Abstract
Polysplenia, as part of the heterotaxy syndrome, is a rare embryological disorder which results from failure of development of the usual left–right asymmetry of organs. It is often associated with cardiac and biliary abnormalities, which are the usual causes of death in early neonatal life. A congenitally short pancreas and abnormalities with portal vein formation, gut malrotations and inferior vena cava anomalies are known to be associated with this rare syndrome. We report a case of polysplenia in an adult female presenting with obstructive jaundice owing to choledocholithiasis, possibly formed by biliary stasis as a result of compression of the common bile duct by the preduodenal portal vein, and review the literature. The patient was also found to have complete agenesis of the dorsal pancreas on CT and endoscopic retrograde cholangiopancreatography.
Case report
A 62-year-old woman with a medical history of breast cancer, hypertension and paroxysmal atrial fibrillation presented with nausea, vomiting and abdominal pain. Blood tests revealed an obstructive pattern with raised alkaline phosphatase and elevated conjugated bilirubin.
She underwent CT which revealed a midline liver and multiple splenunculi to the left of the midline (Figure 1). CT also demonstrated agenesis of the pancreatic tail and lateral part of the body (Figure 2). The inferior vena cava (IVC) was to the left of the midline and crossed to the right at the level of the diaphragmatic hiatus and joined the heart (Figures 3a,b and 4). This morphology was deemed consistent with polysplenia in heterotaxy syndrome.
Figure 1.

Axial post-contrast CT demonstrating a midline liver (ML), small multiple splenunculi (arrows) and a dilated common bile duct.
Figure 2.

Axial post-contrast CT at a lower level demonstrating absence of pancreatic body and tail, right–sided stomach and left–sided inferior vena cava (IVC). AO, aorta; PV, portal vein; *absence of pancreatic body.
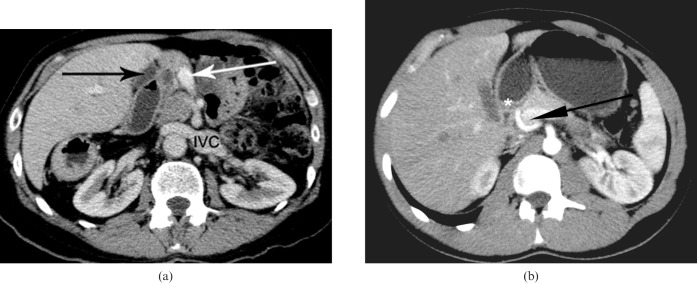
Figure 3.
(a) Axial post-contrast CT demonstrating preduodenal portal vein (white arrow), a dilated common bile duct proximal to the preduodenal portal vein (black arrow) and left-sided inferior vena cava (IVC). (b) Axial maximum intensity projections of a normal control volunteer showing the portal vein (black arrow) relationship to the first part of the duodenum (*). Note the portal vein traversing posterior to the first part of duodenum to enter the porta hepatis.
Figure 4.

Coronal reformatted CT demonstrating bilateral morphological left lungs. Note the bilateral hyparterial bronchi—both of the main bronchi (black arrows) are below the pulmonary arteries (PA).
It was also noted that the gallbladder was significantly dilated with sludge. There was evidence of a high attenuating, well-circumscribed rounded lesion, which was a suspected calculus in the suprapancreatic common bile duct (CBD). This caused mild dilation of the intrahepatic bile ducts.
MRI and magnetic resonance cholangiopancreatography (MRCP) were performed to further evaluate the cause of biliary obstruction. MRCP confirmed a calculus measuring 11×12 mm in the suprapancreatic CBD. It also showed complete absence of the dorsal pancreatic duct (Figure 5). Both MRI and CT demonstrated a preduodenal portal vein which was seen to be causing compression of the suprapancreatic segment of the CBD with a calculus proximal to compression (Figures 6 and 7).
Figure 5.
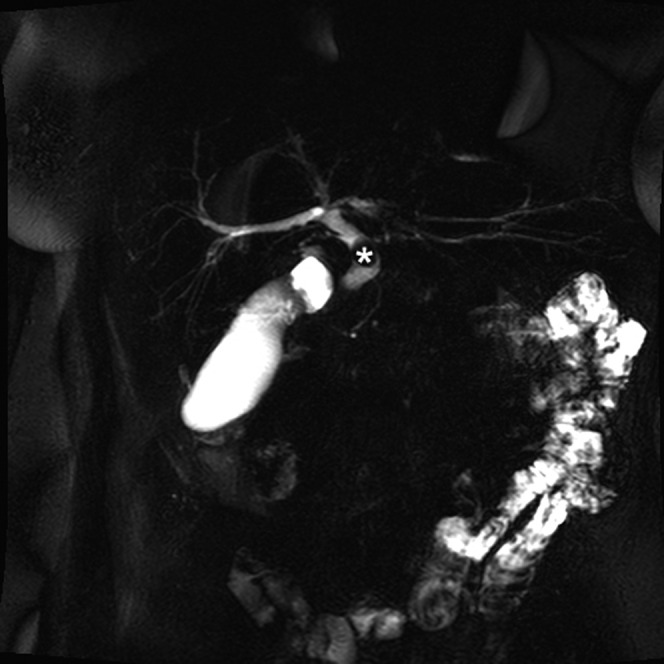
Three-dimensional magnetic resonance cholangiopancreatography reconstruction study demonstrating a calculus (*) in the proximal common bile duct with absence of the dorsal pancreatic duct.
Figure 6.
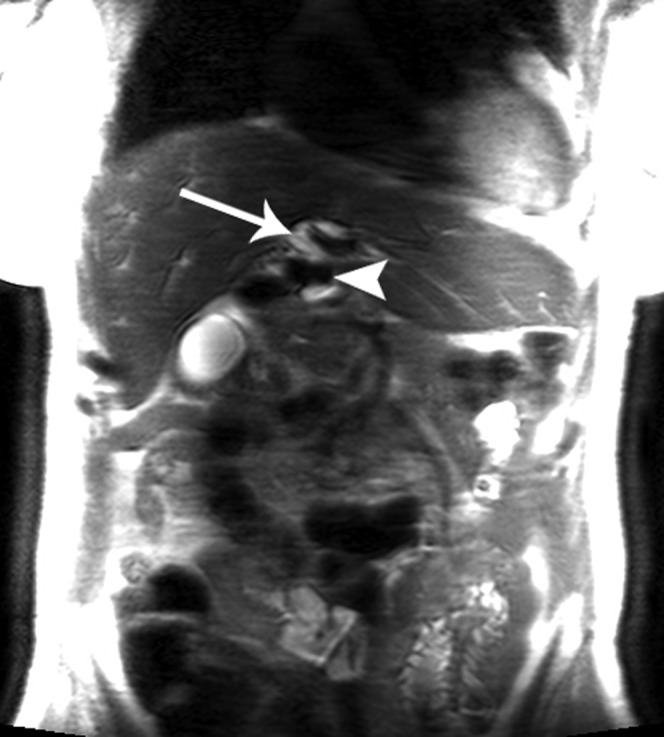
T2 fat saturated axial MR study demonstrating compression of the common bile duct (CBD) (white arrow) by the preduodenal portal vein (arrow head). Note the calculus is posterior to the CBD and cannot be visualised.
Figure 7.
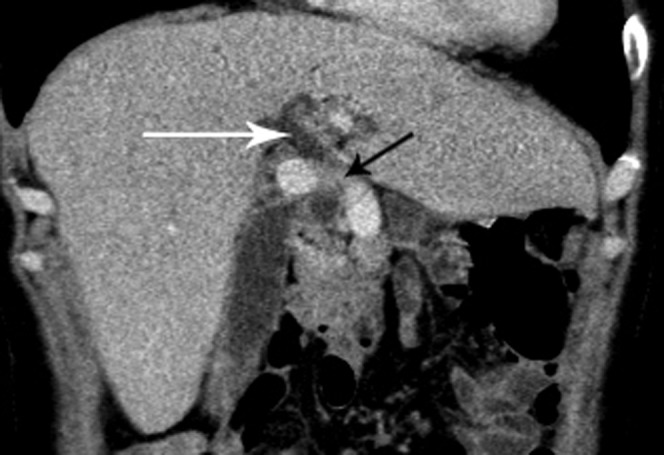
Coronal reformatted CT demonstrating preduodenal portal vein (black arrow) causing compression of the suprapancreatic common bile duct (white arrow).
The patient underwent laparoscopic cholecystectomy and choledocholithotomy.
Discussion
Polysplenia is a rare heterotaxy disorder with a reported incidence of 1 per 250 000 live births. Various studies have attempted to classify the broad spectrum of anomalies into asplenia and polysplenia [1]. Classical polysplenia results in hyparterial bronchi (both main bronchi are below the pulmonary arteries) and bilobed lungs. Asplenia results in trilobed lungs and eparterial bronchi (both main bronchi are located superior to the main pulmonary arteries).
The precise aetiology of polysplenia is unknown. Embryonic, genetic and teratogenic components have all been implicated as causative factors in polysplenia [2]. Although polysplenia syndrome has a wide range of abnormalities, there is no single pathognomic abnormality that characterises this rare entity. The range of anomalies include multiple spleens of equal volume, visceral heterotaxia, right-sided stomach, a left-sided or large midline liver, malrotation of the intestine, a short pancreas and IVC anomalies [3].
Polysplenia has been described mainly in childhood owing to critical anatomic malformations related to cardiac defects or biliary atresia. Only those with mild anatomical abnormalities survive into adulthood. Symptomatic polysplenia in adults is often caused by abnormal biliary and pancreatic duct drainage, cholecystisis and bowel obstruction [4]. Polysplenia is usually an incidental finding on abdominal ultrasound or CT performed for other causes.
In our patient there were multiple small spleens along the greater curvature of the stomach, a midline liver and bilateral hyparterial bronchi. We also noted dorsal pancreatic agenesis and a preduodenal portal vein.
Anomalies of the pancreas have been described in polysplenia syndrome [1]. Normal pancreas formation occurs from fusion of ventral and dorsal pancreatic buds. The ventral pancreatic bud gives rise to the uncinate process and the head, while the dorsal pancreatic bud gives rise to the body and tail. The development of both dorsal pancreatic bud and spleen occur in the dorsal mesogastrium. Consequently, anomalies in both these organs can be expected in patients with polysplenia syndrome [5].
Clinical significance of dorsal pancreatic agenesis is the development of pancreatitis owing to poor drainage from the remnant ventral duct. CT demonstration of a short pancreas is not synonymous with agenesis and is a pitfall well avoided. Fat replacement in the distal pancreas can mimic agenesis. Similarly partial vs complete dorsal duct agenesis can only be differentiated by pancreatic duct studies using either MRCP or endoscopic retrograde cholangiopancreatography.
Presence of preduodenal portal vein was seen in 12 out of 15 patients in 1 large review [6]. First described by Knight in 1921, the preduodenal portal vein is a congenital anomaly that involves the portal vein passing in front of the duodenum [6]. Preduodenal portal vein can be associated with duodenal atresia, stenosis, annular pancreas and malrotation. Surgery may be required for these conditions. A preduodenal portal vein anomaly occurs owing to loss of vitelline veins in their cranial and middle communication during 9 mm stage of embryonic development. In normal development, the loss of caudal and cranial communications result in the development of a normal ‘S’ shaped portal vein.
We postulate that formation of calculus was caused by stasis of bile in the CBD owing to distal compression of the CBD by the preduodenal portal vein. Similar opinion was also expressed by Seo et al [7]. When surgery is required care should be exercised in patients with preduodenal portal vein. Lack of awareness may lead to unwanted ramifications such as severe haemorrhage and other complications related to portal vein ligation.
Conclusion
The diagnosis of polysplenia in adults is usually made during investigation for unrelated causes. Biliary drainage abnormalities could result owing to the altered course of the portal vein in these syndromes. Increased awareness of such anatomical anomalies would prevent serious complications during abdominal surgery. Pancreatic duct anomalies have been described but are rare in polysplenia syndromes. We have reported one such unusual presentation of polysplenia syndrome presenting in older age with obstructive jaundice and both preduodenal portal vein and dorsal pancreatic agenesis.
References
- 1.Applegate KE, Goske MJ, Pierce G, Murphy D. Situs revisited: imaging of the heterotaxy syndrome. Radiographics 1999;19:837–52; discussion 853–4 [DOI] [PubMed] [Google Scholar]
- 2.De laMonte SM, Hutchins GM. Sisters with polysplenia. Am J Med Genet 1985;21:171–6 [DOI] [PubMed] [Google Scholar]
- 3.Gayer G, Apter S, Jonas T, Amitai M, Zissin R, Sella T, et al. Polysplenia syndrome detected in adulthood: report of eight cases and review of the literature. Abdom Imaging 1999;24:178–84 [DOI] [PubMed] [Google Scholar]
- 4.Kapa S, Gleeson FC, Vege SS. Dorsal panceas agenesis and polysplenia/heterotaxy syndrome: a novel association with aortic coarctation and a review of the literature. JOP 2007;8:433–7 [PubMed] [Google Scholar]
- 5.Maier M, Wiesner W, Mengiardi B. Annular pancreas and agenesis of the dorsal pancreas in a patient with polysplenia syndrome. AJR Am J Roentgenol 2007;188:W150–3 [DOI] [PubMed] [Google Scholar]
- 6.Knight HO. An anomalous portal vein with its surgical dangers. Ann Surg 1921;74:697–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seo HI, Jeon TY, Sim MS, Kim S. Polysplenia syndrome with preduodenal portal vein detected in adults. World J Gastroenterol 2008;14:6418–20 [DOI] [PMC free article] [PubMed] [Google Scholar]