Abstract
Renal replacement lipomatosis is a rare benign entity in which extensive fibrofatty proliferation of the renal sinus is associated with marked renal atrophy. In this report, we present a case of massive renal replacement lipomatosis demonstrated on MRI. The presentation was atypical given an absence of associated renal calculus disease, and an initial CT scan was interpreted as suspicious for a liposarcoma. The differential diagnosis and key MRI findings that served to establish this specific diagnosis are reviewed. Histopathological correlation is also presented, as the patient underwent nephroureterectomy.
Renal replacement lipomatosis is a benign pathological entity in which marked atrophy of the renal parenchyma is coupled with extensive fibrofatty proliferation in the renal sinus. In more than 70% of cases, parenchymal atrophy is secondary to calculus disease, resulting in hydronephrosis and chronic inflammation [1]. In this report, we present a case of massive replacement lipomatosis not associated with calculus disease. MRI, including the use of sequences for fat characterisation, played a key role in suggesting the diagnosis pre-operatively, and subsequent nephrectomy provided histopathological confirmation of the diagnosis.
Case report
A 79-year-old woman with a history of hysterectomy complicated by distal left ureteral stricture and subsequent left hydroureteronephrosis and recurrent episodes of pyelonephritis underwent CT at an outside institution for abdominal fullness. This CT scan was interpreted as suspicious for a left retroperitoneal liposarcoma with involvement of the left kidney. The patient then underwent MRI at our institution for further evaluation of the suspected mass.
MRI demonstrated a markedly enlarged left kidney measuring over 23 cm. A coronal single-shot half-Fourier turbo spin-echo image (Figure 1) showed a large T2 hyperintense structure expanding the renal sinus that demonstrated hyperintensity on in-phase T1 weighted gradient-echo images (Figure 2a). This region showed a peripheral rim of signal drop-out along its margin with adjacent renal parenchyma on out-of-phase T1 weighted gradient-echo images (Figure 2b) and complete signal drop-out on chemically selective fat-saturation T1 weighted gradient-echo images (Figure 3a), findings that are indicative of adipose tissue. There were additional ovoid T2 hyperintense structures more peripherally within the renal parenchyma that were hypointense on all of the T1 weighted sequences, corresponding with severely dilated, fluid-filled calyces in the setting of hydronephrosis. There was associated cortical thinning. Post-gadolinium chemically selective fat-saturation T1 weighted gradient-echo images (Figure 3b) demonstrated a thin rim of enhancing renal parenchyma surrounding the severely dilated calyces, but no excretion of contrast into the renal collecting system. The renal sinus fat demonstrated circumscribed margins, conforming to the expected contour of the expanded renal sinus, without invasion into surrounding structures or any other evidence to indicate the presence of a fatty tumour. In addition, visualised portions of the left ureter were markedly dilated, thick walled and enhancing. Based upon these MRI findings, the patient was diagnosed with benign renal replacement lipomatosis with severe hydroureteronephrosis and ureteritis.
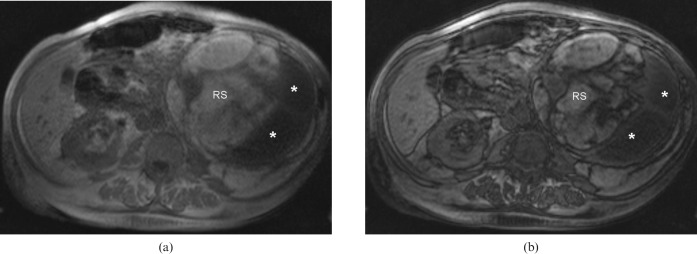
Figure 1.
Coronal single-shot half-Fourier turbo spin-echo image of the abdomen demonstrates a markedly enlarged left kidney with a prominent hyperintense structure expanding the renal sinus (RS) that proved to represent extensive fatty proliferation in the setting of renal replacement lipomatosis. There were additional ovoid hyperintense structures (*) more peripherally within the region of the atrophied renal parenchyma, corresponding with fluid-filled, significantly dilated renal calyces.
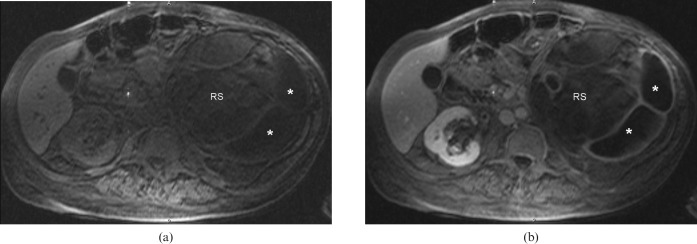
Figure 2.
Axial in-phase (a) and out-of-phase (b) gradient-echo T1 weighted images of the abdomen demonstrate T1 hyperintensity of the tissue expanding the left renal sinus (RS). Although the T1 hyperintensity by itself is non-specific, the peripheral etching along its margin with adjacent renal parenchyma indicates the fatty nature of this tissue. The dilated renal calyces peripherally are T1 hypointense (*), consistent with their fluid content.
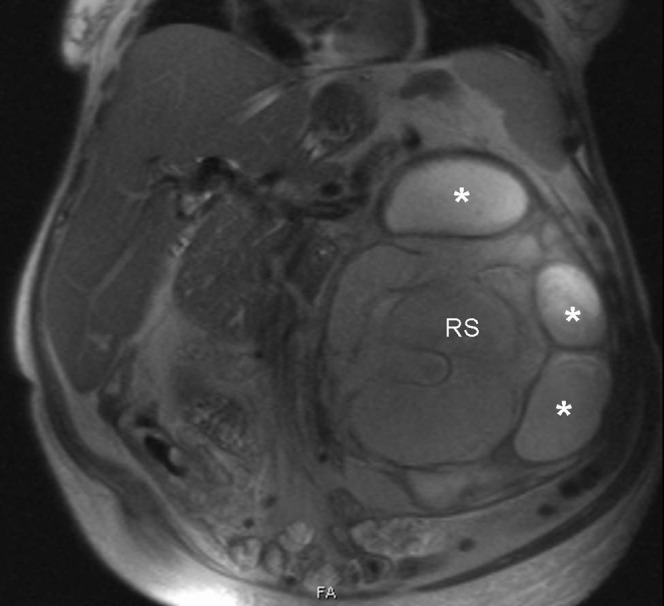
Figure 3.
Axial chemically selective fat-saturation gradient-echo T1 weighted images before (a) and after (b) the intravenous administration of gadolinium chelate demonstrate complete loss of signal of the structure expanding the left renal sinus (RS) that was hyperintense on the in- and out-of-phase T1 weighted images, confirming the fatty nature of this tissue. The dilated renal calyces peripherally (*) fail to demonstrate excretion on the post-contrast images.
The patient proceeded to undergo left nephroureterectomy to the level of the distal ureteral stump. Gross examination confirmed a markedly enlarged dilated kidney weighing 2950 g. The involved kidney showed loss of the usual renal configuration both because of cystic dilatation of the renal pelvis and because of extensive replacement of renal parenchyma by yellow lobulated adipose tissue. Upon bivalving the kidney, 2 l of purulent material exuded from the dilated renal pelvicalyceal system. The renal pelvis focally showed firm white plaque and polypoid material resulting from inflammatory change. On histopathological examination (Figure 4a,b), the kidney showed marked parenchymal atrophy consisting of diffuse interstitial fibrosis of parenchyma with only rare residual glomeruli and dilated tubules showing thyroidisation. The abundant adipose tissue replacing the atrophic renal parenchyma was devoid of any evidence of neoplasia, specifically lacking any evidence of liposarcoma such as atypical lipocytes or lipoblasts. The urothelial lining of the renal pelvis was largely replaced by a dense chronic inflammatory infiltrate, including numerous histiocytes, plasma cells, lymphocytes and neutrophils. The left ureter also demonstrated severe acute and chronic inflammation with denuded surface urothelium. The findings in summary were diagnosed as acute and chronic pyelonephritis with serous atrophy of the kidney and extensive sinus replacement lipomatosis.
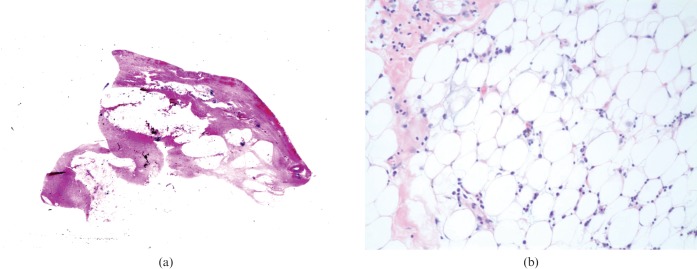
Figure 4.
Low-power photomicrograph (a, haematoxylin and eosin stain (H&E), ×1) shows lobules of fatty tissue interspersed with fibrous bands that encroach on markedly thin atrophic renal parenchyma. High-power photomicrograph (b, H&E stain, ×200) of a lobule of fatty tissue shows mature adipocytes with interspersed chronic inflammation composed of lymphocytes and plasma cells.
Discussion
Benign proliferation of fibrofatty tissue within the renal sinus may occur to varying degrees. Although renal sinus lipomatosis refers to a moderate increase in renal sinus fat, renal replacement lipomatosis refers to a rare and most extreme form of this spectrum that typically occurs unilaterally in which a greater proliferation of renal sinus fat is associated with adjacent renal atrophy such that the kidney appears to be replaced by fatty tissue [1]. Indeed, in its most extensive manifestation, the renal parenchyma undergoes total atrophy with complete fibrofatty replacement [2]. We have identified five previous reports in the English language literature of replacement lipomatosis demonstrated on MRI. Of these, four had associated renal or ureteral stone disease [3–6]; the remaining case occurred in the setting of renal tuberculosis [7].
Review of the literature identifies three possible mechanisms for the sequence of parenchymal atrophy and fibrofatty replacement: pressure atrophy of renal parenchyma by expanding renal sinus fat; invasion of the renal parenchyma by fat; and fatty replacement of the renal parenchyma following destruction and atrophy [8]. While the pathophysiology of this disease is not fully understood, the majority of the cases are associated with a constellation of calculus disease (particularly staghorn calculi), chronic inflammation and hydronephrosis. In fact, it has been suggested that renal calculi trigger a process of hydronephrosis and chronic inflammation that, in turn, results in varying degrees of parenchymal atrophy and sinus fibrofatty replacement [1].
When interpreting the MRI, it is important for the radiologist to be able to distinguish replacement lipomatosis from a fatty tumour such as an angiomyolipoma, lipoma or liposarcoma. Replacement lipomatosis is centred within the renal sinus without mass effect upon the renal collecting system. On the other hand, a neoplasm in this location may exert mass effect upon the renal collecting system and is more likely to extend into the renal sinus while arising from a location within the kidney or in an extrarenal location outside the renal sinus [1, 3, 9, 10]. In addition, associated renal atrophy, hydronephrosis and obstructing calculi are characteristic of a diagnosis of replacement lipomatosis and are less likely to be present in the setting of a fatty neoplasm [1, 10, 11]. Also, liposarcomas in particular may be characterised by the presence of internal thick soft-tissue strands or nodules that would not be expected in replacement lipomatosis [11]. Our case was typical of replacement lipomatosis based on the presence of associated renal atrophy and hydronephrosis, but was atypical because of the absence of renal calculus disease.
Xanthogranulomatous pyelonephritis is a benign disease of chronic renal inflammation that may also have overlapping imaging features with replacement lipomatosis. Like replacement lipomatosis, xanthogranulomatous pyelonephritis is associated with calculus disease and a non-functioning kidney. However, xanthogranulomatous pyelonephritis constitutes a distinct process in which lipid occurs intracellularly within the renal parenchyma via the infiltration of lipid-laden macrophages (inflammatory foam cells) [1, 2]. We do note that xanthogranulomatous pyelonephritis and replacement lipomatosis have been known to coexist [12].
In summary, we have presented a case of massive replacement lipomatosis depicted on MRI, with pathological confirmation. In this case, the MRI allowed for a pre-operative diagnosis of replacement lipomatosis with severe hydronephrosis, despite the somewhat atypical presentation without associated calculus. It is important to be aware of this entity when evaluating fatty lesions of the renal sinus and to understand the imaging features that may be used to distinguish this process from other entities of the renal sinus, including fatty tumours.
References
- 1.Subramanyam BR, Bosniak MA, Horii SC, Megibow AJ, Balthazar EJ. Replacement lipomatosis of the kidney: diagnosis by computed tomography and sonography. Radiology 1983;148:791–2 [DOI] [PubMed] [Google Scholar]
- 2.Ambos MA, Bosniak MA, Gordon R, Madayag MA. Replacement lipomatosis of the kidney. AJR Am J Roentgenol 1978;130:1087–91 [DOI] [PubMed] [Google Scholar]
- 3.Kantarci M, Onbas O, Bozkurt M, Alper F, Okur A. Renal replacement lipomatosis: MR findings in one case. Magn Reson Imaging 2004;22:275–9 [DOI] [PubMed] [Google Scholar]
- 4.Choyke PL, Kressel HY, Pollack HM, Arger PM, Axel L, Mamourian AC. Focal renal masses: magnetic resonance imaging. Radiology 1984;152:471–7 [DOI] [PubMed] [Google Scholar]
- 5.Kocaoglu M, Bozlar U, Sanal HT, Guvenc I. Replacement lipomatosis: CT and MRI findings of a rare renal mass. Br J Radiol 2007;80:e287–9 [DOI] [PubMed] [Google Scholar]
- 6.Kiris A, Kocakoc E, Poyraz AK, Dagli F, Boztosun Y. Xanthogranulomatous pyelonephritis with nephrocutanous fistula and coexisting renal replacement lipomatosis: the report of a rare case. Clin Imaging 2005;29:356–8 [DOI] [PubMed] [Google Scholar]
- 7.Casas JD, Cuadras P, Mariscal A, Domenech S. Replacement lipomatosis related to renal tuberculosis: imaging findings in one case. Eur Radiol 2002;12:810–13 [DOI] [PubMed] [Google Scholar]
- 8.Honda H, McGuire CW, Barloon TJ, Hashimoto K. Replacement lipomatosis of the kidney: CT features. J Comput Assist Tomogr 1990;14:229–31 [DOI] [PubMed] [Google Scholar]
- 9.Yagci C, Kosucu P, Yorubulut M, Akyar S. Renal replacement lipomatosis: ultrasonography and computed tomography findings. Eur Radiol 1999;9:1599–601 [DOI] [PubMed] [Google Scholar]
- 10.Rha SE, Byun JY, Jung SE, Oh SN, Choi YJ, Lee A, et al. The renal sinus: pathologic spectrum and multimodality imaging approach. Radiographics 2004;24 (Suppl 1):S117–31 [DOI] [PubMed] [Google Scholar]
- 11.Chang SD, Coakley FV, Goldstein RB. Case report: renal replacement lipomatosis associated with renal transplantation. Br J Radiol 2005;78:60–1 [DOI] [PubMed] [Google Scholar]
- 12.Prasad KK, Pandey R, Kathuria M, Pradhan PK. Co-existent massive renal replacement lipomatosis and xanthogranulomatous pyelonephritis: a case report. Indian J Pathol Microbiol 2003;46:674–5 [PubMed] [Google Scholar]