Abstract
Objective
The aim of this study was to identify the risk factors associated with the prognosis of a subchondral insufficiency fracture of the femoral head (SIF).
Methods
Between June 2002 and July 2009, 25 patients diagnosed with SIF were included in this study. Sequential radiographs were evaluated for the progression of collapse. Clinical profiles, including age, body mass index, follow-up period and Singh’s index, were documented. The morphological characteristics of the low-intensity band on T1 weighted MRI were also examined with regards to four factors: band length, band thickness, the length of the weight-bearing portion and the band length ratio (defined as the proportion of the band length to the weight-bearing portion of the femoral head in the slice through the femoral head centre).
Results
Radiographically, a progression of collapse was observed in 15 of 25 (60.0%) patients. The band length in patients with progression of collapse [22.5 mm; 95% confidence interval (CI) 17.7, 27.3] was significantly larger than in patients without a progression of collapse (13.4 mm; 95% CI 7.6, 19.3; p<0.05). The band length ratio in patients with progression of collapse (59.8%; 95% CI 50.8, 68.9) was also significantly higher than in patients without a progression of collapse (40.9%; 95% CI 29.8, 52.0; p<0.05). No significant differences were present in the other values.
Conclusion
These results indicate that the band length and the band length ratio might be predictive for the progression of collapse in SIF.
Subchondral insufficiency fractures of the femoral head (SIF) often occur in osteoporotic elderly patients [1-9]. Patients usually suffer from acute hip pain without any obvious antecedent trauma. Radiologically, a subchondral fracture is seen primarily in the superolateral portion of the femoral head [4,5,10]. T1 weighted MRI reveal a very low-intensity band in the subchondral area of the femoral head, which tends to be irregular, disconnected and convex to the articular surface [2,4,5,7,9,11]. This low-intensity band in SIF was histologically proven to correspond with the fracture line and associated repair tissue [5,9]. Some cases of SIF resolve after conservative treatment [5,11-14]; other cases progress until collapse, thereby requiring surgical treatment [4-10,15]. The prognosis of SIF patients remains unclear.
The current study investigated the risk factors that influence the prognosis of SIF based on the progression to collapse.
Methods and materials
The present retrospective study was approved by the institutional review board at the Kyushu University.
Patients
We retrospectively studied 25 consecutive patients diagnosed with SIF between June 2002 and July 2009 at our institution. Patients with a history of any surgery or infection in the hip joint were excluded. The age at the time of the initial MRI, the body mass index (BMI) [16] and the follow-up period were documented in all 25 patients. The follow-up period extended from the time of the first attendance to the latest follow-up. Only one patient ceased follow-up examinations, owing to the disappearance of symptoms, and stopped visiting our hospital on his own judgement. Of the 25 patients, 4 had a known diagnosis of osteoporosis (3 patients used bisphosphonates), 3 had a history of corticosteroid therapy and 1 had chronic renal failure. No patients had any other stress fractures or syndromes of transient osteoporosis. In young patients (<30 years of age), both blood and hormonal examinations were performed; these investigations revealed no conditions that predisposed the patients to osteoporosis, such as hyperparathyroidism or abnormalities in calcium or phosphate metabolism. The bone mineral density measurements were performed by dual energy X-ray absorptiometry in 10 patients.
The diagnosis of SIF was based on several published criteria [4,5,10]: hip pain that began without any apparent history of trauma; radiographs that were normal or that showed the collapse of the femoral head, joint space narrowing and/or a linear patchy sclerotic area in the superior portion of the femoral head; a bone marrow oedema pattern in the femoral head and/or neck on MRI; and a subchondral low signal-intensity band on T1 weighted MRI that was serpiginous or paralleled the articular surface. In some cases, gadolinium-enhanced MRI was performed to differentiate SIF from osteonecrosis of the femoral head.
All patients were initially administered conservative treatment, which consisted of anti-inflammatory drugs and the avoidance of weight bearing for 6–8 weeks.
Radiological measurements
Radiographs were taken using the same technique throughout the study period; a standardised position of the beam and radiographic penetration were adopted. The presence of the collapse at first attendance was evaluated on the anteroposterior (AP) radiographs. The progression of collapse was evaluated at 12 months after the first attendance. We regarded >2 mm progression as a progression of the collapse in comparison with the radiographs obtained at first attendance. In addition, Singh’s index was examined in each patient on the initial AP radiographs [17].
MRI evaluations
Examination of 20 patients was performed using a 1.5 T MR system [Siemens MAGNETOM Symphony or Vision (Siemens AG, Munich, Germany) or Philips Achieva (Philips Medical Systems, Amsterdam, the Netherlands)] and 5 patients underwent examination using a 3.0 T MR system (Philips; Achieva, Amsterdam, the Netherlands). The T1 weighted MRI (repetition time/echo time (TR/TE)=400–600/8–19 ms) and T2 weighted MRI (TR/TE=3000–4000/81–108 ms) in the coronal and oblique axial planes (paralleling the femoral neck axis) were available for all patients.
Four parameters were measured on T1 weighted MRI in the coronal plane: the band length, band thickness, length of the weight-bearing portion and the band length ratio. The band lengths were measured at the slice in which the longest band was detected; similarly, the band thickness was measured at the slice in which the thickest band was detected. The length of the weight-bearing portion was measured at the slice through the femoral head centre. The weight-bearing portion of the femoral head is defined as the area lateral to the mid-vertical line through the acetabular edge and the teardrop bottom. The band length ratio represents the length of the fracture line relative to the length of the weight-bearing portion, thus the band length ratio was measured at the slice through the femoral head centre (Figure 1).
Figure 1.
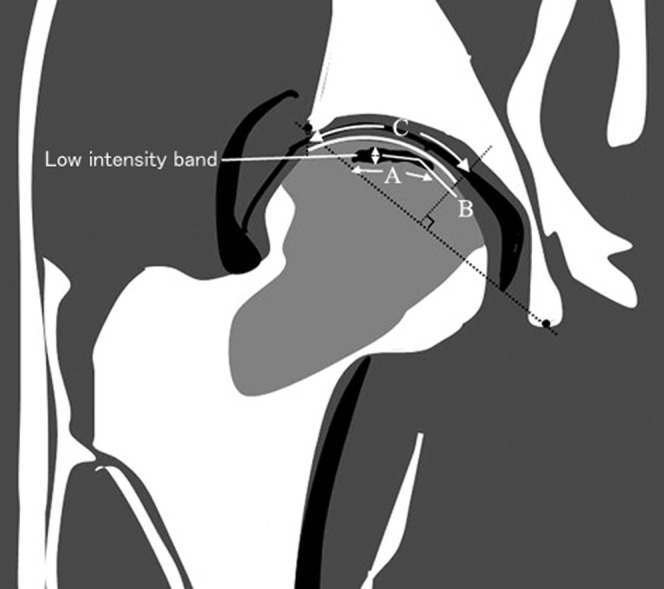
Diagram showing the method used to measure the morphology of the low-intensity band on T1 weighted MRI. The band length (A) and band thickness (B) are indicated. The weight-bearing portion of the femoral head is defined as the area lateral to the mid-vertical line through the acetabular edge and the teardrop bottom (C). The band length ratio is given by (A/C).
Three authors (observer 1, KI; observer 2, SI; observer 3, TY) assessed all the images in a blind trial and independently estimated these values. We calculated the mean of three values as estimated by three observers. All measurements were carried out using the CIS-Image Viewer (IBM, New York, NY), Image J (National Institutes of Health, MD) and Synapse (Fujifilm, Tokyo, Japan) image analysis software programs.
Statistical analysis
In this study, non-progression of the collapse group was compared with the progression of the collapse group. The age, BMI, follow-up period, Singh’s index, bone mineral density (T-score), band length, band thickness, length of the weight-bearing portion and band length ratio were analysed using the Mann–Whitney U-test. The level of statistical significance was set at p<0.05. To evaluate the interobserver variability of the measurement on MRI, the mean differences in the measurement of the respective observers were calculated. The reliability of the measurement was evaluated by Spearman’s correlation coefficient and values >0.7 were considered to be in good agreement.
Results
Clinical data
The study group included 6 male and 19 female patients. All patients showed unilateral involvement. The patient ages at the time of the initial MRI ranged from 19 to 88 years (mean age 56.9 years). The BMI ranged from 18.3 to 31.6 kg m–2 (mean 20.8 kg m–2) and the follow-up period ranged from 4 to 64 months (mean 24 months). Bone mineral density measurements were available for 10 patients and showed either osteopenia or osteoporosis in 9 patients (T-score <−1.0). The clinical data are summarised in Table 1. No significant differences were observed in age, BMI, follow-up period, Singh’s index or bone mineral density between the non-progressive and progressive patients of the collapse group.
Table 1. Patient characteristics.
| Non-progression of collapse (male:female 3:12) | Progression of collapse (male:female 3:7) | p-value | |
| Age (years) | 56.2 (44.5, 67.9) | 57.4 (47.8, 67.0) | 0.522 |
| Body mass index (kg m–2) | 22.5 (20.3, 24.7) | 23.0 (21.2, 24.8) | 0.912 |
| Follow-up period (months) | 23.1 (12.5, 33.7) | 23.9 (15.2, 32.6) | 1.000 |
| Singh’s index | 3.5 (2.8, 4.2) | 3.2 (2.7, 3.7) | 0.349 |
| Bone mineral density (T-score) | −1.50 (−2.47, −0.53)a | −1.96 (−2.56, −1.37)b | 0.409 |
Values are mean (95% confidence intervals).
aMale:female 2:1.
bMale:female 1:6.
Radiographic findings
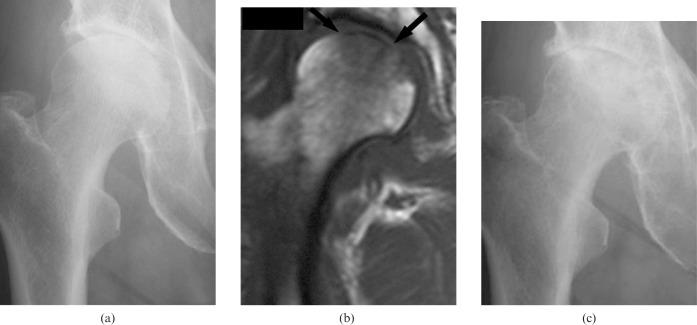
At the time of the first attendance, 21 of 25 patients showed some degree of collapse in the femoral head. Of 25 patients, 15 showed a progression of the collapse (Figure 2) and all patients underwent surgery. By contrast, 10 of the 25 patients showed no progression of the collapse and in all of these patients pain was resolved after conservative therapy.
Figure 2.
A 77-year-old female patient complained of severe right hip pain. (a) A radiograph obtained at the first attendance shows a slight joint space narrowing in the medial part of the hip joint without evidence of femoral head collapse. (b) T1 weighted MRI (repetition time/echo time=403/10 ms) shows a very low signal-intensity band (arrows) just beneath the articular cartilage, surrounded by the low-intensity area (bone marrow oedema). (c) A radiograph obtained 12 months later shows progression of the collapse in the medial part of the femoral head.
MRI evaluations
The T1 weighted MRI showed serpiginous, irregular and discontinuous low signal-intensity bands in all cases. The band length in patients with progression of the collapse was 22.5 mm [95% confidence interval (CI) 17.7, 27.3], whereas the band length in patients without progression of the collapse was 13.4 mm (95% CI 7.6, 19.3). The band length in patients with progression of the collapse was significantly higher than that in patients without a progression of the collapse (p<0.05; Table 2). No significant differences were seen in the band thickness; similarly, no significant differences were seen in the length of the weight-bearing portion. The band length ratio in patients with progression of the collapse (59.8%; 95% CI 50.8, 68.9) was also significantly higher than in patients without a progression of the collapse (40.9%; 95% CI 29.8, 52.0; p<0.05).
Table 2. Results of MRI measurements.
| Non-progression of collapse (male:female 3:12) | Progression of collapse (male:female 3:7) | p-value | |
| Band length (mm) | 13.4 (7.6, 19.3) | 22.5 (17.7, 27.3) | 0.031 |
| Band thickness (mm) | 1.8 (1.5, 2.1) | 1.8 (1.5, 2.0) | 0.978 |
| Length of weight-bearing portion (mm) | 34.8 (33.3, 36.2) | 35.2 (34.0, 36.4) | 0.637 |
| Band length ratio (%) | 40.9 (29.8, 52.0) | 59.8 (50.8, 68.9) | 0.016 |
Values are mean (95% confidence intervals).
Interobserver variabilities in the band length, band thickness and band length ratio are summarised in Table 3. The linear correlations between the measurements (Spearman’s correlation coefficient) were considered to be in good agreement (>0.7) for all measurements.
Table 3. Interobserver variability in the measurement of MR images.
| Mean difference (SD) | 95% CI | R | |
| Band length (mm) | |||
| Observer 1–2 | 0.076 (1.656) | (−0.607, 0.760) | 0.939 |
| Observer 2–3 | −0.148 (1.323) | (−0.694, 0.398) | 0.945 |
| Observer 3–1 | 0.072 (1.676) | (−0.619, 0.764) | 0.926 |
| Band thickness (mm) | |||
| Observer 1–2 | 0.164 (0.312) | (0.035, 0.293) | 0.816 |
| Observer 2–3 | −0.160 (0.314) | (−0.292, −0.032) | 0.743 |
| Observer 3–1 | −0.220 (0.392) | (−0.382, −0.057) | 0.809 |
| Band length ratio (%) | |||
| Observer 1–2 | 0.112 (4.720) | (−1.837, 2.060) | 0.9701 |
| Observer 2–3 | −0.412 (3.720) | (−1.947, 1.123) | 0.9712 |
| Observer 3–1 | 0.300 (4.747) | (−1.659, 2.259) | 0.9773 |
95% CI, 95% confidence interval; R, Spearman’s correlation coefficient.
Discussion
One of the important differential diagnoses in determining SIF is osteonecrosis. The shape of the very low signal-intensity band on T1 weighted MRI is a characteristic finding of SIF: it is generally irregular, serpiginous, convex to the articular surface and is often discontinuous [2,4,5,7,9,11]. Histopathologically, the band in SIF represents the fracture line with associated repair tissue [5,9]. Conversely, in osteonecrosis, because the low-intensity band represents repair tissue, it is generally smooth and circumscribes all of the necrotic segments [4,5,7,9,11]. In this study, in the 15 patients who underwent surgery, the diagnosis of SIF was histologically confirmed. The low-intensity band histologically corresponded to the fractured bone trabeculae with callus formation and vascular granulation tissue. In addition, in the 10 patients without a progression of the collapse, the abnormal findings on MRI (bone marrow oedema and low signal-intensity band) had disappeared at the time of the latest follow-up.
Previous histological studies showed that the portion proximal to the low-intensity band generally consisted of viable bone tissue in SIF and of necrotic tissue in osteonecrosis [4,5,10]. Therefore, on enhanced MRI, both the low-intensity band and the proximal portion tended to show high intensity in SIF [8,10]. However, in osteonecrosis, because the proximal portion beyond the band is an osteonecrotic area, this portion is not enhanced. In this study, only 9 of 25 patients underwent an enhanced MRI on which the low-intensity band, as well as the proximal portion, showed high intensity. In our institution, enhanced MRI is performed only for cases in which it is difficult to differentiate SIF from osteonecrosis by non-enhanced MRI.
Because the band in SIF corresponds to the fracture line, the band length represents the extent of a subchondral fracture and the band length ratio represents the proportion of a subchondral fracture to the weight-bearing portion of the femoral head. As shown in the present study, the extent of a subchondral fracture and the ratio to the femoral head are both important for making an accurate prognosis of SIF. We assumed that the longer band in the weight-bearing portion indicates a mechanically weakened subchondral condition. This weakening causes a further collapse and the incongruity of the femoral head, eventually resulting in osteoarthritic changes. It remains unclear which portion of the femoral head is the common site for SIF, but in most of the present cases the fracture line extended from the superior portion to the anterosuperior portion of the femoral head. Therefore, both the longest and the thickest band were observed at the slice through the femoral head centre or at one or more anterior slices on T1 weighted MRI in the coronal plane, indicating that SIFs are generally eccentric (anterosuperior portion).
A subchondral fracture of the femoral head has been observed in young military trainees; however, such cases are considered to result from fatigue stress fractures and all cases healed after conservative treatment [18,19]. In the present study, five patients were under 50 years of age and three were under 30 years of age. Only one patient had participated in sports activities (badminton in high school), while no patients in this series had any history of overexertion. The histological findings showed thin disconnected bone trabeculae, thus indicating the presence of some degree of osteopenia. Therefore, these young patients were all considered to demonstrate an insufficiency fracture rather than a fatigue stress fracture.
In the present study, 12 patients underwent an arthroplasty and 3 patients underwent an anterior rotational osteotomy owing to the progression of the collapse and increased hip pain. Although the indications for surgery in SIF remain unclear, if a progression of the collapse is observed despite conservative treatment then surgical intervention might be necessary.
The major limitations of this study were the small sample size and the fact that it was performed as a retrospective observational study. The small sample size meant that a multivariate analysis was not feasible and it was also not possible to determine whether effects were independent. Because SIF is a newly proposed concept and is not commonly observed, a large prospective study was not available. Another limitation was the large variation in the follow-up times. It is likely that some patients have insufficient follow-up examinations. In the present study, however, the progression of the collapse occurred within 2 months in all patients. The progression of collapse is thus determined within several months from the onset of symptoms; therefore, the follow-up period appeared to be sufficient to investigate the prognosis of SIF.
In the present study, neither age nor Singh’s index were significant factors for the prognosis of SIF, while Singh’s index seems inadequate to precisely assess osteopenia of the femoral head. A further investigation in a larger number of cases with the measurements of bone mineral density is necessary to clarify whether age and the degree of osteoporosis affect the patient prognosis of SIF.
In the current study, the prognosis of SIF varied even though all patients received similar conservative treatment. If the prognosis for SIF can be predicted at an early stage, it would allow the design of optimal treatments for each patient. In this preliminary investigation, both the band length and band length ratio were demonstrated to be useful in predicting femoral head collapse in SIF.
Acknowledgments
This work was supported by a Grant-in-Aid in Scientific Research (No.21591948) from the Japanese Society for the Promotion of Science, a Research Grant for Intractable Diseases from the Ministry of Health and Welfare of Japan and a grant from the Takeda Science Foundation.
References
- 1.Bangil M, Soubrier M, Dubost JJ, Rami S, Carcanagues Y, Ristori JM, et al. Subchondral insufficiency fracture of the femoral head. Rev Rhum Engl Ed 1996;63:859–61 [PubMed] [Google Scholar]
- 2.Rafii M, Mitnick H, Klug J, Firooznia H. Insufficiency fracture of the femoral head: MRI in three patients. AJR Am J Roentgenol 1997;168:159–63 [DOI] [PubMed] [Google Scholar]
- 3.Vande Berg B, Malghem J, Goffin EJ, Duprez TP, Maldague BE. Transient epiphyseal lesions in renal transplant recipients: presumed insufficiency stress fractures. Radiology 1994;191:403–7 [DOI] [PubMed] [Google Scholar]
- 4.Yamamoto T, Bullough PG. Subchondral insufficiency fracture of the femoral head: a differential diagnosis in acute onset of coxarthrosis in the elderly. Arthritis Rheum 1999;42:2719–23 [DOI] [PubMed] [Google Scholar]
- 5.Yamamoto T, Schneider R, Bullough PG. Subchondral insufficiency fracture of the femoral head: histopathologic correlation with MRI. Skeletal Radiol 2001;30:247–54 [DOI] [PubMed] [Google Scholar]
- 6.Hagino H, Okano T, Teshima R, Nishi T, Yamamoto K. Insufficiency fracture of the femoral head in patients with severe osteoporosis: report of 2 cases. Acta Orthop Scand 1999;70:87–9 [DOI] [PubMed] [Google Scholar]
- 7.Yamamoto T, Takabatake K, Iwamoto Y. Subchondral insufficiency fracture of the femoral head resulting in rapid destruction of the hip joint: a sequential radiographic study. AJR Am J Roentgenol 2002;178:435–7 [DOI] [PubMed] [Google Scholar]
- 8.Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Subchondral insufficiency fracture of the femoral head in younger adults. Skeletal Radiol 2007;36:S38–S42 [DOI] [PubMed] [Google Scholar]
- 9.Yamamoto T, Schneider R, Bullough PG. Insufficiency subchondral fracture of the femoral head. Am J Surg Pathol 2000;24:464–8 [DOI] [PubMed] [Google Scholar]
- 10.Miyanishi K, Hara T, Kaminomachi S, Maeda H, Watanabe H, Torisu T. Contrast-enhanced MRI of subchondral insufficiency fracture of the femoral head: a preliminary comparison with that of osteonecrosis of the femoral head. Arch Orthop Trauma Surg 2009;129:583–9 [DOI] [PubMed] [Google Scholar]
- 11.Ikemura S, Yamamoto T, Nakashima Y, Shuto T, Jingushi S, Iwamoto Y. Bilateral subchondral insufficiency fracture of the femoral head after renal transplantation: a case report. Arthritis Rheum 2005;52:1293–6 [DOI] [PubMed] [Google Scholar]
- 12.Vande Berg BC, Lecouvet FE, Koutaissoff S, Simoni P, Malghem J. Bone marrow edema of the femoral head and transient osteoporosis of the hip. Eur J Radiol 2008;67:68–77 [DOI] [PubMed] [Google Scholar]
- 13.Legroux Gerot I, Demondion X, Louville AB, Delcambre B, Cortet B. Subchondral fractures of the femoral head: a review of seven cases. Joint Bone Spine 2004;71:131–5 [DOI] [PubMed] [Google Scholar]
- 14.Buttaro M, Della Valle AG, Morandi A, Sabas M, Pietrani M, Piccaluga F. Insufficiency subchondral fracture of the femoral head: report of 4 cases and review of the literature. J Arthroplasty 2003;18:377–82 [DOI] [PubMed] [Google Scholar]
- 15.Davies M, Cassar-Pullicino VN, Darby AJ. Subchondral insufficiency fractures of the femoral head. Eur Radiol 2004;14:201–7 [DOI] [PubMed] [Google Scholar]
- 16.Yoshiike N, Matsumura Y, Zaman MM, Yamaguchi M. Descriptive epidemiology of body mass index in Japanese adults in a representative sample from the National Nutrition Survey 1990–1994. Int J Obes Relat Metab Disord 1998;22:684–7 [DOI] [PubMed] [Google Scholar]
- 17.Singh M, Nagrath AR, Maini PS. Changes in trabecular pattern of the upper end of the femur as an index of osteoporosis. J Bone Joint Surg Am 1970;52:457–67 [PubMed] [Google Scholar]
- 18.Song WS, Yoo JJ, Koo KH, Yoon KS, Kim YM, Kim HJ. Subchondral fatigue fracture of the femoral head in military recruits. J Bone Joint Surg 2004;86-A:1917–24 [DOI] [PubMed] [Google Scholar]
- 19.Visuri T. Stress osteopathy of the femoral head: 10 military recruits followed for 5–11 years. Acta Orthop Scand 1997;68:138–41 [DOI] [PubMed] [Google Scholar]