Abstract
Objectives
In the UK, the treatment of patients with mycosis fungoides using total skin electron (TSE) beam therapy is undertaken using a number of different irradiation techniques. As part of a review of these techniques, a comparative set of measurements would be useful to determine how the techniques differ in terms of dose distribution. A dose penetration intercomparison method that could be used as part of such a study is presented here.
Methods
The dose penetrations for six treatment techniques currently or recently used in four centres in the UK were measured. The variation of dose with skin depth was measured in a WT1 solid water mid-torso phantom. The phantom is portable and suitable to be used in all the techniques. It is designed to hold four small radiochromic film dosemeters to investigate the variation in dose around the mid-torso. For each treatment technique, the phantom was irradiated using the clinical set-up.
Results
The phantom performed well and was able to measure dose penetration and the uniformity of penetration for several treatment techniques.
Conclusion
These preliminary results demonstrate that there is some variation in dose distribution between different TSE treatment techniques and that the phantom could be used in a more comprehensive intercomparison. The results are not intended to demonstrate comprehensively the range of penetration that can be achieved in clinical practice as, for one of the treatment techniques, the penetration is customised for the extent of the disease.
Mycosis fungoides is the most common skin lymphoma and is a distinct form of cutaneous T-cell lymphoma. It is rare, with an annual incidence of approximately three new cases per million people [1]. The treatment of mycosis fungoides with total skin irradiation was suggested at least 50 years ago. Since that time, various techniques have been developed and applied successfully to the treatment of this disease [2].
A low-energy electron beam (4–7 MeV) is used to provide the required dose penetration. An extended source to surface distance (SSD) is usually required to produce a large field size at the skin surface. This extended SSD can also have the desirable effect of increasing the relative dose at the skin surface and in the build-up region, demonstrated by Cygler et al [3] for small fields. However, increased SSD will also increase relative photon contamination.
The objective is to minimise toxicity while providing sufficient dose to the target volume, which comprises the epidermis, adnexal structures and dermis [1]. In effect, the aim is a homogeneous dose to a specified distance below the skin surface. In reality, it is impossible to achieve a homogeneous dose as beam obliquity tends to increase side scatter and decrease depth of penetration.
In the UK, several different total skin electron (TSE) delivery techniques are currently being used. To compare dose penetration and uniformity between techniques, a method was required that would perform consistently for all the techniques in use. Such a comparison method could then contribute to assessing techniques against the European Organization for Research and Treatment of Cancer (EORTC) requirements [1] or modifying recommendations based upon the clinical evidence with these techniques.
Here, we present a phantom for the measurement of TSE dose penetration and the results for six delivery techniques currently or recently in use in the UK. This study does not, however, represent a comprehensive intercomparison of the dosimetry of all the techniques currently in use in the UK. In fact, even in a single TSE centre, there may be more than one technique available, e.g. to treat to different depths to accommodate different clinical requirements.
Materials and methods
In order to produce dose distributions that are representative of treatment dose distributions, a realistic patient phantom and an accurate dosemeter system were required. The method also needed to be flexible, so that it could be used with several different treatment techniques, and relatively simple, so that there was a realistic possibility of collecting a significant amount of data.
Phantom design
The TSE phantom was constructed to simulate a section through the mid-torso using the epoxy resin “solid water” material WT1 (St Bartholomew's Hospital, London, UK). The mid-torso was used because the prescription point is typically in this region and it is most representative of the overall dose distribution. The mid-torso section was simplified to an ellipse of height 250 mm and width 400 mm. An ellipse was used to study the effect of the body's natural curvature and the incident angle of the electron beam on the dose received. Because this is a symmetrical design, the phantom could be further reduced to a semi-arc, as shown in Figure 1. The phantom holds four inserts, A, B, C and D, each designed to hold a piece of radiochromic film at 0°, 30°, 60° and 90° to the vertical. Some TSE techniques require the patient to be standing; hence, the phantom can be mounted on a stand at a set height.
Figure 1.
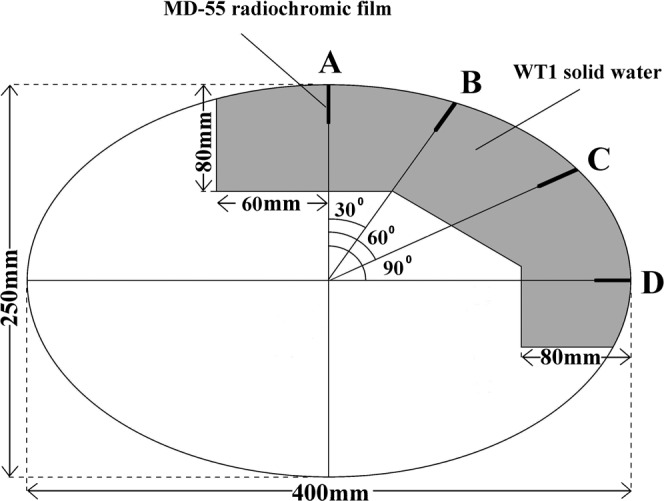
Schematic diagram of the Coventry total skin electron phantom showing radiochromic film positions.
Dosemeter characteristics
Radiochromic film was used to measure dose at depth. The radiochromic film used was GafChromic dosimetry media MD-55 (ISP Technologies, Wayne, NJ). The suitability of the MD-55 film as a dosemeter for megavoltage electron beams has been previously confirmed [4-7].
Crucially, the sensitivity of radiochromic film is relatively independent of energy compared with other dosemeters. The quoted energy variation for MD-55 film is <5% difference in net density for 50 Gy exposures at 1 MeV and 18 MeV. Since the start of this work, radiochromic films such as GafChromic EBT with an even smaller variation with energy have been made available; this will be considered in further studies.
As recommended by AAPM Task Group 55 [4], each film was read after a 24 h stabilisation period. Films were measured using a modified Welhofer WP102 densitometer. The scanning mechanism was modified to scan across the film in fixed (0.32 mm) steps. The densitometer was modified to use a 660 nm light-emitting diode light source corresponding to the peak in the absorption spectrum for the MD-55 film.
Through experiment, it has been found that a dose of 5 Gy at the surface is required to produce sufficient darkening in the film. The accuracy of TSE dose measurements using MD-55 film has been estimated by Gamble et al [5] to be ±0.04 Gy or 0.1% of the maximum dose for a 5 Gy exposure. We estimated the total uncertainty in our percentage depth–dose measurements using MD-55 film and the scanning densitometer to be ±0.7 mm (resulting from errors in positioning in the densitometer and accuracy of scanning). The total uncertainty in phantom measurements, including reproducibility of set-up and film reproducibility, was determined from the standard error for successive measurements as ±5% of the maximum dose.
Additional confidence in the technique was provided by comparison of MD-55 film measurements in the WT1 solid water TSE phantom made as part of this study and thermoluminescent dosemeter measurements in a Perspex phantom made by one of the test centres during commissioning. These two independent sets of measurements were in good agreement considering that different phantoms and dosimetry techniques were used (Figure 2).
Figure 2.
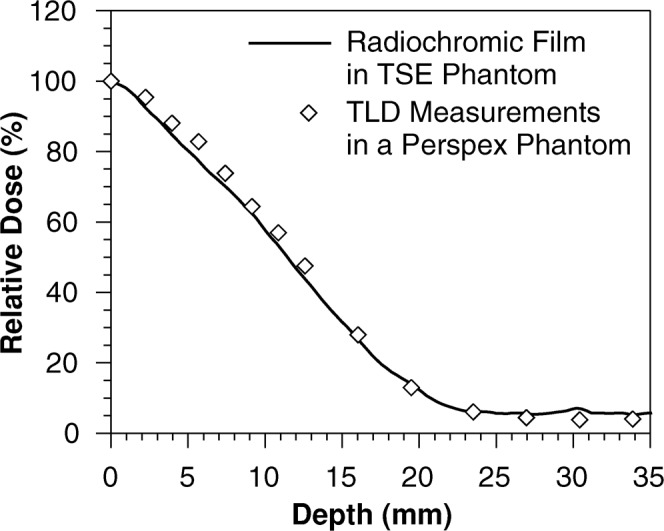
Comparison between MD-55 film measurements and thermoluminescent dosemeter measurements using the rotational technique.
If there was variation in surface dose then the point at which the data were normalised would affect the comparison of the percentage depth–dose curves. Where possible, data were normalised according to the practice adopted by the TSE centre for prescribing the dose.
Reproducibility
Further measurements will be made by sending the TSE phantom to other TSE centres and asking them to expose the phantom and return the radiochromic films for analysis. To test this procedure, the phantom was sent to one of the TSE centres and physics staff there repeated the original phantom exposure. This process also served as an indication of how reproducible the measurements were, as it was likely that there was some random error associated with setting up the phantom.
The repeat measurements agreed with all depth–dose measurements within ±5% maximum dose (Figure 3). Measured depths of 80% maximum dose agreed within ±1.3 mm.
Figure 3.
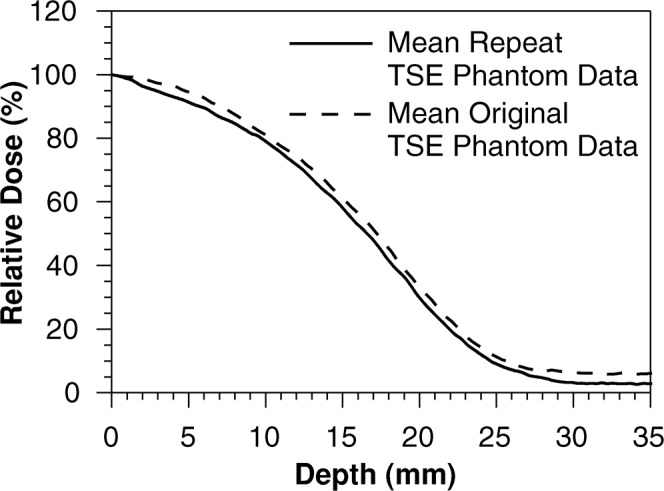
Comparison of mean original depth–dose measurements with those from a repeated exposure by the total skin electron centre.
Benchmark
To increase confidence in the measurements, a test centre was asked to measure a depth–dose for its TSE beam using a WT1 solid water cuboid block loaded with MD-55 film. The centre then supplied its standard measured TSE depth–dose data for comparison with the measurement.
The comparison of the MD-55 film measured depth–dose with the TSE centre′s standard TSE depth–dose data was good. The standard curve agrees with the measured depth–dose within the precision of the technique (Figure 4).
Figure 4.
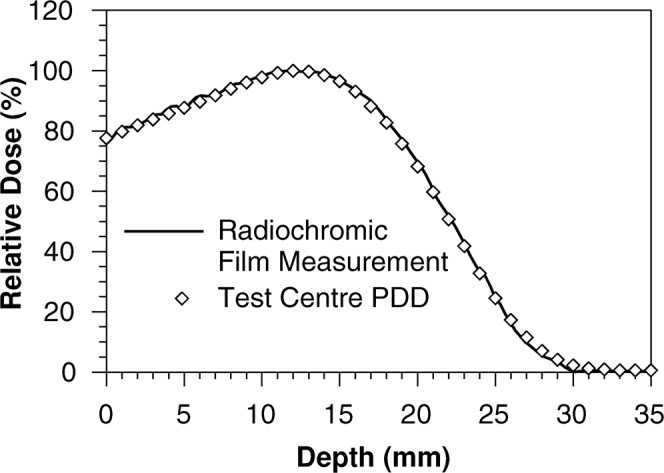
Comparison of MD-55 film measurements with the standard depth–dose curve for the total skin electron beam.
Treatment techniques
A brief description of each TSE technique studied follows. The descriptions are by no means comprehensive and are only intended to assist in interpretation of the versatility of the phantom.
Arcing technique
The arcing technique studied uses a 6 MeV electron beam produced by a linear accelerator. Two posterior and two anterior fields are given. For each field, the patient is lying as the treatment machine gantry is rotated through two arcs. The two arcs, superior and inferior, provide full coverage along the patient. The patient lies on a purpose-built couch, which tilts the lateral axis of the patient at 30° to the horizontal to optimise the dose distribution around the torso at depth.
Translational betatron technique
The translational technique employs a compact betatron. The patient lies on a horizontal couch while the betatron beam is directed at 30° to the vertical, which directs the radiation obliquely at the patient. The betatron is moved along a track over the full length of the patient. Four treatment beams are used in the technique: anterior left and right oblique and posterior left and right oblique; this is achieved by changing the patient’s position on the couch.
Dual angle (Stanford) technique
In this interpretation of the Stanford University linear accelerator technique, the patient stands at 400 cm from the accelerator source on a wooden platform, which rotates on its axis in steps of 60° to receive an anterior, a posterior and four oblique fields. Each field is composed of a dual angulated beam, one with its axis angled 14° above horizontal and the other with its axis angled 14° below horizontal, so that a uniform dose distribution is achieved over the entire height and width of the patient in a vertical plane.
Static four-field technique
This technique employs four fields (anterior, posterior and two laterals), with the patient lying at an extended SSD of nominally 150 cm and placed in various positions to achieve the different beam directions. It uses a customised aluminium cone applicator designed to optimise the penumbra for matching adjacent fields for coverage both around and along the whole body. A 6 MeV electron beam is used with a 6-mm Perspex degrader close to the patient and variable-thickness Perspex degraders placed at the end of the cone—the latter being selected to achieve the specific therapeutic range specified by the treating clinician. For the phantom irradiation, a 3-mm degrader was used at that position to achieve a 5-mm therapeutic range.
Static smoothed technique
To further improve homogeneity of dose distribution around the body, the static four-field technique can be used in a more complex manner. This smoothed technique continues to use four fields around the body in each fraction, but each set of fields is angled differently on each specific fraction in a five-fraction set (0, ±15° and ±30°) and this is repeated over each week of treatment. The intention is to give a smoothing effect to the combined dose distribution. This spreads and combines irradiation from 20 directions, but with only 4 directions used in any one fraction. Again, the combination of degraders can be selected to achieve the therapeutic range requested clinically. For the purpose of this study, the TSE phantom was exposed to 17 of the 20 fields, as 3 fields were deemed to give a negligible dose contribution to the position of the dosemeter.
Rotational (Montreal) technique
In this interpretation of the Montreal technique [8], the patient stands on a rotating platform with one arm extended. The platform and the patient rotate at five revolutions per minute. A 6 MeV electron beam is degraded to 3.6 MeV by a 6-mm Plexiglas shield placed 20 cm from the patient. A single direct beam is used at a gantry angle of 90° and a collimator angle of 45°.
Experimental results
It should be borne in mind that the depth of penetration and the prescription of dose will be dependent upon local techniques and clinical requirements.
Arcing technique
Data were normalised to the surface dose at position A, consistent with the practice of prescribing to the midpoint of the patient (Figure 5).
Figure 5.
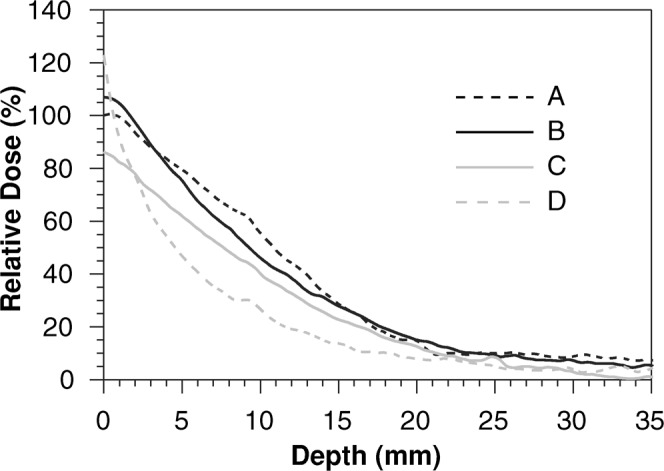
The depth–dose curves relative to the surface dose at position A for the arcing total skin electron technique.
There was reasonable uniformity over the phantom. However, there was a reduction in both the surface dose and the depth–dose with an increase in the angle to the central axis of the beam, with the exception of a relatively high surface dose at position D.
Translational betatron technique
As with the arcing technique, data were normalised to the surface dose at position A (Figure 6).
Figure 6.
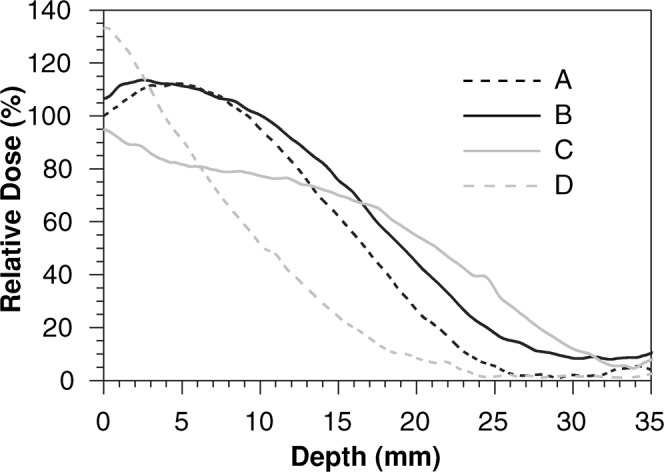
The depth–dose curves relative to the surface dose at position A for the translational betatron total skin electron technique.
There was reduced dose homogeneity when compared with the arcing technique, and the relatively high surface dose at position D remains. The depth of 80% dose was deeper than the other five techniques presented here.
Dual angle (Stanford) technique
Data were normalised to the maximum surface dose, consistent with the prescribing practice of the TSE centre (Figure 7).
Figure 7.
The depth–dose curves relative to the surface dose at position A for the dual angle total skin electron technique.
There was some variation between doses near the skin surface depending on the angle to incident beams, but this effect was reduced beyond 5 mm depth.
Static four-field technique
Data were normalised to the mean surface dose (Figure 8); however, note that in this particular centre dose prescription is tailored to the clinical requirements for the treatment.
Figure 8.
The depth–dose curves relative to the mean surface dose for the static four-field total skin electron technique.
As with the Stanford technique, there was some variation between doses near the skin surface depending on the angle to incident beams, but this effect was small beyond 5 mm depth.
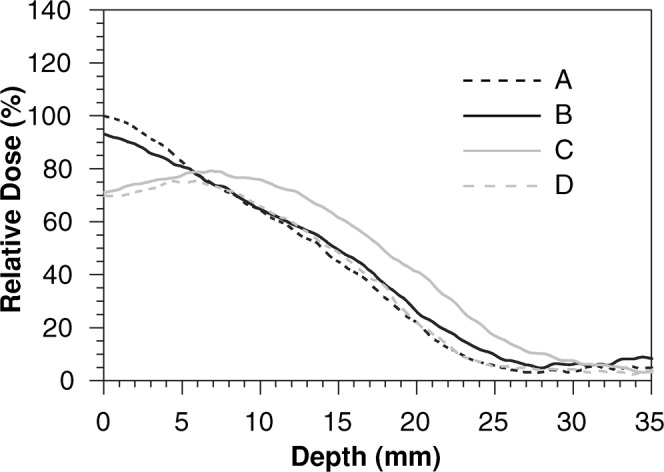
Static smoothed technique
As with the static four-field technique, data were normalised to the mean surface dose (Figure 9), but again note that in this particular centre the dose prescription is tailored to the clinical requirements for the treatment.
Figure 9.
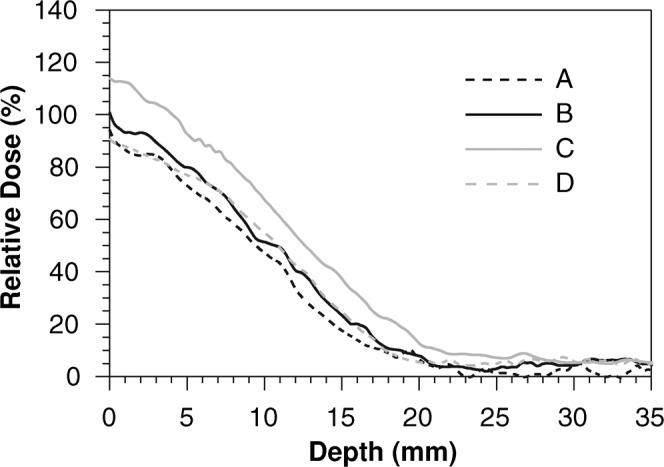
The depth–dose curves relative to the mean surface dose for the static smoothed total skin electron technique.
The smooth technique showed a relationship similar to that of the four-field technique but with improved uniformity owing to the increased number of fields. There was a generally higher dose at position C than at the other three positions.
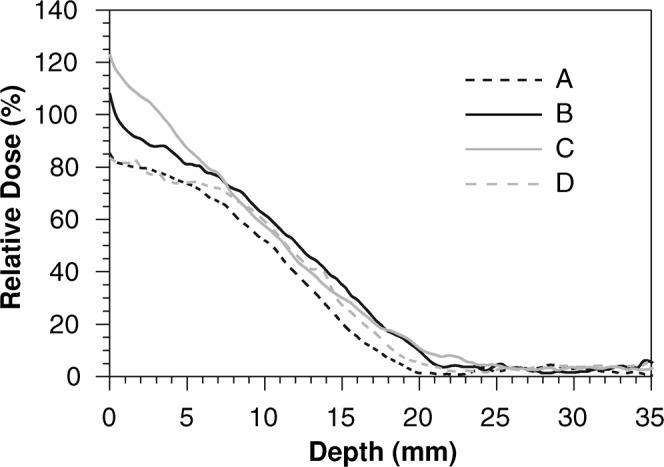
Rotational (Montreal) technique
Data were normalised to the surface dose at position A, consistent with the practice of prescribing to the midpoint of the patient (Figure 10).
Figure 10.
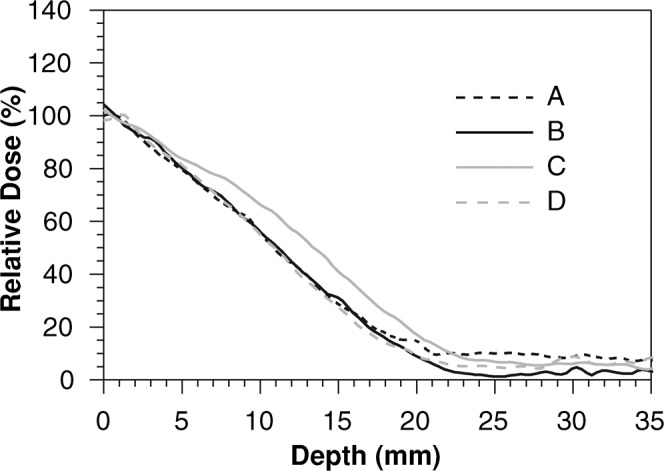
The depth–dose curves relative to the surface dose at position A for the rotational total skin electron technique.
The variation between the depth–doses in the four positions was small. This was as expected as all positions should be irradiated equally; any variation in dose was therefore a result of the phantom geometry.
Comparison of the mean data
A measurement summary is given in Table 1. Data were quoted using the normalisation methods described above. For convenience, penetration was described as the depth to 80% and 20% dose for mean data. These values represented an average depth–dose for each technique by taking the mean of measurements for positions A–D. Non-uniformity was indicated by the spread in values at the four positions A–D.
Table 1. Summary of measurements in the TSE phantom.
| Treatment technique | Depth of 80% dose for mean data (mm) | Spread in depth of 80% dose (mm) | Depth of 20% dose for mean data (mm) | Spread in depth of 20% dose (mm) |
| Arcing | 2.6 | ±1.3 | 15.4 | ±3.1 |
| Translational betatron | 10.3 | ±4.1 | 23.3 | ±5.9 |
| Dual angle | 4.4 | ±1.3 | 21.7 | ±2.1 |
| Static four-field | 4.9 | ±2.2 | 16.6 | ±1.2 |
| Static smooth | 5.1 | ±2.0 | 16.3 | ±2.1 |
| Rotational | 5.3 | ±0.7 | 17.4 | ±1.5 |
TSE, total skin electron.
Discussion
Although reasonable dose penetration was seen for all techniques, the phantom measurements do highlight some differences in both depth of penetration and uniformity. This suggests that a full-scale dosimetry intercomparison study is warranted.
However, it is important to note that only dose penetration is presented. Several other factors need to be considered when reviewing the dose distribution for a TSE technique. Further work should include measurement of absolute surface doses, photon contamination dose at depth and in-air profiles off the central axis. Any study should also take into account the clinical use of the technique. In particular, the normalisation of results needs careful consideration, taking into account the prescribing method at the individual centre. There should also be discussion about the way techniques are tailored to individual patients. The technique may not be fixed, but adaptable to the clinical indications—such that a single measurement is not representative. There may also be benefits to certain techniques in terms of the dose distribution in particular anatomical regions, such as the top of the head or the inner thighs.
When such a dosimetry study is complete, it could form part of a review of UK TSE treatment techniques. Such a review of techniques should also include clinical evidence and practical considerations.
Conclusion
A TSE dose penetration intercomparison method was successfully applied to six TSE techniques. This demonstrated that the Coventry TSE phantom could be utilised for the comparison and evaluation of overall penetration and the variation in depth–dose curves for different TSE treatment techniques. Furthermore, the preliminary results demonstrate that there is some variation in dose distribution between different TSE treatment techniques, which requires further investigation.
Acknowledgments
We are indebted to the participating TSE centres and, in particular, to David Thwaites, Andrew Morgan and Stephen Locks.
References
- 1.Jones GW, Kacinski BM, Wilson LD, Willemze R, Spittle M, Hohenberg G, et al. Total skin electron radiation in the management of mycosis fungoides: consensus of the European Organization for Research and Treatment of Cancer (EORTC) Cutaneous Lymphoma Project Group. J Am Acad Dermatol 2002;47:364–70 [DOI] [PubMed] [Google Scholar]
- 2.Jones GW, Hoppe RT, Glatstein E. Electron beam treatment for cutaneous lymphoma. Hematol Oncol Clin North Am 1995;9:1057–76 [PubMed] [Google Scholar]
- 3.Cygler J, Allen Li X, Ding GX, Lawrence E. Practical approach to electron beam dosimetry at extended SSD. Phys Med Biol 1997;42:1505–14 [DOI] [PubMed] [Google Scholar]
- 4.Niroomand-Rad A, Blackwell C, Coursey B, Gall K, Galvin J, McLaughlin W, et al. Radiochromic film dosimetry recommendations of AAPM Radiation Therapy Committee Task Group 55. Med. Phys 1998;25:2093–115 [DOI] [PubMed] [Google Scholar]
- 5.Gamble LM, Farrell TJ, Jones GW, Hayward JE. Composite depth–dose measurement for total skin electron (TSE) treatments using radiochromic film. Phys Med Biol 2003;48:891–8 [DOI] [PubMed] [Google Scholar]
- 6.Klassen NV, Van derZwan L, Cygler J. GafChromic MD55: investigation as a precision dosemeter. Med Phys 1997;24:1924–34 [DOI] [PubMed] [Google Scholar]
- 7.Zhu Y, Kirov AS, Mishra V, Meigooni AS, Williamson JF. Quantitative evaluation of radiochromic film response for two-dimensional dosimetry. Med Phys 1997;24:223–31 [DOI] [PubMed] [Google Scholar]
- 8.Kim TH, Pla C, Pla M, Podgorsak EB. Clinical aspects of rotational total skin electron irradiation. Br J Radiol 1984;57:501–6 [DOI] [PubMed] [Google Scholar]


