Abstract
A 48-year-old woman presented with cough and chest pain. A chest radiograph and CT scans showed bilateral lung masses containing massive venous varices. A core biopsy specimen revealed benign metastasising leiomyoma with strong expression of progesterone receptors. A review of her medical history revealed a hysterectomy 11 years earlier. The lung masses showed significant reduction in size after induction of artificial menopause, although the pulmonary varices persisted.
A pulmonary varix is a localised enlargement of a segment of a pulmonary vein [1]. Lung varices have been associated with mitral valve disease, tuberculosis, emphysema, systemic hypertension and arteriovenous fistulae. Benign metastasising leiomyoma (BML) is a rare condition characterised by the presence of histologically benign smooth muscle tumours at extra-uterine sites in the presence of uterine leiomyomas [2–4]. Pelvic varices are a common finding in patients with uterine leiomyomas (fibroids); however, varices do not normally occur within the leiomyomas. We report CT findings observed in a 48-year-old woman who developed large varices inside BML lung masses. To our knowledge, this finding has not been previously described in the literature.
Case report
A 48-year-old woman was referred for CT evaluation of pulmonary abnormalities that had appeared on a chest radiograph. She initially presented with a cough and pleuritic chest pain on the right side. Her medical history included a hysterectomy for fibroids 11 years earlier. On examination, she was clearly unwell and had a fever. A chest radiograph showed bilateral volume loss with bilateral indistinct hemidiaphragm and a possible mass in the left lower zone (Figure 1). She was hypoxic in room air. Routine haematological tests were unremarkable except for a C-reactive protein level that increased from 31 to 244 mg L−1. An electrocardiogram was unremarkable and D-dimer and troponin T levels were normal.
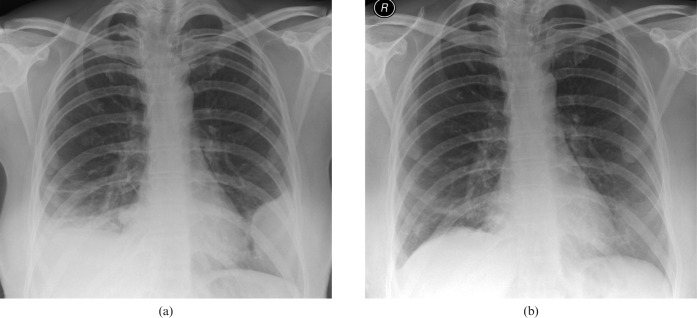
Figure 1.
(a) Chest radiograph from December 2006 demonstrating large lung masses in contact with the diaphragm and chest wall. (b) Chest radiograph from November 2007 demonstrating almost complete regression of lung masses after artificial menopause, induced by hormonal treatment, with subsequent bilateral oophorectomy.
A multislice CT scan of the chest with injection of intravenous contrast medium was performed. The resulting images demonstrated bilateral lung masses up to 9 cm in diameter with obvious venous varices. Vein diameters were as large as 1.2 cm in the lung cortex (Figure 2). Images of the lung varices were demonstrated by CT angiography three-dimensional reconstructions using maximum intensity projection (MIP) and volume-rendering techniques (Figure 3).
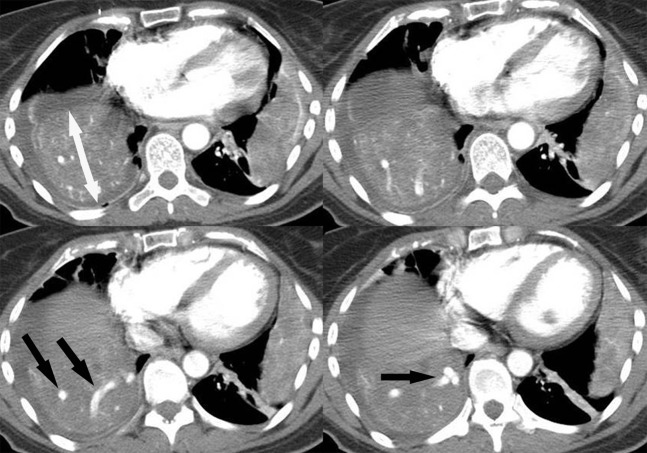
Figure 2.
CT scan from December 2006, before treatment, showing large bilateral lung masses and small right pleural effusion. Varicose veins (black arrows) are noted within the right lung mass (double-headed white arrow).
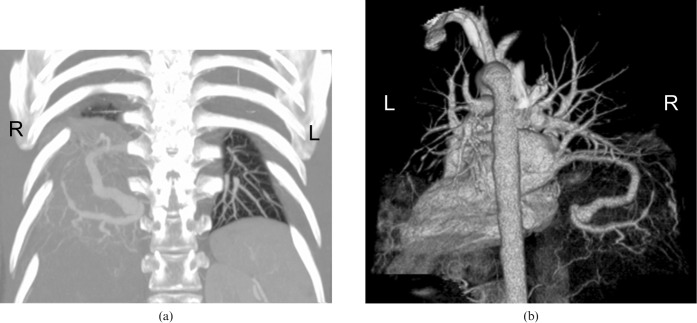
Figure 3.
(a) Thick coronal slab of a maximum intensity projection (MIP) image showing large varicose veins within the right lung mass. Please note that the visualisation of the mass is impaired as the MIP process highlights the structures with high attenuation values. (b) Posteroanterior volume rendering (VR) three-dimensional image, demonstrating the varicose inferior pulmonary vein draining into the left atrium. Please note that the masses are almost transparent as the threshold selected for the VR process was set to highlight the varices.
A CT-guided biopsy of the left lung lesion was performed, targeting the less vascularised area. Histological sections showed bland, predominantly fusiform, cells displaying no mitotic activity and arranged in a whorled pattern, typical of leiomyoma. These results were confirmed by immunolabelling for smooth muscle actin (SMA). Cell nuclei strongly expressed the receptor protein for progesterone, but not the oestrogen receptor, indicating that the cells might be responsive to hormonal manipulation. These features are diagnostic of BML. The patient was treated by inducing artificial menopause, which resulted in partial regression of the lung masses, although the varicose veins persisted. Follow-up scans revealed that some of the masses had suffered cystic degeneration with large fluid-filled cystic spaces (Figure 4). Residual masses were subsequently removed by surgery, which confirmed the diagnosis and findings.
Figure 4.
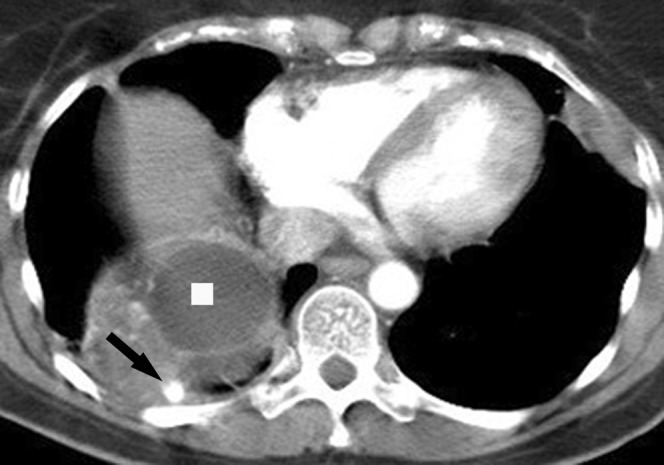
Follow-up CT scan from February 2008 demonstrating almost complete resolution of the left lung mass and significant regression in the right lower lobe mass, which still presents with varicosities (arrow) and cystic degeneration (square).
Discussion
Pulmonary varices are a rare venous abnormality, usually discovered as an incidental finding [1, 5, 6]. The most frequently reported cardiac lesion associated with pulmonary varices is mitral valve disease, which includes mitral stenosis and mitral regurgitation [7]. Some reports have suggested a congenital predisposition to pulmonary varices, with acquired conditions like pulmonary venous hypertension causing dilatation of pre-existing abnormal vessels that dilate further to become varices [1, 6, 7]. Most patients do not have symptoms that are directly related to the pulmonary varices [6, 7]. Therefore, surgical intervention is not generally recommended [1, 6], even though the varices may cause massive haemoptysis with bleeding into a bronchus or can be the source of emboli to the circulation owing to thrombosis within the varices [5, 7]. Lung varices within lung masses have not been previously reported. We propose that, in this case, the mechanism for the development of the varicose veins was related to angiogenic factors rather than an increase in venous pressure, because there were no signs of distal obstruction or arteriovenous fistula.
BML is a rare manifestation of the benign and common condition of uterine leiomyomas [8]. This term is used to describe multiple benign leiomyomas that appear several months to many years after hysterectomy for fibroids [4, 9, 10]. Women who have undergone hysterectomy for leiomyomas are the most commonly affected and are usually asymptomatic at presentation [2, 11]. To our knowledge, no previous cases of BML in the lungs have demonstrated pulmonary varices. Although the origin of the initial tumour remains controversial [3], a review of the literature supports the model that the primary tumour is located in the uterus and that uterine leiomyomas can metastasise, with haematogenous spread characteristic of BML. Histology of the lesions shows bundles of well-differentiated, spindled, mature smooth muscle cells, similar to those found in uterine leiomyomas. There is no atypia, and mitoses are rare or absent [3, 8]. Lung deposits have the same histological appearances as leiomyomas found within the uterus [8].
Typical radiographic findings include well-circumscribed, solitary or multiple homogeneous pulmonary nodules or masses that are round or lobulated with precise margins. They range in size from a few millimetres to several centimetres in diameter and are scattered throughout the lungs [4, 11]. Typically, nodules are homogeneous and not calcified. Obvious enhancement after administration of iv contrast medium is not a commonly described feature [8, 9, 12]. The masses rarely cavitate [4, 8, 9]. Unusual appearances of metastasising leiomyomas include cyst formation [8], tiny calcifications [9], dissemination in a miliary pattern [2, 12], interstitial lung disease [4, 12], pneumothorax [8, 10] and pericardial effusion [12].
The presence of fluid-containing cystic spaces inside the masses, as seen in this case, has been observed in a few rare, previous cases [4, 8, 9]. Uterine leiomyomas may undergo necrosis if they outgrow their blood supply, for example because of pregnancy, or because of rapid involution that occurs during the sudden post-partum hormonal imbalance. Eventually, this may lead to liquefactive necrosis with subsequent degeneration into aerated lung cysts [8]. In conclusion, we present a case demonstrating that lung varices can be found within BML lung masses.
References
- 1.Sellarés J, Santos S, Ballester E, Barberà JA. Pulmonary varix inside a bulla. Arch Bronconeumol 2006;42:39–41 [DOI] [PubMed] [Google Scholar]
- 2.Ferrie R, Smallman JM. Benign metastasising leiomyoma: a rare cause of breathlessness following caesarean section. Int J Obstet Anesth 2001;10:142–5 [DOI] [PubMed] [Google Scholar]
- 3.Egberts JH, Schafmayer C, Bauerschlag DO, Jänig U, Tepel J. Benign abdominal and pulmonary metastasizing leiomyoma of the uterus. Arch Gynecol Obstet 2006;274:319–22 [DOI] [PubMed] [Google Scholar]
- 4.Shin MS, Fulmer JD, Ho KJ. Unusual computed tomographic manifestations of benign metastasizing leiomyomas as cavitary nodular lesions or interstitial lung disease. Clin Imaging 1996;20:45–9 [DOI] [PubMed] [Google Scholar]
- 5.Zhang X, Han HL, Shi ZL. Thoracic exploration for the diagnosis of multiple pulmonary vein varices: case report. Chin Med J (Engl) 2007;120:2053–5 [PubMed] [Google Scholar]
- 6.Shiraishi J, Tatsumi T, Kimata M, Kambayashi D, Mano A, Yamanaka S, et al. Echocardiographic diagnosis of pulmonary vein varix. Circ J 2003;67:796–8 [DOI] [PubMed] [Google Scholar]
- 7.Ferretti GR, Arbib F, Bertrand B, Coulomb M. Haemoptysis associated with pulmonary varices: demonstration using computed tomographic angiography. Eur Respir J 1998;12:989–92 [DOI] [PubMed] [Google Scholar]
- 8.Camenzuli A, Thwaite E, Huda B, Haqqani M, Warburton CJ, Curtis J. Cavitation in lung masses from benign metastasizing leiomyomatosis. Clin Radiol Extra 2004;59:83–5 [Google Scholar]
- 9.Osadchy A, Zehavi T, Zissin R. Pulmonary benign metastasising leiomyomas presenting as fluid-containing masses on CT in a patient with two unrelated malignancies. Br J Radiol 2005;78:639–41 [DOI] [PubMed] [Google Scholar]
- 10.Sapmaz F, Ergin M, Katrancioglu O, Gonlugur T, Gonlugur U, Elagoz S. Benign metastasizing leiomyoma. Lung 2008;186:271–3 [DOI] [PubMed] [Google Scholar]
- 11.Abramson S, Gilkeson RC, Goldstein JD, Woodard PK, Eisenberg R, Abramson N. Benign metastasizing leiomyoma: clinical, imaging, and pathologic correlation. AJR Am J Roentgenol 2001;176:1409–13 [DOI] [PubMed] [Google Scholar]
- 12.Maredia R, Snyder BJ, Harvey LA, Schwartz AM. Benign metastasizing leiomyoma in the lung. Radiographics 1998;18:779–82 [DOI] [PubMed] [Google Scholar]