Abstract
Drug-induced lung diseases are a frequent cause of morbidity. Diffuse pulmonary haemorrhage is an uncommon complication of drug therapy, and is a potentially life-threatening situation. We report the high-resolution CT and clinical findings of a 32-year-old man with diffuse pulmonary haemorrhage induced by ketorolac tromethamine.
Drug-induced lung disease is common. The frequency of diagnosed cases is increasing [1]. Diagnostic criteria include a history of drug exposure, consistent radiological findings, histological evidence of lung damage and exclusion of other common causes of pulmonary involvement such as infection, radiation pneumonitis, pulmonary thromboembolism, collagen vascular disease or progression of any other lung disease [2, 3]. In clinical practice, however, biopsy is seldom performed and the diagnosis is based primarily on clinical and radiological findings [2, 3].
Diffuse pulmonary haemorrhage (DPH) is an uncommon complication of drug therapy, but one that potentially carries significant morbidity and mortality [4]. Ketorolac tromethamine (KT) is a non-steroidal anti-inflammatory drug, known as an effective and popular long-acting analgesic medication. KT is indicated for the short-term management of moderately severe, acute pain that requires analgesia at the opioid level, usually in a post-operative setting [5]. We report the clinical findings and the high-resolution CT (HRCT) abnormalities in a patient with diffuse pulmonary haemorrhage induced by a normal dose of KT. To our knowledge, this is the first report of pulmonary haemorrhage associated with this drug.
Case report
A 32-year-old previously healthy man who had undergone vasectomy took 10 mg of sublingual KT (4 tablets in 24 h) for pain relief. Clinical symptoms started after the ingestion of the fourth tablet of KT, when he started to experience chest discomfort, dyspnoea, cough and fever (38°C). The following day the patient was admitted to the hospital after an episode of haemoptysis of approximately 20 ml of fresh blood. He denied the use of other drugs, trauma or previous episodes of haemoptysis. On admission, the patient was feeling unwell, although his physical examination was unremarkable, except for the presence of dyspnoea and bilateral crackles on chest auscultation. Oxygen saturation measured by pulse oximetry was 93%.
The results of laboratory tests performed on admission were recorded as follows: normal full blood count, with a platelet count of 180 000 mm−3, a prothrombin time of 13 s and an international normalised ratio (INR) of 1.1. Erythrocyte sedimentation rate was 10 mm in the first hour, C-reactive protein level was 4 mg dl–1, and the creatinine level was 1.0 mg dl–1. Antiphospholipid antibodies, c-ANCA, p-ANCA, antibasement membrane antibody, antinuclear factor and rheumatoid factor were all negative. Serum complement (C3, C4, CH50) levels were normal, and serology was negative for fungi and antihuman immunodeficiency virus in two tests. Urinalysis was normal.
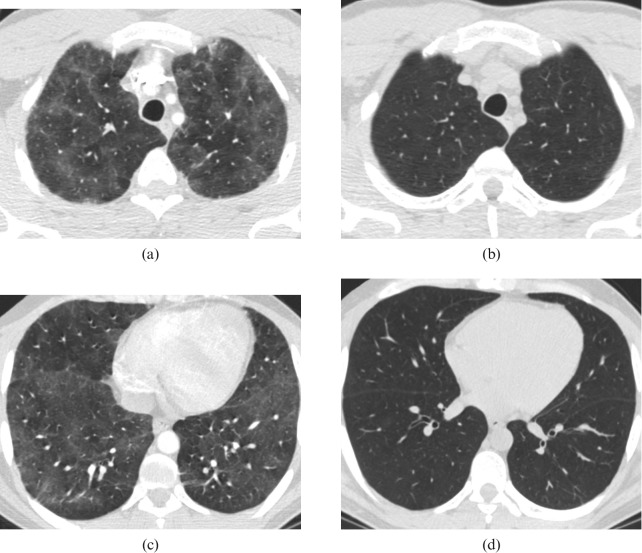
Chest radiography showed mild bilateral interstitial changes. HRCT revealed a diffuse bilateral ground-glass attenuation pattern (Figure 1a,c). Echocardiography, gastrointestinal endoscopy and nasolaryngoscopy revealed no abnormality. Fibre-optic bronchoscopy was performed 2 days after admission and revealed fresh blood in the airways, emerging from various pulmonary segments. There was no visible mass or mucosal damage. Bronchoalveolar lavage confirmed the presence of blood cells, and staining was negative for bacteria (including acid-fast bacilli) or fungi. Cultures were also negative. The diffusing capacity of the lung for carbon monoxide (DLCO) was 12.2 ml min–1mmHg–1 (144% of predicted).
Figure 1.
(a, c) Chest CT scan reveals bilateral diffuse and patchy ground-glass attenuation pattern, without distortion of the lung interstitium; (b, d) follow-up CT scan performed 6 days later showing complete regression of the ground-glass pattern.
The symptoms and signs were resolved without any specific treatment, except for the discontinuation of the drug. The patient was discharged five days after admission, after a follow-up CT scan had revealed complete regression of the ground-glass attenuation pattern (Figure 1b,d).
The diagnosis of pulmonary haemorrhage related to KT was based on the clinical, radiological and functional tests. The patient remained asymptomatic four months after being discharged from the hospital.
Discussion
KT is a popular long-acting non-steroidal anti-inflammatory drug frequently used in medical practice. Its potency is comparable to that of opiates; however, it has no respiratory depression effects [5]. Its relative safety has prompted a neglected complacency in many centres towards its infrequent but potentially life-threatening side-effects. KT is known as a potential cause of bleeding and is contraindicated in patients with haemorrhagic diathesis, incomplete haemostasis, previous gastrointestinal bleeding, suspected or confirmed cerebrovascular bleeding, or as pre-operative or prophylactic intraoperative treatment for pain relief. The drug can also trigger severe bronchospasm or anaphylactic reaction [6]. Non-steroidal anti-inflammatory treatment can cause nasal epistaxis [7] but, to our knowledge, there are no previous published reports on spontaneous pulmonary haemorrhage as a consequence of KT use.
Diffuse pulmonary haemorrhage is an uncommon complication of drug therapy, with potentially significant morbidity and mortality. Anticoagulants, amphotericin B, cyclophosphamide, mitomycin, cytarabine (ara-C) and penicillamine are examples of drugs that can cause DPH [2]. Clinical presentation typically includes haemoptysis, dyspnoea, anaemia and bilateral air–space consolidation with apical sparing on chest radiographs. However, each of these features is non-specific and all of them, including haemoptysis, may be absent. Chest radiograph is usually not helpful to establish the differential diagnosis [8–11]. In general, HRCT shows patchy or diffuse ground-glass opacities, consolidations, ill-defined centrilobular nodules, or a superimposition of these findings [12]. Although these findings are non-specific [13], HRCT is indicated to rule out neoplasm, cavitation or vascular abnormality [14, 15].
The diagnosis of drug reaction is primarily established by clinical and radiological findings [3]. As the signs and symptoms of our patient have resolved completely after stopping the drug and without any other intervention, no biopsy was taken. The diagnosis was done by exclusion after bronchoscopic confirmation of fresh haemoptysis. Upper gastrointestinal endoscopy and examination of the nose, pharynx and larynx were normal. No haematological dyscrasia was detected. The patient was not taking any other drugs that could cause pulmonary haemorrhage. All other possible causes of pulmonary haemorrhage have been excluded based on clinical and laboratory tests. Lung diffusion capacity was supranormal, as expected.
In conclusion, we report the first case of acute DPH caused by KT, which resolved completely after suspending the drug. Pulmonary haemorrhage should be included in the potential complications of KT.
References
- 1.Travis WD, Colby TV, Koss MN, Rosado-de-Christensen ML, Müller NL, King TE. Non-neoplastic disorders of the lower respiratory tract. Atlas of nontumor pathology. Washington, DC: Armed Forces Institute of Pathology, 2002 [Google Scholar]
- 2.Myers JL, Limper AH, Swensen SJ. Drug-induced lung disease: a pragmatic classification incorporating HRCT appearances. Semin Respir Crit Care Med 2003;24:445–53 [DOI] [PubMed] [Google Scholar]
- 3.Silva CI, Müller NL. Drug-induced lung diseases: most common reaction patterns and corresponding high-resolution CT manifestations. Semin Ultrasound CT MR 2006;27:111–16 [DOI] [PubMed] [Google Scholar]
- 4.Rossi SE, Erasmus JJ, McAdams HP, Sporn TA, Goodman PC. Pulmonary drug toxicity: radiologic and pathologic manifestations. Radiographics 2000;20:1245–59 [DOI] [PubMed] [Google Scholar]
- 5.Ketorolac Tromethamine [official FDA information website] October, 2008 [cited 2009, Feb 26]. Available from: http://www.drugs.com/pro/ketorolac-tromethamine.html. [Google Scholar]
- 6.Dias MA, Biedlingmaier JF. Ketorolac-induced status asthmaticus after endoscopic sinus surgery in a patient with Samter's triad. Otolaryngol Head Neck Surg 1997;117:S176–8 [DOI] [PubMed] [Google Scholar]
- 7.Watson MG, Shenoi PM. Drug-induced epistaxis? J R Soc Med 1990;83:162–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Leatherman JW, Davies SF, Hoidal JR. Alveolar hemorrhage syndromes: diffuse microvascular lung hemorrhage in immune and idiopathic disorders. Medicine 1984;63:343–61 [PubMed] [Google Scholar]
- 9.Bowley NB, Steiner RE, Chin WS. The chest X-ray in antiglomerular basement membrane antibody disease (Goodpasture's syndrome). Clin Radiol 1979;30:419–29 [DOI] [PubMed] [Google Scholar]
- 10.Primack SL, Miller RR, Muller NL. Diffuse pulmonary hemorrhage: clinical, pathologic, and imaging features. AJR Am J Roentgenol 1995;164:295–300 [DOI] [PubMed] [Google Scholar]
- 11.Armstrong P, Wilson AG, Dee P, Hansell DM. Imaging of Diseases of the Chest, 3rd edn. London, UK: Mosby, 2000 [Google Scholar]
- 12.Webb WR, Muller NL, Naidich DP, editors High-resolution CT of the Lung, 3rd edn. Philadelphia, PA: Lippincott Williams & Wilkins, 2002 [Google Scholar]
- 13.Cheah FK, Sheppard MN, Hansell DM. Computed tomography of diffuse pulmonary hemorrhage with pathological correlation. Clin Radiol 1993;48:89–93 [DOI] [PubMed] [Google Scholar]
- 14.Set PA, Flower CD, Smith IE, Chan AP, Twentyman OP, Shneerson JM. Hemoptysis: comparative study of the role of CT and fiberoptic bronchoscopy. Radiology 1993;189:677–80 [DOI] [PubMed] [Google Scholar]
- 15.Naidich DP, Funt S, Ettenger NA, Arranda C. Hemoptysis: CT–bronchoscopic correlations in 58 cases. Radiology 1990;177:357–62 [DOI] [PubMed] [Google Scholar]