Abstract
Objectives
To evaluate the effects of employing a 10B-carrier and manipulating intratumour hypoxia on local tumour response and lung metastatic potential in boron neutron capture therapy (BNCT) by measuring the response of intratumour quiescent (Q) cells.
Methods
B16-BL6 melanoma tumour-bearing C57BL/6 mice were continuously given 5-bromo-2′-deoxyuridine (BrdU) to label all proliferating (P) cells. The tumours received reactor thermal neutron beam irradiation following the administration of a 10B-carrier [L-para-boronophenylalanine-10B (BPA) or sodium mercaptoundecahydrododecaborate-10B (BSH)] in combination with an acute hypoxia-releasing agent (nicotinamide) or mild temperature hyperthermia (MTH). Immediately after the irradiation, cells from some tumours were isolated and incubated with a cytokinesis blocker. The responses of the Q and total (P+Q) cell populations were assessed based on the frequency of micronuclei using immunofluorescence staining for BrdU. In other tumour-bearing mice, macroscopic lung metastases were enumerated 17 days after irradiation.
Results
BPA-BNCT increased the sensitivity of the total tumour cell population more than BSH-BNCT. However, the sensitivity of Q cells treated with BPA was lower than that of BSH-treated Q cells. With or without a 10B–carrier, MTH enhanced the sensitivity of the Q cell population. Without irradiation, nicotinamide treatment decreased the number of lung metastases. With irradiation, BPA-BNCT, especially in combination with nicotinamide treatment, showed the potential to reduce the number of metastases more than BSH-BNCT.
Conclusion
BSH-BNCT in combination with MTH improves local tumour control, while BPA-BNCT in combination with nicotinamide may reduce the number of lung metastases.
A neutron capture reaction in boron (10B(n,α)7Li) is, in principle, very effective at destroying tumours, provided a sufficient amount of 10B can be accumulated in the target tumour and a sufficient number of very low energy thermal neutrons can be delivered there. The two particles generated in this reaction have a high linear energy transfer (LET) and have a range of roughly the diameter of one or two tumour cells. It is theoretically possible to kill tumour cells without affecting adjacent healthy cells, if 10B atoms can be selectively accumulated in the interstitial space of tumour tissue and/or intracellular space of tumour cells. Thus, successful boron neutron capture therapy (BNCT) requires the selective delivery of large amounts of 10B to malignant cells [1].
The two most common 10B-carriers used in clinical BNCT trials designed for the treatment of malignant gliomas, melanomas, inoperable head and neck tumours and oral cancer are sodium mercaptoundecahydrododecaborate-10B (sodium borocaptate-10B, BSH, Na210B12H11SH) and boronophenylalanine-10B (BPA, C9H1210BNO4) [1]. In the case of BSH, the delivery of 10B relies on passive diffusion from blood to brain tumour through a disrupted blood–brain barrier [2]. Invariably, the use of BSH results in a high concentration of boron in blood and subsequent vascular damage during BNCT [3]. BPA is designed to be mostly taken up by active transport across the cancer cell membrane [4]. The transport mechanism is operative even in normal cells leading to the accumulation of BPA in normal brain, although at a lower rate. It has been suggested that tumour response can be improved by combining BSH and BPA [5].
Many cancer cells in solid tumours are non-proliferating [quiescent (Q)], whose features are still unknown [6]. To improve cancer treatment, the response of Q cells to anticancer treatment should be determined because tumour cells that are quiescent in situ are often still clonogenic [6]. Meanwhile, within solid tumours, there are hypoxic areas resulting from either limited oxygen diffusion (chronic hypoxia) or limited perfusion (acute hypoxia) [7]. It has also been reported that acute and cyclic, but not chronic, hypoxia significantly increased the number of spontaneous lung metastases, and that this effect was due to the influence of acute hypoxia treatment on the primary tumour [8,9].
Here, we tried to analyse the effects of 10B-carriers and of manipulating intratumour hypoxia on local tumour response and lung metastatic potential in BNCT using a readily metastasising murine melanoma cell line. The neutron capture reaction was performed with two 10B-carriers, BSH and BPA. Tumour hypoxia was manipulated by treatment with an acute hypoxia-releasing agent (nicotinamide) through its inhibiting action on temporary fluctuations in tumour blood flow [10,11] or mild temperature hyperthermia (MTH), which has been shown to have the potential to release tumour cells from diffusion-limited chronic hypoxia [10,11]. Concerning the local tumour response, the effect not only on the total [proliferating (P)+ Q] tumour cell population but also on the Q cell population was evaluated using our original method for selectively detecting the response of Q cells in solid tumours [12].
Materials and methods
Mice and tumours
B16-BL6 murine melanoma cells (Institute of Development, Aging and Cancer, Tohoku University) derived from C57BL/6 mice were maintained in vitro in RPMI-1640 medium supplemented with 10% foetal bovine serum. Tumour cells (1.25×105) were inoculated subcutaneously into the left hind leg of 8-week-old syngeneic female C57BL/6 mice (Japan Animal Co., Ltd, Osaka, Japan). 18 days later, the tumours, approximately 7 mm in diameter, were employed for BNCT, and the body weight of the tumour-bearing mice was 20.1±2.3 g (mean±standard error). Mice were handled according to the Recommendations for Handling of Laboratory Animals for Biomedical Research, compiled by the Committee on Safety Handling Regulations for Laboratory Animal Experiments at our university. The p53 of B16-BL6 tumour cells is the wild type [13].
Labelling with 5-bromo-2′-deoxyuridine
12 days after the inoculation, mini-osmotic pumps (Durect Corporation, Cupertino, CA) containing 5-bromo-2'-deoxyuridine (BrdU) dissolved in physiological saline (250 mg ml–1) were implanted subcutaneously into the back of the animal for 6 days to label all P cells. The percentage of labelled cells after continuous labelling with BrdU was 54.3±6.1%, and reached a plateau at this stage. Therefore, tumour cells not incorporating BrdU after continuous labelling were regarded as Q cells.
Treatment
BSH (125 mg kg−1) and BPA (250 mg kg−1) were purchased from KatChem Ltd (Rez, Czech Republic) and were freshly prepared by dissolving them in physiological saline and injecting intraperitoneally in a volume of 0.02 ml g−1 mouse body weight. In accordance with our previous studies [14], at a dose of less than 500 mg kg−1 for BSH and less than 1500 mg kg−1 for BPA no overt toxicity was observed. Based on the certificate of analysis and material safety data sheet provided by the manufacturer, borocapatate dimmer (BSSB, [10B24H22S2]4-) was not contaminated. Since the intratumour 10B concentration during neutron irradiation is a crucial determinant for cell-kill effect in BNCT, to obtain similar intratumour 10B concentrations during exposure to the neutron beam, irradiation was started at selected time points after the intraperitoneal injection of the 10B-carriers at a selected dose of 10B. Based on a preliminary study of the biodistribution of 10B, irradiation was started 60 min after the intraperitoneal injection of 125 mg kg−1 and 250 mg kg–1 (71.0 mg 10B kg−1 and 12.0 mg 10B kg−1) of BSH and BPA, respectively. 10B concentrations were determined with a thermal neutron guide tube installed at the Kyoto University Research Reactor (KUR) [15].
Some tumour-bearing mice further received an intraperitoneal administration of nicotinamide (1000 mg kg–1) dissolved in physiological saline 1 h before the neutron irradiation. Others were subjected to local MTH at 40°C for 60 min by immersing the implanted tumour in a water bath immediately before being irradiated [11]. Temperatures at the tumour's centre equilibrated within 3−4 min after immersion in the water bath and remained 0.2–0.3°C below the bath's temperature. The water bath's temperature was maintained at 0.3°C above the desired tumour temperature [16].
For irradiation of the tumours implanted into the left hind legs of the mice, a device made of acrylic resin and capable of holding 12 mice was used, and the tumour-bearing mice were irradiated with a reactor neutron beam at a power of 1 MW at KUR after being fixed in position with adhesive tape. A lithium fluoride (LiF) thermoplastic shield was employed to avoid irradiating other body parts except implanted solid tumours. Neutron irradiation was performed using a reactor neutron beam with a cadmium ratio of 9.4. The neutron fluence was measured from the radioactivation of gold foil at both the front and back of the tumours. Since the tumours were small and located just beneath the surface, the neutron fluence was assumed to decrease linearly from the front to the back of the tumours. Thus, we used the average neutron fluence determined from the values measured at the front and back. Contaminating γ-ray, including secondary γ-ray, doses were measured with a thermoluminescence dosimeter (TLD) powder at the back of the tumours. The TLD used was beryllium oxide (BeO) enclosed in a quartz glass capsule. BeO itself is sensitive to thermal neutrons. The thermal neutron fluence of 8×1012 cm−2 is equal to approximately 1 cGy γ-ray dose. We usually use the TLD together with gold activation foil for neutron-sensitivity correction; this is described in detail in Sakurai and Kobayashi [17]. For the estimation of neutron energy spectra, 8 kinds of activation foil and 14 kinds of nuclear reaction were used [17]. The absorbed dose was calculated using the flux-to-dose conversion factor [18]. The tumours contained H (10.7% of the weight), C (12.1% of the weight), N (2% of the weight), O (71.4% of the weight) and others (3.8% of the weight) [19]. The average neutron flux (Φ) and kerma rate of the employed beam were 1.0×109 n cm−2 s−1 and 48.0 cGy h−1 for the thermal neutron range (less than 0.6 eV), 1.6×108 n cm−2 s−1 and 4.6 cGy h−1 for the epithermal neutron range (0.6−10 keV), and 9.4×106 n cm−2 s−1 and 32.0 cGy h−1 for the fast neutron range (more than 10 keV). The kerma rate for boron dose per Φ n cm−2 s−1 of thermal neutron flux for 1 μg g−1 of 10B was 2.67×10−8 Φ cGy h−1. The contaminating γ-ray dose rate was 66.0 cGy h−1.
Each irradiation group also included mice that were not pre-treated with BrdU.
Immunofluorescence staining of BrdU-labelled cells and micronucleus assay
Immediately after irradiation, some tumours excised from the mice given BrdU were minced and trypsinised (0.05% trypsin and 0.02% ethylenediamine-tetraacetic acid (EDTA) in phosphate-buffered saline (PBS), 37°C, 15 min). Tumour cell suspensions were incubated for 72 h in tissue culture dishes containing complete medium and 1.0 μg ml–1 of cytochalasin-B to inhibit cytokinesis while allowing nuclear division. The cultures were trypsinised and cell suspensions were fixed and resuspended with cold Carnoy's fixative (ethanol:acetic acid, 3:1 in volume). Each suspension was placed on a glass microscope slide, dried at room temperature and treated with 2 M hydrochloric acid for 60 min at room temperature to dissociate the histones and partially denature the DNA. The slides were immersed in borax-borate buffer (pH 8.5) to neutralise the acid. BrdU-labelled tumour cells were detected by indirect immunofluorescence staining using a monoclonal anti-BrdU antibody (Becton Dickinson, San Jose, CA) and a fluorescein isothiocyanate (FITC)-conjugated antimouse IgG antibody (Sigma, St. Louis, MO). To distinguish the tumour cells stained with green-emitting FITC and observe them separately, cells on the slides were treated with red-emitting propidium iodide (PI, 2 μg ml–1 in PBS) as background staining and monitored under a fluorescence microscope.
When cell division is disrupted, or the chromosomes are broken or damaged by chemicals or radiation, then the distribution of genetic material between the two daughter nuclei during cell division is affected and pieces or entire chromosomes fail to be included in either of the two daughter nuclei. The genetic material that is not incorporated into a new nucleus forms its “micronucleus” (MN). Thus, the frequency of MN formation reflects the genotoxicity of a chemical compound and radiation very well. The MN frequency in cells not labelled with BrdU could be examined by counting the micronuclei in the binuclear cells that showed only red fluorescence. The MN frequency was defined as the ratio of the number of micronuclei in the binuclear cells to the total number of binuclear cells observed [12].
The ratios obtained in tumours not pre-treated with BrdU indicated the MN frequency at all phases in the total tumour cell population. More than 300 binuclear cells were counted to determine the MN frequency.
Clonogenic cell survival assay
The clonogenic cell survival assay was also performed for the implanted tumours in mice given no BrdU using an in vivo−in vitro assay method immediately after irradiation. The BrdU-unlabelled tumours were excised, weighed, minced and disaggregated by stirring for 20 min at 37°C in PBS containing 0.05% trypsin and 0.02% EDTA. The cell yield was 1.2±0.4×107 g–1 tumour weight. Appropriate numbers of viable tumour cells from the single cell suspension were plated on 60 or 100 mm tissue culture dishes and, 12 days later, colonies were fixed with ethanol, stained with Giemsa, and counted. For the tumours that received no irradiation, the plating efficiencies for the total tumour cell populations and the MN frequencies for the total and Q cell populations are shown in Table 1. The plating efficiency indicates the percentage of cells seeded that grew into colonies when the tumours received no irradiation. The fraction of cells surviving a given dose is determined by counting the number of macroscopic colonies as a fraction of the number of cells seeded, followed by allowance, i.e. dividing by the plating efficiency.
Table 1. Plating efficiency and micronucleus frequency at 0 Gy.
| Without nicotinamide or MTH | With nicotinamide | With MTH |
| Plating efficiency (%) | ||
| Without 10B-carrier | ||
| 84.4±8.2 | 81.4±7.3 | 83.5±8.7 |
| With BPA | ||
| 76.9±7.7 | 69.9±6.5 | 73.9±7.3 |
| With BSH | ||
| 81.4±8.3 | 74.9±6.3 | 78.9±6.8 |
| Micronucleus frequency | ||
| Total cell population | ||
| Without 10B-carrier | ||
| 0.050±0.008 | 0.057±0.006 | 0.054±0.005 |
| With BPA | ||
| 0.063±0.008 | 0.081±0.008 | 0.077±0.007 |
| With BSH | ||
| 0.059±0.008 | 0.078±0.009 | 0.074±0.008 |
| Quiescent cell population | ||
| Without 10B-carrier | ||
| 0.077±0.008 | 0.084±0.009 | 0.081±0.009 |
| With BPA | ||
| 0.091±0.009 | 0.110±0.011 | 0.105±0.010 |
| With BSH | ||
| 0.095±0.009 | 0.120±0.011 | 0.115±0.011 |
BPA, L-para-boronophenylalanine-10B; BSH, mercaptoundecahydrododecaborate-10B; MTH, mild temperature hyperthermia.
Values are mean±standard error (n=9).
As stated above, the MN frequencies for Q cells were obtained from BrdU-unlabelled cells in tumours after continuous BrdU labelling in vivo. The MN frequencies and surviving fractions (SFs) for total tumour cell populations were obtained from cells in tumours not pre-treated with BrdU. Thus, we could not detect any interaction between BrdU and irradiation in our data for the MN frequency and SF.
Growth of B16-BL6 tumours
After neutron beam irradiation at an absorbed dose of 0 or 2.75 Gy with or without a 10B-carrier in combination with nicotinamide or MTH on the 18th day after inoculation, the size of the tumour implanted in the left hind legs of some of the tumour-bearing mice was checked 2 or 3 times a week for approximately 20 days. Tumour volume was calculated using the formula: V=π/6×a×b2, where a and b are the longest and shortest diameter of the tumour measured with callipers, respectively.
Metastasis assessment
17 days after irradiation (i.e. 35 days after the inoculation of B16-BL6 melanoma cells) the tumour-bearing mice were killed by cervical dislocation and their lungs were removed and briefly washed with distilled water, cleaned of extraneous tissue, fixed in Bouin's solution overnight (Sigma) and stored in buffered formalin 10% (Sigma) until the metastases were counted. Macroscopically visible metastases were counted under a dissection microscope [20]. 18 days after the inoculation and immediately before exposure to the neutron beam, macroscopic lung metastases were also counted as background data; the number was 7.5±2.2.
Data analysis and statistics
Three mice with a tumour in the left hind leg were used to assess each set of conditions and each experiment was repeated three times, i.e. nine mice were used for each set of conditions. To examine the difference between pairs of values, Student's t-test was used when variances of the two groups could be assumed to be equal; otherwise the Welch t-test was used. The p-values are from two-sided tests. The data on cell survival and MN frequencies were fitted to the linear quadratic dose relationship [21].
Results
Table 1 shows the plating efficiencies for the total tumour cell population and the MN frequencies without irradiation for the total and Q cell populations. The Q cell population showed significantly higher MN frequencies than the total cell population under each set of conditions.
Table 2 shows the 10B concentrations in irradiated tumours for each set of conditions. The values are averages obtained using the 10B concentrations at the start and end points of irradiation time. When BPA was employed as a 10B-carrier, MTH tended to increase the concentration slightly more than nicotinamide did. In contrast, with BSH as the 10B-carrier, nicotinamide tended to increase the concentration slightly more than MTH. The difference was not significant in either case.
Table 2. 10B concentration (μg g−1=ppm) in tumours and boron dose rate (cGy h−1).
| Without nicotinamide or MTH | With nicotinamide | With MTH |
| 10B concentration (μg g−1=ppm) | ||
| L-para-boronophenylalanine-10B | ||
| 6.9±0.8 | 7.3±1.0 | 8.3±1.1 |
| Mercaptoundecahydrododecaborate-10B | ||
| 7.2±0.9 | 8.4±1.1 | 7.9±1.0 |
| Boron dose rate (cGy h−1) | ||
| L-para-boronophenylalanine-10B | ||
| 184.2±21.4 | 194.9±26.7 | 221.6±29.4 |
| Mercaptoundecahydrododecaborate-10B | ||
| 192.2±24.0 | 224.3±29.4 | 210.9±26.7 |
MTH, mild temperature
Values are mean±standard error (n=9).
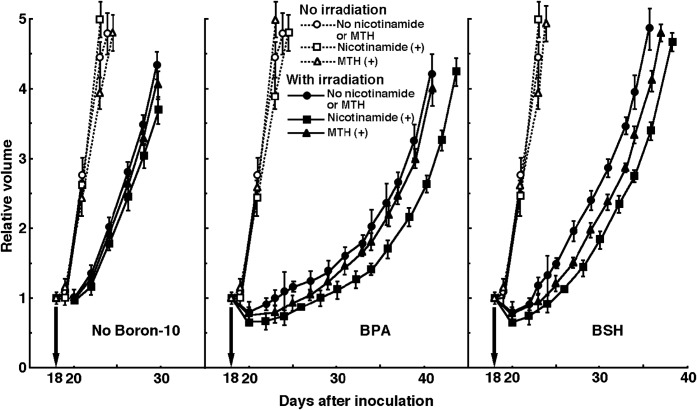
Figure 1 shows cell survival curves for the total cell population as a function of the absorbed dose of neutron beam irradiation with or without a 10B-carrier in combination with nicotinamide or MTH. Figure 2 shows net MN frequencies as a function of irradiated absorbed dose with or without a 10B-carrier in combination with nicotinamide or MTH in the total and Q tumour cell populations. The net MN frequency was the MN frequency in tumours that received irradiation minus those that did not. Overall, the net MN frequencies were significantly smaller in Q cells than in the total cell population (p<0.05).
Figure 1.
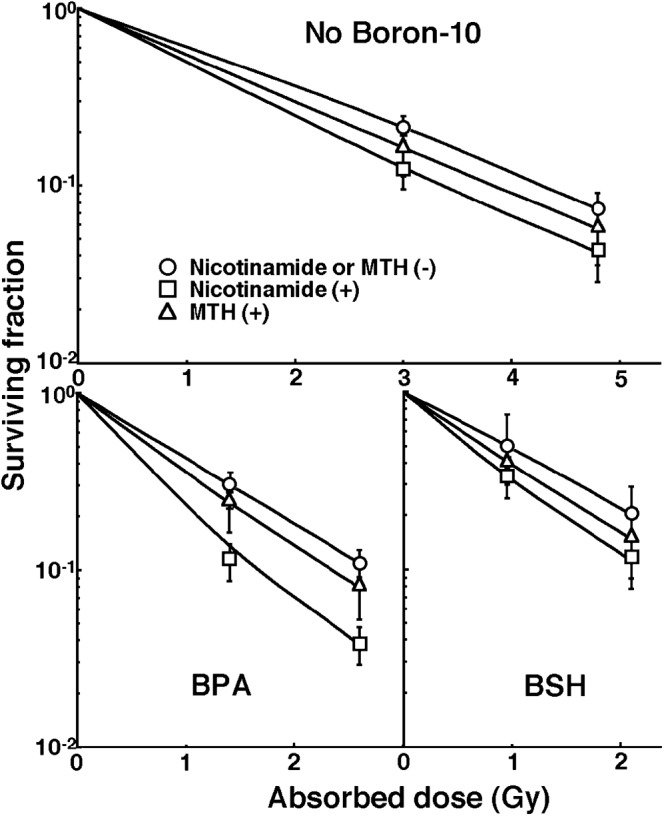
Cell survival curves for the total cell population from B16-BL6 tumours irradiated with reactor neutron beams following the administration of a 10B-carrier [upper panel, no 10B-carrier; lower left panel, L-para-boronophenylalanine-10B (BPA); lower right panel, sodium mercaptoundecahydrododecaborate-10B (BSH)] in combination with nicotinamide treatment or mild temperature hyperthermia (MTH) on day 18 after tumour cell inoculation. ○, irradiation without nicotinamide treatment or MTH; □, irradiation with nicotinamide treatment; Δ, irradiation with MTH. Bars represent standard errors (n=9).
Figure 2.
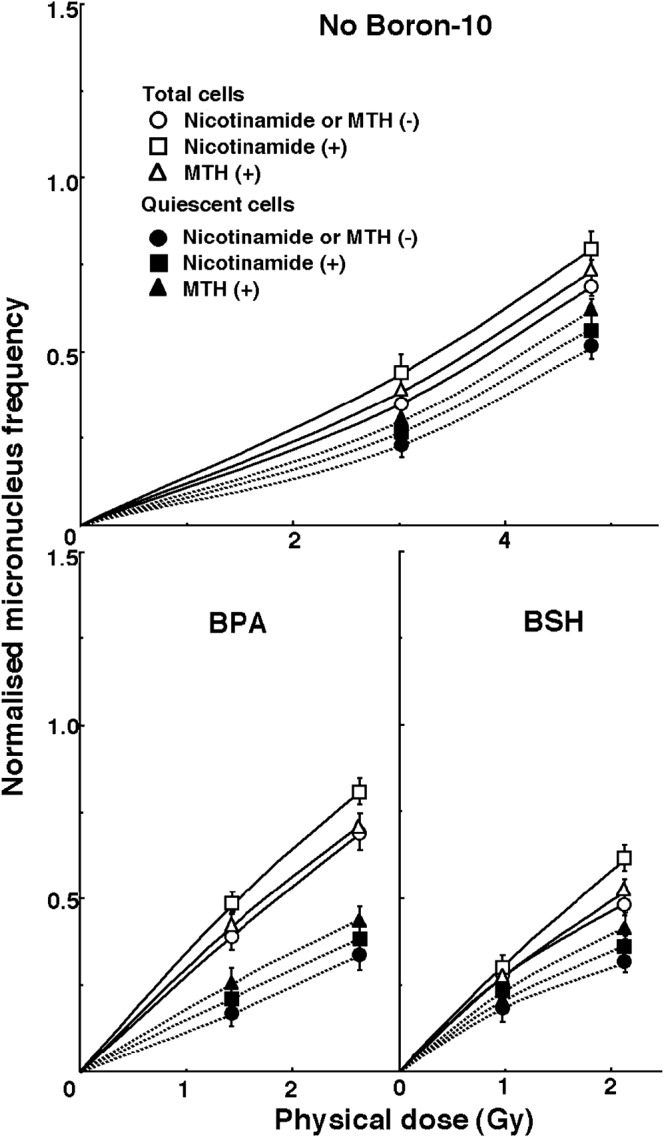
Dose–response curves of the net micronucleus frequency for total (open symbols) and quiescent (solid symbols) cell populations from B16-BL6 tumours irradiated with reactor neutron beams following the administration of a 10B-carrier [upper panel, no 10B-carrier; lower left panel, L-para-boronophenylalanine-10B (BPA); lower right panel, sodium mercaptoundecahydrododecaborate-10B (BSH)] in combination with nicotinamide treatment or mild temperature hyperthermia (MTH) on day 18 after tumour cell inoculation.○,•, irradiation without nicotinamide treatment or MTH; □, ▪, irradiation with nicotinamide treatment; ▵, ▾, irradiation with MTH. Bars represent standard errors (n=9).
To estimate the radio-enhancing effect of 10B-carriers, irradiation with BPA and BSH in both the total and Q cell populations was compared with neutron beam irradiation alone using the data obtained without nicotinamide or MTH shown in Figures 1 and 2 (Table 3). Both BPA and BSH enhanced the sensitivity of the total cell population significantly more than that of the Q cell population (p<0.05). BPA showed a tendency to affect the total cell population more than BSH did. In contrast, the sensitivity of Q cells was, relatively, more enhanced with BSH than with BPA.
Table 3. Enhancement ratiosa due to combination with a 10B-carrier.
| 10B-carrier | Total cell population | Quiescent cells |
| Surviving fraction=0.3 | ||
| BPA | 1.8±0.2 | |
| BSH | 1.5±0.1 | |
| Net micronucleus frequency=0.3 | ||
| BPA | 2.7±0.2 | 1.5±0.1 |
| BSH | 2.3±0.2 | 1.8±0.15 |
BPA, L-para-boronophenylalanine-10B; BSH, sodium mercaptoundecahydrododecaborate-10B.
Values are mean±standard error (n=9).
aThe ratio of the dose of radiation necessary to obtain each end-point without a 10B-carrier to that needed to obtain each end-point with a 10B-carrier.
To estimate the radio-enhancing effect of combined treatment with nicotinamide or MTH in both the total and Q cell populations, the data shown in Figures 1 and 2 were used (Table 4). With or without a 10B-carrier, the sensitivity of the total cell population seemed to be slightly more enhanced with nicotinamide than with MTH. In contrast, the sensitivity of the Q cell population tended to be enhanced more with MTH than with nicotinamide. Notably, with BPA or BSH as the 10B-carrier, MTH enhanced the sensitivity of the Q cell populations significantly more than that of total cell populations (p<0.05).
Table 4. Enhancement ratiosa due to combined treatment with nicotinamide or mild temperature hyperthermia.
| Neutron capture |
Mild temperature |
|
| therapy | Nicotinamide | hyperthermia |
| Surviving fraction=0.3 | ||
| Total cell population | ||
| Without 10B-carrier | 1.2±0.1 | 1.15±0.1 |
| With BPA | 1.15±0.1 | 1.2±0.1 |
| With BSH | 1.3±0.1 | 1.1±0.1 |
| Net micronucleus frequency=0.3 | ||
| Total cell population | ||
| Without 10B-carrier | 1.15±0.1 | 1.1±0.1 |
| With BPA | 1.15±0.1 | 1.2±0.1 |
| With BSH | 1.3±0.1 | 1.1±0.1 |
| Quiescent cell population | ||
| Without 10B-carrier | 1.1±0.1 | 1.25±0.1 |
| With BPA | 1.2±0.1b | 1.45±0.1b |
| With BSH | 1.2±0.1b | 1.4±0.1b |
BPA, L-para-boronophenylalanine-10B; BSH, sodium mercaptoundecahydrododecaborate-10B.
Values are mean±standard error (n=9).
aThe ratio of the dose of radiation necessary to obtain each end-point without combined treatment to that needed to obtain each end-point with the combined treatment.
bThe differences between two values were significant (p<0.05).
To examine the difference in radiosensitivity between the total and Q cell populations, dose-modifying factors were calculated using the data in Figures 1 and 2 (Table 5). Overall, all the values were significantly larger than 1.0 (p<0.05). Whichever 10B-carrier was used, the difference was significantly increased (p<0.05), although the difference was smaller with BSH than with BPA. With or without a 10B-carrier, the difference in radiosensitivity tended to be greater with nicotinamide and smaller with MTH.
Table 5. Dose-modifying factors for quiescent cells relative to the total cell populationa.
| Without nicotinamide or MTH | With nicotinamide | With MTH |
| Net micronucleus frequency=0.3 | ||
| Without 10B-carrier | ||
| 1.3±0.1 | 1.35±0.1 | 1.25±0.1 |
| With BPA | ||
| 2.0±0.2 | 2.0±0.2 | 1.9±0.15 |
| With BSH | ||
| 1.5±0.1 | 1.65±0.15 | 1.35±0.1 |
BPA, L-para-boronophenylalanine-10B; BSH, sodium mercaptoundecahydrododecaborate-10B; MTH, mild temperature hyperthermia.
Values are mean±standard error (n=9).
aThe ratio of the dose of radiation necessary to obtain each end-point in the quiescent cell population to that needed to obtain each end-point in the total tumour cell population.
Figure 3 shows tumour growth curves after neutron beam irradiation with or without a 10B-carrier in combination with nicotinamide or MTH 18 days after the tumour cell inoculation. To evaluate tumour growth, the period required for each tumour to become 3 times as large as it was on day 18 was obtained using the data shown in Figure 3 (Table 6). The tumour progressed to be three times as large as the initial size at the time of irradiation; this can be clearly confirmed in clinics. Without irradiation, with or without a 10B-carrier, there was no significant difference in the period among without nicotinamide or MTH, with nicotinamide, and with MTH. With irradiation at an absorbed dose of 2.75 Gy, overall, the period required was significantly prolonged compared with no irradiation (p<0.05), and the treatments ranked in the following order: without a 10B-carrier<with BSH<with BPA (p<0.05). With or without a 10B-carrier, the period seemed to be prolonged with nicotinamide or MTH, especially nicotinamide. In particular, with BSH, nicotinamide prolonged the period significantly compared with no combination (p<0.05).
Figure 3.
Tumour growth curves for B16-BL6 tumours with (solid symbols) or without (open symbols) neutron beam irradiation following the administration of a 10B-carrier [left panel, no 10B-carrier; centre panel, L-para-boronophenylalanine-10B (BPA); right panel, sodium mercaptoundecahydrododecaborate-10B (BSH)] in combination with nicotinamide treatment or mild temperature hyperthermia (MTH) on day 18 after tumour cell inoculation. Tumour growth was determined by comparing tumour volume with that on irradiation. ○,•, without nicotinamide treatment or MTH; □, ▪, with nicotinamide treatment; Δ, ▾, with MTH. Bars represent standard errors (n=9).
Table 6. The period in days required for each tumour to become 3 times as large as on day 18 following tumour cell inoculation.
| Without nicotinamide or MTH | With nicotinamide | With MTH |
| Without irradiation | ||
| Without 10B-carrier | ||
| 3.4±0.5 | 3.4±0.5 | 3.8±0.6 |
| With BPA | ||
| 3.3±0.5 | 3.6±0.6 | 3.3±0.6 |
| With BSH | ||
| 3.4±0.5 | 3.3±0.5 | 3.6±0.6 |
| With irradiation | ||
| Without 10B-carrier | ||
| 8.7±1.2 | 10.0±1.3 | 9.2±1.3 |
| With BPA | ||
| 20.1±2.0 | 23.2±2.4 | 21.0±2.1 |
| With BSH | ||
| 13.5±1.5 | 16.8±1.8 | 15.4±1.7 |
BPA, L-para-boronophenylalanine-10B; BSH, sodium mercaptoundecahydrododecaborate-10B; MTH, mild temperature hyperthermia. Values are mean±standard error (n=9).
Figure 4 shows the numbers of lung metastases on day 35 after inoculation as a function of the absorbed dose of neutron beam irradiation with or without a 10B-carrier in combination with nicotinamide or MTH. Without irradiation, irrespective of a 10B-carrier, nicotinamide and MTH seemed to slightly decrease and increase the numbers of macroscopic metastases, respectively. With neutron beam irradiation, as the absorbed dose increased, the numbers decreased. The number showed a more marked decrease with a 10B-carrier, especially BPA, than without. There was an almost parallel shift in the curves and no apparent change in the slope of the curves for the tumours treated without a 10B-carrier or with BPA or BSH. This means no apparent radio-sensitising or radio-protecting effect was observed with or without nicotinamide or MTH in terms of the numbers of lung metastases. However, with irradiation, nicotinamide seemed to slightly reduce the numbers of metastatic nodules from the local tumours treated with the neutron beam only, BPA-BNCT or BSH-BNCT.
Figure 4.
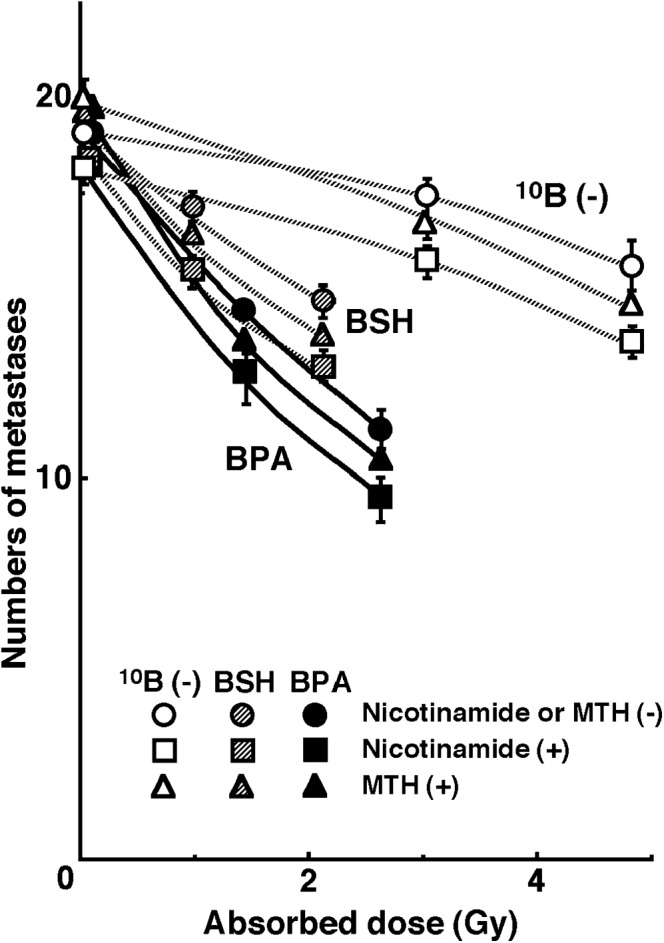
Counted numbers of macroscopic metastases in the lung on day 35 after tumour cell inoculation as a function of the dose of neutron beam irradiation following the administration of a 10B-carrier [open symbols, no 10B-carrier; solid symbols, L-para-boronophenylalanine-10B (BPA); grey symbols, sodium mercaptoundecahydrododecaborate-10B (BSH)] in combination with nicotinamide treatment or mild temperature hyperthermia (MTH) on day 18 after tumour cell inoculation. Circles, without nicotinamide treatment or MTH; squares, with nicotinamide treatment; triangles, with MTH. Bars represent standard errors (n=9).
The numbers of lung metastases from local tumours that received irradiation under each set of conditions, which produced an identical SF of 0.3 as an initial effect (Figure 1), were estimated using the data shown in Figure 4 (Table 7). Overall, BNCT with a 10B-carrier, especially BPA, decreased the numbers more than neutron beam irradiation only. Irrespective of a 10B-carrier, irradiation in combination with nicotinamide resulted in slightly smaller numbers than any other combination.
Table 7. The numbers of metastases from the irradiated tumours that received cytotoxic treatment producing a similar initial local effecta.
| Without nicotinamide or MTH | With nicotinamide | With MTH |
| Surviving fraction=0.3 | ||
| Without 10B-carrier | ||
| 17.9 | 16.6 | 17.9 |
| With BPA | ||
| 14.5 | 14.2 | 14.3 |
| With BSH | ||
| 15.6 | 14.8 | 15.4 |
BPA, L- para-boronophenylalanine-10B; BSH, sodium mercaptoundecahydrododecaborate-10B; MTH, mild temperature hyperthermia.
aBased on the data shown in Figure 4, the estimated numbers of lung metastatic nodules from local tumours that received neutron beam irradiation with or without a 10B-carrier in combination with nicotinamide or mild temperature hyperthermia, which produced an identical surviving fraction of 0.3 as an initial effect on Figure 1.
Discussion
The cellular distribution of 10B from BSH is thought to be mostly dependent on the diffusion of the drug, whereas that from BPA is more dependent on the ability of the cells to take up 10B [2]. As Q cell populations have been shown to have a much larger hypoxic fraction (HF) than total cell populations [10], and hypoxic cells are thought to exhibit less uptake than aerobic cells [6], it follows that Q cells have a lower uptake capacity than the total cell population, and that the distribution of 10B from 10B-carriers into Q cells is more dependent on the diffusion of the drugs than on the uptake ability of the cells.
Tumour microvasculatures frequently have structural and functional abnormalities, such as a disorganised vascular network, dilations, an elongated and tortuous shape, an incomplete endothelial lining, a lack of physiological or pharmacological receptors, an absence of flow regulation, and intermittent stasis [6,22]. Perfusion-related oxygen delivery leads to ischaemic hypoxia, which is often transient. Thus, perfusion-limited acute hypoxic areas are distributed throughout the tumour depending on these causative factors [6,7,22]. Nicotinamide, a vitamin B3 analogue, prevents these transient fluctuations in tumour blood flow that lead to the development of acute hypoxia [23]. Diffusion-related chronic hypoxia is caused by an increase in diffusion distances with tumour expansion; this results in an inadequate oxygen supply for cells distant (>70 μm) from the nutritive blood vessels. Diffusion-limited hypoxia may also be caused by a deterioration of diffusion “geometry”; for example, concurrent vs countercurrent blood flow within the tumour microvessel network [6,7,22]. MTH immediately before irradiation decreased the HF, even combined with nicotinamide treatment. In contrast, MTH did not decrease the HF when tumour-bearing mice were placed in a circulating carbogen (95% O2, 5% CO2) chamber during irradiation [10]. Thus, MTH was shown to increase the tumour response to radiation by improving tumour oxygenation through an increase in tumour blood flow, thereby preferentially overcoming chronic hypoxia rather than acute hypoxia [10].
As shown in Table 2, the distribution of 10B in the total cell population within tumours, a small improvement was achieved through the chronic hypoxia-releasing treatment MTH when BPA, which delivers more 10B to normoxia-rich total tumour cells than BSH does, was used. In contrast, a small improvement was achieved through the acute hypoxia-releasing agent, nicotinamide, when BSH, which delivers more 10B to hypoxia-rich Q cells than BPA does, was used. Namely, whichever 10B-carrier was used, the 10B concentration in tumours may be raised in combination with a treatment that can efficiently release hypoxic areas where it is hard to distribute 10B from each 10B-carrier.
Table 3 shows the distribution of 10B in the tumour from BSH, which relies mostly on passive diffusion, whereas that from BPA relies on uptake capacity in the tumour by active transport, the former resulting from a greater effect on Q cells, and the latter from the total tumour cell population.
The enhancing effect of treatment combined with the boron neutron capture reaction on the total cell population (Table 4) almost paralleled the changes in the 10B concentration in tumours shown in Table 2. In other words, MTH combined with BPA and nicotinamide combined with BSH induced a slightly greater enhancing effect on the total cell population. In the Q cell population, MTH induced a significantly greater enhancing effect (p<0.05), whichever 10B-carrier was used, especially with BPA. Based on these findings, when a 10B-carrier was used, the difference in sensitivity between total and Q cell populations increased with nicotinamide and decreased with MTH (Table 5). Taking into account our previous finding that the HFs in the total and Q cell populations of B16-BL6 tumours, like squamous cell carcinoma VII tumours, are predominantly composed of acute and chronic HFs, respectively [11], and the fact that the employed reactor neutron beams included not only high LET neutrons but also low LET γ-rays, even when a 10B-carrier was not used, it is reasonable that nicotinamide and MTH had a marginal enhancing effect on the total and Q cell populations, respectively. Thus, even without a 10B-carrier, the difference in sensitivity between the total and Q cell populations increased with nicotinamide and decreased with MTH (Table 5). Meanwhile, the changes in tumour growth as a whole (Figure 3, Table 6) were consistent with and supported the changes in the radiosensitivity of total tumour cell populations in cell survival curves (Figure 1) and dose–response curves of the net MN frequency (Figure 2).
The presence of Q cells is probably due, at least in part, to hypoxia and the depletion of nutrition, which is a consequence of poor vascular supply [6,22]. As a result, Q cells are viable and clonogenic, but have ceased dividing. This might promote the formation of micronuclei at 0 Gy in Q tumour cells (Table 1). Q cells have been shown to have significantly less radiosensitivity than the total cell population [6,12,22]. This is shown to also be applicable to BNCT, i.e. more Q cells survive BNCT than P cells (p<0.05) (Figure 2, Table 5). Thus, the control of chronic hypoxia-rich Q cells has a great impact on the outcome of BNCT for controlling local tumours, resulting in the superiority of BSH as a 10B-carrier in BNCT owing to the delivery of more 10B from BSH in the Q cell population than from BPA. With or without a 10B-carrier in the boron neutron capture reaction, nicotinamide and MTH enhanced the radiosensitivity of the total and Q cell populations, respectively. As a result, the use of nicotinamide and MTH led to an increase and a decrease in the difference in radiosensitivity, respectively (Table 5). Although the use of a 10B-carrier in BNCT, especially BPA, significantly increased the difference in radio-sensitivity between total and Q cell populations (p<0.05), MTH is thought to be more useful than nicotinamide in terms of local tumour response because it reduces the difference in radiosensitivity between radiosensitive total and radio-resistant Q cell populations. The use of BSH as a 10B-carrier in combination with MTH is thought to be advantageous and promising in terms of local tumour response in BNCT.
Hypoxia is suggested to enhance metastasis by increasing genetic instability [9]. Acute, but not chronic, hypoxia increased the number of macroscopic metastases in mouse lungs [8,9]. We recently reported the significance of the injection of an acute hypoxia-releasing agent, nicotinamide, into tumour-bearing mice as a combined treatment with γ-ray irradiation in terms of repressing lung metastasis [11]. With or without irradiation, nicotinamide seemed to reduce the number of macroscopic metastases (Figure 4, Table 7). Without irradiation, MTH seemed to increase the number, implying that the release from chronic hypoxia is not as important in repressing metastasis as the release from acute hypoxia. However, hyperthermia is not thought to induce metastasis in the clinical setting [24]. Meanwhile, as the delivered total dose increased with irradiation, the number of macroscopic lung metastases decreased, reflecting the decrease in the number of clonogenically viable tumour cells in the primary tumour (Figure 4). The metastasis-repressing effect achieved through a reduction in the number of clonogenic tumour cells by irradiation is much greater than that achieved by releasing tumour cells from acute hypoxia. On the other hand, more 10B from BPA than from BSH could be distributed into the acute hypoxia-rich total tumour cell population, resulting in a greater decrease in the number of highly clonogenic P tumour cells with BPA-BNCT than with BSH-BNCT and with neutron beam irradiation only. BPA-BNCT rather than BSH-BNCT has some potential to decrease the number of lung metastases, and an acute hypoxia-releasing treatment, such as the administration of nicotinamide, may be promising for reducing numbers of lung metastases. Consequently, BPA-BNCT in combination with nicotinamide treatment may show a little more potential in the reduction of metastases. Finally, it was elucidated that control of the chronic hypoxia-rich Q cell population in the primary solid tumour has the potential to impact the control of local tumours as a whole and that control of the acute hypoxia-rich total tumour cell population in the primary solid tumour has the potential to impact the control of lung metastases.
Acknowledgments
This study was supported, by a grant-in-aid for scientific research (C) (20591493) from the Japan Society for the Promotion of Science.
References
- 1.Barth RF, Coderre JA, Vicente MG, Blue TE. Boron neutron capture therapy of cancer: current status and future prospects. Clin Cancer Res 2005;11:3987–4002 [DOI] [PubMed] [Google Scholar]
- 2.Soloway AH, Hatanaka H, Davis MA. Penetration of brain and brain tumor. VII. Tumor-binding sulfhydryl boron compounds. J Med Chem 1967;10:714–17 [DOI] [PubMed] [Google Scholar]
- 3.Coderre JA, Turcotte JC, Riley KJ, Binns PJ, Harling OK, Kiger WS., 3rd Boron neutron capture therapy, cellular targeting of high linear energy transfer radiation. Technol Cancer Res Treat 2003;2:355–75 [DOI] [PubMed] [Google Scholar]
- 4.Wittig A, Sauerwein WA, Coderre JA. Mechanisms of transport of p-boronophenylalanine through the cell membrane in vitro. Radiat Res 2000;153:173–80 [DOI] [PubMed] [Google Scholar]
- 5.Miyatake S, Kawabata S, Kajimoto Y, Aoki A, Yokoyama K, Yamada M, et al. Modified boron neutron capture therapy for malignant gliomas performed using epithermal neutron and two boron compounds with different accumulation mechanisms: an efficacy study based on findings on neuroimages. J Neurosurg 2005;103:1000–9 [DOI] [PubMed] [Google Scholar]
- 6.Vaupel P. Tumor microenvironmental physiology and its implications for radiation oncology. Semin Radiat Oncol 2004;14:198–206 [DOI] [PubMed] [Google Scholar]
- 7.Brown JM. Evidence of acutely hypoxic cells in mouse tumours, and a possible mechanism of reoxygenation. Br J Radiol 1979;2:650–6 [DOI] [PubMed] [Google Scholar]
- 8.Cairns BA, Kalliomaki T, Hill RP. Acute (cyclic) hypoxia enhances spontaneous metastasis of KHT murine tumors. Cancer Res 2001;61:8903–8 [PubMed] [Google Scholar]
- 9.Rofstad EK, Galappathi K, Mathiesen B, Ruud E-BM. Fluctuating and diffusion-limited hypoxia in hypoxia-induced metastasis. Clin Cancer Res 2007;13:1971–8 [DOI] [PubMed] [Google Scholar]
- 10.Masunaga S, Ono K, Suzuki M, Nishimura Y, Hiraoka M, Kinashi Y, et al. Alteration of the hypoxic fraction of quiescent cell populations by hyperthermia at mild temperatures. Int J Hyperthermia 1997;13:401–11 [DOI] [PubMed] [Google Scholar]
- 11.Masunaga S, Matsumoto Y, Hirayama R, Kashino G, Tanaka H, Suzuki M, et al. Significance of hypoxia manipulation in solid tumors in the effect on lung metastases in radiotherapy, with reference to its effect on the sensitivity of intratumor quiescent cells. Clin Exp Metastasis 2009;26:693–700 [DOI] [PubMed] [Google Scholar]
- 12.Masunaga S, Ono K. Significance of the response of quiescent cell populations within solid tumors in cancer therapy. J Radiat Res 2002;43:11–25 [DOI] [PubMed] [Google Scholar]
- 13.Duan X, Zhang H, Liu B, Li XD, Gao QX, Wu ZH. Apoptosis of murine melanoma cells induced by heavy-ion radiation combined with Tp53 gene transfer. Int J Radiat Biol 2008;84:211–17 [DOI] [PubMed] [Google Scholar]
- 14.Masunaga S, Ono K, Sakurai Y, Takagaki M, Kobayashi T, Kinashi Y, et al. Evaluation of apoptosis and micronucleation induced by reactor neutron beams with two different cadmium ratios in total and quiescent cell populations within solid tumors. Int J Radiat Oncol Biol Phys 2001;51:828–39 [DOI] [PubMed] [Google Scholar]
- 15.Kobayashi T, Kanda K. Microanalysis system of ppm-order 10B concentrations in tissue for neutron capture therapy by prompt γ-ray spectrometry. Nucl Instrum Methods 1983;204:525–31 [Google Scholar]
- 16.Nishimura Y, Ono K, Hiraoka M, Masunaga S, Jo S, Shibamoto Y, et al. Treatment of murine SCC VII tumors with localized hyperthermia and temperature-sensitive liposomes containing cisplatin. Radiat Res 1990;122:161–7 [PubMed] [Google Scholar]
- 17.Sakurai Y, Kobayashi T. Characteristics of the KUR heavy water neutron irradiation facility as a neutron irradiation field with variable energy spectra. Nucl Instrum Meth A 2000;453:569–96 [Google Scholar]
- 18.Kobayashi T, Sakurai Y, Kanda K, Fujita Y, Ono K. The remodeling and basic characteristics of the heavy water neutron irradiation facility of the Kyoto University Research Reactor, mainly for neutron capture therapy. Nucl Tech 2000;131:354–78 [Google Scholar]
- 19.Snyder WS, Cook MJ, Nasset ES, Karhausen LR, Parry Howells G, Tipton I. Gross and elemental content of reference man. Snyder WS. (ed) Report of the task group on reference man. Oxford, UK: Pergamon Press, 1975; 273–324 [Google Scholar]
- 20.De Jaeger K, Kavanagh M-C, Hill RP. Relationship of hypoxia to metastatic ability in rodent tumours. Br J Cancer 2001;84:1280–5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hall EJ. Time, dose, and fractionation in radiotherapy. Hall EJ, Giaccia AJ. (eds). Radiobiology for the radiologist. 6th edn Philadelphia, PA: Lippincott Williams & Wilkins, 2006:378–97 [Google Scholar]
- 22.Vaupel P, Kallinowski F, Okunieff P. Blood flow, oxygen and nutrient supply, and metabolic microenvironment of human tumors: a review. Cancer Res 1989;49:6449–65 [PubMed] [Google Scholar]
- 23.Chaplin DJ, Horsman MR, Trotter MJ. Effect of nicotinamide on the microregional heterogeneity of oxygen delivery within a murine tumor. J Natl Cancer Inst 1990;82:672–6 [DOI] [PubMed] [Google Scholar]
- 24.Moller MG, Lewis JM, Dessureault S, Zager JS. Toxicities associated with hyperthermic isolated limb perfusion and isolated limb infusion in the treatment of melanoma and sarcoma. Int J Hyperthermia 2008;24:275–89 [DOI] [PubMed] [Google Scholar]