Abstract
Left ventricular aneurysms are uncommon complications of myocardial infarction. However, it is important to identify them because they are associated with increased morbidity and mortality. True aneurysms tend to be managed conservatively whereas false aneurysms, because of the risk of rupture, are usually treated with urgent surgery. Distinguishing these two subtypes is therefore critical and cardiovascular magnetic resonance (MR) is being used more frequently to characterise the type of aneurysm as well as to provide clear three-dimensional images of aneurysm morphology. We present a very rare case of a true and a false aneurysm of the left ventricle in the same patient. MR enabled accurate delineation of both aneurysms and the late gadolinium-enhancement images provided evidence confirming both true and false aneurysms to be present.
Case report
A 63-year-old female presented with a 2 day history of chest pain. She had experienced brief self-limiting episodes of palpitations associated with dizziness over the preceding month but had otherwise been fit and well. An electrocardiogram showed a regular broad complex tachycardia, consistent with ventricular tachycardia (VT). An attempt at chemical cardioversion with iv amiodarone was unsuccessful, but direct-current (DC) cardioversion reverted the patient to sinus rhythm. A portable chest radiograph showed no obvious abnormality. Transthoracic echocardiography showed an inferior wall left ventricular aneurysm with moderate mitral regurgitation.
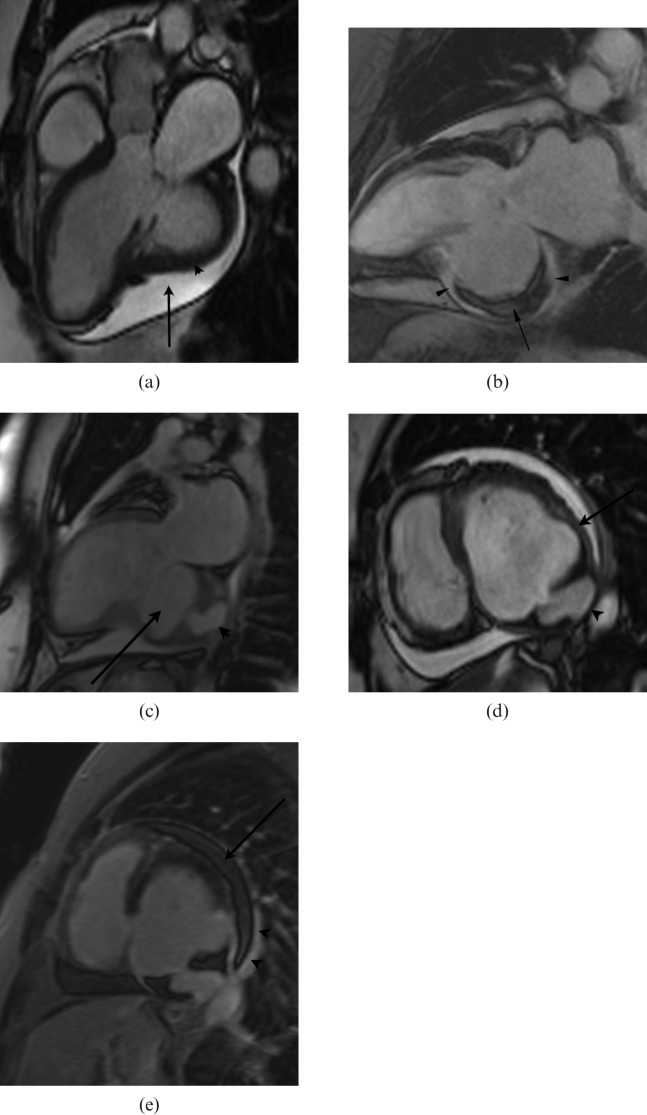
An adenosine stress cardiovascular magnetic resonance (MR) study was performed (Siemens Avanto 1.5 T, Erlangen, Germany) to look for an ischaemic substrate for VT and to better characterise the inferior wall aneurysm. This revealed no inducible perfusion defect but did demonstrate a large 6 cm wide-necked aneurysm arising from the base of the inferior and inferolateral wall of the left ventricle (LV) close to the mitral valve annulus (Figure 1a). The wall of this aneurysm demonstrated full-thickness late gadolinium enhancement (LGE) with associated mural thrombus (Figure 1b), while the adjacent myocardium in the rest of the inferior and inferolateral wall returned a normal nulled signal. The aneurysm was almost completely surrounded by pericardial fluid (Figure 1a). A further 3.5 cm narrow-necked aneurysm arose from the apex of this larger aneurysm (Figure 1c,d). This smaller aneurysm was adherent to pericardium. Full-thickness LGE was also seen throughout its wall. Further LGE was seen over the pericardial surface close to the smaller aneurysm (Figure 1e). The appearances were therefore those of a large true aneurysm of the inferior wall with an additional false aneurysm arising from its apex.
Figure 1.
(a) Three-chamber steady-state free precession (SSFP) image showing a large wide-necked aneurysm arising from the inferolateral wall of the left ventricle (LV) (arrowhead), surrounded by pericardial fluid (arrow). (b) Late gadolinium-enhancement (LGE) image in a two-chamber plane shows the large aneurysm extending from the proximal inferior wall of the LV with full-thickness LGE in its wall (arrowheads) and contained mural thrombus (arrow). (c) Low-resolution two-chamber SSFP scout image shows the large true aneurysm at the base of the inferior wall (arrow) and the additional small narrow-necked false aneurysm arising from its apex (arrowhead). (d) SSFP short-axis image at the base of the LV demonstrates the large true aneurysm of the inferior and inferolateral wall (arrow) and the smaller false aneurysm adherent to adjacent pericardium (arrowhead). (e) LGE image in short axis shows some enhancement of the pericardium in the region of the false aneurysm (arrowheads). The pericardial fluid is of low signal on this image (arrow).
The patient proceeded to surgery urgently given the presence of a false aneurysm. The MR findings were confirmed at surgery, with a large true aneurysm of the basal inferior wall and a small false aneurysm arising from its apex (Figure 2). There was pericardial adhesion to the false aneurysm but not the true aneurysm. The false aneurysm was opened and the site of rupture sutured and repaired. The true aneurysm was plicated and the mitral valve was replaced because of significant associated mitral regurgitation. The patient subsequently made an uneventful post-operative recovery.
Figure 2.
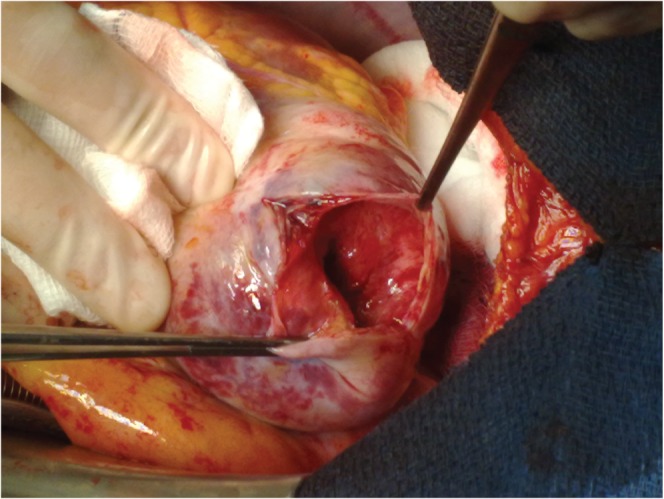
Intra-operative view confirming the presence of both true and false aneurysms. The false aneurysm has been opened to reveal the point of perforation from the wall of the true aneurysm.
Discussion
True and false LV aneurysms are both complications of myocardial infarction (MI). True aneurysms are more commonly found in the anteroapical wall and represent a bulging of the scarred myocardium, usually in the setting of a large infarct. They have a broad diameter, which is similar in size to the aneurysm neck. False aneurysms occur following contained myocardial rupture post MI. Usually, myocardial rupture produces haemopericardium, tamponade and death, but occasionally the rupture is contained by locally adherent pericardium to produce a cavity communicating with the LV cavity through the point of rupture and hence a false aneurysm. False aneurysms arise more commonly from the base of the inferior and inferolateral wall and usually have a relatively narrow neck compared with the dimension of the aneurysm sac [1, 2].
LGE is now accepted as a useful technique for identifying myocardial fibrosis, most commonly due to MI. This involves an inversion recovery MR sequence performed at 10–15 min post iv injection of gadolinium. Our protocol is to image at 15 min post iv administration of 0.15 mmol kg−1 of gadolinium dimeglumine (Multihance, Bracco s.p.a., Milan, Italy) using a combination of two-dimensional (2D) and 3D multislice sequences. On the images obtained, normal myocardium is nulled to produce a low signal while areas of fibrosis demonstrate significant increased signal owing to local gadolinium accumulation. Recently, LGE has been demonstrated to be a useful tool in the differentiation of true from false aneurysms [2]. Although both types of aneurysm show late enhancement in the wall of the aneurysm sac, enhancement of the pericardium has been shown more frequently in patients with false aneurysms and is thought to represent the effects of seepage of blood into the pericardial space at the time of rupture, with subsequent pericardial inflammation and pericardial fibrosis.
The identification of true and false LV aneurysms in the same patient is very rare [3, 4]. It can be conceived that contained rupture occurs in the early days post infarct and there is then subsequent bulging of the infarct tissue to produce an additional true aneurysm.
MR is an increasingly useful tool in the 3D characterisation of LV aneurysms and may be able to distinguish true from false aneurysms as shown in this case. The MR findings provided accurate information to guide subsequent surgical intervention.
References
- 1.Yeo TC, Malouf JF, Reeder GS, Jae KO. Clinical characteristics and outcome in post-infarction pseudoaneurysm. Am J Cardiol 1999;84:592–5 [DOI] [PubMed] [Google Scholar]
- 2.Konen E, Merchant N, Gutierrez C, Provost Y, Mickleborough L, Paul NS, et al. true vs false left ventricular aneurysm: differentiation with MR imaging: initial experience. Radiology 2005;236:65–70 [DOI] [PubMed] [Google Scholar]
- 3.Kumar Das A, Wilson GM, Furnary AP. Coincidence of true and false left ventricular aneurysm. Ann Thor Surg 1997;64:831–4 [DOI] [PubMed] [Google Scholar]
- 4.Oxorn DC, Morgan CD. Coexistent true and false left ventricular aneurysms. Eur J Cardiothorac Surg 2000;18:251. [DOI] [PubMed] [Google Scholar]