (cm) | 0.774 | 0.452 | −0.740 | 0.472 | −0.642 | 0.531 | ||||
| ≤160 | 7 | 0.93±0.31 | 0.14±0.05 | 0.23±0.10 | ||||||
| >160 | 9 | 0.83±0.18 | 0.17±0.07 | 0.27±0.13 | ||||||
| Weight (kg) | 0.458 | 0.654 | −0.048 | 0.962 | −0.211 | 0.836 | ||||
| ≤60 | 9 | 0.90±0.28 | 0.16±0.07 | 0.24±0.11 | ||||||
| >60 | 7 | 0.84±0.19 | 0.16±0.05 | 0.26±0.13 | ||||||
| Position of lesions | 0.831 | 0.420 | −1.019 | 0.325 | 0.688 | 0.503 | ||||
| Pancreatic head | 11 | 0.91±0.26 | 0.15±0.07 | 0.26±0.12 | ||||||
| Pancreatic body | 5 | 0.80±0.20 | 0.18±0.04 | 0.22±0.11 | ||||||
| Lesion size (ml) | −0.312 | 0.760 | −0.298 | 0.770 | 0.888 | 0.389 | ||||
| ≤27 | 6 | 0.85±0.14 | 0.15±0.08 | 0.28±0.12 | ||||||
| >27 | 10 | 0.89±0.29 | 0.23±0.12 | 0.16±0.05 |
Table 3. Multiple linear regressions analysis of influencing factors for motion in the y direction.
| Factor | β | SE | t | p |
| Age (years) | 0.000 | 0.003 | 0.120 | 0.907 |
| Height (cm) | 0.004 | 0.006 | 0.667 | 0.519 |
| Weight (kg) | −0.002 | 0.004 | −0.526 | 0.609 |
| Lesion size (ml) | −9.2E-5 | 0.001 | −0.096 | 0.925 |
Table 4. Multiple linear regressions analysis of influencing factors for motion in the z direction.
| Factor | β | SE | t | p |
| Age (years) | −0.002 | 0.006 | −0.360 | 0.726 |
| Height (cm) | −0.012 | 0.011 | −1.051 | 0.316 |
| Weight (kg) | 0.004 | 0.008 | 0.469 | 0.648 |
| Lesion size (ml) | 0.001 | 0.002 | 0.533 | 0.604 |
Discussion
Conformal radiotherapy requires irradiation fields to be as small as possible to increase the dose to the tumour but spare nearby normal tissues. Changes in volume and motional range due to respiratory or other physiological movement of nearby organs can grossly influence the targeting of thoracic and abdominal tumours [2]. The displacement of thoracic and abdominal organs due to respiration and its influence on targeting have been measured using X-ray imaging, CT scans, four-dimensional CT, B-ultrasound imaging and MRI [3–6]. However, reports on the range and characteristics of movement of pancreatic lesions are scarce.
In 2002, Ozhasoglu and Murphy [7] implanted a gold marker into the tumour of a pancreatic cancer patient and marked the location on the thoracic surface. Using this approach, the motions of the internal tumour marker and the thoracic surface marker were observed on the same X-ray fluoroscopy screen. Their results showed that the right–left and anteroposterior motions of the pancreatic lesions were quite complicated. The respiratory movement and the cardiac impulse both contributed to the movement in these directions; the periodic anteroposterior displacement caused by cardiac impulse could reach half that of the total displacement of the tumour; the anteroposterior motion of the interior marker was not correlated with the motion of the marker on the thoracic surface; the motion in the superoinferior direction was relatively regular; it was influenced only by the respiratory movement and was linearly correlated with the anteroposterior motion of the marker on the thoracic surface. In 2000, Murphy et al [6] also analysed the motion of an internal tumour marker over time and its relationship with respiratory motion as well as the cardiac impulse. Their results were similar to those of Ozhasoglu and Murphy [7]. In 2002, Murphy et al [8] implanted four gold markers around each tumour of four pancreatic cancer patients and took these as reference points and reference markers of the portal image. The locations of these markers were verified by X-ray fluoroscopy. They found that pancreatic lesions were not only influenced by respiratory motion but also forced by the heart to move about ±1 mm in the right–left direction. When the respiration movement was regulated by breath-holding, the uncertainty of the location of the pancreatic tumours in the small sample was reduced to 2.5 mm. It was concluded that the method of breath-holding could be used to reduce the mobility of pancreatic lesions to <2 mm among representative patients with pancreatic tumours. Suramo et al [4] compared the mobility of the lesions during free respiration with that under the breath-holding conditions by means of the respiratory gating technique. The mobility of the lesions was found to decrease from 20 mm to 1 mm.
The purpose of our research in this paper has been to identify any general rules affecting the motion of pancreatic lesions, and then offer guidance for the clinical construction of PTVs for pancreatic tumours so as to increase the dose to the tumour through stereotactic radiotherapy and reduce serious side effects (such as stomach or duodenal ulcer, or haemorrhage in the digestive tract). Our results are notably different from the findings of related researchers but similar to the results of Murphy et al [6]. The differences are possibly due to different methods of measurement and racial disparity. Nevertheless, our method is more representative of the real-time movements of pancreatic lesions during radiation treatment. Our results also indicate that the movement of the markers in the superoinferior direction is apparently more pronounced than movements in the left–right or anteroposterior direction. This may be caused by respiration motion, whose influence is mainly in the superoinferior direction. Among all our cases, there was only one patient whose markers moved farther (1.6 cm) than the rest of the patients (0.5–1.0 cm) in the superoinferior direction, i.e. the movements of more than 90% of the internal markers were less than or equal to 1 cm in this direction, whereas they were comparatively stationary in other directions (0.1–0.4 cm). Although our sample was not large enough to explore the general laws that govern movement of pancreatic lesions, our results still offer a reference for determining the margin of uncertainty for PTV. In addition, we compared related factors by multiple linear regression analysis. No factors were discovered that can impact movement in all three directions. In an earlier report, Bhasin et al [9] had shown that pancreatic motion did not behave differently with respect to age, gender, calcification of the pancreas and application of a drainage tube. No correlation between pancreatic motion and gender, age, height and weight was found in the results of Busselsa et al [3] either. However, Bhasin et al [9] did find that the difference between pancreatic motion of people more than 60 years old and that of younger people could be as large as 1 cm. In our future work, we will continue to examine the motion of pancreatic lesions in order to gain better insight into this subject.
In summary, respiratory movement is the main factor influencing the movement of pancreatic lesions in the superoinferior direction. In addition to respiratory movement, the beating of the heart can also affect the motion of pancreatic lesions in the left–right and anteroposterior directions. Therefore, in determining margins of the PTV, especially in the estimation of the margin of uncertainty around the gross tumour volume, one should be mainly concerned with the movement in the superoinferior direction. Furthermore, respiratory control methods such as breath-hold and gating can also be used to reduce the extent of movement of pancreatic tumours during radiotherapy and, therefore, increase the irradiation dose to the target volume with a rapid dose fall-off, so that the local control rates can be improved and the complications of the normal tissues can be reduced.
References
- 1.Warshaw AL, Fernandez-del Castillo C. Pancreatic carcinoma. N Engl J Med 1992;326:455–65 [DOI] [PubMed] [Google Scholar]
- 2.Horst E, Micke O, Moustakis C, Schuck A, Schater U, Willich NA. Conformal therapy for pancreatic cancer: variation of organ position due to gastro intestinal distention implications for treatment planning. Radiology 2002;222:681–6 [DOI] [PubMed] [Google Scholar]
- 3.Bussels B, Goethals L, Feron M, Bielen D, Dymarkowski S, Suetens P, et al. Respiration-induced movement of the upper abdominal organs: a pitfall for the three-dimensional conformal radiation treatment of pancreatic Cancer. Radiother Oncol 2003;68:69–74 [DOI] [PubMed] [Google Scholar]
- 4.Suramo I, Päivänsalo M, Myllylä V. Cranio-caudal movements of the liver, pancreas and kidneys in respiration. Acta Radiol Diag 1984;25:129–31 [DOI] [PubMed] [Google Scholar]
- 5.Bryan PJ, Custar S, Haaga JR, Balsara V. Respiration movement of the pancreas: an ultrasonic study. J Ultrasound Med 1984;3:317–20 [DOI] [PubMed] [Google Scholar]
- 6.Murphy MJ, Adler JR, Jr, Bodduluri M, Dooley J, Forster K, Hai J, et al. Image-guided radiosurgery for the spine and pancreas. Computer Aided Surg 2000;5:278–88 [DOI] [PubMed] [Google Scholar]
- 7.Ozhasoglu C, Murphy MJ. Issues in respiratory motion compensation during external-beam radiotherapy. Int J Radiat Oncol Biol Phys 2002;52:1389–99 [DOI] [PubMed] [Google Scholar]
- 8.Murphy MJ, Martin D, Whyte R, Hai J, Ozhasoglu C, Le QT. The effectiveness of breath-holding to stabilize lung and pancreas tumors during radiosurgery. Int J Radiat Oncol Biol Phys 2002;53:475–82 [DOI] [PubMed] [Google Scholar]
- 9.Bhasin DK, Rana SS, Chandail VS. The pancreas and respiration: oblivious to the obvious. J Pancreas 2006;7:578–83 [PubMed] [Google Scholar]


