Abstract
We report a peculiar case of recurrent hyperparathyroidism caused by hyperplasia of a forearm graft implanted following a total parathyroidectomy in a 38-year-old patient with chronic renal failure. The forearm graft hyperplasia was detected using 99Tcm-sestamibi scanning, which identified hyperplastic transplanted parathyroid tissue in the forearm of the patient. During the initial surgery, the surgeon failed to mark the parathyroid tissue with sutures or clips to facilitate locating it. Therefore, we referred the patient for radioguided surgery. This surgical procedure allowed us to locate and completely remove the hyperfunctioning transplanted parathyroid tissue.
Radioguided surgery for hyperparathyroidism (HPTH) combines parathyroid scanning, using 99Tcm-sestamibi, with a hand-held intra-operative detector that guides the surgeon to the area with high tracer uptake. This method is suggested in the literature especially for minimally invasive radioguided parathyroidectomy (MIRP) or for surgery of recurrent or aberrant parathyroid adenomas [1,2]. Surgical options for secondary HPTH from renal failure include total parathyroidectomy with forearm autograft implantation and subtotal parathyroidectomy, leaving a small remnant of parathyroid tissue on a vascular pedicle in the neck. These techniques do not usually require the use of intra-operative gamma probes.
We report a case of recurrent HPTH in a patient with chronic renal failure and hyperplasia of a forearm graft implanted 7 years before, following a total parathyroidectomy. The intra-operative gamma probe allowed quick identification and removal of the abnormal parathyroid tissue in a case that was particularly challenging owing to the absence of clips or non-absorbable sutures to mark the autograft.
Case report
A 38-year-old male presented to our endocrine surgery unit in May 2005 with symptomatic recurrent HPTH. In April 1997, the patient had started haemodialysis treatment for chronic renal failure. In September 2000, the patient underwent a renal transplant which was complicated by acute rejection. The patient underwent three consecutive parathyroidectomies for elevated levels of parathyroid hormone (PTH) with normocalcaemia. We have no additional documentation on these surgical procedures. During surgery in November 2003, a fragment of parathyroid tissue was autotransplantated in the left brachioradialis muscle.
In February 2005, the patient presented with bone pain, general weakness and skin itching. A diagnosis of recurrent HPTH was made. The patient had high levels of PTH (about 800 pg ml−1) and hypocalcaemia (calcium: 6.5 mg dl−1).
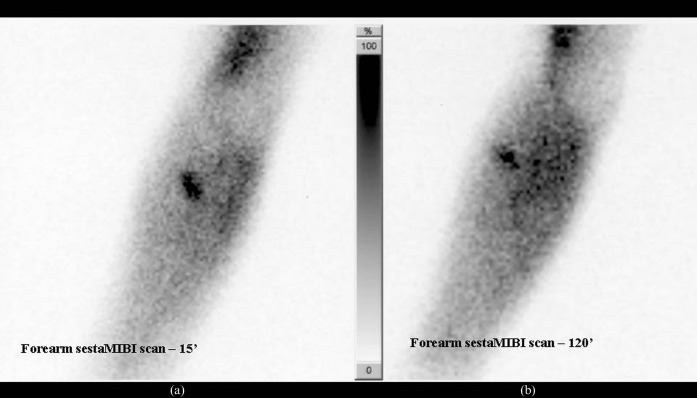
The patient underwent a parathyroid 99Tcm-sestamibi scan, an ultrasound of the neck and left forearm, and scintigraphy of the neck and left forearm was performed using the dual-phase technique following administration of 20 mCi (740 MBq) of 99Tcm-sestamibi. Planar scintigrams of the neck and both forearms were taken in anterior view. The scan showed hyperfunctioning parathyroid tissue in the left forearm (Figure 1). No tracer uptake was detected in the neck area. The ultrasound showed a solid regular area about 1.5 cm in diameter in the brachioradialis muscle that was compatible with hyperplastic parathyroid tissue (Figure 2).
Figure 1.
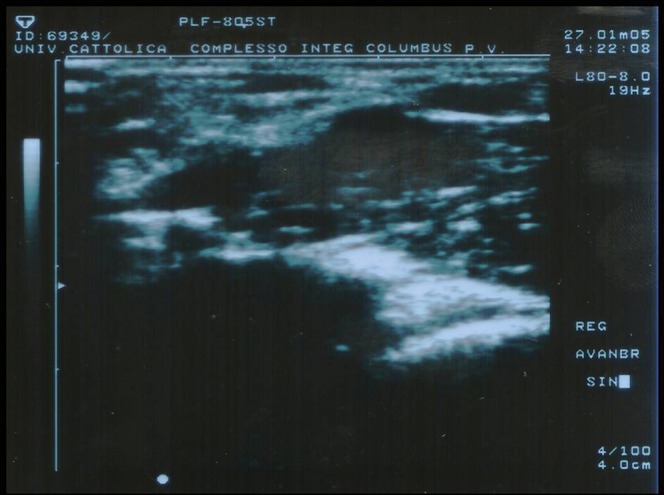
Pre-operative right forearm ultrasound scan.
Figure 2.
(a) Early (15′ p.i.) 99Tcm-sestamibi image of the left forearm showed a focal area of increased uptake of the radiotracer in the left forearm. Some diffuse unspecific uptake was also detectable in the muscles, mainly in the distal biceps brachii, while no vascular uptake was detectable. (b) Delayed (120′ p.i.) image showed persistent focal uptake in the left forearm as well as diffuse unspecific muscle uptake. The pattern of persistent focal 99Tcm-sestamibi uptake is typical of hyperfunctioning parathyroid tissue.
We planned to surgically remove the hyperfunctioning implanted parathyroid tissue. There were no sutures or clips to mark the location of the parathyroid fragments so we decided to use the radioguided technique to identify the fragment sites. 60 min before surgery, the patient received a 10 mCi (370 MBq) 99Tcm-sestamibi injection. Intra-operative scanning with the gamma probe revealed high counts of the tracer in the area of the implant (in vivo 1406 counts s−1). The parathyroid fragment was excised (ex vivo 584 counts s−1). No further abnormalities were identified (forearm following excise: 111 counts s−1).
At the start of the surgery, the patient had an intra-operative PTH (iPTH) level of 290.0 pg ml−1 (normal range 10–65 pg ml−1) and an iPTH level of 320.6 pg ml−1 at the lesion. 5 min following the removal of the graft, the iPTH level was 180.3 pg ml−1, 15 min later it was 120.4 pg ml−1 and 30 min later it was 53.2 pg ml−1. Because there was a significant drop of the iPTH (>50% reduction from baseline) and the tracer counts in the forearm were low, the operation was terminated. Pathological examination confirmed hyperplastic parathyroid tissue (Figure 3). The PTH levels in the patient have been under control in follow-up tests. The patient's PTH level was 12 pg ml−1 3 weeks following the surgery. 4 months later it was 15 pg ml−1, 7 months later it was 16 pg ml−1 and 1 year later it was 7.4 pg ml−1.
Figure 3.
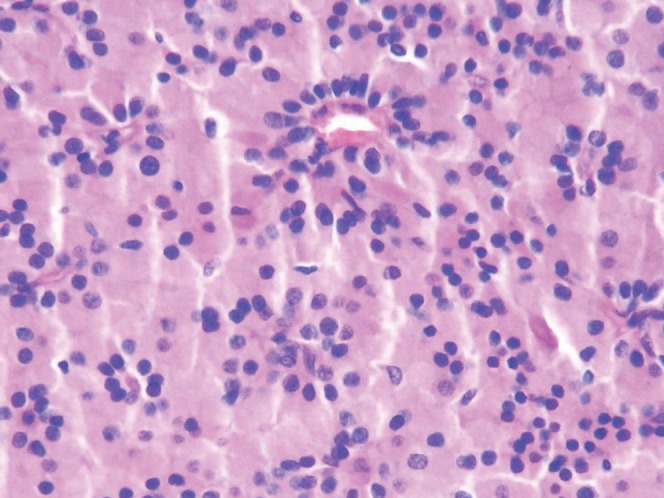
Histological examination shows hyperplastic parathyroid tissue.
Discussion
Radioguided parathyroidectomy has primarily been described for primary HPTH and many reports have shown the effectiveness of this technique in patients with parathyroid adenoma [1,3-5]. Furthermore, most authors have emphasised the role of radioguided surgery and have stated that these techniques may have potential benefit in selected patients. Radioguided parathyroidectomy has been shown to be very effective in patients with recurrent HPTH, in the post-operative neck and in mediastinal parathyroid adenomas [2].
The standard operation performed for secondary HPTH is bilateral neck dissection, which allows us to perform either a subtotal parathyroidectomy or total parathyroidectomy with or without autotransplantation [6-8]. Many experienced surgeons tend to perform total parathyroidectomies with transcervical thymectomies and immediately implant the parathyroid tissue in the forearm. This procedure is favoured over subtotal parathyroidectomy because of the significant risk of recurrent HPTH in the parathyroid tissue remaining in the neck [9-11]. However, even with a total parathyroidectomy and forearm graft, recurrence can occur, and it is usually related to hyperplasia of the autografted tissue.
Forearm graft hyperplasia can be detected using 99Tcm-sestamibi scanning [12-14]. The treatment of forearm graft hyperplasia requires complete excision of hyperplastic parathyroid fragments transplanted in the forearm. To assist locating the small pararthyroid fragments for excision, it is necessary to mark them individually with a non-absorbable suture and/or radio-opaque surgical clips. If an operation for recurrent HPTH is required, the use of gamma probes might help guide the surgeon during the exploration of the forearm. Only a single such case has been described in the literature up to now [13,14].
To assure complete removal of diseased parathyroid tissue, we checked the parathyroid hormone (iPTH) levels with a quick PTH assay during the procedure. This test confirmed the gamma probe results [14]. Our data seem to confirm that the intra-operative gamma probe technique enables the surgeon to localise foream autoimplanted parathyroid hyperplastic tissue in the absence of marking sutures or clips [9,15].
References
- 1.Giordano A, Rubello D, Casara D. New trends in parathyroid scintigraphy. Eur J Nucl Med 2001;28:1409–20 [DOI] [PubMed] [Google Scholar]
- 2.Mariani G, Gulec SA, Rubello D, Boni G, Puccini M, Pelizzo MR, et al. Preoperative localization and radioguided parathyroid surgery. J Nucl Med 2003;44:1443–58 [PubMed] [Google Scholar]
- 3.Costello D, Norman J. Minimally invasive radioguided parathyroidectomy. Surg Oncol Clin N Am 1999;8:555–64 [PubMed] [Google Scholar]
- 4.Norman J, Chheda H. Minimally invasive parathyroidectomy facilitated by intraoperative nuclear mapping. Surgery 1997;122:998–1003 [DOI] [PubMed] [Google Scholar]
- 5.Rubello D, Casara D, Giannini S, Piotto A, Dalle Carbonare L, Pagetta C, et al. Minimally invasive radioguided parathyroidectomy: an attractive therapeutic option for elderly patients with primary hyperparathyroidism. Nucl Med Commun 2004;25:901–8 [DOI] [PubMed] [Google Scholar]
- 6.Zaraca F, Mazzaferro S, Catarci M, Saputelli A, Alò P, Carboni M. Prospective evaluation of total parathyroidectomy and autotransplantation for the treatment of secondary hyperparathyroidism. Arch Surg 1999;134:68–72 [DOI] [PubMed] [Google Scholar]
- 7.Tominaga Y, Kohara S, Namii Y, Nagasaka T, Haba T, Uchida K, et al. Clonal analysis of nodular parathyroid hyperplasia in renal hyperparathyroidism. World J Surg 1996;20:744–50 [DOI] [PubMed] [Google Scholar]
- 8.De Francisco ALM, Fresnedo GF, Rodrigo E, Pinera C, Amado JA, Arias M. Parathyroidectomy in dialysis patients. Kidney Int 2002;80:161–6 [DOI] [PubMed] [Google Scholar]
- 9.Chou FF, Lee CH, Chen JB, Hsu KT, Sheen-Chen SM. Intraoperative parathyroid hormone measurement in patients with secondary hyperparathyroidism. Arch Surg 2002;137:341–4 [DOI] [PubMed] [Google Scholar]
- 10.Rothmund M, Wagner PK, Schark C. Subtotal parathyroidectomy versus total parathyroidectomy and autotransplantation in secondary hyperparathyroidism: a randomized trial. World J Surg 1991;15:745–50 [DOI] [PubMed] [Google Scholar]
- 11.Hargrove GM, Pasieka JL, Hanley DA, Murphy MB. Short- and long-term outcome of total parathyroidectomy with immediate autografting versus subtotal parathyroidectomy in patients with end-stage renal disease. Am J Nephro 1999;19:559–64 [DOI] [PubMed] [Google Scholar]
- 12.Chen H, Civelek AC, Westra WH, Scheel PJ, Udelsman R. Use of technetium Tc 99m sestamibi scintigraphy for recurrent tertiary hyperparathyroidism from a parathyroid forearm graft. South Med J 2000;93:215–17 [PubMed] [Google Scholar]
- 13.Cutress RI, Manwaring-White C, Dixon K, Dhir A, Skene AI. Gamma probe radioguided parathyroid forearm surgery in recurrent hyperparathyroidism. Ann R Coll Surg Engl 2009;91:1–3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Sippel RS, Bianco J, Chen H. Radioguided parathyroidectomy for recurrent hyperparathyroidism caused by forearm graft hyperplasia. J Bone Miner Res 2003;18:939–42 [DOI] [PubMed] [Google Scholar]
- 15.Chou FF, Lee CH, Chen HY, Chen JB, Hsu KT, Sheen-Chen SM. Persistent and recurrent hyperparathyroidism after total parathyroidectomy with autotransplantation. Ann Surg 2002;235:99–104 [DOI] [PMC free article] [PubMed] [Google Scholar]