Abstract
Lymphocoele of the thoracic duct, alternatively referred to as thoracic duct cyst, is an uncommon abnormality that can present occasionally as a left supraclavicular fossa mass. Recognition of the origin of such a neck mass on imaging is crucial to avert unnecessary intervention. A case of such a mass is presented with discussion of the fascinating variable anatomy of the thoracic duct.
Lymphocoele of the thoracic duct, alternatively referred to as a thoracic duct cyst, is an uncommon abnormality that can present rarely as a left neck mass arising from the supraclavicular fossa. Recognition of the aetiology of such a neck mass on imaging is crucial to avert unnecessary intervention and, where surgical intervention is planned, to avoid both unexpected findings at surgical exploration and secondary complications. We present such a case of a cervical neck mass. We discuss the embryology and normal anatomy of the thoracic duct and the radiological diagnosis and management, including radiologically directed diagnostic intervention.
Case report
A 53-year-old Afro-Caribbean female presented to our ear, nose and throat clinic with a 4 month history of a painless, non-pulsatile lump in the left supraclavicular fossa. She had noticed it only incidentally and did not feel that it had increased in size over the 4 months. There was no history of any subjective neurological abnormality of the left upper limb. The patient was otherwise fit and well, was a non-smoker and consumed alcohol only very occasionally. There was no history of notable trauma in the past and no history of surgery. Examination identified a firm, non-tender mass in the medial left supraclavicular fossa. The remainder of the external examination of the neck was unremarkable and flexible nasoendoscopy was normal. Ultrasound assessment yielded a flowless non-pulsatile hypoechoic cystic mass in the left supraclavicular fossa, which was related to the distal subclavian and internal jugular veins. Radiologically, concern was raised over a cystic nerve sheath tumour arising from one of the trunks of the brachial plexus or the vagus nerve or a pseudoaneurysm of the left subclavian artery. As a result, immediate ultrasound-guided fine-needle aspiration (FNA) was not undertaken, but instead MRI of the neck and brachial plexus was performed (Figure 1). MRI confirmed a cystic mass in the left supraclavicular fossa, located at the confluence of the internal jugular vein and the subclavian vein. The mass was not associated with the brachial plexus or the carotid sheath. Repeat ultrasound assessment was performed with ultrasound-guided FNA. The aspirate was of milky consistency in keeping with chyle. The sample was sent for cytology and also biochemical analysis, including assays for triglycerides and chylomicrons. The imaging determined that the mass was of lymphatic origin and probably a lymphocoele of the thoracic duct. Cytology and biochemistry confirmed the contents as lymph. Prior to surgical follow-up, CT of the neck, chest and abdomen was performed to exclude other abnormalities of the thoracic duct course (Figure 2). This imaging revealed that the proximal part of the thoracic duct in the posterior mediastinum was also dilated. At follow-up, a decision for conservative management was reached.
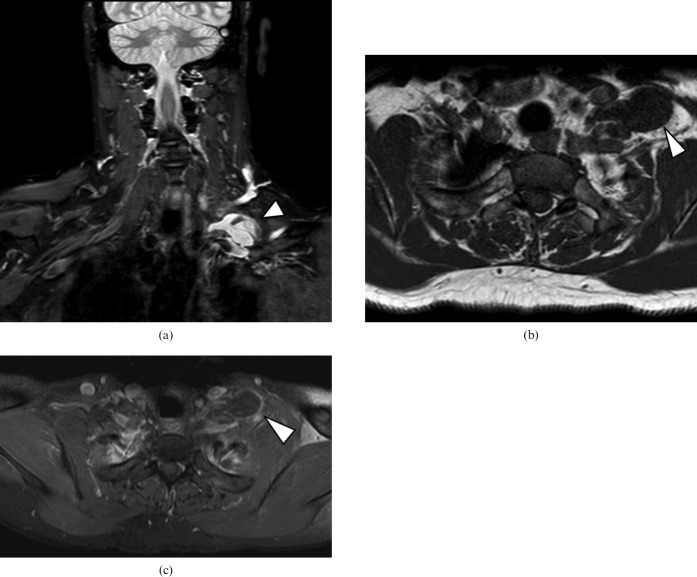
Figure 1.
(a) Coronal short tau inversion recovery sequence: a cystic lesion (arrowhead) is identified in the left supraclavicular fossa. (b) Axial unenhanced T1 weighted sequence shows a hypointense cyst (arrowhead) with a “pedicle” extending posterior to the internal jugular vein and anterior to the subclavian artery. (c) In the axial contrast-enhanced T1 weighted sequence with fat suppression the lesion has an absence of enhancement and a location consistent with a lymphocoele (arrowhead) of the thoracic duct termination.
Figure 2.

Axial contrast-enhanced CT image through the posterior mediastinum. The thoracic duct is dilated in the posterior mediastinum (arrow).
Discussion
Lymph is delivered to the venous circulation via the right and left cervical lymphovenous portals, which are located at or near the junctions of the internal jugular and subclavian veins where these veins converge to form the right and left brachiocephalic veins [1, 2]. On the right, three main lymph trunks, the (right) jugular trunk, the (right) subclavian trunk and the (right) bronchomediastinal trunk, converge at their venous junction. On the left, there are three similarly named trunks plus a fourth trunk, the largest, called the thoracic duct (Figure 3) [1, 2].
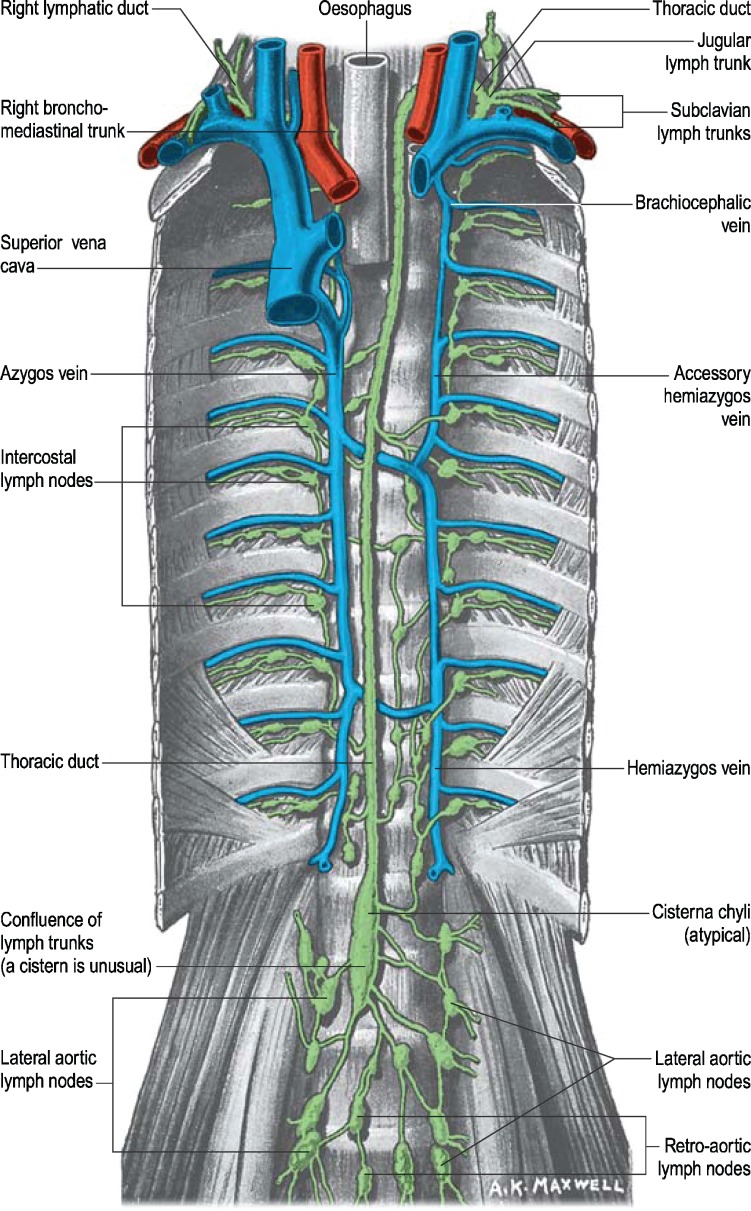
Figure 3.
Anatomical illustration of the origin, course and termination of the thoracic duct. (Reproduced with permission from Stranding S, Healy J, Johnson D, Williams A. The Mediastinum. In: Ellis H, editor. Gray's anatomy: the anatomical basis of clinical practice. Edinburgh, UK: Elsevier Churchill Livingstone, 2004: 985).
The thoracic duct, which is subject to considerable morphological variation throughout its course [1], drains lymph from most (though not all) of the subdiaphragmatic regions of the body. The abdominal confluence of lymph trunks, which gives rise to the caudal origin of the thoracic duct, may be a simple duct-like extension or may be duplicate, triplicate or plexiform. In a small proportion of people, it is a singular simple fusiform dilatation called the cysterna chyli. The abdominal confluence, or the true cysterna chyli when present, extends from the caudal beginning of the thoracic duct to the right of the first and second lumbar vertebrae, lying immediately to the right of the abdominal aorta [1, 2].
The thoracic duct terminates by descending anterior to the first part of the subclavian artery and draining into the junction of the left subclavian vein and the internal jugular vein [1, 2]. A valve at this site prevents reflux of blood into the duct. Morphological variability of the duct's termination includes drainage into either of the great veins near the junction or division into smaller vessels before terminating [1, 3, 4]. Kinnaert [3] reviewed dissections of the thoracic duct termination, giving an account of its marked morphological variability: an ampulla was observed at the extremity of the thoracic duct in 25% of the reviewed cases. Another variation was a localised bulging of the subclavian vein at the lymphovenous junction [1, 3].
Lymphocoeles or cysts of the terminal part of the thoracic duct are a rare entity compared with the more common thoracic duct cysts of the mediastinum. It is not until 1965 that a report of a left supraclavicular region thoracic duct cyst is identifiable in the literature [5].
Liu et al [6] studied the contrast-enhanced CT neck examinations of 301 patients and were able to identify 161 distal duct systems. They described three basic morphological appearances: simple tubular, flared dilatation and segmental fusiform dilatation. No frank cystic formation of the cervical thoracic duct was found; in one patient, the thoracic duct was dilated throughout both its mediastinal course and its cervical course [6], as in the present case.
Numerous theories have been suggested to explain the aetiology of lymphocoele of the terminal thoracic duct. Both congenital weakness in the thoracic duct wall and acquired degenerative process from inflammation have been proposed as causative mechanisms. Trauma has also been suggested as the underlying aetiology [7–9]. In the present case, no history of trauma was identified. It is worth noting that obstruction by ligation of the thoracic duct does not result in cystic dilatation [5, 7].
The clinical significance of a thoracic duct cyst lies in its misidentification as a pathological lesion at radiological assessment, which can ultimately lead to inappropriate management. Awareness of the anatomical course of the thoracic duct and of the existence of this morphological anomaly is therefore paramount. A number of important differential diagnoses warrant consideration, and these can be excluded by appropriate cross-sectional imaging and ultimately by ultrasound-guided FNA of the cyst. Exclusion of a cystic nodal metastasis of a supraclavicular or medial level 5B lymph node is foremost. Papillary carcinoma of the thyroid and squamous cell carcinoma of the aerodigestive tract are the most common causes of pathological cystic lymphadenopathy in the neck; ultrasound assessment of the thyroid at the time of FNA of the supraclavicular cyst should be undertaken to identify any potential thyroid aetiology. Infraclavicular tumours, particularly of pulmonary, abdominal or pelvic origin, also warrant exclusion as the primary source. Nerve sheath tumours arising from the lower carotid sheath or brachial plexus can demonstrate a significant cystic component. Pseudoaneurysms arising from the inferior part of the common carotid artery or from the subclavian artery also warrant consideration and exclusion, particularly prior to needle aspiration. Branchiogenic cysts and lymphatic vasoformative lesions are other considerations. Lymphomatous lymph nodes in the neck can demonstrate a pseudocystic appearance on ultrasound assessment, but their underlying lymphoproliferative process is revealed on CT or MRI.
Ultrasound-guided FNA can be extremely helpful. Lymph (or chyle) has a very distinct appearance on gross inspection, exhibiting a milky appearance. It also has a very unique composition and so aspirate should be sent for both cytological and biochemical analysis to consolidate the diagnosis. In lymph (or chyle), lymphocytes are the predominant cell type with T-lymphocytes making up the majority of the count [7, 8]. Occasional macrophages, neutrophils and epithelial cells may be present. The protein content of lymph is relatively high, particularly in relation to its albumin content. Most striking, however, is the high concentration of triglycerides (and chylomicrons), which makes biochemical analysis both essential and confirmatory [7, 8]. In this way, surgery and the potential complications thereof, such as a chylous fistula or leak, can be averted.
Given the rarity of these lesions, there is some contention as to the most appropriate mode of treatment. Unless the cyst is symptomatic or cosmetically displeasing to the patient, conservative management is generally advocated for lymphocoeles of the thoracic duct so as to avoid the potential complications outlined. Nevertheless, there are reports of surgical excision in the literature [5, 7–9].
Conclusion
Knowledge of the normal course of the thoracic duct, particularly in relation to its cervical course, and of the morphological variations that it can demonstrate, including the rare formation of a lymphocoele, is invaluable in distinguishing morphological anomalies from pathological lesions of the lower cervical region.
References
- 1.Stranding S, Healy J, Johnson D, Williams A. Cardiovascular: topography of lymph nodes and vessels. Ellis H, editor. Gray's anatomy: the anatomical basis of clinical practice. Edinburgh, UK: Elsevier Churchill Livingstone, 2004:1606–11 [Google Scholar]
- 2.Sinnatamby CS. Thorax. Last RJ, Sinnatamby CS. Last's Anatomy: regional and applied. Edinburgh, UK: Elsevier Churchill Livingstone, 1999:203–4 [Google Scholar]
- 3.Kinnaert P. Anatomical variations of the cervical portion of the thoracic duct in man. J Anat 1973;115:45–52 [PMC free article] [PubMed] [Google Scholar]
- 4.Langford RJ, Daudia AT, Malins TJ. A morphological study of the thoracic duct at the jugulosubclavian junction. J Craniomaxillofac Surg 1999;27:100–4 [DOI] [PubMed] [Google Scholar]
- 5.Kolbenstvedt A, Aanesen J. Cystic dilation of the thoracic duct presenting as a supraclavicular mass. Br J Radiol 1986;59:1228–9 [DOI] [PubMed] [Google Scholar]
- 6.Liu M, Branstetter BF, Whetstone J, Escott EJ. Normal CT appearance of the distal thoracic duct. AJR Am J Roentgenol 2006;187:1615–20 [DOI] [PubMed] [Google Scholar]
- 7.Brauchle RW, Risin SA, Ghorbani RP, Pereira KD. Cervical thoracic duct cysts. Arch Otolaryngol Head Neck Surg 2003;129:581–3 [DOI] [PubMed] [Google Scholar]
- 8.Mattila PS, Tarkkanen J, Mattila S. Thoracic duct cysts: a case report and review of 29 cases. Ann Otol Rhinol Laryngol 1999;108:505–8 [DOI] [PubMed] [Google Scholar]
- 9.Lecanu JB, Gallas D, Biacabe B, Bonfils P. Lymphocele of the thoracic duct presenting as a left supraclavicular mass: a case report and review of the literature. Auris Nasus Larynx 2001;28:275–7 [DOI] [PubMed] [Google Scholar]