Abstract
Objectives
The increasing use of CT scans in the paediatric population raises the question of a possible health impact of ionising radiation exposure associated with CT scans. The aim of this study was to describe the pattern of CT use in early childhood.
Methods
In 14 major French paediatric radiology departments, children undergoing at least 1 CT scan before age 5, between 2000 and 2006, were included. For each examination, absorbed organ doses were calculated.
Results
43% of the 27 362 children in the cohort were aged less than 1 year during their first exposure, with 9% being aged less than 1 month. The mean number of examinations per child was 1.6 (range 1–43). The examinations included: head in 63% of the cases, chest in 21%, abdomen and pelvis in 8% and others in 8%. Brain and eye lenses received the highest cumulative doses from head examinations, with mean organ dose values of 22 mGy (maximum 1107 mGy) and 26 mGy (maximum 1392 mGy), respectively. The mean cumulative effective dose was 3.2 mSv (range 0.1–189 mSv).
Conclusion
CT scan exposure in childhood is responsible for relatively high doses to radiosensitive organs. The rather large dose range according to the protocols used requires their optimisation. The cohort follow-up will study the risk of long-term radiation-induced cancer.
Exposure for medical purposes is the main source of artificial radiation. In France, it represents 40% of the annual exposure of the whole population [1]. These exposures are mostly in relation to radiodiagnosis, which is associated with low levels of ionising radiation (IR). Previously, it has been observed that pre-natal and childhood exposure to X-rays was associated with an increased risk of cancer [2-4]; however, this was not confirmed by a review based on more recent studies published since 1990 [5]. The doses that used to be involved in pre-natal and post-natal diagnostic exposures in the past were much higher than those reported nowadays, and no evidence of an increased risk of leukaemia has been observed. However, some specific procedures, such as CT, are associated with much higher radiation doses than conventional radiodiagnosis: CT accounts for only 5% of all X-ray examinations but represents between 40% and 67% of the total medical dose received by the population [6]. Over the last 20 years the ease and speed of image acquisition linked to technological developments has encouraged the proliferation of procedures and has led to increased doses to patients. These trends are also observed in paediatric diagnostic imaging, leading to an increase in the use of CT and, therefore, an increase in the level of exposure to IR in children. About 11% of CT scans are carried out in the paediatric population [7]. Assessment of cancer risk after childhood radiation exposure remains a concern regardless of the radioprotection used for children. Children actually present an increased radiosensitivity of certain tissues compared with that of adults, which, combined with a long life expectancy, could allow cancer to develop. A lack of adjustment of specific technical parameters during imaging has also been noted.
The objective of this study was to build a cohort of children who attended the major French radiology departments very early in life, in order to describe the pattern of CT scan use in early childhood and to estimate doses associated with these examinations.
Material and methods
Study population
A retrospective cohort study on patients subjected to CT scans in 14 major paediatric radiology departments in France was formed in collaboration with the French Society of Paediatric and Pre-natal Radiology. The centres involved were: Angers, Bordeaux, Marseille, Montpellier, Nantes, Paris (centres Trousseau, Béclère, Bicêtre, Necker, Saint Vincent de Paul, R. Debré, L. Mourier, Jean Verdier) and Tours. All are university hospitals. Children who were less than 5 years old at the first examination between 1 January 2000 and 31 December 2006 were eligible. Patients who were permanent residents in France at the first examination were included.
Information collected
Referral criteria for the examination and radiological diagnosis were not recorded in the hospitals' electronic files. However, we were able to flag patients with a diagnosis of cancer or leukaemia through the French paediatric cancer registries [Registre des Tumeurs Solides de l'Enfant (RTSE) and Registre National des Hemopathies de l'Enfant (RNHE)]. The RNHE and RTSE have recorded all childhood (i.e. under 15 years old at diagnosis) cases of leukaemia and cancer in France since 1990 and 2000, respectively. The RNHE and the RTSE have previously been used as a study base for several large-scale childhood cancer investigations [8-10].
Electronic files concerning all the CT examinations conducted in these hospitals during the study period were obtained and the following information was retrieved: first name, surname, hospital identification number, date of birth, postal code (based on home address), date of examination, anatomical region of the body examined, use – or not – of a contrast agent and, for part of the cohort, identification of the medical department requesting the CT scan. Anatomical areas of focus were the following: head, neck, chest, abdomen, pelvis, extremities (feet, knees, hands and elbows) and multiple areas.
Exposure assessment
To estimate the radiation exposure of the children included in the cohort, we calculated organ absorbed doses. The organ dose represents a rather appropriate dosimetric indicator to express the energy deposited in a specific organ but cannot be directly measured in patients. It needs to be assessed using either physical or mathematical phantoms that simulate the process of depositing energy at a given point or in a given organ. Monte Carlo simulation programs have been developed to produce dose conversion coefficients translating a dosimetric quantity such as the volume CT dose index measured under well-defined conditions for a given CT machine model into organ absorbed doses. The software CT-Expo [11], which allows organ doses to be calculated for two categories of children (babies and young children), was used to estimate organ doses for each exposed child according to several technical parameters associated with the examination. The two categories of age we chose were: below 1 year old and above 1 year old. When the protocol was different according to age within one of our two age groups (<1 year and ≥1 year), we applied the protocol linked to the age under consideration even if the size of the phantom did not change. The parameters, which include the anatomical region of the body that was exposed, tube voltage (in kilovolts), current (in milliamperes), slice thickness and type of CT machine, were not individually available for the majority of the patients because of the delayed use of electronic parameter storage in France. Dose reconstructions were then based on the specific protocols of each of the radiology departments taking into account anatomical area, number of series, age and type of scanner. The protocols were obtained for several anatomical areas and not for various clinical diagnoses. However, we could not exclude that the parameters could have been modified for a specific indication in some cases, independently of the protocol. These protocols enabled us to estimate radiation doses for a specific type of examination, e.g. head, neck, chest, abdomen and pelvis. It also allowed us to estimate the effective dose, which is a dosimetric indicator that represents the overall health detriment to the whole body in adults but needs to be considered with caution in the paediatric field. When the protocol was not available, because of lack of storage of the information after a change of the CT machine, a reconstruction of that protocol was carried out for the main types of examinations and categories of age using a sample of images from the time period and the type of machine. In all, 22 CT machines were used over the whole period studied, with 10 single-detector CT (SDCT) and 12 multidetector CT (MDCT) machines. MDCT machines included 4, 16 and 64 slices in 3, 7 and 2 cases, respectively. Globally, 18 protocols were available and 4 needed to be reconstructed. During the study period, modulation of current was used in only one centre for examinations outside the head. We, therefore, included only those patients who had undergone head examinations from this centre, because of the difficulty in reconstructing doses from the medical protocol in examinations using current modulation. In the case of an examination with unspecified anatomical areas and/or with no associated medical protocol, the exposure assessment could not be carried out and cumulative radiation doses could therefore not be calculated. These patients were thus excluded from the dosimetric analysis. The patients in whom the anatomical area scanned was the extremities (feet, knees, hands and elbows) were considered as non-exposed.
Statistical analysis
Baseline characteristics were computed for all children included in the study. The median effective and organ doses, according to the exposed anatomical area, were calculated for two age groups (0–1 year and 1–5 years) taking into account the type of CT machine, i.e. SDCT or MDCT. Procedural frequencies were calculated for the whole study population over the 9 year follow-up period, with cumulative effective and organ doses being estimated until 30 December 2008. Comparisons by category of referral (referral for cancer diagnosis and follow-up or referral for non-cancer disease) were calculated with t-tests for quantitative variables and with χ2 tests for categorical variables.
Ethics approval
Use of the computer database containing all of the collected information was agreed by the Commission Nationale Informatique et Libertés (CNIL), which ensures that data privacy laws are enforced in France.
Results
Study population
After exclusion of 863 patients who were not permanent residents in France at the time of the study, the cohort included 27 362 patients. On average, 3900 patients entered the cohort per year. The mean age of the patients at inclusion was 21 months (Table 1). Almost half of the population, i.e. 11 857 (43%) children, entered the cohort at less than 12 months old; of these, 2437 (9%) were less than 1 month old. The majority of patients were boys (58%), but there were no significant differences between girls and boys in mean inclusion age or in the average number of examinations. The follow-up was performed until 31 December 2008.
Table 1. Baseline characteristics of participants in the Paediatric Scanner Study, France, 2000–2006.
| Characteristic | Total subjects, n=27362 (%) | Non-cancer referrals, n=26189 (%) | Cancer referrals, n=1173 (%) |
| All subjects | 100 | 96 | 4 |
| Sex | |||
| Boys | 58 | 58 | 55 |
| Girls | 42 | 42 | 45 |
| Age at first examination | |||
| Mean (SD) (months) | 21 (18) | 21 (18) | 28 (17) |
| <1 month | 9 | 9 | 3 |
| 1 month–1 year | 34 | 35 | 21 |
| 1–2 years | 18 | 18 | 21 |
| ≤3 years | 14 | 13 | 19 |
| ≤4 years | 13 | 13 | 19 |
| ≤5 years | 12 | 12 | 17 |
| Number of examinations per patient | |||
| Total | 44417 | 40134 | 4283 |
| Mean (SD) | 1.6 (1.7) | 1.5 (1.4) | 3.7 (3.9) |
| 1 | 72 | 74 | 31 |
| 2 | 16 | 15 | 22 |
| 3 | 5 | 5 | 14 |
| 3+ | 7 | 6 | 33 |
| Anatomical area explored | |||
| Head | 63.0 | 65.7 | 37.4 |
| Neck | 2.1 | 2.2 | 1.1 |
| Chest | 21.0 | 20.8 | 22.3 |
| Abdomen and pelvis | 7.5 | 6.5 | 17.4 |
| Extremities | 0.2 | 0.2 | 0.0 |
| Multiple areas | 3.7 | 2.3 | 17.6 |
| Unknown areas | 1.9 | 1.7 | 3.6 |
| Other | 0.6 | 0.6 | 0.6 |
Referral for cancer diagnosis or follow-up accounted for 1173 patients (4%) in the cohort. A comparison of the characteristics of the cancer cases with the non-cancer cases is shown in Table 1. On average, patients with cancer had more examinations than those without malignant disease (p<0.0001).
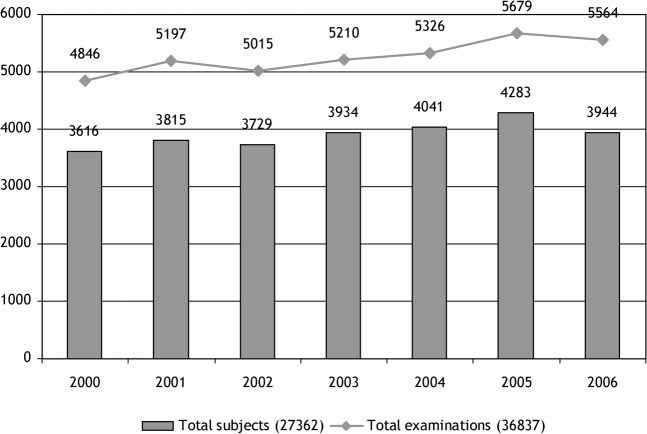
Exposure
CT scans were performed in the 14 radiology departments that were included in the study (11 paediatric units and 3 adult units with a large number of examinations in children), with various models of CT machines including 10 SDCT and 12 MDCT machines. A total of 44 417 CT examinations were identified, with a mean of 1.6 procedures per person (range 1–43) during the whole period. Even though the number of children included in the cohort remained approximately the same each year, the number of CT scans performed increased significantly over the study period, rising from 4846 in 2000 to 5564 in 2006 (Figure 1). Most of the patients had only 1 recorded examination (n=19 806, 72%). A further 4228 (16%) patients had 2; 1453 (5%) had 3; and 1875 (7%) had more than 3 CT scan examinations (Table 1). The mean number of examinations per child decreased significantly with increasing age at the first examination, ranging from 1.7 during the first month of life to 1.5 for the 4–5 years category. The most frequent anatomical area explored was the head, accounting for 63% of all the examinations, with a significantly higher frequency in the non-cancer cases (66%) than in the cancer cases (37%) (p<0.0001). The number of chest, abdomen or pelvis, and multiple area (referring to examinations performed at several anatomical areas at the same time) CT scans were significantly increased in cancer cases compared with non-cancer cases (p<0.0001). Unspecified anatomical area accounted for 2% of the total of the examinations.
Figure 1.
Yearly inclusion of patients and number of examinations recorded in this year over the period 2000–2006.
The median effective and organ doses per examination according to the anatomical area explored, the type of CT machine (SDCT vs MDCT), the radiology department protocol and the age of the patient (<1 year or ≥1 year) are reported in Tables 2 and 3, respectively. The median observed dose values did not differ significantly according to the category of age of the children, except in cases of middle ear examination, which were associated with decreasing dose values as the age increased. However, MDCT examinations were associated with slightly decreased doses, except in the case of head examination.
Table 2. Median effective dose values per examination, according to the age at exposure and type of CT machine.
| Explored anatomical area | Median effective dose in mSv (min–max) by age at exposure |
|||
| < 1 year |
1–5 years |
|||
| SDCT | MDCT | SDCT | MDCT | |
| Head | 0.9 (0.4–1.6) | 1.4 (0.6–3.2) | 0.8 (0.3–2.1) | 1.4 (0.7–2.7) |
| Middle ear | 1.3 (0.4–2.1) | 2.0 (0.2–7.1) | 0.4 (0.2–1.1) | 0.5 (0.1–2.6) |
| Chest | 3.6 (0.4–11.5) | 2.7 (1.0–6.8) | 2.5 (0.2–8.3) | 1.7 (0.7–5.1) |
| Abdomen and Pelvis | 10.0 (4.4–21.5) | 5.7 (2.5–10.6) | 9.1 (3.3–19.6) | 6.6 (1.8–18.1) |
MDCT, multidetector CT; SDCT, single-detector CT.
Table 3. Median organ dose values per examination, according to the age at exposure and type of CT machine.
| Explored anatomical area | Median organ doses in mGy (min–max) by age at exposure |
|||
| < 1 year |
1–5 years |
|||
| SDCT | MDCT | SDCT | MDCT | |
| Head | ||||
| Brain | 14 (6–28) | 23 (8–55) | 14 (6–40) | 26 (11–47) |
| Eye Lenses | 21 (0.4–32) | 23 (1–73) | 24 (0.6–50) | 37 (1–60) |
| Bone marrow | 4 (1–7) | 6 (3–15) | 2 (1–6) | 4 (2–7) |
| Middle ear | ||||
| Brain | 13 (3–21) | 17 (2–55) | 5 (2–14) | 6 (1–37) |
| Eye Lenses | 49 (17–96) | 55 (9–206) | 45 (18–127) | 43 (8–195) |
| Bone marrow | 6 (2–10) | 9 (1–33) | 2 (1–5) | 2 (0.4–10) |
| Chest | ||||
| Thyroid | 10 (1–31) | 7 (3–18) | 8 (1–25) | 5 (2–15) |
| Oesophagus | 9 (1–27) | 6 (2–15) | 6 (1–21) | 4 (2–12) |
| Lungs | 10 (1–30) | 6 (3–16) | 7 (1–22) | 5 (2–13) |
| Breast | 10 (1–30) | 6 (3–16) | 8 (1–25) | 5 (2–15) |
| Thymus | 10 (1–30) | 6 (3–17) | 7 (1–22) | 5 (2 –13) |
| Bone marrow | 2 (0.3–7) | 2 (1–4) | 1 (0.1–3) | 1 (0.3–2) |
| Abdomen and pelvis | ||||
| Liver | 15 (6–29) | 7 (3–13) | 13 (5–25) | 9 (2–25) |
| Stomach | 15 (7–30) | 7 (3–13) | 16 (6–31) | 10 (3–27) |
| Colon | 14 (6–28) | 7 (3–13) | 16 (6–32) | 10 (3–27) |
| Small bowel | 16 (7–31) | 8 (4–13) | 17 (6–33) | 11 (3–28) |
| Testicles | 7 (4–16) | 7 (3–13) | 12 (4–23) | 10 (3–28) |
| Ovaries | 16 (7–31) | 8 (4–14) | 15 (6–30) | 9 (3–25) |
MDCT, multidetector CT; SDCT, single-detector CT.
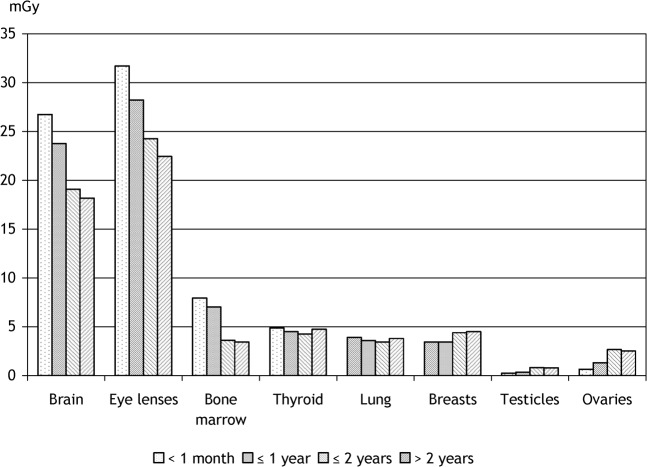
Cumulative dose estimation could be assessed for 87% (23 894 children) of the whole cohort. The mean cumulative effective dose per child was 3.2 mSv, ranging from 0 mSv to 189 mSv (Table 4). The mean value was significantly higher in the cancer group than in the non-cancer group: 11.9 mSv and 3.2 mSv, respectively. The median and mean cumulative organ doses are reported in Table 4. Taking into account the distribution of anatomical areas studied, which were mostly head CT scans, the median cumulative organ doses were relatively high for head organs, but rather low for chest, abdomen and pelvis radiosensitive organs. Maximum values remained high, because a small proportion of the children were subjected to more than 10 CT scans. The mean cumulative dose by age at the first exposure decreased with increasing age at exposure for brain, eye lenses and bone marrow (Figure 2), but increased with increasing age at exposure for testicles and ovaries.
Table 4. Cumulative effective and organ dose values per child.
| Mean | Median | 1st and 3rd quartiles | Min–Max | |
| Effective dose (mSv) | 3.2 | 1.6 | 0.8–3.1 | 0.1–189 |
| Organ dose (mGy) | ||||
| Brain | 22 | 15 | 1–30 | 0–1107 |
| Eye lenses | 26 | 15 | 1–34 | 0–1392 |
| Bone marrow | 5 | 4 | 2–6 | 0–161 |
| Thyroid | 4 | 1 | 1–3 | 0–287 |
| Lung | 3 | 0.4 | 0.2–2 | 0–250 |
| Breasts (girls only) | 4 | 0.3 | 0.1–2 | 0–183 |
| Colon | 2 | 0.006 | 0–0.2 | 0–281 |
| Testicles | 0.6 | 0.0002 | 0–0.004 | 0–79 |
| Ovaries | 2 | 0.007 | 0.002–0.1 | 0–291 |
The cumulative effective dose was calculated only for the 23 894 children who had an individual dosimetric estimation.
Figure 2.
Mean cumulated organ dose by age at first exposure.
Discussion
Our study allowed us to characterise the radiation exposure linked to the CT scan procedure in early infancy in a large population of patients. This is one of the few studies focusing on the distribution of CT scan procedures in a very young population [12,13]. Even though IR is usually carefully used in childhood, we observed that the CT scan procedure is likely to be used in very young children, since near half of our population was less than 1 year old at the time of the first examination, with about 10% aged younger than 1 month. We observed an increase in the number of CT scans performed over the study period, despite the number of children included in the study remaining approximately the same each year. The observed increasing use of CT, particularly for the youngest children, is surprising because of the advised switch from CT scan to MRI in routine practice [14]. This may be related to several factors: the limited number of MRI units in France compared with other European countries and North America, especially in emergency suites, and the need for sedation in young children for MRI, whereas the very short CT acquisition time (mainly with MDCT) allows examinations to be performed without any sedation procedure.
Organ doses were calculated in our study and could be compared with literature values, or measured with the help of anthropomorphic or cylindrical phantoms. Few paediatric values of organ doses are available [6,15-17,35] and concern mostly optimisation efforts [6,18-21,36]. The CT-Expo software allowed us to calculate doses for the paediatric population. The use of this software has been previously validated [22,23]. One limit of the study in dose estimation is the fact that CT-Expo software has only two sizes of phantoms to calculate organ doses. Indeed, the software uses a baby phantom of 7 weeks old and a child phantom of 5–7 years old. The uncertainties around the dose increased for children whose height increasingly differed from that of the phantom used, resulting in underestimations or overestimations for older and younger children, respectively. The estimation of doses were based on technical parameters extracted from the radiology department protocol and on the type of CT machine. Individual technical parameters, such as tube voltage or current, could not be extracted individually for each child, but comparison of a sample of individual data with technical parameters of the protocols showed a good agreement between the two approaches (data not shown). Taking into account the modulation of current would have made the reconstruction of doses from the medical protocol difficult. In our study, this point has not been a source of difficulty because only one centre used this technique for dose optimisation for CT scans not including head CT scans. In this centre, only those children who had examinations of the head—without modulation of current—were included in the study. For the head procedure, which was carried out in 63% of cases in our population, the median cerebral dose ranged from 14 mGy to 26 mGy with a wide range of doses (6–55 mGy) according to the type of CT machine and age category. These values are in the range of those described in previous studies [16,24]. The eye lens is also largely affected by CT scan, with a median lens dose ranging from 21 mGy to 37 mGy, which is either greater than previously reported [15] or in the range of other studies [17,24]. However, the highest doses received by the eye lens were observed in cases of middle ear examination, with a median dose ranging from 45 mGy to 55 mGy. According to the literature, eye lens doses vary from 10 mGy to 60 mGy in this type of exposure [6,25-27]. Median doses to the red bone marrow, which is exposed in head and chest examinations, ranged from 2 mGy to 6 mGy in head CT scans and from 1 mGy to 2 mGy in chest CT scans. These doses were similar to the doses reported elsewhere [15,24]. Considering chest, abdominal and pelvis examinations, median doses to the breast, lungs and gonads were in the range of those reported in the literature [15,24,28,29], with, as stated above, a large variation in dose according to the protocol. Effective doses were also calculated in our study in order to give a single dose value associated with an examination. However, it should kept in mind that the application of the underlying risk coefficients (averaged over several populations, both genders and all ages) to calculate this quantity is, in principle, inappropriate in the paediatric population. However, it is the only one that could be used when a single quantity is required to express a risk-related dose value. Specific values of doses for babies could be calculated in our study, taking into account specific radiological protocols for this age range. Comparing our results with other studies remains difficult because of the few reports concerning dose estimations for neonates or babies [30]. We observed that, as a consequence of the large difference in height and weight between the ages of 0 and 5 years, organ doses were usually higher in babies than those calculated in older age groups, except in the case of head examinations. This latter observation is consistent with the rather large volume of the head in early infancy.
The observed variability in doses for the same age category remains of concern. CT model and scan parameters used in the medical protocol were the two main reasons for this variability. An almost twofold difference in dose values has been observed among MDCT models of scanners after normalising technical parameters [24]. The discrepancy between technical protocols appeared to be linked both to the radioprotection awareness of the radiologist, as shown by several studies on dose reduction by optimisation [18-21], and to the referral diagnosis. The wide range of doses linked to the lack of protocol optimisation should no longer be observed. Indeed, French recommendations concerning dose reference levels in paediatric radiology, first published in 2005 [31], were updated in 2009 [14], and radiologists should have been applying them before the end of 2010.
The strength of our study was to calculate the cumulative organ and effective doses per child during the maximum 9 year follow-up of the cohort. All the examinations concerning one child were summed, despite some of the examinations being performed in several of the study hospitals. Although the vast majority of children were exposed to only one CT scan, about 7% were exposed to more than three CT scans. However, the total exposure of the children may have been underestimated because of possible examinations performed outside the participating hospitals' radiology departments. The mean cumulative effective dose was 3.2 mSv, ranging from 0.1 mSv to 189 mSv. The very high upper limit of cumulative doses was linked mainly to the number of CT scans performed per child. Indeed, a few of the children were subjected to a total of more than 30 CT scans. The highest mean cumulative organ doses were observed for brain and eye lens, 22 mGy and 26 mGy, respectively, as a result of the frequency of repeated head scans in our study. It must be noted that some children presented cumulative brain or eye lens doses even greater than 1 Gy. If the total organ doses for chest, abdomen and pelvis were rather high for one child, the small number of such procedures in our study decreased the mean value of the cohort cumulative dose. The mean cumulative doses reported in our study could not be compared with literature values because the few described surveys of paediatric patients subjected to CT scans concerned only those patients with specific diseases, such as cystic fibrosis [32] or hydrocephalus [33].
The levels of cumulative organ doses reported in our study raise concerns about the possible detriment to the health of children caused by radiation exposure. Evaluation of cancer risk after CT scan exposure in childhood has previously been done according to established risk models [34]. No epidemiological study concerning the risk of cancer following CT exposure in childhood has been published yet, but several national studies are ongoing or planned. In France, this study is the first to focus on this subject. All the major paediatric radiology departments were included in this study, with five additional departments to be included in the future. This allowed us to cover all the regions of the country and to describe the French paediatric radiology pattern of use. The next step will be to assess the risk of cancer or leukaemia following IR exposure linked to CT scans in our cohort. For this purpose, the follow-up will concern only those children exposed to CT scans for a non-cancer referral diagnosis. Indeed, patients exposed to CT scans because of a malignant disease diagnosis or follow-up should be excluded from the analysis because they are known to be at greater risk of a second cancer, owing to a specific susceptibility or to the treatment of the first malignancy. Patients with CT examination of the extremities, i.e. feet, knees, hands and elbows, should not be excluded from the cohort because they would constitute a reference group within the cohort, allowing us to compare non-exposed and exposed patients. The choice of this reference group will enable increased comparability between these two groups for the underlying disease. Follow-up of the health status of the children in the cohort will be assessed in the future. Because of the lack of a national adult cancer registry, we focused our study on very young exposed children in order to follow them on data incidence for at least 10 years through the paediatric cancer registries. Furthermore, very young children are known to have an increased sensitivity to radiation compared with adults and have a long life expectancy, which could allow cancer to develop. The follow-up of the cohort when they are adults will also be done, but only through mortality follow-up, pending the establishment of an adult nationwide cancer registry. A planned joint analysis of our study with other European transnational cohorts will increase the statistical power of the study.
In conclusion, this study allows us to characterise the radiation exposure of young children exposed to CT scans. Relatively high observed organ doses raise the question of whether the benefit–risk ratio of diagnostic CT examinations is being carefully estimated. Optimisation of the procedures should also be considered, taking into account the wide range of observed doses. Long follow-up of this exposed population will permit the study of the risk of long-term radiation-induced cancer.
Acknowledgments
This study has been carried out with the help of the Société Francophone d'Imagerie Pédiatrique et Prénatale and the participation of the following radiologists and paediatric radiology departments: Prof. C Adamsbaum (Hôpital Saint-Vincent de Paul, Paris), Prof. F Brunelle (CHU Necker-Enfants-Malades, Paris), Prof. J-F Chateil (CHU Pellegrin, Bordeaux), Prof. Dion (CHU Louis Mourier, Colombes), Prof. H Ducou Le Pointe (CHU Armand Trousseau, Paris), Dr S Franchi (CHU de Bicêtre, Le Kremlin-Bicêtre), Prof. Musset (CHU Béclère, Clamart), Dr Le François (CHU de Nantes, Nantes), Dr Loisel (CHU d'Angers, Angers), Prof. D Pariente (CHU de Bicêtre, Le Kremlin-Bicêtre), Prof. Petit (CHU Marseille, Marseille), Dr M Saguintaah (CHU Arnaud de Villeneuve, Montpellier), Prof. G Sebag (CHU Robert Debré, Paris), Prof. Sellier (CHU Jean Verdier, Bondy), Prof. D Sirinelli (CHU Clocheville, Tours). We also acknowledge the French paediatric registries: Registre des Tumeurs Solides de l'Enfant (RTSE) and Registre National des Hemopathies de l'Enfant (RNHE). This study was financially supported by grants from the Ligue Contre le Cancer.
References
- 1.Billon S, Morin A, Caer S, Baysson H, Gambard JP, Backe JC, et al. French population exposure to radon, terrestrial gamma and cosmic rays. Radiat Prot Dosimetry 2005;113:314–20 [DOI] [PubMed] [Google Scholar]
- 2.Bithell JF, Stewart AM. Pre-natal irradiation and childhood malignancy: a review of British data from the Oxford Survey. Br J Cancer 1975;31:271–87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Boice JD, Jr, Morin MM, Glass AG, Friedman GD, Stovall M, Hoover RN, et al. Diagnostic X-ray procedures and risk of leukemia, lymphoma, and multiple myeloma. JAMA 1991;265:1290–4 [PubMed] [Google Scholar]
- 4.Doody MM, Lonstein JE, Stovall M, Hacker DG, Luckyanov N, Land CE. Breast cancer mortality following diagnostic X-rays: findings from the US Scoliosis cohort study. Spine 2000;25:2052–63 [DOI] [PubMed] [Google Scholar]
- 5.Schulze-Rath R, Hammer GP, Blettner M. Are pre- or postnatal diagnostic X-rays a risk factor for childhood cancer? A systematic review. Radiat Environ Biophys 2008;47:301–12 [DOI] [PubMed] [Google Scholar]
- 6.UNSCEAR 2000. The United Nations Scientific Committee on the Effects of Atomic Radiation. Health Phys 2000;79:314. [PubMed] [Google Scholar]
- 7.Mettler FA, Jr, Wiest PW, Locken JA, Kelsey CA. CT scanning: patterns of use and dose. J Radiol Prot 2000;20:353–9 [DOI] [PubMed] [Google Scholar]
- 8.Rudant J, Menegaux F, Leverger G, Baruchel A, Nelken B, Bertrand Y, et al. Household exposure to pesticides and risk of childhood hematopoietic malignancies: The ESCALE study (SFCE). Environ Health Pers pect 2007;115:1787–93 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Benhammou V, Warszawski J, Bellec S, Doz F, Andre N, Lacour B, et al. Incidence of cancer in children perinatally exposed to nucleoside reverse transcriptase inhibitors. Aids 2008;22:2165–77 [DOI] [PubMed] [Google Scholar]
- 10.Brosselin P, Rudant J, Orsi L, Leverger G, Baruchel A, Bertrand Y, et al. Acute childhood leukaemia and residence next to petrol stations and automotive repair garages: the ESCALE study (SFCE). Occup Environ Med 2009;66:598–606 [DOI] [PubMed] [Google Scholar]
- 11.Stamm G, Nagel HD. CT-expo: a novel program for dose evaluation in CT. [In German.] Rofo 2002;174:1570–6 [DOI] [PubMed] [Google Scholar]
- 12.Galanski M, Nagel HD, Stamm G. Results of a federation inquiry 2005/2006: pediatric CT X-ray practice in Germany. [In German.] Rofo 2007;179:1110–11 [DOI] [PubMed] [Google Scholar]
- 13.Verdun FR, Gutierrez D, Vader JP, Aroua A, Alamo-Maestre LT, Bochud F, et al. CT radiation dose in children: a survey to establish age-based diagnostic reference levels in Switzerland. Eur Radiol 2008;18:1980–6 [DOI] [PubMed] [Google Scholar]
- 14.Société Française de Radiologie. Guide pratique à l'usage des médecins radiologues pour l'évaluation de leurs pratiques professionnelles. Paris: Société Française de Radiologie, 2009 [Google Scholar]
- 15.Fearon T, Vucich J. Normalized pediatric organ-absorbed doses from CT examinations. AJR Am J Roentgenol 1987;148:171–4 [DOI] [PubMed] [Google Scholar]
- 16.Colang JE, Killion JB, Vano E. Patient dose from CT: a literature review. Radiol Technol 2007;79:17–26 [PubMed] [Google Scholar]
- 17.Rybka K, Staniszewska AM, Bieganski T. Low-dose protocol for head CT in monitoring hydrocephalus in children. Med Sci Monit 2007;13 (Suppl. 1):147–51 [PubMed] [Google Scholar]
- 18.Chan CY, Wong YC, Chau LF, Yu SK, Lau PC. Radiation dose reduction in paediatric cranial CT. Pediatr Radiol 1999;29:770–5 [DOI] [PubMed] [Google Scholar]
- 19.Wong ET, Yu SK, Lai M, Wong YC, Lau PC. MAPD: an objective way to select mAs for paediatric brain CT. Br J Radiol 2001;74:932–7 [DOI] [PubMed] [Google Scholar]
- 20.Mulkens TH, Broers C, Fieuws S, Termote JL, Bellnick P. Comparison of effective doses for low-dose MDCT and radiographic examination of sinuses in children. AJR Am J Roentgenol 2005;184:1611–18 [DOI] [PubMed] [Google Scholar]
- 21.Udayasankar UK, Braithwaite K, Arvaniti M, Tudorascu D, Small WC, Little S, et al. Low-dose nonenhanced head CT protocol for follow-up evaluation of children with ventriculoperitoneal shunt: reduction of radiation and effect on image quality. AJNR Am J Neuroradiol 2008;29:802–6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zankl M, Drexler G. An analysis of the equivalent dose calculation for the remainder tissues. Health Phys 1995;69:346–55 [DOI] [PubMed] [Google Scholar]
- 23.Brix G, Lechel U, Veit R, Truckenbrodt R, Stamm G, Coppenrath EM, et al. Assessment of a theoretical formalism for dose estimation in CT: an anthropomorphic phantom study. Eur Radiol 2004;14:1275–84 [DOI] [PubMed] [Google Scholar]
- 24.Nishizawa K, Mori S, Ohno M, Yanagawa N, Yoshida T, Akahane K, et al. Patient dose estimation for multi-detector-row CT examinations. Radiat Prot Dosimetry 2008;128:98–105 [DOI] [PubMed] [Google Scholar]
- 25.Maclennan AC, Hadley DM. Radiation dose to the lens from computed tomography scanning in a neuroradiology department. Br J Radiol 1995;68:19–22 [DOI] [PubMed] [Google Scholar]
- 26.Zammit-Maempel I, Chadwick CL, Willis SP. Radiation dose to the lens of eye and thyroid gland in paranasal sinus multislice CT. Br J Radiol 2003;76:418–20 [DOI] [PubMed] [Google Scholar]
- 27.Bassim MK, Ebert CS, Sit RC, Senior BA. Radiation dose to the eyes and parotids during CT of the sinuses. Otolaryngol Head Neck Surg 2005;133:531–3 [DOI] [PubMed] [Google Scholar]
- 28.Mabille M, Beauvais-March H, Rehel JL, Kalifa G. Organ doses from CT examinations in children. [In French.] J Radiol 2005;86:487–91 [DOI] [PubMed] [Google Scholar]
- 29.Fujii K, Aoyama T, Koyama S, Kawaura C. Comparative evaluation of organ and effective doses for paediatric patients with those for adults in chest and abdominal CT examinations. Br J Radiol 2007;80:657–67 [DOI] [PubMed] [Google Scholar]
- 30.Akahane K, Hashimoto M, Hada M, Takano Y, Ono K, Kai M, et al. Radiation doses to neonates during X-ray computed tomography examinations. Radiat Prot Dosimetry 2003;103:41–5 [DOI] [PubMed] [Google Scholar]
- 31.Société Française de Radiologie. Guide des procédures radiologiques. Paris: Société Française de Radiologie, 2005 [Google Scholar]
- 32.Donadieu J, Roudier C, Saguintaah M, Maccia C, Chiron R. Estimation of the radiation dose from thoracic CT scans in a cystic fibrosis population. Chest 2007;132:1233–8 [DOI] [PubMed] [Google Scholar]
- 33.Holmedal LJ, Friberg EG, Borretzen I, Olerud H, Laegreid L, Rosendahl K. Radiation doses to children with shunt-treated hydrocephalus. Pediatr Radiol 2007;37:1209–15 [DOI] [PubMed] [Google Scholar]
- 34.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. AJR Am J Roentgenol 2001;176:289–96 [DOI] [PubMed] [Google Scholar]
- 35.Brisse HJ, Aubert B. CT exposure from pediatric MDCT: results from the 2007-2008 SFIPP/ISRN survey. J Radiol 2009;90:207–15 [DOI] [PubMed] [Google Scholar]
- 36.Brisse HJ, Robilliard M, Savignoni A, Pierrat N, Gaboriaud G, De Rycke Y, et al. Assessment of organ absorbed doses and estimation of effective doses from pediatric anthropomorphic phantom measurements for multi-detector row CT with and without automatic exposure control. Health Phys 2009;97:303–14 [DOI] [PubMed] [Google Scholar]