Abstract
The presence of the appendix within a femoral hernia is rare. It was first described by the French surgeon Jacques Croissant de Garengeot in 1731. This phenomenon accounts for 0.8–1% of all femoral hernias. Acute appendicitis occurring within a femoral hernia is even rarer and is difficult to diagnose pre-operatively. This type of hernia is termed a de Garengeot hernia. The ultrasonographic and CT imaging features of de Garengeot hernias have been described previously. We report a case of a 57-year-old female who presented with a painful right-sided groin mass. She underwent MRI of the inguinal region, which successfully diagnosed this rare hernia pre-operatively. To our knowledge, this is the first description of a de Garengeot hernia diagnosed using MRI.
Case report
A 57-year-old female was admitted with a painful right-sided groin mass, which had been present for 3 days. She had no significant medical or surgical history. She denied any vomiting, change in bowel habit or recent trauma.
Abdominal examination demonstrated a soft non-distended abdomen with an erythematous mass in the right inguinal region measuring 5×5 cm. The mass was felt to be clinically pulsatile, mildly tender on palpation and non-reducible. No signs of peritonism were elicited and the remainder of the physical examination was non-contributory. Laboratory data revealed a raised C-reactive protein (CRP) of 65.6 mg l−1 and a slightly raised white blood cell count of 12 800 mm−3.
An incarcerated femoral hernia was suspected but, given the seemingly pulsatile nature of the mass, an ultrasound of the groin and pelvis was performed. This demonstrated a tubular abnormality surrounded by fluid and soft tissue of heterogeneous echotexture. There was no vascular component to the mass seen. The patient was referred for cross-sectional imaging.
MRI was employed as the patient had an allergy to iodinated contrast. Imaging was performed in a 1.5 T MRI scanning unit (Symphony, Siemens Healthcare, Erlangen, Germany). The patient was scanned in supine using a circular polarised four-element phased array body coil. Axial and coronal half-Fourier acquired single-shot turbo spin-echo (repetition time (TR)/echo time (TE), 1460/123 ms; flip angle, 150°; slice thickness 5 mm, 256 matrix, field of view 400 mm) imaging was performed. Further axial and coronal true fast imaging with steady state precession (TR/TE, 5.030/2.520; slice thickness 5 mm, 256 matrix, field of view 400 mm) was performed.
The appendix was identified as a blind-ending tubular structure herniating into the femoral triangle. The lumen was dilated to 8 mm and there was a significant amount of high signal seen on T2 weighted images, both around the appendix and within its lumen, consistent with peri-appendiceal inflammatory change (Figures 1 and 2). The MRI findings were consistent with appendicitis within a femoral hernia, i.e. a de Garengeot hernia. Intra-operative examination confirmed the radiological diagnosis and the patient subsequently underwent a repair of the femoral hernia and an appendectomy.
Figure 1.
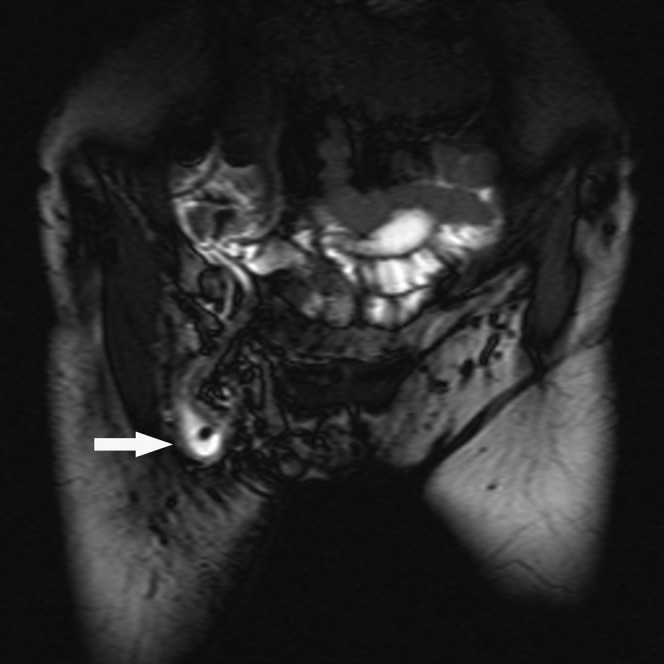
A coronal image of the pelvis using true fast imaging with steady-state precession. The image demonstrates a tubular abnormality in the right inguinal region (arrow). High signal fluid is seen to surround a low signal linear structure which was thought to represent the appendix. This was confirmed at surgery to be an inflamed appendix in the femoral canal. The focal area of low signal area within the high signal abnormality was believed to represent air.
Figure 2.
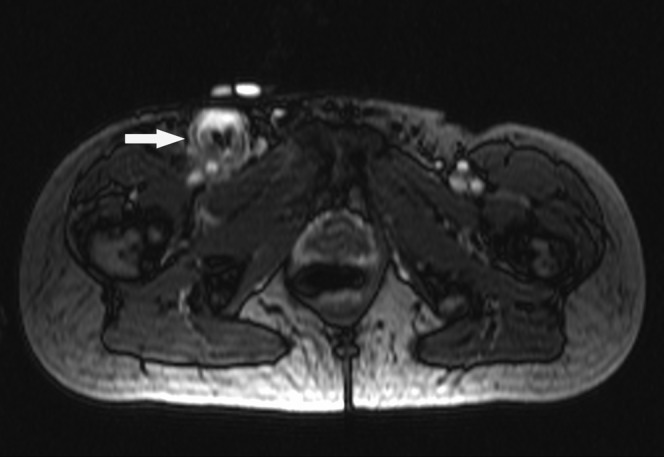
An axial image of the pelvis using true fast imaging with steady-state precession. The image demonstrates an area of high signal surrounding a low signal tubular structure (arrow). Its relationship to the femoral vessels led to the pre-operative suggestion that it represented an inflamed appendix lying within the femoral canal.
Discussion
The presence of the appendix within a femoral hernia is rare. It was first described by the French surgeon Jacques Croissant de Garengeot in 1731 [1]. This phenomenon accounts for 0.8–1% of all femoral hernias [2]. Acute appendicitis occurring within a femoral hernia is even rarer and it is difficult to diagnose pre-operatively. This type of hernia is termed a de Garengeot hernia.
Femoral hernias are twice as common in females as in males and this ratio is also true for the incidence of de Garengeot hernias. The median age for presentation of this condition was 55 years in one retrospective study [2]. The demographics of the case we present correlate appropriately with these figures. It is important to understand the anatomy of the femoral triangle to accurately diagnose this form of hernia radiologically. It is formed by the adductor longus muscle (medially), sartorius (laterally) and the inguinal ligament (superiorly), while iliopsoas, pectineus and adductor longus form its floor. The femoral canal lies medial to the femoral vein within the femoral triangle [3]. The neck of a femoral hernia is formed by the femoral ring. This opening is significantly narrower than its counterpart in an inguinal hernia. This increases the chances that the bowel or omentum within a femoral hernia will be compressed or obstructed. Appendicitis may arise as a result of pressure from the neck of the hernia causing luminal obstruction.
Cases such as this will usually present as a tender inguinal mass, characteristic of an incarcerated femoral or inguinal hernia, thus potentially masking an underlying appendicitis [1]. Although most cases are diagnosed intra-operatively, pre-operative imaging, including ultrasound and CT, have been shown to be an aid to early diagnosis [4]. Our search of the literature did not yield any previous reports of a de Garengeot hernia having been imaged by MRI.
The features identified on ultrasound in our patient (a blind-ending tubular structure surrounded by fluid and echogenic material in the inguinal region) correlated well with the only dedicated description of the sonographic characteristic of a de Garengeot hernia in the literature by Filatov et al [5]. In our case the exact relationship of the hernia to the femoral vessels was not ascertained on ultrasound. As described by Filatov et al, depiction of this relationship is important in terms of the pre-operative diagnosis of this type of hernia.
In our institution we would usually perform a contrast-enhanced CT examination of the abdomen and pelvis to further evaluate such a patient; however, the patient's contrast allergy precluded this. MRI was performed as an alternative. MRI has been shown to be a useful radiological investigation for the diagnosis of acute appendicitis. A recent meta-analysis demonstrated its sensitivity and specificity in this setting to be 97% and 95%, respectively [6]. In particular MRI has been advocated as an important step in the algorithm for assessing pregnant patients with suspected appendicitis [7]. It should be noted that MRI is contraindicated in the first trimester. Meta-analysis has shown the sensitivity and specificity of CT in the diagnosis of acute appendicitis to be 91% and 90%, respectively. The same study revealed the sensitivity and specificity of graded compression ultrasound in this setting to be 78% and 83% [8]. The figures for CT and MRI are comparable, while the performance of ultrasound lags slightly behind. CT remains the investigation of choice in cases of suspected acute appendicitis, while ultrasound is a valuable tool that is also frequently used in these patients. Despite high sensitivities and specificities, MRI is not routinely used because access to it can be limited, particularly out of hours, and the cost is higher than both CT and ultrasound. However, it can be used in certain cases as a valuable problem-solving tool.
As with other imaging techniques, the detection of the appendix using MRI can sometimes be challenging. Clearly the goal is to identify a blind-ending tubular structure arising from the right iliac fossa. Features which can help to suggest a normal appendix include the detection of high signal within the lumen on T2 weighted images indicating intraluminal fluid and the presence of a blooming artefact on gradient echo sequences, which indicates the presence of intramural air [9]. In the setting of acute appendicitis, T2 weighted sequences are most useful. Inflammatory fluid surrounding the appendix will be of high signal [9]. The excellent contrast resolution afforded by T2 weighting makes it ideal for identifying the inflamed appendix. Fat suppression can also help in this regard. The anatomical measurements of the appendix used to suggest a diagnosis of acute appendicitis (i.e. an appendiceal diameter of >6 mm or a wall thickness of >2 mm) are the same across all imaging modalities. While some authors advocate the use of either oral or intravenous contrast agents, neither are necessary. In our institution we routinely perform only non-contrast MRI in this setting [7]. The other obvious advantage MRI has over CT is the lack of ionising radiation.
The first description of an inguinal hernia on MRI was made in 1989 and now MRI is frequently used to evaluate groin masses [10]. It can be used to differentiate between the various types of hernias in this region [3]. The inguinal ligament, which is important in differentiation of femoral and inguinal hernias, can be easily identified on MRI, while the use of dynamic MRI enables the detection of hernias, which may be only intermittently present and missed on other imaging modalities. MRI has been shown to have a sensitivity of up to 94.5% in the diagnosis of inguinal hernias. A pre-peritoneal lipoma or a patent processus vaginalus are the most common causes of a false-positive study and dynamic imaging is important to differentiate these findings from a true hernia [10]. However, these abnormalities would be unlikely to cause a diagnostic dilemma in the acute setting. In the non-acute setting, MRI is also useful because it can frequently demonstrate alternative causes for groin pain when an investigation is negative for femoral or inguinal hernia [11].
To our knowledge, this is the first description of a de Garengeot hernia using MRI as an imaging tool. The combination of good anatomical detail and excellent contrast resolution afforded by MRI allowed a pre-operative diagnosis to be made. MRI offers the advantages of not having ionising radiation and not requiring intravenous contrast material. We feel it can be considered as an alternative to CT in cases such as these.
References
- 1.Thomas B, Thomas M, McVay B, Chivate J. De Garengeot hernia. JSLS 2009;13:455–7 [PMC free article] [PubMed] [Google Scholar]
- 2.Sharma H, Jha PK, Shekhawat NS, Memon B, Memon MA. De Garengeot hernia: an analysis of our experience. Hernia 2007;11:235–8 [DOI] [PubMed] [Google Scholar]
- 3.Shadbolt CL, Heinze SB, Dietrich RB. Imaging of groin masses: inguinal anatomy and pathological conditions revisited. Radiographics 2001;21:S261–71 [DOI] [PubMed] [Google Scholar]
- 4.Ebisawa K, Yamazaki S, Kimura Y, Kimura M, Kurita K, Yasumuro S, et al. Acute appendicitis in an incarcerated femoral hernia: a case of de Garengeot hernia. Case Rep Gastroenterol 2009;3:313–17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Filatov J, Ilibitzki A, Davidovitch S, Soudack M. Appendicitis within a femoral hernia: sonographic appearance. J Ultrasound Med 2006;25:1233–5 [DOI] [PubMed] [Google Scholar]
- 6.Barger RL, Jr, Nandalur KR. Diagnostic performance of magnetic resonance imaging in the detection of appendicitis in adults: a meta-analysis. Acad Radiol 2010;17:1211–16 [DOI] [PubMed] [Google Scholar]
- 7.Cobben LP, Groot I, Haans L, Blickman JG, Puylaert J. MRI for clinically suspected appendicitis during pregnancy. AJR Am J Roentgenol 2004;183:671–5 [DOI] [PubMed] [Google Scholar]
- 8.van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology 2008;249:97–106 [DOI] [PubMed] [Google Scholar]
- 9.Tkacz JN, Anderson SA, Soto J. MR imaging in gastrointestinal emergencies. Radiographics 2009;29:1767–80 [DOI] [PubMed] [Google Scholar]
- 10.van denBerg JC. Inguinal hernias: MRI and ultrasound. Semin Ultrasound CT MR 2002;23:156–73 [DOI] [PubMed] [Google Scholar]
- 11.Tuite MJ, DeSmet AA. MRI of selected sports injuries: muscle tears, groin pain, and osteochondritis dissecans. Semin Ultrasound CT MR 1994;15:318–40 [DOI] [PubMed] [Google Scholar]


