Abstract
The aim of this study was to evaluate the role of multidetector CT (MDCT) arthrography in the diagnosis of intra-articular hip pathology. A retrospective review of 96 patients who had undergone CT hip arthrography was performed. Data regarding the presence of a labral tear, paralabral cyst, chondral loss, acetabular version, femoral morphology and fibrocystic change were collected. We detected 28 labral tears (24 anterior, 2 anterolateral, 1 lateral and 1 posterolateral). An abnormal labral-chondral transitional zone was seen in 9 patients and 4 patients had surface labral fraying. We identified three paralabral cysts. Acetabular cartilage loss was detected in 45 and femoral cartilage loss in 9 patients. An abnormal anterior femoral head and neck junction was present in 18 hips and fibrocystic change in 8. Acetabular retroversion was present in 11 hips. 63 sets of patient notes were reviewed, of which 49 were in-patients with abnormal MDCT arthrogram findings. Surgical correlation was available in 27 patients. There was a discrepancy between the findings of a labral tear in one patient (false negative, 90% sensitivity and 100% specificity) and the presence of acetabular cartilage loss (88% sensitivity and 100% specificity) and femoral cartilage loss (94% sensitivity and 100% specificity) in three patients. MDCT arthrography affords accurate detection of intra-articular hip pathology.
The investigation of suspected intra-articular hip pathology is challenging. Arthroscopy represents the gold standard but is invasive, necessitates a general anaesthetic and is best reserved for patients in whom concomitant therapeutic intervention is to be undertaken. Much of the radiology literature has focused on the use of MR arthrography of the hip to detect labral and cartilage pathology [1–5]. A number of groups have also studied the role of non-contrast MRI in the detection of labral tears associated with femoroacetabular impingement and acetabular dysplasia [6–9]. Both non-contrast MRI and MR arthrography have limitations in terms of spatial resolution, which can make the detection of subtle labral and cartilage pathology challenging [4].
Modern spiral multidetector CT (MDCT) technology allows submillimetre spatial resolution and has revitalised interest in the role of CT arthrography in the wrist, shoulder, knee, elbow and ankle [10–17]. There are few published data on the utility of this technique in the investigation of intra-articular hip pathology. Several studies have investigated the ability of MDCT arthrography to assess cartilage loss in the hip and have demonstrated that its accuracy is equal to, or can outperform, MR arthrography [18–20]. There are limited reports regarding the ability of MDCT arthrography to assess labral pathology [9]. The aim of this study was to evaluate the role of MDCT arthrography in the diagnosis of intra-articular hip pathology in a consecutive group of patients.
Methods and materials
A retrospective review of 96 consecutive patients (37 male, 59 female; age range 10–65 years, mean age 38 years) who had undergone CT arthrography of the hip over a 20-month period was performed. The predominant patient complaint was of hip or groin pain and all had been assessed by a specialist hip surgeon prior to referral for imaging. Any history of a pre-existing condition such as Perthe’s disease or hip dysplasia was recorded, as well as the nature of any previous hip or pelvic surgery. The predominant clinical articular diagnosis was a suspected labral tear with or without articular cartilage injury. Data regarding the presence and site of labral abnormality, paralabral cyst formation, presence and site of chondral loss, acetabular version, femoral head and neck morphology and the presence of fibrocystic change of the femoral head and neck junction were collected.
Pathology involving the labrum was subcategorised on the basis of the pattern of abnormality of the labrum. A labral tear was defined as contrast extension into the body of the labrum. A labral chondral transitional zone abnormality referred to contrast extension through the labral base at the attachment of the labrum to the acetabulum or acetabular rim. Finally, the presence of surface irregularity, fissuring or fraying of the labral margins was also commented upon. The location of the labral tear or labral chondral transitional zone abnormality was subdivided into thirds: anterior, lateral and posterior. If the lesion crossed these zones then it was termed anterolateral or posterolateral accordingly. Likewise, acetabular and femoral cartilage loss was defined using similar thirds; however, where cartilage loss was seen to involve multiple areas this was termed diffuse. Where typical appearances of a sublabral sulcus were identified (often posteriorly), this finding was considered a normal variant and data on this were not collected. Notes were available for review in 63 patients and a correlation between the clinical intervention (if any) and the CT arthrogram findings was performed. Institutional review board approval was not required for the retrospective analysis of cases performed in this study.
Procedure technique
Patient informed consent was obtained prior to arthography. Arthrograms were performed using an anterolateral approach, under fluoroscopic guidance. Dilute iodinated contrast (10–12 ml; Omnipaque GE Healthcare, Uppsala, Sweden) was injected into the hip joint (50:50 mix of 240-strength iodinated contrast and normal saline). The normal saline was replaced with 5–6 ml 0.5% bupivicaine if a diagnostic injection was required, and the patient was given a pain diary to assess response. The hip joint was briefly passively exercised before a block axial acquisition (Siemens four-channel MDCT, Siemens, Erlangen, Germany) at 0.6-mm intervals was obtained. The study was then reported by a single fellowship-trained musculoskeletal radiologist from a workstation using axial, axial oblique, coronal and sagittal reconstructions.
Results
Out of a total of 96 patients, 69 (71%) had abnormal findings. Table 1 demonstrates the range and site of pathology detected by MDCT arthrography. Pre-existing conditions included developmental dysplasia of the hip (14 patients), Perthe’s disease (3 patients), previous hip trauma (2 patients) and previous triple pelvic osteotomy (3 patients). Table 2 further subcategorises the findings of Table 1 by demonstrating the labral lesions and cartilage loss patterns seen in specific conditions. Patient notes were available for review for 63 (66%) patients, 49 (51%) of whom had abnormal MDCT arthrograms. Of these, 27 (55%) patients had operative intervention, with the remainder being treated conservatively. A total of 17 (63%) patients underwent hip arthroscopy and 10 (37%) had open surgery. Open surgical procedures included hip resurfacing (4), femoral de-rotational osteotomy (2), triple pelvic osteotomy (2) and surgical dislocation and debridement (2). In the patients who had undergone arthroscopy, there was one false-negative report of a labral tear and nine true positives (90% sensitivity and 100% specificity, 100% positive predictive value and 86% negative predictive value). Slight under-reporting of cartilage loss was seen in two patients and over-reporting of chondral loss in one. Table 3 details these discrepancies further. These findings give MDCT a sensitivity of 88% and specificity of 100% for acetabular cartilage loss detection and a sensitivity of 94% and specificity of 100% for femoral cartilage loss. There was good correlation between the remaining 11 arthroscopies and the arthrogram findings. Abnormal osseous protuberances were detected by MDCT in five patients and were successfully debrided in four cases; one lesion could not be reached during arthroscopy.
Table 1. The range and sites of pathology detected by MDCT arthrography.
| Pathology | Total patient number | Pathology location and patient number |
| Labral tears | 28 | Anterior 24 (86%) |
| Anterolateral 2 (7%) | ||
| Lateral 1 (3.5%) | ||
| Posterolateral 1 (3.5%) | ||
| Abnormal labral surface fissuring and fraying (no definite labral tear defined by intralabral extension of contrast) | 4 | Anterior 2 (50%) |
| Anterolateral 1 (25%) | ||
| Lateral 1 (25%) | ||
| Abnormal labral chondral transitional zone (no extension of tear into labral body) | 9 | Anterior 6 (67%) |
| Anterolateral 1 (11%) | ||
| Lateral 2 (22%) | ||
| Acetabular cartilage loss | 45 | Anterior 30 (67%) |
| Anterolateral 5 (11%) | ||
| Lateral 5 (11%) | ||
| Diffuse 5 (11%) | ||
| Femoral cartilage loss | 9 | Anterior 5 (56%) |
| Posterior 1 (11%) | ||
| Diffuse 3 (33%) | ||
| Paralabral cysts | 3 | Anterior 1 |
| Anterolateral 1 | ||
| Lateral 1 | ||
| Femoral head and neck junction osseous bump | 18 | |
| Fibrocystic change at femoral head and neck junction | 8 | |
| Acetabular retroversion | 11 | |
| Coxa vara | 1 | |
| Hypertrophy of the ligamentum teres | 1 |
MDCT, multidetector CT.
Table 2. The degree of labral and chondral pathology associated with specific conditions.
| Condition (patient number) | Labral tear | Labral chondral transitional zone | Acetabular cartilage loss | Femoral cartilage loss |
| DDH (14 patients) | 10 patients: 8 anterior; 1 anterolateral; 1 lateral | 1 anterior | 11 patients: 9 anterior; 1 lateral; 1 diffuse | 3 patients: 1 anterior; 1 lateral; 1 posterior |
| Perthe's disease (3 patients) | 2 tears anterior | 0 | 3 patients: 2 anterior; 1 diffuse | 1 diffuse |
| Acetabular retroversion (11 patients) | 5 patients: 4 anterior; 1 anterolateral | 1 anterior | 5 patients: 5 anterior | 0 |
| FAI (20 patients) | 8 patients: 7 anterior; 1 anterolateral | 6 patients: 5 anterior; 1 anterolateral | 15 patients: 11 anterior; 3 anterolateral; 1 anterior and posterior | 2 patients: 1 anterior; 1 central |
DDH, developmental dysplasia of the hip; FAI, femoro-acetabular impingement
Table 3. Patients in whom discrepancy existed between the surgical findings and the MDCT arthrogram.
| Surgical findings | MDCT arthrogram findings |
| Badly frayed anterolateral labrum | Normal labrum |
| No impingement | Fibrocystic changes at femoral head and neck junction |
| Torn anterior labrum | Torn anterior labrum |
| Anterior cam lesion | Fibrocystic change |
| Very early acetabular chondral delamination | Normal femoral and acetabular cartilage |
| Anterolateral labral tear | Anterolateral labral tear |
| Mild acetabular cartilage loss | Well-preserved femoral and acetabular cartilage |
| Cam lesion | Cam lesion |
| Normal labrum | Intact labrum |
| Patchy femoral and acetabular cartilage loss | Anterior acetabular cartilage loss |
MDCT, multidetector CT. Patients in whom discrepancy existed between the surgical (arthroscopic) and the MDCT arthrogram.
Discussion
With the development of MDCT technology, MDCT arthrography is becoming an increasingly useful modality in the detection of joint pathology. Multiple studies have demonstrated excellent diagnostic results when used in the wrist, shoulder, elbow and knee [10–17]. There is, however, little published literature regarding MDCT arthrography of the hip in the assessment of intra-articular hip pathology.
Detection of hip labral pathology has traditionally presented a diagnostic challenge. The majority of studies have focused on the use of MRI, using both non-contrast and direct arthrographic techniques. Using a high-resolution surface-coil technique, James and co-workers [6, 7] reported that non-contrast MRI has good ability to detect labral and chondral pathology in both femoroacetabular impingement and acetabular dysplasia. Multiple studies have also reported excellent results for the detection of labral pathology using direct MR arthrography [3, 21]. It has, however, been recognised that the lack of spatial resolution of MRI can make the detection of small labral tears difficult. In a study performed by Keeney et al [2], 102 patients with clinical symptoms indicative of a labral tear underwent MR arthrography and subsequent arthroscopy. MR arthrography was found to have a sensitivity of 71%, specificity of 44%, positive predictive value of 93%, negative predictive value of 13% and accuracy of 69% for the detection of labral pathology. The authors concluded that, although MR arthrography was an excellent positive predictor of labral pathology, it had limited sensitivity and a negative study could not exclude important pathology amenable to treatment. Further studies have assessed the usefulness of radial reformatted images to improve the sensitivity of labral tear detection. Chan et al [22] evaluated 16 patients with suspected labral tear by MR arthrography with radial reformatted images and used the arthroscopic findings as a reference; they demonstrated 100% sensitivity and 96% accuracy. However, more recent work by Yoon et al [23] found no difference in sensitivity in the detection of labral tears between radial reformats and standard MR arthrographic views.
CT arthrography of the hip is not a new technique, but the improved resolution of MDCT has made it a viable alternative to MRI. Nishii et al [9] recently investigated the ability of MDCT to assess disorders of the acetabulum and labrum in hip dysplasia in 41 patients using radial reformatted images. They compared imaging findings with those of arthroscopy in approximately 50% of patients. Excellent correlation was seen: the sensitivity, specificity and accuracy of CT arthrography for the detection of labral tears was found to be 97%, 87% and 92%, respectively. In the current study, we used similar criteria for the detection of labral tears with CT to those used in MR arthrography, namely extension of contrast into the labral substance or between the labrum and acetabulum as well as alteration of the normal smooth contour of the labrum [1, 3, 24]. We aimed to distinguish between a labral tear where contrast extension was seen into the labrum itself from lesions involving the acetabular rim/margin (i.e. the labral chondral transitional zone) and those that showed surface changes to the labrum. By doing this we were able to show differences in the patterns of labral tears when secondary to developmental dysplasia of the hip vs femoroacetabular impingement. In the latter condition, we have shown the injury frequently occurs at the labral–chondral transitional zone, as demonstrated previously [6]. We have demonstrated excellent correlation between the MDCT arthrogram findings and those of arthroscopy. The majority of labral tears (86%) were detected in the anterior labrum (Figure 1), nine tears were confined to the labral chondral transitional zone (Figure 2) and three paralabral cysts (Figure 3) were seen.
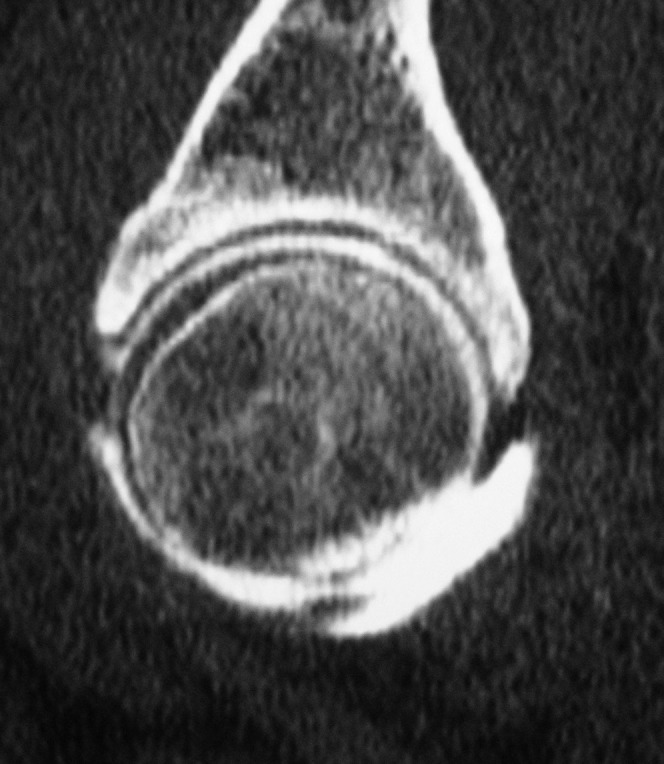
Figure 1.

Axial CT demonstrates contrast extension (arrow) into an elongated anterior labrum in a patient with developmental dysplasia of the hip.
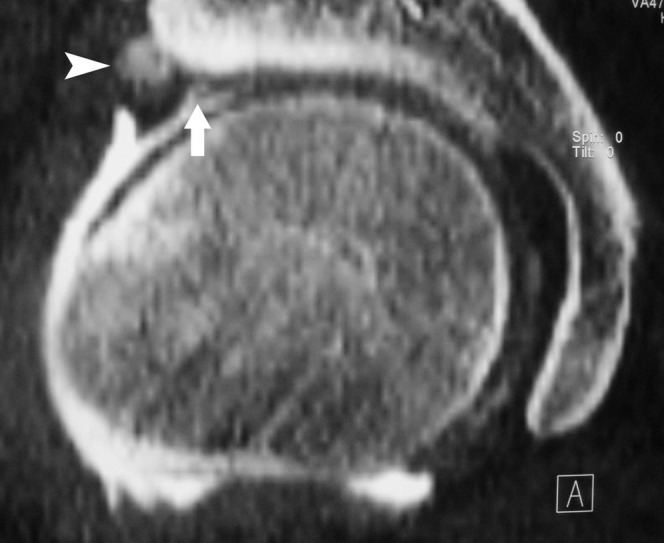
Figure 2.
Sagittal reconstruction showing contrast extension through the labral base at the labral chondral transitional zone. Note how clearly the femoral and acetabular cartilage thickness is defined as being normal in this case.
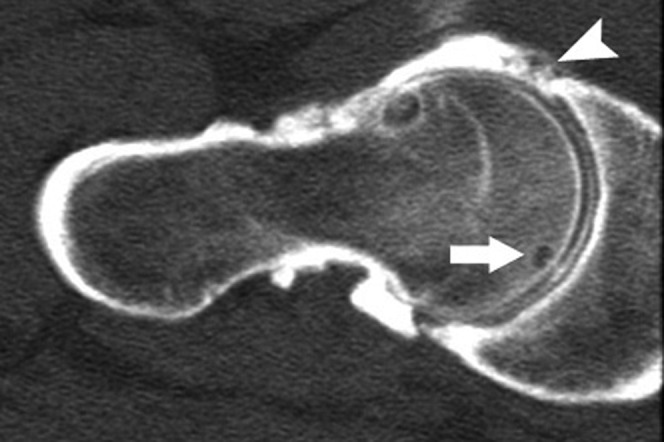
Figure 3.
Coronal reconstruction demonstrating a lateral paralabral cyst (arrowhead). There is also chondral loss with a discreet flap in the acetabular articular cartilage at the labral–chondral transitional zone (arrow).
Recent work suggests that MDCT arthrography has a sensitivity equal to, or better than, that of MR arthrography for the detection of cartilage loss in the hip [9, 18, 20]. It has been suggested that the curved articular surface and thin layer of hyaline articular cartilage found in the hip, compared with the knee, can make cartilage loss more difficult to detect with the somewhat limited spatial resolution of MRI. In addition, as the hip is situated deep in the body, loss of signal-to-noise ratio occurs, which is compounded by the lack of an effective surface coil [4]. MDCT allows for high-resolution multiplanar reformatted images to be obtained, which enable excellent assessment of both femoral (Figure 4) and acetabular cartilage (Figure 5) [9, 18, 19]. In our series we have demonstrated good correlation between the imaging and arthroscopic findings. Discrepancies were seen in only three hips: underestimation of acetabular cartilage loss was seen in one hip, underestimation of femoral cartilage loss in another and an overestimation of acetabular cartilage loss was made in the last hip.
Figure 4.

Axial CT illustrates marked chondral loss in the posterior femoral head and adjacent acetabulum (arrow).
Figure 5.

Sagittal reconstruction showing acetabular cartilage loss anteriorly (arrow) and a focal area of fibrocystic change in the anterior femoral head and neck junction (arrowhead). The anterior labrum demonstrates surface fraying and irregularity.
Femoroacetabular impingement is now well recognised as an important cause of hip pain and early-onset osteoarthritis. Femoral head and neck and acetabular morphological abnormalities in femoroacetabular impingement are well depicted by MDCT. An abnormal femoral head–neck junction osseous bulge was seen in 18 (19%) patients (Figure 6) and fibrocystic change at the head–neck junction in 8 (8%) patients (Figures 7 and 8) in our series. Using MDCT arthrography we were also able to assess associated damage to the underlying labrum and cartilage, which is so often present in impingement. Furthermore, MDCT allowed assessment of the degree of acetabular version. The acetabulum is normally anteverted between 15 and 20 degrees. Acetabular version can be determined on anteroposterior radiographs of the pelvis with the pelvis in a neutral position. The anterior and posterior margins of the acetabulum should normally lie 1.5 cm apart and should meet at the superolateral margin of the acetabulum. If the acetabulum is retroverted, the lines will meet in the midportion of the acetabulum (“cross-over sign”) and lie closer than 1.5 cm together [25]. The difficulty with this method lies in obtaining a radiograph with the pelvis in a truly neutral position, as alterations in pelvic tilt can lead to over- or underestimation of anteversion [26]. The radiographic studies give only an estimate of the degree of acetabular version, whereas CT allows for a more accurate assessment to be made. In our study we determined acetabular version by the method described by Tonnis et al [27]. A line is drawn connecting the anterior and posterior rims of the acetabulum; a second line, perpendicular to a line between the posterior pelvic margins, is then drawn. The angle between the intersection of these lines is the angle of acetabular version. Acetabular retroversion was seen in 11 (11%) patients in our study (Figure 9). This retroversion is associated with decreased clearance between the femur and acetabular rim during hip flexion, leading to pinching of the anterior labrum and increased incidence of tears and rim damage to the anterosuperior acetabular margin [28]. Of these patients with acetabular retroversion, five (45%) had labral tears, the majority of which were in the anterior labrum (see Table 2), and one patient had abnormality within the anterior labral–chondral transitional zone. Acetabular cartilage loss was also present in five patients, all in an anterior location. Associated pathology included one patient with a history of Perthe’s disease and two with a history of developmental hip dysplasia. Os acetabuli were seen in two patients. It was difficult to determine if these were true accessory ossicles or old rim fractures secondary to the abnormal acetabular version. Only 2 of the 11 patients had retroversion in both hips.
Figure 6.

Coronal reconstruction shows abnormal osseous prominence at the femoral head and neck junction (arrowhead) in association with a lateral labral tear (arrow) in a patient with femoroacetabular impingement.
Figure 7.

Coronal reconstruction showing an area of fibrocystic change at the femoral head and neck junction (arrow) in association with a lateral labral tear (arrowhead).
Figure 8.
Axial oblique reconstruction in a patient with femoroacetabular impingement. An area of fibrocystic change is seen at the anterior femoral head and neck junction. There is a markedly irregular and torn anterior acetabular labrum (arrowhead). There is also a small subchondral cyst in the femoral head (arrow) and a tiny chondral cleft/fissure is seen superficial to this, extending from the surface of the articular cartilage to the subchondral bone.
Figure 9.
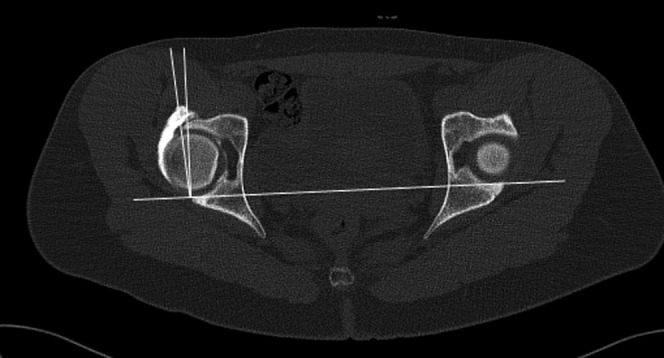
Axial CT image demonstrating acetabular retroversion. A line is drawn along the posterior margin of the acetabulum with a further line drawn perpendicular to this. A third line is then drawn between the anterior and posterior margins of the acetabulum, thus providing a measurement of the degree of acetabular version.
MDCT arthrography has further advantages beyond those of spatial resolution. Image acquisition is much faster than for MRI, reducing any potential problems regarding patient movement. Furthermore, patients tolerate the examination well and claustrophobia is much less of an issue. Finally, if there are contraindications to MRI, or if the patient has had previous surgery with metal work in situ, then MDCT arthrography confers further advantages.
There are several limitations to our study. Firstly, a single musculoskeletal radiologist reported the studies; thus, intra- and interobserver variability could not be assessed. Secondly, the limited number of patients with operative correlation makes it difficult to draw conclusions on the sensitivity and specificity of MDCT arthrography in the hip. It is likely that a formal prospective trial with operative comparison would allow the relative strengths and weaknesses of this technique to be further evaluated. In this study we have termed the presence of lucency at the femoral head and neck junction as fibrocystic change. This definition is made on the basis of its typical appearance, location and morphology; however, pathological examination of these areas was not undertaken.
By performing MDCT arthrography rather than MRI, there is loss of the exquisite soft-tissue contrast that MRI affords. There is, therefore, the potential for unexpected findings within the soft tissues to be missed. To reduce this possibility, images were viewed on both soft tissue and bone algorithms; however, previous workers have demonstrated that when comparing CT and MRI in the detection of recurrent malignant disease, MRI is superior only for lesions less than 15 cm3 [29]. MR arthrography is usually performed with the use of a surface coil and a small field of view; thus, unexpected pelvic lesions might also be missed using this technique. Finally, CT imparts radiation on the pelvis, with the patient cohort included in this study being predominantly young patients. To minimise this radiation exposure, referral required assessment by a dedicated hip surgeon and abnormal findings were seen in 71% of cases.
We have demonstrated the wide range of abnormalities that can be identified by the use of MDCT hip arthrography. We believe that MDCT arthrography is a useful additional tool in the assessment of patients with suspected intra-articular hip pathology. This technology seems to have a similar sensitivity to MRI for the detection of labral pathology and superior ability to detect chondral loss. Finally, MDCT arthrography is likely to be of further use in patients for whom MRI is contraindicated or where previous surgery has been undertaken.
References
- 1.Petersilge CA, Haque MA, Petersilge WJ, Lewin JS, Lieberman JM, Buly R. Acetabular labral tears: evaluation with MR arthrography. Radiology 1996;200:231–5 [DOI] [PubMed] [Google Scholar]
- 2.Keeney JA, Peelle MW, Jackson J, Rubin D, Maloney WJ, Clohisy JC. Magnetic resonance arthrography versus arthroscopy in the evaluation of articular hip pathology. Clin Orthop Relat Res 2004;429:163–9 [DOI] [PubMed] [Google Scholar]
- 3.Toomayan GA, Holman WR, Major NM, Kozlowicz SM, Vail TP. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol 2006;186:449–53 [DOI] [PubMed] [Google Scholar]
- 4.Schmid MR, Notzli HP, Zanetti M, Wyss TF, Hodler J. Cartilage lesions in the hip: diagnostic effectiveness of MR arthrography. Radiology 2003;226:382–6 [DOI] [PubMed] [Google Scholar]
- 5.Neumann G, Mendicuti AD, Zou KH, Minas T, Coblyn J, Winalski CS, et al. Prevelance of labral tears and cartilage loss in patients with mechanical symptoms of the hip: evaluation using MR arthrography. Osteoarthritis Cartilage 2007;15:909–17 [DOI] [PubMed] [Google Scholar]
- 6.James SLJ, Ali K, Malara F, Young D, O'Donnell J, Connell DA. MRI findings of femoroacetabular impingement. AJR Am J Roentgenol 2006;187:1412–19 [DOI] [PubMed] [Google Scholar]
- 7.James SLJ, Miocevic M, Malara F, Pike J, Young D, Connell D. MR imaging findings of acetabular dysplasia in adults. Skeletal Radiol 2006;35:378–84 [DOI] [PubMed] [Google Scholar]
- 8.Mintz DN, Hooper T, Connell D, Buly R, Padgett DE, Potter HG. Magnetic resonance imaging of the hip: detection of labral and chondral abnormalities using non contrast imaging. Arthroscopy 2005;21:385–93 [DOI] [PubMed] [Google Scholar]
- 9.Nishii T, Tanaka H, Sugano N, Miki H, Takao M, Yoshikawa H. Disorders of the acetabular labrum and articular cartilage in hip dysplasia: evaluation using isotropic high-resolutional CT arthrography with sequential radial reformation. Osteoarthritis Cartilage 2007;15:251–7 [DOI] [PubMed] [Google Scholar]
- 10.Vande Berg BC, Lecouvet FE, Poilvache P, Jamart J, Materne R, Lengele B, et al. Assessment of knee cartilage in cadavers with dual-detector spiral CT arthrography and MR imaging. Radiology 2002;222:430–6 [DOI] [PubMed] [Google Scholar]
- 11.Berland LL, Smith JK. Mulitdetector-array CT: once again, technology creates new opportunities. Radiology 1998;209:327–9 [DOI] [PubMed] [Google Scholar]
- 12.Schmid MR, Schertler T, Pfirrmann CW, Saupe N, Manestar M, Wildermuth S, et al. Interosseous ligament tears of the wrist: comparison of multi-detector row CT arthrography and MR imaging. Radiology 2005;237:1008–13 [DOI] [PubMed] [Google Scholar]
- 13.Moser T, Dosch J, Moussaoui A, Dietemann J. Wrist ligament tears: evaluation of MRI and combined MDCT and MR arthrography. AJR Am J Roentgenol 2007;188:1278–86 [DOI] [PubMed] [Google Scholar]
- 14.Waldt S, Bruegel M, Ganter K, Kuhn V, Link TM, Rummeny EJ, et al. Comparison of multislice CT arthrography and MR arthrography for the detection of articular cartilage lesion of the elbow. Eur Radiol 2005;15:784–91 [DOI] [PubMed] [Google Scholar]
- 15.Omlor G, Jung M, Grieser T, Ludwig K. Depiction of the triangular fibro-cartilage in patients with ulnar sided wrist pain: comparison of direct multislice CT arthrography and direct MR arthrography. Eur Radiol 2009;19:147–51 [DOI] [PubMed] [Google Scholar]
- 16.De Filippo M, Bertellini A, Sverzellati N, Pogliacomi F, Costantino C, Vitale M, et al. Multidetector computed tomography arthrography of the shoulder: diagnostic accuracy and indications. Acta Radiol 2008;49:540–9 [DOI] [PubMed] [Google Scholar]
- 17.De Filippo M, Bertellini A, Pogliacomi F, Sverzellati N, Corradi D, Garlaschi G, et al. Multidetector computed tomography arthrography of the knee: diagnostic accuracy and indications. Eur J Radiol 2009;70:342–51 [DOI] [PubMed] [Google Scholar]
- 18.Wyler A, Bousson V, Bergot C, Polivka M, Leveque E, Vicaut E, et al. Comparison of MR arthrography and CT arthrography in hyaline cartilage thickness measurement in radiographically normal cadaver hips with anatomy as gold standard. Osteoarthritis Cartilage 2009;17:19–25 [DOI] [PubMed] [Google Scholar]
- 19.Wyler A, Bousson V, Bergot C, Polivka M, Leveque E, Vicaut E, et al. Hyaline cartilage thickness in radiographically normal cadaveric hips: comparison of spiral CT arthrographic and macroscopic measurements. Radiology 2007;242:441–9 [DOI] [PubMed] [Google Scholar]
- 20.Nishii T, Tanaka H, Nakanishi K, Sugano N, Miki H, Yoshikawa H. Fat-suppressed 3D spoiled gradient-echo MRI and MDCT arthrography of articular cartilage in patients with hip dysplasia. AJR Am J Roentgenol 2005;185:379–85 [DOI] [PubMed] [Google Scholar]
- 21.Czerny C, Hofmann S, Neuhold A, Tschauner C, Engel A, Recht MP, et al. Lesions of the acetabular labrum: accuracy of MR imaging and MR arthrography in detection and staging. Radiology 1996;200:225–30 [DOI] [PubMed] [Google Scholar]
- 22.Chan YS, Lien LC, Hsu HL, Wan YL, Lee MS, Hsu KY, et al. Evaluating hip labral tears using magnetic resonance arthrography: a prospective study comparing hip arthroscopy and magnetic resonance arthrography diagnosis. Arthroscopy 2005;21:1250. [DOI] [PubMed] [Google Scholar]
- 23.Yoon LS, Palmer WE, Kassarjian A. Evaluation of radial-sequence imaging in detecting acetabular labral tears at hip MR arthrography. Skeletal Radiol 2007;36:1029–33 [DOI] [PubMed] [Google Scholar]
- 24.Czerny C, Hofmann S, Urban M, Tschauner C, Neuhold A, Pretterklieber M, et al. MR arthrography of the adult acetabular capsular-labral complex: correlation with surgery and anatomy. AJR Am J Roentgenol 1999;173:345–9 [DOI] [PubMed] [Google Scholar]
- 25.Peele MW, Deela Rossa GJ, Maloney WJ, Curry MC, Clohisy JC. Acetabular and femoral radiographic abnormalities associated with labral tears. Clin Orthop Relat Res 2005;441:327–33 [DOI] [PubMed] [Google Scholar]
- 26.Anda S, Svenningsen S, Grontvedt T, Benum P. Pelvic inclination and spatial orientation of the acetabulum. A radiographic, computer tomographic and clinical investigation. Acta Radiol 1990;31:389–94 [PubMed] [Google Scholar]
- 27.Tonnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am 1999;81:1747–70 [DOI] [PubMed] [Google Scholar]
- 28.Lavigne M, Parvizi J, Beck M, Siebenrock KA, Ganz R, Leunig M. Anterior femoracetabular impingement, part 1: techniques of joint preserving surgery. Clin Orthop Relat Res 2004;418:61–6 [PubMed] [Google Scholar]
- 29.Reuther G, Mutschler W. Detection of local recurrent disease in musculoskeletal tumors: magnetic resonance imaging versus computed tomography. Skeletal Radiol 1990;19:85–90 [DOI] [PubMed] [Google Scholar]


