Abstract
Objectives
This study used a postal survey to assess the current use of small bowel imaging investigations for Crohn’s disease within National Health Service (NHS) radiological practice and to gauge gastroenterological referral patterns.
Methods
Similar questionnaires were posted to departments of radiology (n = 240) and gastroenterology (n = 254) identified, by the databases of the Royal College of Radiologists and British Society of Gastroenterologists. Questionnaires enquired about the use of small bowel imaging in the assessment of Crohn’s disease. In particular, questionnaires described clinical scenarios including first diagnosis, disease staging and assessment of suspected extraluminal complications, obstruction and disease flare. The data were stratified according to patient age.
Results
63 (27%) departments of radiology (20 in teaching hospitals and 43 in district general hospitals (DGHs)) and 73 (29%) departments of gastroenterology replied. These departments were in 119 institutions. Of the 63 departments of radiology, 55 (90%) routinely performed barium follow-though (BaFT), 50 (80%) CT, 29 (46%) small bowel ultrasound (SbUS) and 24 (38%) small bowel MRI. BaFT was the most commonly used investigation across all age groups and indications. SbUS was used mostly for patients younger than 40 years of age with low index of clinical suspicion for Crohn’s disease (in 44% of radiology departments (28/63)). MRI was most frequently used in patients under 20 years of age for staging new disease (in 27% of radiology departments (17/63)) or in whom obstruction was suspected (in 29% of radiology departments (18/63)). CT was preferred for suspected extraluminal complications or obstruction (in 73% (46/63) and 46% (29/63) of radiology departments, respectively). Gastroenterological referrals largely concurred with the imaging modalities chosen by radiologists, although gastroenterologists were less likely to request SbUS and MRI.
Conclusion
BaFT remains the mainstay investigation for luminal small bowel Crohn’s disease, with CT dominating for suspected extraluminal complications. There has been only moderate dissemination of the use of MRI and SbUS.
Crohn’s disease is a chronic inflammatory condition of the bowel that predominately affects the young and requires lifelong medical and often surgical therapy [1]. It affects approximately 60 000 people in the UK (around 1 in 1000), with between 3000 and 6000 new diagnoses made each year. Crohn’s disease can affect the digestive system anywhere from the mouth to the anus, but most commonly affects the small intestine and/or colon. Despite advances in technology, the small bowel remains relatively inaccessible to conventional endoscopic techniques. Thus, radiological imaging plays a major role in the assessment and diagnosis of both luminal small bowel disease and extra-enteric complications.
Although barium fluoroscopy and CT remain the conventional tests used to investigate Crohn’s disease, both impart a significant radiation dose to patients [2,3]. This is of major importance given the relative youth of the patient population afflicted by Crohn’s disease [4]. The recently published European evidence-based consensus on the diagnosis and management of Crohn’s disease [5] states “the radiation burden from fluoroscopy and CT is considerable, so alternatives such as ultrasound and MRI should be considered when possible”. Advocates of ultrasound and particularly MRI suggest that these modalities could be the ideal “one stop shop” in Crohn’s disease imaging, allowing evaluation of luminal, mural and extramural disease. There is, however, a relatively small evidence base upon which to rationalise the implementation of new imaging technologies within the NHS, and the extent to which they have been disseminated into routine UK clinical practice is unclear. The purpose of the survey reported here was therefore to assess the current use of individual small bowel imaging investigations for Crohn’s disease within the National Health Service (NHS) radiological practice, and to gauge current gastroenterological referral patterns.
Methods and materials
Two similar questionnaires were devised for distribution to UK NHS departments of radiology and gastroenterology (Appendices A and B). The questionnaires asked for information on various clinical scenarios relevant to the use of imaging in the diagnosis and management of Crohn’s disease, including first diagnosis of small bowel disease, small bowel staging in known disease, assessment of suspected extraluminal complications and possible obstruction, and imaging of suspect disease flare. They were devised in collaboration with local gastroenterologists who approved the clinical definitions that were used.
Additional information that was captured by the radiological questionnaire included the type of hospital (teaching, district general or other) and the specific use of oral contrast agent if small bowel MRI was being performed. Space for additional comment was included on the questionnaires. Conventional endoscopy is, in the main, at the disposal of clinicians rather than radiologists; hence, only the gastroenterological questionnaire included colonoscopy as an investigatory option. The imaging options available to gastroenterologists were also simplified (e.g. MRI techniques were not subdivided into enterography and enteroclysis) in order to improve respondent compliance and reduce any potential confusion regarding imaging terminology.
For each question, respondents were permitted to tick more than one imaging test if more than one test was routinely performed concurrently. Importantly, in each clinical scenario, patients were substratified according to age so as to capture data on any perceived barrier to the use of tests involving exposure to ionising radiation in younger cohorts.
Questionnaire distribution
A list of UK departments of radiology was obtained from the Royal College of Radiologists with approval from the Audit Committee. A list of gastroenterology departments was obtained from the British Society of Gastroenterologists. In January 2008, questionnaires were sent out to the clinical directors of 240 departments of radiology and 254 departments of gastroenterology, each with a covering letter asking that the questionnaire be given to the most appropriate clinician in the department to fill out. A stamped addressed envelope was included for return of the questionnaires. The questionnaires were sent out a second time 2 months later to departments that had not replied. A copy of the questionnaire was also posted on the British Society of Gastrointestinal and Abdominal Radiologists website, and their members were invited to participate if their hospital had not done so already.
Results
Final return rates were 27% for radiology departments (63 replies from 20 teaching hospitals and 43 district general hospitals (DGHs)) and 29% for departments of gastroenterology (73 replies). For 17 hospitals, both the radiology and gastroenterology departments replied.
Tests offered and overall frequency of use
55 of the 63 radiology departments (90%) routinely performed barium studies. Barium follow-through was the most commonly performed procedure, with an average of 15.4 examinations per department per month (range 1–50 examinations), of which 67% were for suspected diagnosis and 33% for disease follow-up. 22 (35%) radiology departments offered barium enteroclysis (with 59% of such examinations being carried out in cases of suspected disease).
44 (72%) departments performed CT with oral contrast, averaging 5.1 scans per department per month (range 1–20 scans). Of the CT scans performed, 51% were in cases of suspected disease whereas 49% were for disease follow-up. CT enteroclysis was performed in 7 (11% of total departments) centres, 5 of which were teaching hospitals.
46% (29/63) of radiology departments offered small bowel ultrasound (SbUS), on average 7.5 examinations per department per month (range 1–30 examinations), 61% of these examinations were for suspected disease and 39% were for follow-up. 13 of the 29 centres that offered SbUS were teaching hospitals.
Just 38% (24/63) of the radiology departments who replied offered any small bowel MRI service. On average, 5.04 scans were performed per department per month (range 1–20 scans) in those departments that offered MRI, of which 60% were performed for disease follow-up. When departments provided information about their preferred oral contrast regime for MRI, Kleen prep and mannitol were each preferred by 21% of departments, locust bean gum/mannitol solution by 12.5% and Gastrograffin by 9%. 7 centres (6 of which were teaching hospitals) offered MR enteroclysis, performing an average of 78 such investigations each month between them (mean 11.1 investigation per centre per month), the majority of which were (62%) for disease follow-up.
11 radiology departments (6 in teaching hospitals) performed an average of 83 capsule endoscopies per month between them, 64% for suspected disease.
Use of tests according to indication
Radiologists
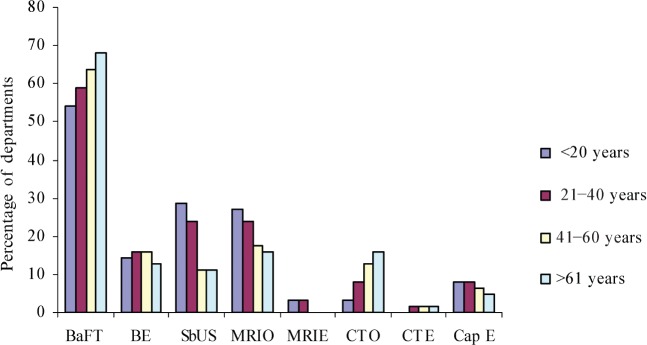
Barium follow-through was the most commonly used investigation across all age groups for imaging of the small bowel in newly diagnosed Crohn’s disease (Figure 1). For example, 34 (54%) radiology departments used it in those younger than 20 years of age and 43 (68%) for patients above the age of 61 years. SbUS and MRI were used more frequently in patients below 40 years of age, but even then only in 18 (29%) and 17 (27%) departments, respectively. CT was infrequently used for this indication in patients below 40 years of age; in fact CT was used even in those over 60 years of age by just 10 (16%) of departments. 60% of departments used a single imaging modality, with the remainder offering more than one test in combination.
Figure 1.
First-line investigation performed by radiologists in newly diagnosed Crohn’s disease patients. Barium follow-through (BaFT) is most commonly used, whereas small bowel ultrasound (SbUS) and MRI (oral contrast) (MRIO) are used relatively more frequently in younger patients. BE, barium enteroclysis; Cap E, capsule endoscopy; CTE, CT enteroclysis; CTO, CT (oral contrast); MRIE, MRI enteroclysis.
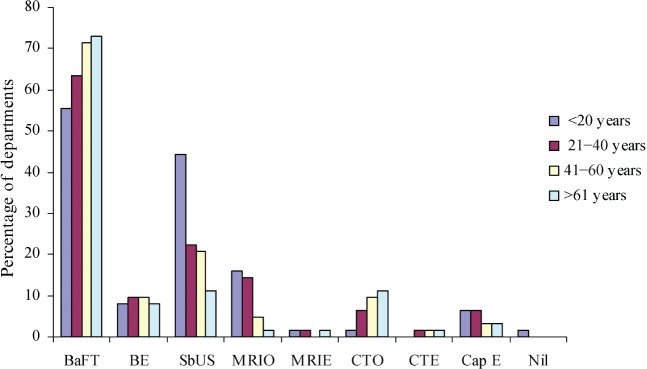
Similarly, in patients with a suspected but unconfirmed diagnosis of small bowel Crohn’s disease, barium follow-through was the most commonly used investigation, regardless of whether there was high or low clinical suspicion of disease (used in 42 (67%) departments averaged across the age groups). Interestingly, in those with a low index of clinical suspicion for Crohn’s disease, SbUS was used relatively commonly, particularly in those aged below 20 years (28 (44%) of departments) (Figure 2). Once again CT was used infrequently, most often for older patients; even then, just 12 departments (19%) used CT for patients aged over 61 years with a high clinical suspicion of disease. MRI was used most frequently in those aged less than 20 years with a high clinical suspicion (in 14 (22%) departments).
Figure 2.
Investigation in cases where there is a low index for clinical suspicion of Crohn’s disease. Barium follow-through (BaFT) is the most commonly used investigation in all age groups, whereas small bowel ultrasound (SbUS) is used relatively commonly in patients younger than 20 years. BE, barium enteroclysis; Cap E, capsule endoscopy; CTE, CT enteroclysis; CTO, CT (oral contrast); MRIE, MRI enteroclysis; MRIO, MRI (oral contrast).
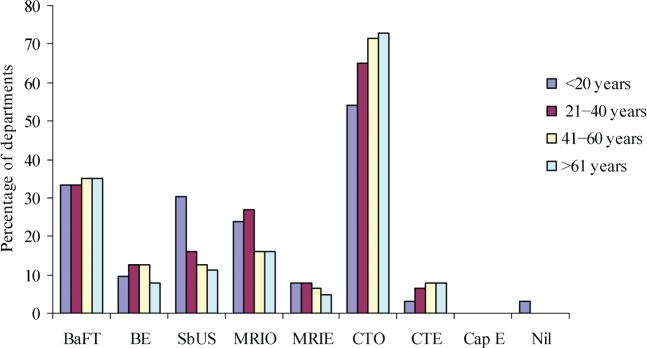
Conversely, when extraluminal complications (such as fistula or abscess) were suspected, CT became the most commonly performed examination (e.g. by 34 (54%) and 46 (73%) departments for those aged <20 and >60 years, respectively). SbUS and MRI studies were also used more commonly, but not as much as CT, in younger patients with suspected extraluminal complications (Figure 3).
Figure 3.
Investigation for suspected extraluminal complications. CT is the preferred investigation in all age groups, followed by barium follow-through (BaFT), although small bowel ultrasound (SbUS) and MRI are used with increased frequency in younger patients. BE, barium enteroclysis; Cap E, capsule endoscopy; CTE, CT enteroclysis; CTO, CT (oral contrast); MRIE, MRI enteroclysis; MRIO, MRI (oral contrast).
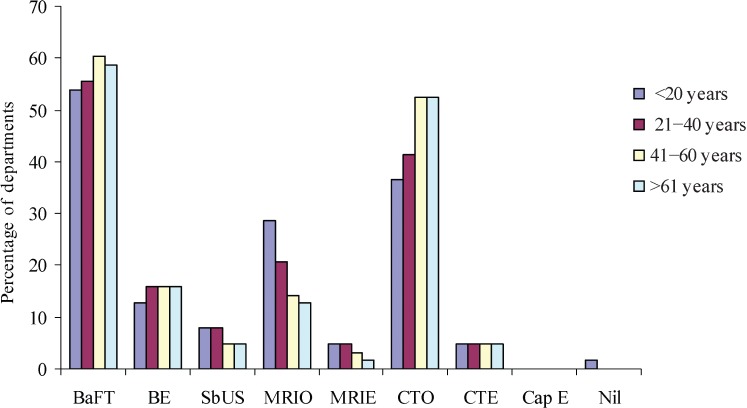
In outpatients with suspected obstruction, barium follow-through (BaFT) and CT with oral contrast (CTO) were used most frequently (in 36 (57%) and 29 (46%) of departments averaged across the age groups, respectively) (Figure 4). Once again, when MRI was used, it was mainly as a substitute for CT for younger patients: MRI was used in 18 (29%) departments in those aged less than 20 years. Again, many departments suggested that they would employ different tests concurrently (e.g. 20% would perform both BaFT and CTO).
Figure 4.
Investigation of suspected small bowel obstruction. Barium follow-through (BaFT) and CT are commonly performed, often concurrently. MRI is performed with relatively increased frequency in younger patients. BE, barium enteroclysis; Cap E, capsule endoscopy; CTE, CT enteroclysis; CTO, CT (oral contrast); MRIE, MRI enteroclysis; MRIO, MRI (oral contrast); SbUS, small bowel ultrasound.
Finally, for those with a clinically suspected flair needing re-evaluation of the small bowel, BaFT was the investigation of choice in 35 radiology departments (56%) averaged across the age groups, but CTO was used more frequently (in 21 (33%) departments averaged across the age groups) than it was for newly diagnosed or suspected disease. Small bowel ultrasound and MRI were used more frequently in patients younger than 20 years, and then by 20 (32%) and 13 (21%) radiology departments, respectively.
Gastroenterologists
To assess disease extent in newly diagnosed Crohn’s disease, BaFT was the most requested modality (out of the 73 gastroenterology departments who replied, 53 (73%) request it for patients older than 41 years of age and 45 (62%) for patients younger than 40 years of age). In 50% of departments, BaFT was the only imaging requested. MRI was requested in 15 (21%) departments for patients under 20 years of age, and SbUS was requested on average by 8 (11%) departments for patients older than 40 years of age. Capsule endoscopy was requested by no more than 6 (8%) departments (for any patient age group or indication) and almost always in combination with a radiological test. 70% of gastroenterologists requested only a single investigation in all age groups, whereas up to 7 (10%) departments would not perform any investigation to assess disease extent in newly diagnosed Crohn’s disease.
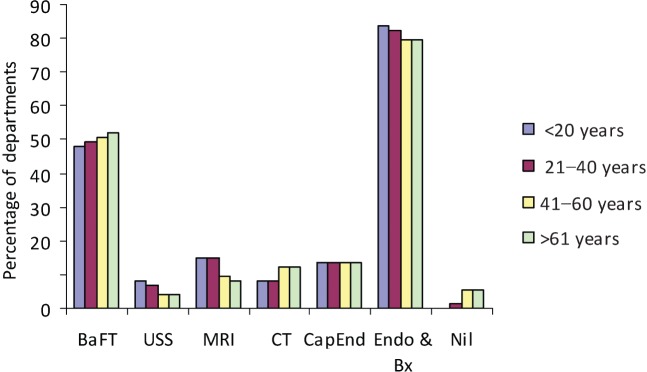
In patients with a high index of clinical suspicion for Crohn’s disease, 59 (81%) gastroenterology departments would perform endoscopy and biopsy essentially regardless of age, of which around one-third would also perform BaFT on the same patients. SbUS was the least frequently used imaging modality, requested by less than 10% of gastroenterology departments across all age groups. MRI was most frequently requested in those younger than 40 years of age, and then in just 11 (15%) departments (Figure 5).
Figure 5.
Investigations performed and/or requested by gastroenterologists for patients with high index of suspicion for Crohn’s disease. Endoscopy and biopsy with concurrent barium follow-through (BaFT) is preferred. CapEnd, capsule endoscopy; Endo & Bx, endoscopy and biopsy; USS, ultrasound.
In patients with a low clinical index of suspicion for Crohn’s disease, 14 (19%) departments would not perform any investigations. When investigations were requested, these tended to be similar to those carried out when there was a high clinical suspicion, although SbUS was requested a little more often when the clinical suspicion was low (by 9 (12%) departments in those aged below 40 years).
CT was requested regardless of patient age by 41 (57%) gastroenterology departments when assessing suspected extraluminal disease. BaFT was requested by 29 (40%) gastroenterology departments and SbUS by at most 13 (17%) (in those aged less than 20 years). MRI was more popular when extraluminal disease is suspected, being requested by 22 (30%) gastroenterology departments in patients below the age of 20 years. BaFT was the investigation of choice for assessing obstruction, being requested across all age groups by 50 (68%) gastroenterology departments.
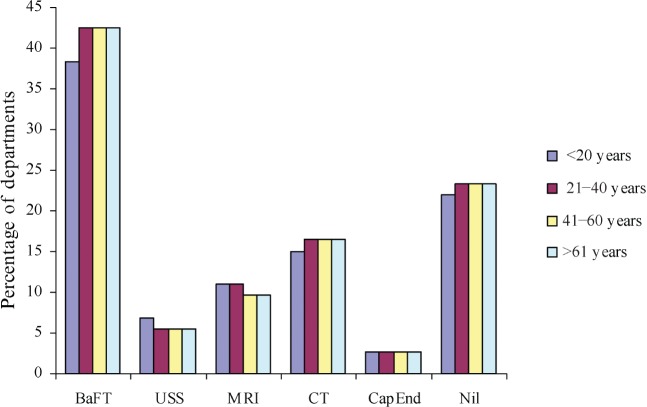
When there was a clinical flare, 17 (23%) gastroenterology departments reported that they would not request further imaging. Across all age groups, an average of 30 (41%), 4 (6%), 8 (10%) and 12 (16%) gastroenterology departments would, however, request BaFT, ultrasound, MRI and CT, respectively (Figure 6).
Figure 6.
Investigations performed and/or requested by gastroenterologists for patients with suspected clinical flare. Barium follow-through (BaFT) is the most frequently requested examination. CapEnd, capsule endoscopy; USS, ultrasound.
Comparison of the imaging preferences of radiologists and gastroenterologists
BaFT remains the preferred small bowel imaging technique for all patient groups, and its usage was similar between gastroenterologists and radiologists. There was also agreement between the two specialties in the use of CT as the primary modality for the assessment of extraluminal complications. For the assessment of a suspected obstruction, radiologists were more likely to recommend CT than gastroenterologists were to request it. Radiologists were more likely than gastroenterologists to use SbUS and MRI when assessing patients with either suspected or proven disease, especially in patients younger than 40 years of age (Figures 2 and 5).
Discussion
For many years, barium follow-through has been the routine radiological investigation for assessing known or suspected Crohn’s disease of the small bowel. Recently, however, literature is increasingly available on the alternative use of cross-sectional imaging techniques, notably SbUS, CT and MRI, for this disease. Potential advantages include the ability to better assess extramural complications, grade disease activity and, in the case of ultrasound and MRI, eliminate the radiation burden in the generally young patient cohort [6-8]. European guidelines increasingly advocate the use of cross-sectional techniques (particularly MRI and SbUS), but anecdotal evidence suggests that their dissemination in the UK has been patchy and ad hoc.
Our survey confirms that barium studies remain the imaging investigation performed most commonly for both diagnosis and assessment of Crohn’s disease in all ages. This is perhaps not surprising given this study’s availability, relative simplicity and familiarity to both radiologists and gastroenterologists alike. Furthermore, the examination remains very much part of the core curriculum training of UK radiologists, unlike more specialist investigations such as ultrasound and MRI, which as this survey shows are limited to less than 50% of UK departments. When performed well, it provides detailed analysis of the extent of diseased mucosal surfaces. It also has reasonable performance in the diagnosis of Crohn’s disease, with a sensitivity of 85–95% and a specificity of 89–94% having been documented [9]. There is evidence that the level of interpretive performance of barium enema may be suboptimal in the UK [10], and it is not clear whether small bowel fluoroscopy is suffering a similar fate as the popularity of new cross-sectional techniques increases. Although the majority of UK radiology departments now have access to MRI technology, only 38% of those departments who responded to our survey offered MRI of the small bowel, mainly for those with known Crohn’s disease or a high clinical suspicion of this disease. The aim of our survey was to assess current practice, and we did not complicate the questionnaire by collecting data on why one test was preferred over another. Recent meta-analysis of data suggests that MRI has high performance in inflammatory bowel disease [11]. Nevertheless, it is important to state that although MRI is a theoretically attractive option for imaging Crohn’s disease, no randomised trial data have confirmed its superiority over, or even equivalence to, conventional barium investigations. Without these data, it is likely that MRI small bowel provision will remain ad hoc. In addition, lack of interpretative expertise and scanner capacity certainly contribute to the low level of dissemination. It is interesting to note, however, that radiologists were more likely to use MRI than gastroenterologists were to request it. Although knowledge of the technique and the supporting data is slowly increasing amongst UK radiologists, there will inevitably be a lag period while such information permeates through to the gastroenterological community. It is also interesting to note that although MR enteroclysis probably has better sensitivity than MR enterography [11], the latter is used significantly more widely, probably because of its greater simplicity and reduced invasiveness. Different oral contrast media have been used for MR enterography, including non-absorbable osmotic laxatives (such as polyethylene glycol), mannitol, locust bean gum or a combination of these.
46% of departments performed SbUS. Although the use of ultrasound for small bowel disease has been advocated for many years, it is clear that the level of dissemination in the UK remains relatively low. The known reliance on expertise and associated steep learning curve [12], together with technical difficulties in obese or “gassy” abdomens, have always limited the uptake of SbUS, as has the general reluctance of clinicians to request the examination (which is confirmed in this survey). However, studies investigating the diagnostic accuracy of ultrasound have shown reasonable results with sensitivity ranging between 84% and 90% and specificity between 98% and 100% [13-18]. The rapidity and safety of ultrasound, together with the relative accessibility of the terminal ileum in most patients, probably explain the relatively frequent use of this technique by radiologists seeking to exclude disease, particularly in younger patients with a low underlying clinical suspicion of disease. The ability of SbUS to assess disease activity and response to treatment through the use of colour flow Doppler and contrast agents is also an advantage [19]. Both MRI and SbUS tended to be offered more frequently in teaching hospitals than in other hospitals.
CT was used infrequently in staging those without a proven diagnosis of Crohn’s disease or for assessing those with a new diagnosis. As for MRI, there are no hard data to support the superiority of CT over other tests in this context, and of course the examination imparts a reasonable radiation burden which is of special concern in this generally younger patient cohort [3,4]. Nevertheless, CT is currently preferred by most radiologists and gastroenterologists for detecting extraluminal complications (such as abscesses). Extramural complications show up well on CT, and hence CT is probably the reference standard test for the detection of intra-abdominal sepsis [20-23]. CT was also performed more frequently in those with suspected obstruction than in other patients, but despite its potential disadvantages in comparison with cross-sectional techniques, BaFT was still the most widely performed test in those with obstructive symptoms.
Evidence throughout the survey results did however show that radiation dose was considered by participants: MRI and SbUS tended to be used more frequently in younger patient groups than in older patients. Nevertheless, tests using ionising radiation (especially barium follow-through) were used more frequently than other techniques for every indication listed, even for patients below 20 years of age.
It is of note that the use of capsule endoscopy was relatively infrequent, even amongst gastroenterologists, confirming its role as a very much second-line test in Crohn’s disease. This is perhaps surprising given the known high sensitivity of capsule endoscopy in detecting early mucosal disease. The data suggest that access to this technology may be relatively limited at present, and we speculate that its use is perhaps more widespread for diagnosis in cases of unexplained gastrointestinal bleeding. Furthermore, for most of the clinical scenarios we presented in the survey, a small but not insignificant percentage of gastroenterologists would not perform any diagnostic test. For example, 19% of gastroenterology departments would not request or perform any tests for those with a low clinical suspicion of disease. In a survey of this nature, we clearly cannot recreate the real-life complexities presented by each individual patient. Nevertheless, it is interesting to observe that a percentage of gastroenterologists clearly feel the management of Crohn’s disease is possible on the basis of clinical assessment alone.
The survey does have limitations. At best, it can only provide a snap-shot of UK practice and it cannot detect changing trends in the uptake of new imaging technologies, this would require a repeat survey in the future. Our questionnaire return rate was relatively low, but perhaps not unexpected given the relatively detailed nature of the survey. We cannot, however, exclude the possibility that our sample is biased; for example, departments with an interest in small bowel imaging might have been more willing to reply. If anything, however, such bias would perhaps tend to overestimate the use of new imaging technologies. In addition, this is, at least to our knowledge, the only such survey of UK small bowel imaging carried out to date. Although we sampled radiology and gastroenterology departments separately, there was unavoidable overlap in the centres who responded, but this concerned only 17 departments. Finally, as noted above, although we allowed the responders free text space, we did not specially enquire as to reasons why one imaging test was preferred over another. Neither did we ask what, if any, were the perceived barriers to the introduction of new tests. It is, however, relatively difficult to capture these data without introducing bias within the phraseology of questions, and our main aim was to produce a simple snap-shot of the use of small bowel tests in the UK for various clinical indications.
In summary, our survey of UK radiology and gastroenterology departments showed that barium follow-though remains the most frequently performed and requested examination for known or suspect luminal small bowel Crohn’s disease, except when extraluminal complications are suspected, in which case CT is performed most frequently. There has been only moderate dissemination of new small bowel technologies: MRI and SbUS are at present performed by a minority of UK imaging departments, and their use is focused on patients aged less than 40 years. In general, radiologists are more likely to recommend MRI or SbUS than gastroenterologists are to request them. In the absence of hard trial data on which to base national guidelines, it is likely that the uptake of MRI will remain rather patchy and ad hoc. The onus is on the radiological community to produce this evidence base in order to guide the appropriate dissemination of new technologies such as small bowel MRI into standard clinic practice.
Acknowledgments
This work was undertaken at the Comprehensive Biomedical Centre, University College Hospital London, which received a proportion of its funding from the National Institute for Health Research. The views expressed in this publication are those of the authors and not necessarily those of the UK Department of Health.
Appendix A
Gastroenterologist questionnaire
1. In a patient with newly diagnosed, biopsy proven, Crohn’s disease which test(s) would you normally request to assess small bowel involvement in the following age groups? (You may tick more than one test if multiple concurrent tests are normally requested.)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enteroclysis | ||||
| Capsule endoscopy |
2. In a new patient with a high clinical suspicion of small bowel Crohn’s disease, e.g. chronic diarrhoea, abdominal pain and weight loss with anaemia, thrombocytosis and a raised CRP etc, which test would you normally request to establish a diagnosis of Crohn’s disease? (You may tick more than one test if multiple concurrent tests are normally requested.)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Colonoscopy with ileoscopy and biopsies | ||||
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enteroclysis | ||||
| Capsule endoscopy |
3. In a new patient with a low clinical suspicion of small bowel Crohn’s disease, e.g. with occasional diarrhoea, vague abdominal pain and no weight loss or anaemia, and a normal CRP, which test would you normally request to exclude small bowel Crohn’s disease? (You may tick more than one test if multiple concurrent tests are normally requested.)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Colonoscopy with ileoscopy and biopsies | ||||
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enteroclysis | ||||
| Capsule endoscopy |
4. In a patient with known small bowel Crohn’s disease in whom an extraluminal complication such as fistula or abscess is suspected, which of the following tests would you routinely request? (You may tick more than one test if multiple concurrent tests are normally requested)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enteroclysis | ||||
| Capsule endoscopy |
5. In an out-patient with known Crohn’s disease and symptoms suggestive of stricturing disease, which of the following tests would you routinely request to determine the level of obstruction? (You may tick more than one test if multiple concurrent tests are routinely requested)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enteroclysis | ||||
| Capsule endoscopy |
6. In a patient with known Crohn’s disease with a clinical flare-up of the disease, which test would you routinely request to reassess the small bowel? (You may mark more than one test if multiple concurrent tests are routinely requested)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through/enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI | ||||
| CT +/− CT enterocolysis | ||||
| Capsule endoscopy |
Appendix B
Radiologist questionnaire
1. In your department in a month, on average, how many of the following investigations do you perform for diagnosis or follow-up of small bowel Crohn’s disease? (Please put numbers in the appropriate box, if none are performed pleased place a 0 in the appropriate box)
| Investigation | Number performed for suspected diagnosis | Number performed for follow-up of disease |
| Barium follow-through | ||
| Barium enteroclysis | ||
| Small bowel ultrasound | ||
| Small bowel MRI (oral contrast) | ||
| MRI enteroclysis | ||
| CT (oral contrast) | ||
| CT enteroclysis | ||
| Capsule endoscopy |
If you perform small bowel MR please state your preferred oral contrast agent if any? _________________________
2. In a patient with biopsy proven newly diagnosed Crohn’s disease, which investigation would you normally use, if any, to assess small bowel involvement in the following age groups? (You may tick more than one investigation per age group if multiple concurrent investigations are usually performed.)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through | ||||
| Barium enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| Small bowel MRI (oral contrast) | ||||
| CT (oral contrast) | ||||
| CT enteroclysis | ||||
| Capsule endoscopy |
3. In a patient with clinical suspicion of small bowel Crohn’s disease but no biopsy proof, which of the following investigations would you normally use for diagnosis in a patient with (a) high clinical suspicion of disease and (b) low clinical suspicion of disease? (You may tick more than one investigation per age group if multiple concurrent investigations are normally performed.)
a) In a patient with high clinical suspicion of disease?
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through | ||||
| Barium enterocolysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| MRI enteroclysis | ||||
| CT (oral contrast) | ||||
| CT enteroclysis | ||||
| Capsule endoscopy |
b) In a patient with low clinical suspicion of disease?
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow- through | ||||
| Barium enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| MRI enteroclysis | ||||
| CT (oral contrast) | ||||
| CT enterocolysis | ||||
| Capsule endoscopy |
4. In a patient with known Crohn’s disease in whom an extraluminal complication such as fistula or abscess is clinically suspected, which of the following investigations would you perform to confirm this? (You may tick more than one investigation per age group if multiple concurrent investigations are normally performed.)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through | ||||
| Barium enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| MRI enteroclysis | ||||
| CT (oral contrast) | ||||
| CT enteroclysis | ||||
| Capsule endoscopy |
5. In an out-patient with known Crohn’s disease and obstructive symptoms suggesting stricturing disease, which of the following tests would you normally perform to determine the level of obstruction? (You may tick more than one investigation if multiple concurrent investigations are normally performed)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through | ||||
| Barium enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| MRI enteroclysis | ||||
| CT (oral contrast) | ||||
| CT enteroclysis | ||||
| Capsule endoscopy |
6. In a patient with known Crohn’s disease with a clinical flare-up, which test would you normally perform to reassess the small bowel disease? (You may tick more than one investigation if multiple concurrent investigations are normally performed)
| Investigation | Patient <20 years old | Patient 21–40 years old | Patient 41–60 years old | Patient >61 years old |
| Barium follow-through | ||||
| Barium enteroclysis | ||||
| Small bowel ultrasound | ||||
| Small bowel MRI (oral contrast) | ||||
| MRI enteroclysis | ||||
| CT (oral contrast) | ||||
| CT enteroclysis | ||||
| Capsule endoscopy |
References
- 1.Sands BE. Inflammatory bowel disease: past, present and future. J Gasteroenterol 2007;42:16–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maglinte DD, Sandrasegaran K, Tann M. Advances in alimentary tract imaging. World J Gastroenterol 2006;12:3139–45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Desmond AN, O’Regan K, Curran C, McWilliams S, Fitzgerald T, Maher MM, et al. Crohn’s disease: factors associated with exposure to high levels of diagnostic radiation. Gut 2008;57:1524–9 [DOI] [PubMed] [Google Scholar]
- 4.Gaca AM, Jaffe TA, Delaney S. Yoshizumi T, Toncheva G, Nguyen G, et al. Radiation doses from small bowel follow-through and abdomen/pelvis MDCT in pediatric Crohn’s disease. Pediatr Radiol 2008;38:285–91 [DOI] [PubMed] [Google Scholar]
- 5.Stange EF, Travis SPL, Vermeire S, Beglinger C, Kupcinskas L, Geboes K, et al. European evidence based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. Gut 2006;55:i1–i15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bernstien CN, Greenberg H, Boult I, Chubey S, Leblanc C, Ryner L. A prospective comparison study of MRI versus small bowel follow-through in recurrent Crohn’s disease. Am J Gastroenterol 2005;100:2493–502 [DOI] [PubMed] [Google Scholar]
- 7.Martin DR, Lauenstien T, Sitaraman SV. Utility of magnetic resonance imaging in small bowel Crohn’s disease. Gastroenterology 2007;133:385–90 [DOI] [PubMed] [Google Scholar]
- 8.Sheridan MB, Nicholson DA, Martin DF. Transabdominal ultrasonography as the primary investigation in patients with suspected Crohn’s disease or recurrence: a prospective study. Clin Radiol 1993;48:402–4 [DOI] [PubMed] [Google Scholar]
- 9.Masselli G, Casciani E, Polettini E, Lanciotti S, Bertini L, Gauldi G. Assessment of Crohn’s disease in small bowel: prospective comparison of magnetic resonance small bowel radiography and with conventional small bowel radiography. Eur Radiol 2006;16:2817–27 [DOI] [PubMed] [Google Scholar]
- 10.Halligan S, Marshall M, Taylor S, Bartram C, Bassett P, Cardwell C, et al. Observer variation in the detection of colorectal neoplasia on double-contrast barium enema: implications for colorectal cancer screening and training. Clin Radiol 2003;58:948–54 [DOI] [PubMed] [Google Scholar]
- 11.Horsthuuis K, Bipat S, Bennink RJ, Stoker J. Inflammatory bowel disease diagnosed with US, MR, scintigraphy and CT: meta-analysis of prospective studies. Radiology 2008;247:64–79 [DOI] [PubMed] [Google Scholar]
- 12.Sheridan MB, Nicholson DA, Martin DF. Transabdominal ultrasonography as the primary investigation in patients with suspected Crohn’s disease or recurrence: a prospective study. Clin Radiol 1993;48:402–4 [DOI] [PubMed] [Google Scholar]
- 13.Pallotta N, Tomei E, Viscido A, Calabrese E, Marcheggiano A, Caprilli R, et al. Small intestine contrast ultrasonography: an alternative to radiology in the assessment of small bowel disease. Inflamm Bowel Dis 2005;11:146–53 [DOI] [PubMed] [Google Scholar]
- 14.Hollerbach S, Geissler A, Schiegl H, Kullmann F, Lock G, Schmidt J, et al. The accuracy of abdominal ultrasound in the assessment of bowel disorders. Scand J Gastroenterol 1998;33:1201–8 [DOI] [PubMed] [Google Scholar]
- 15.Parente F, Greco S, Molteni M, Cucino C, Maconi G, Sampietro GM, et al. Role of early ultrasound in detecting inflammatory disorders and identifying their anatomical location within the bowel. Aliment Pharmacol Ther 2003;18:1009–16 [DOI] [PubMed] [Google Scholar]
- 16.Bozkurt T, Richter R, Lux G. Ultrasonography as primary diagnostic tool in patients with inflammatory bowel disease and tumour of small intestine and large bowel. J Clin Ultrasound 1994;22:85–91 [DOI] [PubMed] [Google Scholar]
- 17.Tarjan Z, Toth G, Gyorke T, Mester A, Karlinger K, Mako EK. Ultrasound in Crohn’s disease of the small bowel. Eur J Radiol 2000;35:176–82 [DOI] [PubMed] [Google Scholar]
- 18.Bremmer AR, Pridgeon J, Fairhurst J, Beattie RM. Ultrasound scanning may reduce the need for barium radiology in assessment of small bowel Crohn’s disease. Acta Paediatr 2004;93:479–81 [DOI] [PubMed] [Google Scholar]
- 19.Esteban JM, Maldonado L, Sanchiz V, Minguez M, Benages A. Activity of Crohn’s disease assessed by colour Doppler ultrasound analysis of affected loops. Eur Radiol 2001;11:1423–8 [DOI] [PubMed] [Google Scholar]
- 20.Jamieson DH, Shipman PJ, Israel DM, Jacobson K. Comparison of multidetector CT and barium studies of small bowel: inflammatory bowel disease in children. AJR Am J Roentgenol 2003;180:1211–16 [DOI] [PubMed] [Google Scholar]
- 21.Hara A, Leighton JA, Heigh RI, Sharma VK, Silva AC, De Petris G, et al. CD of small bowel: preliminary comparison among CT enterography, capsule endoscopy, small bowel follow-through and ileoscopy. Radiology 2006;238:128–34 [DOI] [PubMed] [Google Scholar]
- 22.Choi D, Jin Lee S, Ah Cho Y, Lim HK, Hoon Kim S, Jae Lee W, et al. Bowel wall thickening in patients with Crohn’s disease: CT pattern and correlation with inflammatory activity. Clin Radiol 2003;58:68–74 [DOI] [PubMed] [Google Scholar]
- 23.Amitai MM, Arazi-Kleinman T, Hertz M, Apter S, Portnoy O, Guranda L, et al. Multislice CT compared to small bowel follow-through in the evaluation of patients with Crohn’s disease. Clin Imaging 2008;32:355–61 [DOI] [PubMed] [Google Scholar]