Abstract
Objective
The two currently acceptable treatment options for locally advanced laryngeal cancer are total laryngectomy and organ preservation using chemoradiation. To facilitate therapeutic decision making, the accurate pre-treatment evaluation of cartilage invasion is of paramount importance. The purpose of this study was to evaluate the positive predictive value (PPV) and negative predictive value (NPV) of detecting neoplastic cartilage invasion in laryngeal cancer patients using fast-speed multidetector CT (MDCT).
Methods
61 consecutive patients with clinically staged T3 or T4 squamous cell carcinoma of the larynx or hypopharynx who underwent total laryngectomy were analysed. All patients had MDCT of the neck within 2 weeks prior to surgery. Central radiographic and pathological review was performed in an attempt to correlate findings. MDCT invasion of cartilage was graded based on objective criteria.
Results
MDCT scan was found to have a PPV of 78% and an NPV of 100% for detection of invasion through cartilage, with sensitivity being 100% and specificity 96%. For detection of any cartilage invasion (minor, major or through cartilage invasion), PPV and NPV were 63% and 92%, respectively. The sensitivity was 85% and specificity was 75%. For the detection of tumour invasion through cartilage or major cartilage invasion, MDCT scan had a PPV of 53% and an NPV of 95%. 47% (9/19) patients were down-staged from T4 to T3 after central pathology review.
Conclusion
The low PPV for cartilage destruction using MDCT suggests that a significant proportion of patients who were treated by total laryngectomy could have been appropriately offered organ preservation if more accurately staged at initial diagnosis.
Cartilage invasion is one of the critical determinants of tumour staging for laryngeal cancer, the most common squamous cell carcinoma of the head and neck. According to the current American Joint Committee on Cancer (AJCC) staging guidelines, minor cartilage invasion is classified as T3, whereas invasion through cartilage is T4. These definitions are inherently problematic owing to the subjective nature of cartilage invasion. For instance, limited evidence in the 1990s suggested that CT has the tendency towards “over-calling” thyroid cartilage invasion, largely due to reactive inflammation [1, 2]. In recent years, there has been increasingly renewed interest in the accuracy of pre-treatment imaging evaluation of cartilage invasion, in view of the results from the Veterans Association (VA) Laryngeal Cancer Study and Radiation Therapy Oncology Group (RTOG) trial 91–11. These studies demonstrated the feasibility and effectiveness of organ preservation for locally advanced head and neck cancers involving the larynx [3, 4]. However, there is general agreement that for patients with T4 disease, total laryngectomy is preferred owing to the questionable efficacy of radiation therapy in the setting of cartilage invasion. As such, both the American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) expert panels have recommended laryngectomy for patients with thyroid cartilage destruction [5, 6]. Therefore, overstaging with pre-treatment CT study could potentially result in loss of the possible benefit of organ preservation in many patients.
However, these aforementioned studies published in the 1990s had limited clinical ramification because (1) they were performed before fast-speed multidetector CT (MDCT) was widely available as a standard staging modality, or (2) they did not differentiate minor cartilage invasion (T3) vs invasion through thyroid cartilage (T4). The purpose of this study was to therefore evaluate the positive predictive value (PPV) and negative predictive value (NPV) of detecting neoplastic cartilage invasion (T3 vs T4) in laryngeal cancer patients using MDCT, which has been widely accepted as the preferred pre-treatment imaging modality in most practice settings in the past 10 years.
Methods and materials
Patients and tumour characterisation
This was a retrospective study approved by the Institutional Review Board at the University of California Davis School of Medicine. Medical charts of all patients with clinical T3 or T4 squamous cell carcinoma of the larynx or hypopharynx who had been treated at one tertiary teaching hospital between 2003 and 2009 were identified and reviewed. There were 61 consecutive patients who underwent total laryngectomy and had MDCT of the neck performed within 2 weeks prior to the surgery.
CT imaging protocol and evaluation
The contrast-enhanced MDCT was performed in 64-row scanner with a slice thickness of 2.5 mm and overlapping reconstructions every 1 mm. The MDCT reports dictated by board-certified neuroradiologists were retrospectively reviewed. All the MDCT images were retrieved and then centrally reviewed by a single board-certified neuroradiologist who was blind to final pathological diagnosis. The following criteria were used for clinical staging of thyroid cartilage involvement: (1) minor involvement, which was defined as minor lysis or erosion at the inner aspects of the cartilage without intercartilaginous spread; (2) major involvement, which was defined as having both major lysis or erosion at the inner cartilage lamina and intercartilaginous spread that does not disrupt inner cartilage; (3) invasion through cartilage, which was defined as continuous disruption of both inner and outer aspects of the cartilage, or tumour found on both sides of the cartilage, including extralaryngeal soft tissues.
Histopathological evaluation
All laryngectomy tissue specimens were retrieved for central review. These had been cut into axial whole-organ serial slices parallel to the level of the vocal cord, at 3–5-mm thick intervals and reviewed by a single pathologist specialising in head and neck cancer using criteria previously described by Becker et al [7]. Briefly, cartilage invasion was diagnosed as grade 1 if tumour was identified within the collagen bundles that form the inner perichondrium; grade 2 if there were both intracartiligous tumour spread and the absence of outer perichondrium disruption; and grade 3 if there was tumour on both sides of the cartilage with continuous cartilage destruction.
Statistical analysis
Using the JMP statistical software package (SAS Corporate, Cary, NC), the following factors were calculated: PPV, NPV, sensitivity and specificity. These factors were calculated for the CT grade 3 alone, combination of CT grade 2 and grade 3, and combination of CT grade 1, grade 2 and grade 3.
Results
Patient characterisation
Patient and disease characteristics are shown in Table 1. The majority of patients (85%) had laryngeal cancer. Among the laryngeal cancer cases, 90% arose from the supraglottic larynx. For those with clinically staged T3 cancer, 54% of them had minor thyroid cartilage involvement, while the rest of the cases involved the post-cricoid area, pre-epiglottic tissues or paraglottic space, or had vocal cord fixation with the absence of thyroid cartilage invasion.
Table 1. Patient and tumour characteristics.
| Variable | No. patients | % |
| Age | Mean 57 years | |
| Continuous | Range 33–82 years | |
| Gender | ||
| Male | 42 | 69 |
| Female | 19 | 31 |
| Primary site | ||
| Larynx | 52 | 85 |
| Supraglottis | 47 | 76 |
| Glottis | 4 | 7 |
| Subglottis | 1 | 2 |
| Hypopharynx | 9 | 15 |
| T stage | ||
| cT3 | 52 | 85 |
| Minor thyroid cartilage erosion | 33 | 54 |
| Others | 19 | 31 |
| cT4 | 9 | 15 |
| N stage | ||
| N0 | 8 | 13 |
| N+ | 53 | 87 |
| Post-operative treatment | ||
| None | 6 | 10 |
| Radiation alone | 37 | 60 |
| Chemo alone | 1 | 2 |
| Radiation + chemo | 17 | 28 |
Clinicopathological correlation
Using histology as the gold standard, we determined that the MDCT scan has a PPV of 78% and an NPV of 100% for detection of invasion through cartilage. The sensitivity was 100% and specificity was 96% (Table 2).
Table 2. Patient number and predictive values for detection of grade 3 vs grade 2 or less.
| Pathology grade 3 | Pathology grade 2 or less | PPV (%) (95% CI) | NPV (%) (95% CI) | Sens (%) (95% CI) | Spec (%) (95% CI) | |
| CT scan grade 3 | 7 | 2 | 78 (40–96) | 100 (91–100) | 100 (56–100) | 96 (86–99) |
| CT scan grade 2 or less | 0 | 52 |
PPV, positive predictive value; NPV, negative predictive value; Sens, sensitivity; Spec, specificity; CI, confidence interval.
For detection of any thyroid cartilage invasion (minor, major or through cartilage invasion), MDCT scan has a PPV of 63% and an NPV of 92% (Table 3). The sensitivity was 85% and specificity was 75%. Two of the MDCT-negative patients were upgraded to grade 2 pathology with major cartilage invasion.
Table 3. Patient number and predictive values for detection of any cartilage invasion vs no invasion.
| Pathology any invasion | Pathology no invasion | PPV (%) (95% CI) | NPV (%) (95% CI) | Sens (%) (95% CI) | Spec (%) (95% CI) | |
| CT scan any invasion | 17 | 10 | 63 (42–80) | 92 (75–98) | 85 (61–96) | 75 (59–87) |
| CT scan no invasion | 3 | 31 |
PPV, positive predictive value; NPV, negative predictive value; Sens, sensitivity; Spec, specificity; CI, confidence interval.
For detection of major cartilage invasion (grade 2), MDCT scan has a PPV of 30% (Table 4), with 7 out of 10 patients with CT grade 2 downgraded to a lower pathology grade. This extremely low PPV contributed remarkably to the poor predictive values for detection of grade 2 or higher invasion. PPV was as low as 53% for tumour invasion through cartilage or major cartilage invasion, and NPV was 95%. The proportion of patients who were down-staged from T4 (either tumour invasion through cartilage or major cartilage invasion) to T3 (minor cartilage invasion) after pathology review was 47% (9/19). Figures 1–3 illustrate a case example of a patient who was overstaged using MDCT and was downstaged in such a fashion after pathology review.
Table 4. Patient number and predictive values for detection of grade 2 (major cartilage invasion) vs grade 1 or less.
| Pathology Grade 2 | Pathology Grade 1 or less | PPV (%) (95% CI) | NPV (%) (95% CI) | Sens (%) (95% CI) | Spec (%) (95% CI) | |
| CT scan grade 2 | 3 | 7 | 30 (8–64) | 95 (82–99) | 60 (17–93) | 85 (71–93) |
| CT scan grade 1 or less | 2 | 40 |
PPV, positive predictive value; NPV, negative predictive value; Sens, sensitivity; Spec, specificity; CI, confidence interval.
Figure 1.
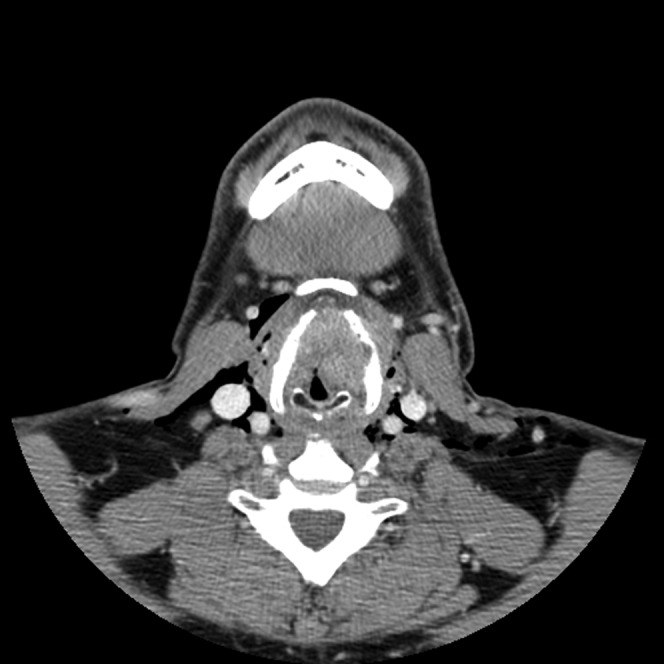
Case example: 55-year-old male with a 100 pack-year smoking history who presented with a month of hoarseness. On multidetector CT, the patient was found to have a large mass measuring 3.5 cm in greatest dimension. On formal review, the lesion was centred on the left false vocal cord extending superiorly along left hypopharyngeal wall and inferiorly involving the true vocal cord. The mass crossed midline involving the anterior commissure and pre-epiglottic fat. The lamina of the thyroid cartilage on the left side was believed have been invaded with disease extension through the thyroid cartilage into the strap muscles. Illustrated is an axial section using soft-tissue windows.
Figure 3.
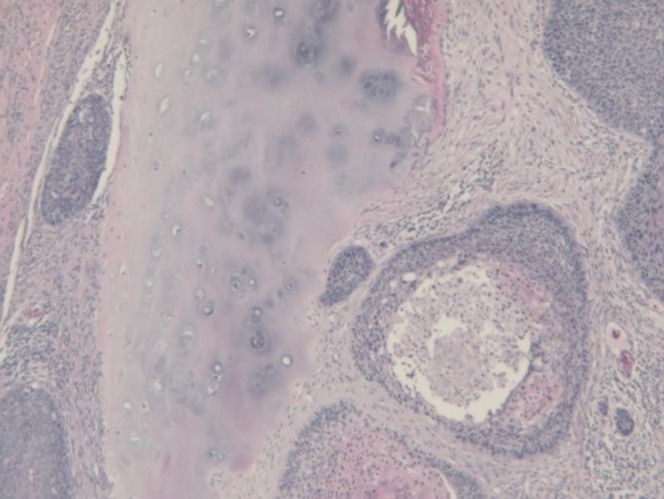
High-powered magnification view of tumour cells abutting but not invading the thyroid cartilage for the patient discussed in Figures 1 and 2.
Figure 2.

Axial section using bone windows for the same case as illustrated in Figure 1. Invasion through the left thyroid cartilage is clearly demonstrated.
Discussion
To our knowledge, this is the first study using fast-speed MDCT to evaluate the PPV of different levels of cartilage invasion (minor, major or through) in a cohort of patients treated by total laryngectomy for clinically staged T3 or T4 cancer. Most notably, we demonstrated, through clinicopathological review, a surprisingly low PPV for detection of any laryngeal cartilage invasion, particularly major invasion. This finding is of critical interest and clinical importance to all members involved in the multidisciplinary head and neck cancer team, because patients with laryngeal cancer with cartilage destruction have generally not been considered appropriate candidates for organ preservation with definitive chemoradiation therapy. Therefore, overstaging with pre-treatment CT theoretically results in a loss of the possible benefit of organ preservation in many potential patients.
In daily practice, the decision-making process for the treatment of locally advanced laryngeal cancer varies significantly among physicians and institutions. The relative weighting of pre-treatment variables to determine the optimal treatment approach also differ. Regardless, the predominant school of thought in head and neck surgery recommends laryngectomy in the presence of positive cartilage destruction, including tumour invasion through thyroid cartilage or major cartilage invasion. The clinical implications of our findings are critically important since we showed a PPV of 53% using MDCT (the most commonly accepted modality for pre-treatment imaging) for tumour invasion through cartilage or major cartilage invasion. Importantly, 9 of 19 patients with clinical T4 disease were downstaged to T3 disease based on pathological findings showing only minor cartilage invasion or absence of invasion. We hypothesise that these findings were mainly due to the very poor PPV for detection of major cartilage invasion. As such, we recommend that patients undergoing total laryngectomy give informed consent specifically regarding the uncertainty of the pre-operation imaging findings. Since most radiation oncologists would recommend organ preservation with chemoradiation therapy for patients with absence of major cartilage destruction, the advent of more accurate pre-treatment staging systems would greatly affect practice patterns in the future. On the other hand, the NPV of 95% for MDCT detection of major cartilage invasion or invasion through cartilage is reassuring.
At most institutions, standard state-of-the-art MDCT is still the preferred imaging method for evaluation of the larynx and hypopharynx [1]. Since multiple studies have shown great variation in PPV, NPV, sensitivity and specificity because of variable technical parameters or variable diagnostic criteria, the value of this technology is still somewhat uncertain [2, 8]. With the help of appropriately selected and combined criteria such as extralaryngeal tumours, sclerosis, and erosion or lysis, Becker et al [7] showed that CT scanning has significantly improved accuracy of the thyroid cartilage invasion detection, with a PPV of 54–76% and an NPV of 79–89%. These radiographical criteria were adapted in this study. Our results are consistent with those from Becker et al and others published in the 1990s [7, 9–11] demonstrating a lack of significant improvement in accuracy of thyroid cartilage differentiation in spite of the use of fast-speed MDCT, which has been the preferred imaging method at our facility in the past 10 years. Notably, other imaging modalities such as MRI have been used in an attempt to improve predictive values. In spite of its excellent soft-tissue delineation capacity, MRI has been shown to have a similar PPV and specificity for cartilage invasion relative to CT and also has a tendency toward over-staging cartilage involvement by tumour. This phenomenon may be secondary to peritumoural inflammation, which may be indistinguishable from cancer on imaging [1, 12]. Using revised criteria, Becker et al [12] recently were able to improve specificity for thyroid cartilage invasion to 75%, compared with 54% using conventional MRI criteria. Further studies on improved methods of distinguishing between T3 and T4 disease is needed for patients diagnosed with locally advanced laryngeal cancer.
Controversy exists regarding the association between CT-depicted cartilage involvement in laryngeal carcinoma and poor outcomes after radiation therapy for locally advanced head and neck cancer [13, 14]. Although clinical evidence of cartilage involvement has historically been considered a contraindication for organ preservation with radiation therapy, more recent studies have suggested that cartilage abnormalities on CT or MRI are not an independent predictor of local failure [15–18]. However, this issue has become of limited clinical importance because definitive radiotherapy alone is no longer recommended in light of results from RTOG 9111 showing that definitive radiotherapy alone had significantly worse local control, distant metastasis and larynx preservation rate than chemoradiotherapy [4]. Consequently, the standard of care for T3 or T4 laryngeal cancer is either concurrent chemoradiation or total laryngectomy.
The results of the present study demonstrate that patient selection for chemoradiotherapy or total laryngectomy is not as straightforward as it appears on the surface. Notably, the relatively low PPV for the detection of cartilage invasion using MDCT suggests that a large proportion of clinically staged T4 laryngeal cancer patients who were excluded from organ preservation with chemoradiation therapy in fact could have only had minor cartilage invasion or absence of cartilage invasion on subsequent pathology (and hence technically eligible for organ preservation). If these clinically overstaged T4 patients had been treated with chemoradiation therapy, one could have anticipated local control and functional outcomes similar to patients with T3 disease treated with chemoradiation. To complicate matters, several recently published retrospective reports suggest that patients with cartilage invasion can successfully be treated in a non-surgical manner [19, 20]. Although the extent of cartilage invasion was not specifically quantified in these studies, the findings are nonetheless provocative. Knab et al [19] reported on patients treated by definitive chemoradiotherapy for T4 laryngeal cancer patients with tumour extension through the thyroid cartilage. They showed local regional control, disease-g0ree survival and laryngectomy-g0ree survival similar to the results from T3 patients treated in RTOG 9111. In another retrospective study, Do et al [20] showed similar local regional control rates between patients with cartilage invasion treated with definitive chemoradiation therapy or surgery followed by chemoradiation. Large prospective trials are needed to test the feasibility and effectiveness of definitive chemoradiation therapy for T4 laryngeal cancer patients.
However, as organ preservation therapy with chemoradiation has gain popularity, an increasing number of studies have suggested that chemoradiation is associated with significant late toxicities. One recent finding from a secondary analysis of three RTOG trials showed that severe late toxicity, particularly with respect to swallowing and xerostomia, was common (43%) in head and neck patients who underwent concurrent chemoradiation, and that advanced T-stage and larynx/hypopharynx primary site were strong independent risk factors [21]. Therefore, one may re-evaluate the role of total laryngectomy given the high risk of radiation-induced late toxicity associated with organ preservation with chemoradiation therapy. The reality, however, is that many of those patients treated with surgery upfront ultimately require post-operative radiation because of perineural invasion, lymphovascular involvement or N2/N3 nodal disease, all of which are highly associated with T3 or T4 disease. A significant portion of them even require trimodality treatment with post-operative chemoradiaiton owing to the presence of positive margins or extracapsular nodal spread found at surgical pathology. This is well exemplified in our study, where a majority (60%) of the patients received post-operative radiotherapy, and 28% received post-operative chemoradiation. Unfortunately, for those patients who received radiation therapy either after surgery or in combination with chemotherapy, they suffered significant high-grade dysphagia and impaired quality of life in general, as demonstrated by a large prospective study [22].
The present study is limited by factors inherent in any retrospective analysis. Notably, heterogeneity existed in the quality of pathological specimens given that tissue samples were prepared by different pathologists. Furthermore, this study included a relatively small number of patients, particularly with respect to the subgroup of patients with major cartilage invasion alone (grade 2). Therefore, these conclusions still must be interpreted with caution. Future prospective studies with larger patient number are needed to validate the findings from our hypothesis-generating exercise.
Lastly, one should keep in mind that a pre-treatment imaging finding of cartilage invasion is certainly not the sole factor in determining the optimal treatment of locally advanced laryngeal cancer. In most cases, treating physicians should consider the combination of imaging results together with other conditions such as disease volume, laryngoscopy findings, pre-treatment voice quality, medical urgency, patient comorbidities, psychosocial situation, patient preference and local therapeutic expertise. In this regard, we recommend that all patients with newly diagnosed locally advanced laryngeal cancer undergo assessment by a multidisciplinary team with appropriate selection and optimisation of therapy in accord with guidelines proposed by the American Society of Clinical Oncology [5].
Conclusion
The low PPV for cartilage destruction using MDCT suggests that a significant proportion of patients who are treated by total laryngectomy for locally advanced laryngeal cancer could have been appropriately offered organ preservation if staged accurately at diagnosis. This finding has critical implications regarding the selection of therapy and patient quality of life. Prospective studies with larger sample sizes are recommended to validate this hypothesis in the future. In the meantime, further investigation is needed to improved methods of distinguishing between T3 and T4 disease for patients diagnosed with locally advanced laryngeal cancer. The importance of multidisciplinary co-ordination to optimise therapy for an individual patient cannot be overstated.
References
- 1.Hermans R. Staging of laryngeal and hypopharyngeal cancer: value of imaging studies. Eur Radiol 2006;16:2386–400 [DOI] [PubMed] [Google Scholar]
- 2.Becker M, Neoplastic invasion of laryngeal cartilage: radiologic diagnosis and therapeutic implications. Eur J Radiol 2000;33:216–29 [DOI] [PubMed] [Google Scholar]
- 3.The Department of Veterans Affairs Laryngeal Cancer Study Group Induction chemotherapy plus radiation compared with surgery plus radiation in patients with advanced laryngeal cancer. N Engl J Med 1991;324:1685–90 [DOI] [PubMed] [Google Scholar]
- 4.Forastiere AA, Goepfert H, Maor M. Concurrent chemotherapy and radiotherapy for organ preservation in advanced laryngeal cancer. N Engl J Med 2003;349:2091–8 [DOI] [PubMed] [Google Scholar]
- 5.Pfister DG, Laurie SA, Weinstein GS, Mendenhall WM, Adelstein DJ, Ang KK, et al. American Society of Clinical Oncology clinical practice guideline for the use of laryn-preservation strategies in the treatment of laryngeal cancer. J Clin Oncol 2006;24:3693–704 [DOI] [PubMed] [Google Scholar]
- 6.National Comprehensive Cancer Network The NCCN Head and Neck Cancers Clinical Practice Guidelines in Oncology (Verson 1. 2009) Available at URL: http://www.nccn.org. Accessed on 1 September, 2009 . [Google Scholar]
- 7.Becker M, Abaren P, Delavelle J, Kurt AM, Egger C, Rüfenacht DA, et al. Neoplastic invasion o the laryngeal cartilage: reassessment of criteria for diagnosis at CT. Radiology 1997;203:521–32 [DOI] [PubMed] [Google Scholar]
- 8.Fernandes R, Gopalan P, Spyridakou C, Joseph G, Kumar M. Predictive indicators for thyroid cartilage involvement in carcinoma of the larynx seen on spiral computed tomography scans. J Laryngol Otol 2006;120:857–60 [DOI] [PubMed] [Google Scholar]
- 9.Becker M, Zbaren P, Laeng H, Stoupis C, Porcellini B, Vock P. Neoplastic invasion o the laryngeal cartilage: comparison of MR imaging and CT with histopathologic correlation. Radiology 1995;194:661–9 [DOI] [PubMed] [Google Scholar]
- 10.Castelijns JA, Gerritsen GJ, Kaiser MC, Valk J, van Zanten TE, Golding RG, et al. Invasion of laryngeal cartilage by cancer: comparison of CT and MR imaging. Radiology 1988;167:199–206 [DOI] [PubMed] [Google Scholar]
- 11.Sulfaro S, Barzan L, Querin F, Lutman M, Caruso G, Comoretto R, et al. T-staging of the laryngopharyngeal carcinoma: a 7-year multidisciplinary experience. Arch Otolaryngol Head Neck Surg 1989;115:613–20 [DOI] [PubMed] [Google Scholar]
- 12.Becker M, Zbaren P, Casselman JW, Kohler R, Dulguerov P, Becker CD. Neoplastic invasion o the laryngeal cartilage: reassessment of criteria for diagnosis at CT imaging. Radiology 2008;249:551–9 [DOI] [PubMed] [Google Scholar]
- 13.Issacs JH, Mancuso AA, Mendenhall WM, Parsons JT. Deep spread patterns in CT staging of T2-4 squamous cell laryngeal carcinoma. Otolaryngol Head Neck Surg 1988;99:455–64 [DOI] [PubMed] [Google Scholar]
- 14.Million RR. The myth regarding bone or cartilage involvement by cancer and the likelihood of cure by radiotherapy. Head Neck 1989;11:30–40 [DOI] [PubMed] [Google Scholar]
- 15.Hermans R, Van denBogaert W, Rijnders A, Doornaert P, Baert AL. Predicting the local outcome of glottic cancer treated by definitive radiation therapy: value of computed tomography determined tumor parameters. Radiother Oncol 1999;50:39–46 [DOI] [PubMed] [Google Scholar]
- 16.Hermans R, Van denBogaert W, Rijnders A, Doornaert P, Baert AL. Value of computed tomography determined tumor parameters as outcome predictor of supraglottic cancer treated by definitive radiation therapy. Int J Radiat Oncol Biol Phys 1999;44:755–65 [DOI] [PubMed] [Google Scholar]
- 17.Castelijns JA, van denBrekel MWM, Tobi H, Smit EM, Golding RP, van Schaik C, et al. Laryngeal carcinoma after radiation therapy: correlation of abnormal MR imaging signal pattern in laryngeal cartilage with the risk of recurrence. Radiology 1996;198:151–5 [DOI] [PubMed] [Google Scholar]
- 18.Ljumanovic R, Langendijk JA, Schenk B, Van Wattingen M, Knol DL, Leemans CR, et al. Supraglottic carcinoma treated with curative radiation therapy: identification of prognostic groups with MR imaging. Radiology 2004;232:440–8 [DOI] [PubMed] [Google Scholar]
- 19.Knab BR, Salama JK, Solanki A, Stenson KM, Cohen EE, Witt ME, et al. Functional organ preservation with definitive chemoradiotherapy for T4 laryngeal squamous cell carcinoma. Annal Oncol 2008;19:1650–4 [DOI] [PubMed] [Google Scholar]
- 20.Do L, Puthawala A, Syed N, Azawi S, Williams R, Vora N. Treatment outcomes of T4 locally advanced head and neck cancers with soft tissue invasion or bone and cartilage invasion. Am J Clin Oncol. doi: 10.1097/COC.0b013e31819380a8. Epub ahead of print. [DOI] [PubMed] [Google Scholar]
- 21.Machtay M, Moughan J, Trotti A, Gargen AS, Weber RS, Cooper JS, et al. Factors associated with severe late toxicity after concurrent chemoradiation for locally advanced head and neck cancer: an RTOG analysis. J Clin Oncol 2008;26:3581–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Langendijk JA, Doornaert P, Verdonck-de Leeuw IM, Leemans CR, Aaronson NK, Slotman BJ. Impact of late treatment-related toxicity on quality of life among patients with head and neck cancer treated with radiotherapy. J Clin Oncol 2008;26:3770–6 [DOI] [PubMed] [Google Scholar]


