Abstract
Malignant peripheral nerve sheath tumours are rare and aggressive soft-tissue sarcomas of ectomesenchymal origin. These tumours commonly occur in patients with neurofibromatosis Type 1 with a cumulative lifetime risk of 10%. The vast majority of cases present with clinical evidence of a soft-tissue mass with or without features of nerve irritation and loss of function arising from the lesion of origin. The primary presentation of a malignant peripheral nerve sheath tumour with a pneumothorax in the absence of widespread metastatic disease in a patient with no medical or family history of neurofibromatosis has never been reported in the literature.
We present a unique case of a systemically well 34-year-old male who presented with clinical evidence of a right-sided pneumothorax. The chest radiograph identified the right-sided pneumothorax and revealed an apical pleural mass that was confirmed by intravenous contrast-enhanced CT of the thorax. The patient was referred for video-assisted thorascopic surgical pleurodesis and biopsy of the lesion. Histopathology analyses confirmed the diagnosis of malignant peripheral nerve sheath tumour.
To the best of our knowledge, no such case reports have been published in the literature. A diagnosis of malignant peripheral nerve sheath tumour should be considered as one of the rarer possibilities in patients presenting with pneumothoraces in association with apical pleural lesions.
Case resport
A 34-year-old male presented to our emergency department with acute dyspnoea associated with right-sided pleuritic chest pain. The symptoms had developed suddenly and occurred at rest. There was no history of recent trauma or illness. The patient was a smoker with a 15-pack year history, but had previously been fit and well with no significant medical or family history.
On examination, the patient appeared in mild respiratory distress with a respiratory rate of 26 breaths per minute and an oxygen saturation of 91% on room air. He was haemodynamically stable and afebrile. Examination of the respiratory system revealed reduced chest expansion, a hyper-resonant percussion note and reduced air entry over the apex of the right hemithorax. There was no evidence of mediastinal shift. Examination was otherwise unremarkable. Full blood count, biochemistry and electrocardiogram were all normal. A chest radiograph showed a large right-sided pneumothorax associated with a right apical lesion (Figure 1).
Figure 1.

Chest radiograph showing a large right-sided pneumothorax associated with a right apical lesion.
The right-sided pneumothorax was treated by insertion of a Seldinger intercostal drain and the patient was admitted to hospital. An intravenous contrast-enhanced CT scan of the thorax identified a persistent right-sided pneumothorax associated with a lobulated soft-tissue mass at the apex of the right lung and nodular thickening of the pleura in the right upper zone (Figure 2). The patient was transferred to the local tertiary cardiothoracic surgical unit where he underwent video-assisted thorascopic surgical biopsy of the pleural lesion.
Figure 2.
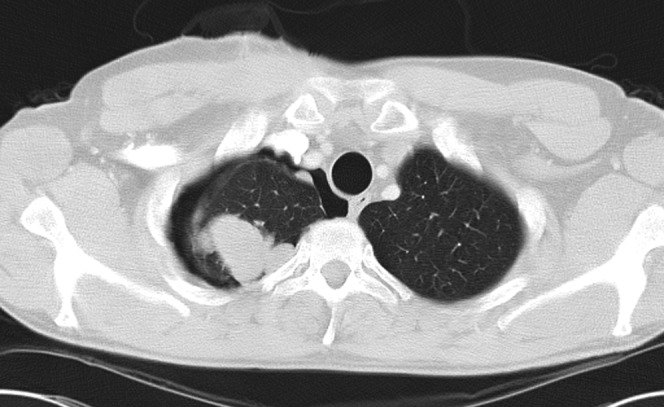
CT axial image showing a persistent right-sided pneumothorax associated with a lobulated soft-tissue mass at the apex of the right lung and nodular thickening of the pleura in the right upper zone.
Histological examination of the specimen revealed a tumour that contained malignant spindle cells arranged predominantly in wavy fascicles but with focal vague palisading (Figure 3). On immunohistochemical analysis the spindle cells showed patchy focal expression with glial fibrillary acidic protein (GFAP), which favours neural differentiation and membranous accentuation with CD56 (neural cell adhesion molecule). This combination of morphological and immunohistochemical features favoured a diagnosis of a high-grade malignant peripheral nerve sheath tumour.
Figure 3.

Biopsy shows the pleural mass to contain malignant spindle cells with characteristic features. In conjunction with immunohistochemistry these favour a diagnosis of malignant peripheral nerve sheath tumour.
The patient was transferred to a specialist tertiary oncology centre and was enrolled onto a Phase 2 therapeutic trial of the multikinase inhibitor, brivanib. Despite this the patient later developed widespread metastatic disease and died 12 months later.
Discussion
Malignant peripheral nerve sheath tumours are rare and aggressive soft-tissue sarcomas of ectomesenchymal origin [1]. These tumours are derived from Schwann or pleuripotent cells of neural crest origin and arise from peripheral nerve branches or sheaths of peripheral nerve fibres [1-3]. Malignant peripheral nerve sheath tumours have been referred to by a number of names including “neurogenic sarcoma”, “malignant schwannoma”, “malignant neurilemmoma” and “neurofibrosarcoma” [1,3].
It is estimated that malignant peripheral nerve sheath tumours represent 5% of all soft-tissue sarcomas with an incidence of 0.001% in the general population [2]. They usually occur in adult patients aged 20–50 years old [2]. The majority of malignant peripheral nerve sheath tumours occur in patients with neurofibromatosis Type 1 with a cumulative lifetime risk approaching 10% [1]. Malignant peripheral nerve sheath tumours have also been associated with previous radiation therapy [1-2].
As with other neural origin tumours, the majority of patients with malignant peripheral nerve sheath tumours present with clinical features of nerve irritation and loss of function arising from the lesion of origin [2,4]. In one series the most common presenting symptom was a mass (96%) followed by pain (71%) [4]. The most commonly affected sites include the sciatic nerve, brachial plexus, spinal nerve roots, lumbosacral plexus and the obturator and femoral nerves [2]. Rare sites of origin for malignant peripheral nerve sheath tumours include the pericardial sac, breast and paranasal sinuses [2,5,6]. There are only two previously reported cases in the English-language literature of benign peripheral nerve sheath tumours primarily presenting as a pneumothorax [7-8]. This is the first case of a malignant peripheral nerve sheath tumour primarily presenting with pneumothorax in the absence of widespread metastatic disease.
Patients with malignant peripheral nerve sheath tumours generally have a poor prognosis because metastatic spread at initial presentation is common [1]. Adverse prognostic factors include large size (>5 cm), high-grade tumour, advanced histological characteristics, tumour invasion of resection margins and neurofibromatosis Type 1 [1].
Conclusion
We present a unique case of a malignant peripheral nerve sheath tumour presenting as a pneumothorax in a patient with no clinical evidence of metastatic disease or history of neurofibromatosis Type 1. A diagnosis of malignant peripheral nerve sheath tumour should be considered a rare cause of pneumothorax when associated with apical pleural lesions.
References
- 1.Gupta G, Maniker A. Malignant peripheral nerve sheath tumours. Neurosurg focus 2007;22:e12. [DOI] [PubMed] [Google Scholar]
- 2.Dhingra KK, Mandal S, Roy S., Khurana N Malignant peripheral nerve sheath tumor of the breast: case report. World J Surg Oncol 2007;5:142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kim DH, Murovic JA, Tiel RL, Moes G, Kline DG. A series of 397 peripheral neural sheath tumors: 30-year experience at Louisiana State University Health Sciences Center. J Neurosurg 2005;102:246–55 [DOI] [PubMed] [Google Scholar]
- 4.Kar M, Deo SS, Shukla NK, Malik A, DattaGupta S, Mohanti BK, et al. Malignant peripheral nerve sheath tumors (MPNST) clinicopathological study and treatment outcome of twenty-four cases. World J Surg Oncol 2006;4:55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nkere UU, Walter NM. Malignant peripheral nerve sheath tumour: a rare tumour and an unusual intrapericardial presentation. European Journal of Cardio-thoracic Surgery 1997;12:144–6 [DOI] [PubMed] [Google Scholar]
- 6.Ahsan F, Lee MK, Ah-See KW, Chapman AD. Malignant peripheral nerve sheath tumor of the paranasal sinuses. Ear Nose Throat J 2004;83:699–701 [PubMed] [Google Scholar]
- 7.Engdahl R, Vivas D, Lajam F. Spontaneous pneumothorax as initial presentation of neurofibromatosis. Am Surg 2010;76:1034. [PubMed] [Google Scholar]
- 8.Torrington KG, Ashbaugh DG, Stackle EG. Recklinghausen's disease occurrence with intrathoracic vagal neurofibroma and contralateral spontaneous pneumothorax. Arch Intern Med 1983;143:568–9 [DOI] [PubMed] [Google Scholar]


