Abstract
Objective
The use of stress cardiovascular MR (CMR) to evaluate myocardial ischaemia has increased significantly over recent years. We aimed to assess the indications, incidental findings, tolerance, safety and accuracy of stress CMR in routine clinical practice.
Methods
We retrospectively examined all stress CMR studies performed at our tertiary referral centre over a 20-month period. Patients were scanned at 1.5 T, using a standardised protocol with routine imaging for late gadolinium enhancement. Angiograms of patients were assessed by an interventional cardiologist blinded to the CMR data.
Results
654 patients were scanned (mean age 65±29 years; 63 inpatients; 9.6%). 14% of patients had incidental extracardiac findings, the commonest being liver or renal cysts (6%) and pulmonary nodules (4%). 639 patients (97.7%) received intravenous adenosine, 10 received intravenous dobutamine and 5 patients had both. Of the 15 patients who received dobutamine, 12 had no side-effects/complications, 2 experienced nausea and 1 chest tightness. Of the 644 patients who received adenosine, 43% experienced minor symptoms, 1% had transient heart block and 0.2% had severe bronchospasm requiring termination of infusion. There were no cases of hospitalisation or myocardial infarction. 241 patients also had coronary angiography. For detecting at least moderate stenosis of ≥50%, sensitivity was 86%, specificity 98% and accuracy 89%. For detecting severe stenoses of ≥70%, sensitivity was 91%, specificity 86% and overall accuracy 90%. These results compare very favourably with previous smaller research studies and meta-analyses.
Conclusion
We conclude that stress CMR, with adenosine as the main stress agent, is well tolerated, safe and accurate in routine clinical practice.
The routine use of stress cardiovascular MR (CMR) to evaluate myocardial ischaemia has increased significantly over the last few years [1,2]. Stress CMR is an attractive non-invasive technique because it does not require radiation exposure, and it can potentially play an important role in the diagnosis and management of patients with coronary artery disease. More recent studies have also demonstrated that stress CMR results have important prognostic value: a negative result predicts a 3-year event-free survival of >99% and a positive result is an independent predictor of future cardiac events [3,4].
Studies are usually performed during first-pass perfusion imaging, using vasodilatory pharmacological stress with either intravenous adenosine or dipyridamole [2]. Adenosine is the most widely used, and, in the presence of coronary stenoses, flow heterogeneities result in regional perfusion defects during first-pass gadolinium contrast imaging. Alternatively, if adenosine is contraindicated, myocardial ischaemia could also be assessed by regional wall motion abnormalities with dobutamine as an inotropic stress agent.
Despite the increasing use of stress CMR clinically, previous research studies have involved relatively small numbers. A recent study examined the safety and tolerance of stress CMR in 351 subjects, but 46 of these were healthy, normal volunteers [5]. A current meta-analysis of 35 studies, which included 13–229 patients, revealed a high sensitivity of 89% but only a moderate specificity of 80% [6].
We therefore aimed to assess a new stress CMR service, as routinely conducted in a single tertiary centre run jointly by a radiologist and a cardiologist, including examining the referral patterns, incidental findings, its safety, tolerance and accuracy.
Methods and materials
We retrospectively reviewed all stress CMR scans reported on our electronic database over 20 months, from the start of the service in April 2007 to December 2008.
Cardiovascular MR protocol
Patients were scanned in a 1.5 T magnet (Siemens Avanto®, Erlangen, Germany) according to a standardised protocol, with routine imaging for late gadolinium enhancement (LGE).
Subjects were screened for contraindications to adenosine (Workhadt UK Ltd, Wrexham, UK), which included severe asthma and second- or third-degree atrioventricular (AV) block, and asked to abstain from caffeine for at least 12 h before the scan. A 12-lead electrocardiogram (ECG) was performed before the CMR scan. Anti-anginal therapies, including beta-blockers, were not discontinued. Intravenous adenosine was infused at 140 μg kg−1 min−1 for at least 2 min (average of 3 min), until a haemodynamic response was achieved (a drop in blood pressure of >10 mmHg and/or a rise in heart rate of >10 bpm). Intravenous dobutamine was used if there was a contraindication to adenosine. To achieve 85% of maximum age-predicted heart rate, patients were given 5–40 μg kg−1 min−1 of dobutamine, and, if necessary, 0.6–1.2 mg of atropine.
Perfusion imaging was performed in every cardiac cycle using a T1 weighted fast gradient echo following the first pass of the gadolinium diethylene triamine pentaacetic acid contrast agent (0.1 mmol kg−1 gadopentetate dimeglumine, Magnevist® (Bayer plc, Newbury, UK); 0.05 mmol kg−1 was used for the seven patients scanned as part of a separate research study; these seven patients, all with severe aortic stenosis, represented only 1% of the total cohort audited, and were not specifically selected into this study, but happened to have had their stress CMR scans performed within the timeframe of this audit). Depending on the heart rate, three or four short axis slices, positioned from the base to the apex of the left ventricle, were obtained. Perfusion imaging was repeated at rest, after short axis steady-state free precession cine images were performed. LGE imaging was then performed with a segmented inversion–recovery technique after 5–10 min. Matched stress–rest perfusion defects in the absence of infarction on LGE were considered to be artefacts [7]. Analysis was performed with Argus Syngo® software (Siemens Healthcare, Erlangen, Germany) and perfusion defects were assessed visually. Patients with homogeneous global subendocardial perfusion defects were reported as probable microvascular dysfunction, especially if left ventricular (LV) hypertrophy was present, but it was stated in the report that epicardial coronary disease could not be excluded. For receiver operating characteristic (ROC) curve analysis, stress CMR results were graded into five categories (normal, probably normal, possibly abnormal, probably abnormal and abnormal). Viable myocardium was defined as myocardial segments with <75% transmural LGE.
Coronary angiography
A proportion of patients (37%) also had coronary angiography within 6 months, either before or after their CMR scan, at the discretion of the referring consultant cardiologist. These coronary angiography images were retrieved and reassessed by an interventional cardiologist, blinded to the CMR data. At least moderate coronary stenoses was defined visually as the presence of at least one luminal stenosis of ≥50% diameter in any of the main epicardial coronary arteries or their branches with a diameter of ≥2 mm. Similarly, severe stenosis was defined visually as the presence of at least one stenosis of ≥70% diameter. We also separately identified arteries which were chronic total occlusions (CTOs) and examined for the extent of reversible perfusion defects and viability on stress CMR.
Statistics
Data were examined for normality and presented as the mean±standard deviation. Analyses, including ROC curves, were performed with SPSS Statistics software v. 17 (SPSS Inc., Chicago, IL).
Results
Patient demographics
A total of 654 patients were scanned within a period of 20 months. The mean age was 65 years and ages ranged from 27 to 89 years. There was a total of 63 inpatients (9.6%). 231 (35%) patients had previous revascularisation, 23% had previous percutaneous coronary intervention, 10% had coronary artery bypass surgery and 2% had both. The majority (639 patients; 97.7%) received intravenous adenosine, 10 received intravenous dobutamine and 5 patients had both.
Indications
Reasons for referral for stress CMR studies are shown in Table 1. Combining the first three categories of patients with chest pain, LV dysfunction or left bundle branch block, a total of 286 (44%) patients did not have previously known coronary disease and stress CMR was requested for evidence of reversible ischaemia to imply underlying significant coronary disease. A further 361 (55%) patients had previous coronary angiography showing coronary disease of at least moderate or indeterminate severity and stress CMR was requested to evaluate the presence and extent of reversible perfusion defects and/or infarction, to guide further intervention. A very small number of patients (1%), who were part of a research study, also had their scans within the timeframe of this study and hence were included.
Table 1. Indications for stress cardiac MR.
| Indication | n | % |
| Chest pain: evidence of reversible perfusion defects? | 129 | 20 |
| Left ventricular dysfunction: evidence of reversible perfusion defects? | 112 | 17 |
| Left bundle branch block: evidence of reversible perfusion defects? | 45 | 7 |
| Known coronary disease: evidence of reversible perfusion defects? | 361 | 55 |
| Part of research study | 7 | 1 |
Of the 129 patients referred with chest pain, stress CMR was positive for reversible perfusion defects in 47 (36%) patients; of the 112 patients referred with LV dysfunction, 51 (46%) had reversible perfusion defects; and, of the 45 patients referred with left bundle branch block, 12 (27%) had reversible perfusion defects. 237 of the 361 (66%) patients with known coronary disease had reversible perfusion defects demonstrated on stress CMR.
Incidental findings
Notable non-coronary cardiac incidental findings, which may account for symptoms or affect patient management, are shown in Table 2. There was a small but not insignificant number of patients with at least moderate valve disease, LV thrombus and cardiomyopathies. Incidental extracardiac findings, present in 13.5% of all scans, included liver or renal cysts (5.8%), lung nodules (3.5%), hiatus hernias (3.1%), left-sided superior vena cava (0.6%), thyroid goitre (0.3%) and subclavian artery stenosis (0.2%). The single patient with left subclavian artery stenosis also had a left internal mammary artery graft and demonstrable stress perfusion defects.
Table 2. Incidental cardiac findings.
| Finding | n | % |
| Valve disease (at least moderate severity) | 40 | 6.1 |
| Left ventricular thrombus | 15 | 2.3 |
| Hypertrophic cardiomyopathy | 12 | 1.8 |
| Non-compaction cardiomyopathy | 3 | 0.5 |
| Restrictive cardiomyopathy | 2 | 0.3 |
| Arrhythmogenic right ventricular cardiomyopathy | 1 | 0.2 |
| Left atrial lipoma | 1 | 0.2 |
Tolerance and safety
Of the 15 patients who received dobutamine, 12 had no side-effects/complications, 2 experienced nausea and 1 chest tightness. None required intervention and there were no major complications such as hospitalisation, myocardial infarction or death.
With adenosine, the systemic blood pressure dropped, on average, from 144/82 to 131/73 mmHg, and the heart rate rose from 68 to 88 bpm. Tolerance and safety data for all 644 patients who received adenosine are shown in Table 3. As expected, adenosine infusion did result in common minor symptoms in nearly half of all patients. The incidence of transient second-degree heart block was low (overall 1.1%) and there was no sustained advanced heart block. 27 (4%) patients required midazolam sedation for the CMR study.
Table 3. Symptoms and complications from adenosine stress.
| Symptom or complication | n | % |
| Minor symptoms (chest pain, breathlessness) | 285 | 43 |
| Adenosine discontinued prematurely | 12 | 1.9 |
| Reasons: | ||
| Claustrophobia | 4 | 0.6 |
| Significant hypotension | 3 | 0.5 |
| Transient heart block | 2 | 0.3 |
| Significant sinus bradycardia | 1 | 0.2 |
| Bronchospasm | 1 | 0.2 |
| Severe chest pain | 1 | 0.2 |
| Scanner breakdown | 1 | 0.2 |
| Transient heart block | 5 | 0.8 |
| Medical intervention (bronchodilators) | 4 | 0.6 |
| Hospitalisation | 0 | 0 |
| Myocardial infarction or death | 0 | 0 |
Accuracy
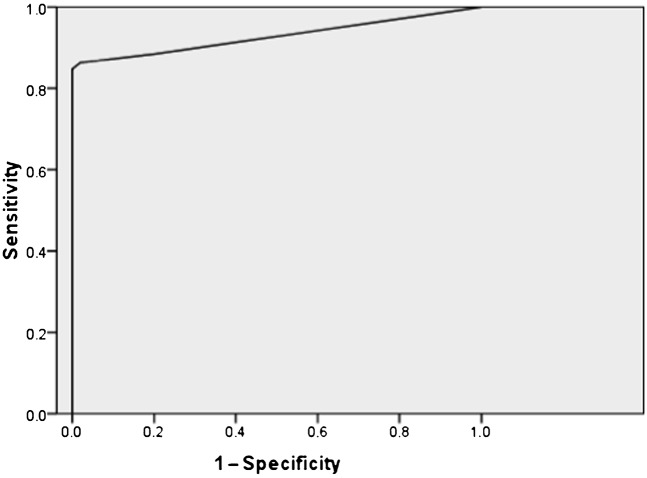
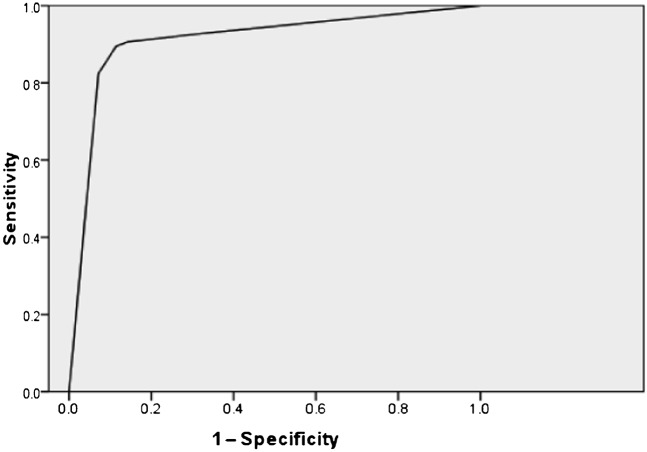
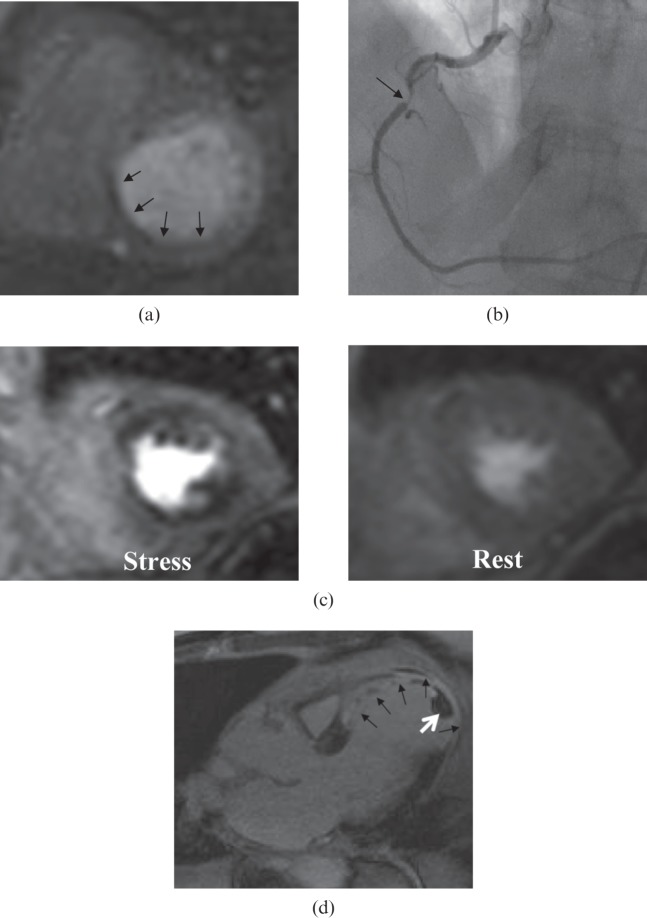
241 patients (37%) had invasive coronary angiography within 6 months of their CMR scan. ROC curve analyses for detecting significant stenoses of ≥50% and ≥70% are shown in Figures 1 and 2, respectively. An example of a stress-induced perfusion defect correlating to a severe right coronary artery stenosis and an LGE image with transmural infarction and associated apical left ventricular thrombus are shown in Figure 3.
Figure 1.
Receiver operating characteristic curve analysis for detection of moderate coronary artery stenoses of ≥50%. The area under the curve is 0.93±0.16.
Figure 2.
Receiver operating characteristic curve analysis for detection of severe coronary artery stenoses of ≥70%. The area under the curve is 0.91±0.02.
Figure 3.
(a) Stress-induced perfusion defect in the inferoseptal and inferior walls on first-pass perfusion imaging (arrows). (b) Correlating severe right coronary artery stenosis on coronary angiography (arrow). (c) Global subendocardial perfusion defects in a patient with severe triple-vessel coronary disease (stress perfusion image on the left, and comparative rest perfusion image on the right). (d) Late gadolinium enhancement image showing transmural infarction (non-viable myocardium) in the territory of the left anterior descending artery (black arrows), and an associated apical thrombus (white arrow) in the left ventricle.
For detection of moderate coronary stenosis (≥50%), the area under the curve (AUC) is 0.93±0.16, with a prevalence of 79%. The overall sensitivity is 86%, specificity 98% and accuracy 89%. The positive predictive value (PPV) is 99% and negative predictive value (NPV) is 66%.
For detection of severe coronary stenosis (≥70%), the AUC is 0.91±0.02 with a prevalence of 71%. The overall sensitivity is 91%, specificity 86% and accuracy 90%. The PPV is 94% and NPV is 79%.
Chronic total occlusions
We identified the arteries which contained CTOs, and, in the myocardial territory supplied by the artery, we reported the extent of infarction/viability with LGE and the number of segments with reversible perfusion defects on stress CMR. The results, analysed for each coronary artery, are shown in Table 4. Overall, in 28% of CTOs, the myocardial territory supplied was non-viable, implying that revascularisation would not be appropriate. A further 9% of CTOs supplied myocardium containing both non-viable segments and segments showing reversible perfusion defects. The majority of CTOs (63%) supplied viable myocardium with demonstrable reversible perfusion defects. All viable myocardium supplied by CTOs had stress-induced reversible perfusion defects but the extent seen was very variable (between one and seven segments).
Table 4. Non-viable myocardium, and segments with reversible perfusion defects in chronically occluded arteries.
| Artery | n | Non-viable | RPD | Mixed | No. of segments |
| LAD | 29 | 11 (38%) | 14 (48%) | 4 (14%) | 3.9±2.2 |
| CX | 10 | 2 (20%) | 7 (70%) | 1 (10%) | 3.3±1.8 |
| RCA | 50 | 12 (24%) | 35 (70%) | 3 (6%) | 3.8±1.4 |
| Total | 89 | 25 (28%) | 56 (63%) | 8 (9%) | 3.6±1.7 |
CX, circumflex artery; LAD, left anterior descending artery; RCA, right coronary artery.
‘Mixed’ implies that the myocardial territory supplied contained both non-viable and segments with reversible perfusion defects (RPDs); number of segments with RPDs is shown as the mean±standard deviation.
Discussion
We believe that this study is important at a time when stress CMR is rapidly expanding and may be particularly relevant for centres considering opening a new service. We have shown that, in daily practice, stress CMR is safe, well tolerated and accurate.
There were a few significant non-coronary cardiac findings which may account for symptomatology or influence management, which other functional stress imaging modalities may not be able to provide. For example, LV thrombus and subtle cardiomyopathies may be missed by echocardiography [8].
Stress CMR studies were well tolerated. Most patients experienced common, minor side-effects with adenosine, similar to those reported in previous studies [5,6]. There were only 12 patients in whom the infusion was terminated early. Reasons included claustrophobia, significant hypotension, significant transient heart block or bradycardia, bronchospasm and severe chest pain. The scanner unfortunately malfunctioned in one case. Only 4% of patients required midazolam sedation. Although midazolam could potentiate the effects of adenosine in previous animal studies, this was not validated in a human study [9], and it is therefore unlikely to influence adenosine stress perfusion.
The safety profile was also excellent, even in this cohort of patients with a high prevalence of significant coronary disease. There were a significant number of inpatients (10%), the majority of whom were admitted with troponin-positive acute coronary syndrome or ST elevation myocardial infarction. Our study supports previous work showing that stress CMR is safe, even in patients admitted with acute ST elevation myocardial infarcts [10]. The total incidence of heart block reported was lower (1.1%) than in a previous smaller study of 351 subjects (8%), also in a population with a high prevalence of coronary disease [5]. Only four patients required the use of bronchodilators for bronchospasm and there were no major complications. Bernhardt et al [11] further demonstrated that adenosine stress CMR was safe to be performed in a mobile scanner, without any major complications. A further study by Bernhardt et al [12] also demonstrated an excellent safety profile in 3174 outpatients referred for evaluation of suspected ischaemic heart disease with adenosine stress CMR. They did not include inpatients, whereas about 10% of our cohort were inpatients, proving that stress CMR is safe even in this population. Our data reflect mainly the use of adenosine as the stress agent in the majority of our patients. We accept that, as only 15 patients received dobutamine, the numbers are too few to draw definitive conclusions about dobutamine stress CMR. Although there are few data supporting the need for a 12-lead ECG to be performed before a stress CMR study, this continues to be routine practice in many centres. A pre-procedural ECG may be helpful in ruling out pre-existing second-degree AV or complete heart block, and can be useful as a baseline comparison, should the patient develop persistent chest pain with ischaemic ST segment changes following stress.
In terms of accuracy, our results compare very favourably with previously published smaller research studies and meta-analyses. As expected, there is increased sensitivity at the expense of decreased specificity, when the threshold for defining significant stenoses moved from 50% to 70%. Using a similar visual assessment protocol on 92 patients with routine imaging for LGE, Klem et al [7] reported a sensitivity of 89%, specificity of 87% and accuracy of 88%, for the detection of ≥70% stenoses. For the detection of ≥50% stenoses, they reported a sensitivity of 77%, specificity of 88% and accuracy of 83%. As advocated by Klem et al [7], LGE imaging is very sensitive for infarction and its routine use significantly improves the specificity for ischaemia detection with adenosine stress CMR (from 58% to 87%). The prevalence of moderate coronary disease (defined as ≥50% stenoses) was 40% in that study and there was uncertainty as to how this strategy would perform in a population with a higher prevalence of disease. With a high prevalence of moderate stenoses in our cohort (79%), we have now shown that accuracy was certainly comparable using a similar interpretation protocol.
A previous meta-analysis for detection of ≥70% stenoses showed an overall sensitivity of 91% and specificity of 81% [13]. A more recent meta-analysis of 35 studies [6], which included 13–229 patients, again revealed a similar, high sensitivity of 89% but a moderate specificity of 80%. 18 of the studies included in the latter meta-analysis used perfusion analyses alone, without cine or LGE imaging, and this may explain the lower specificity. The low specificity may also be due to perfusion defects caused by dark rim artefacts or Gibbs phenomenon (low intensities seen in the endocardial border during first pass of the contrast, probably due to a combination of the bolus injection, resolution and motion). Alternatively, as in a few of our cases, the presence of microvascular disease in hypertrophic cardiomyopathy could also result in global subendocardial perfusion defects mimicking triple-vessel coronary disease. Sensitivity may further improve with higher field strength magnets (3 T), owing to better signal-to-noise and contrast-to-noise ratios [14].
This is a “real world” study and hence not all patients have had coronary angiography close to the time of their CMR scan for comparison when not clinically indicated. Indeed, most patients with negative stress CMR results did not have coronary angiography and this would explain the low NPVs in our study. Additionally we did not stop anti-anginal medication and therefore this may have reduced the amount of ischaemia associated with severe coronary stenosis. A recent study of 158 patients referred for coronary angiography specifically looked at the NPV of normal adenosine stress CMR prior to angiography [15]. It found a very high NPV for coronary disease (96%), supporting CMR-based decision-making for the indication to coronary angiography. In addition, semi-quantitative perfusion analysis gave significantly prolonged arrival time index and peak time index in the false-negative group, and this may further improve accuracy. A separate study also found that quantitative perfusion reserve analysis may be helpful in differentiating moderate from severe stenoses [16]. However, performing such quantitative analyses may be time-consuming and not applicable to current practice. We demonstrated a high degree of accuracy using a visual, qualitative assessment alone.
Coronary angiography, although currently accepted as the “gold standard”, provides anatomical (luminal) data, with no assessment of the haemodynamic significance of stenoses—the use of 50% or 70% stenosis to indicate moderate and severe stenoses can be regarded as arbitrary, as the true functional significance may vary. Furthermore, angiographic data are obtained in several single planes, and assessment is usually performed qualitatively rather than quantitatively in clinical practice, resulting in operator bias. We also used visual, qualitative assessment of the coronary anatomy in our study, which itself is a limitation. In contrast, stress CMR provides functional data on myocardial ischaemia. Direct comparison may not be appropriate, without the use of additional pressure wire assessment for fractional flow reserve (FFR) during angiography [17]. A recent study comparing adenosine stress CMR with FFR showed that stress CMR had an excellent sensitivity of 91% and specificity of 94%, with PPVs and NPVs of 91% and 94% [18].
Patients were asked to abstain from caffeine for 24 h prior to their CMR scan but we did not test for caffeine levels. However, this is unlikely to influence the accuracy of the stress CMR results, as it has previously been demonstrated that even those patients who consume coffee within 1–2 h before scanning and reach peak levels of caffeine during adenosine infusion may have a similar haemodynamic response to patients who had no caffeine [19]. Lack of an observed haemodynamic response to adenosine may imply inadequate stress and hence reduce the sensitivity of the test. For a few of our patients, adenosine infusion was prolonged if there was initial lack of haemodynamic response. A recent study has shown good safety data using higher adenosine infusion rates in non-responders, and this may be a feasible option to overcome this problem [20].
Revascularisation for CTO is potentially challenging and not without clinical risk [21]. Clinicians within our institution are increasingly requesting stress CMR for evidence of viability and significant reversible perfusion defects before considering intervention. We found that, in 28% of CTOs, the myocardial territory supplied was completely non-viable, implying that revascularisation would not be appropriate. Even in the majority of CTOs which supplied viable, ischaemic myocardium, the degree of ischaemia was very variable, which is likely to be influenced by collateral flow. Therefore, if the decision to revascularise a CTO is primarily based on the ischaemic burden then stress CMR is useful. A small stress CMR study of 20 patients [22] found that pre-interventional stress-induced perfusion defects and wall motion abnormalities in viable myocardium disappeared after successful percutaneous recanalisation of CTOs. We realise that the CTO subgroup within our study is small and larger studies focusing on this group would be required to draw more definitive conclusions.
There is a high prevalence of coronary artery disease among our patients. This is because we selectively route patients with LV dysfunction or previous myocardial infarction to stress CMR and those patients who have a negative scan are very unlikely to subsequently have angiography within the 6-month time frame we used in this study. Hence, our findings may not necessarily apply in the wider population or in a different non-tertiary setting.
Despite the above limitations, we believe our study provides an important and timely audit of routine stress CMR practice. We have verified that, in daily practice, a protocol combining visual assessment of perfusion defects and LGE infarct imaging can accurately diagnose coronary artery disease. With the increasing use of stress CMR, protocols should be standardised and there may be a basis for a wider, multicentre audit.
Conclusions
Stress CMR, with adenosine as the main stress agent, is well tolerated, safe and has excellent accuracy for the detection of obstructive coronary artery disease in routine clinical practice. In addition, CMR can occasionally provide useful non-coronary data that may be clinically relevant. This study would strongly support the wider use of stress CMR in the routine management of patients with known or suspected coronary disease.
Acknowledgments
We thank Dr Natalie Austin for help in data collection and Dr Miroslav Munclinger for reporting the angiograms.
Footnotes
CDS and GPM are supported in part by the National Institute of Health Research Leicester Cardiovascular Biomedical Research Unit.
References
- 1.van derWall EE, Vliegen HW, de Roos A, Bruschke AV. Magnetic resonance imaging in coronary artery disease. Circulation 1995;92:2723–39 [DOI] [PubMed] [Google Scholar]
- 2.Gerber BL, Raman SV, Nayak K, Epstein FH, Ferreira P, Axel L, et al. Myocardial first-pass perfusion cardiovascular magnetic resonance: history, theory, and current state of the art. J Cardiovasc Magn Reson 2008;10:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pilz G, Jeske A, Klos M, Ali E, Hoefling B, Scheck R, et al. Prognostic value of normal adenosine-stress cardiac magnetic resonance imaging. Am J Cardiol 2008;101:1408–12 [DOI] [PubMed] [Google Scholar]
- 4.Jahnke C, Nagel E, Gebker R, Kokocinski T, Kelle S, Manka R, et al. Prognostic value of cardiac magnetic resonance stress tests: adenosine stress perfusion and dobutamine stress wall motion imaging. Circulation 2007;115:1769–76 [DOI] [PubMed] [Google Scholar]
- 5.Karamitsos TD, Arnold JR, Pegg TJ, Cheng AS, van Gaal WJ, Francis JM, et al. Tolerance and safety of adenosine stress perfusion cardiovascular magnetic resonance imaging in patients with severe coronary artery disease. Int J Cardiovasc Imaging 2009;25:277–83 [DOI] [PubMed] [Google Scholar]
- 6.Hamon M, Fau G, Née G, Ehtisham J, Rémy M, Hamon M. Meta-analysis of the diagnostic performance of stress perfusion cardiovascular magnetic resonance for detection of coronary artery disease. J Cardiovasc Magn Reson 2010;12:29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Klem I, Heitner JF, Shah DJ, Sketch MH, Jr, Behar V, Weinsaft J, et al. Improved detection of coronary artery disease by stress perfusion cardiovascular magnetic resonance with the use of delayed enhancement infarction imaging. J Am Coll Cardiol 2006;47:1630–8 [DOI] [PubMed] [Google Scholar]
- 8.Rickers C, Wilke NM, Jerosch-Herold M, Casey SA, Panse P, Panse N, et al. Utility of cardiac magnetic resonance imaging in the diagnosis of hypertrophic cardiomyopathy. Circulation 2005;112:855–61 [DOI] [PubMed] [Google Scholar]
- 9.van Ginneken EE, Drooglever-Fortuyn H, Smits P, Rongen GA. The influence of diazepam and midazolam on adenosine-induced forearm vasodilation in humans. J Cardiovasc Pharmacol 2004;43:276–80 [DOI] [PubMed] [Google Scholar]
- 10.Greenwood JP, Younger JF, Ridgway JP, Sivananthan MU, Ball SG, Plein S. Safety and diagnostic accuracy of stress cardiac magnetic resonance imaging vs exercise tolerance testing early after acute ST elevation myocardial infarction. Heart 2007;93:1363–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bernhardt P, Steffens M, Kleinertz K, Morell R, Budde R, Leischik R, et al. Safety of adenosine stress magnetic resonance imaging using a mobile cardiac magnetic resonance system. J Cardiovasc Magn Reson 2006;8:475–8 [DOI] [PubMed] [Google Scholar]
- 12.Bernhardt P, Levenson B, Engels T, Strohm O. Contrast-enhanced adenosine-stress magnetic resonance imaging: feasibility and practicability of a protocol for detection or exclusion of ischemic heart disease in an outpatient setting. Clin Res Cardiol 2006;95:461–7 [DOI] [PubMed] [Google Scholar]
- 13.Nandalur KR, Dwamena BA, Choudhri AF, Nandalur MR, Carlos RC. Diagnostic performance of stress cardiac magnetic resonance imaging in the detection of coronary artery disease. J Am Coll Cardiol 2007;50:1343–53 [DOI] [PubMed] [Google Scholar]
- 14.Cheng AS, Pegg TJ, Karamitsos TD, Searle N, Jerosch-Herold M, Choudhury RP, et al. Cardiovascular magnetic resonance perfusion imaging at 3-tesla for the detection of coronary artery disease: a comparison with 1.5-tesla. J Am Coll Cardiol 2007;49:2440–9 [DOI] [PubMed] [Google Scholar]
- 15.Pilz G, Eierle S, Heer T, Klos M, Ali E, Scheck R, et al. Negative predictive value of normal adenosine-stress cardiac MRI in the assessment of coronary artery disease and correlation with semiquantitative perfusion analysis. J Magn Reson Imaging 2010;32:615–21 [DOI] [PubMed] [Google Scholar]
- 16.Patel AR, Antkowiak PF, Nandalur KR, West AM, Salerno M, Arora V, et al. Assessment of advanced coronary artery disease: advantages of quantitative cardiac magnetic resonance perfusion analysis. J Am Coll Cardiol 2010;56:561–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rieber J, Huber A, Erhard I, Mueller S, Schweyer M, Koenig A, et al. Cardiac magnetic resonance perfusion imaging for the functional assessment of coronary artery disease: a comparison with coronary angiography and fractional flow reserve. Eur Heart J 2006;27:1465–71 [DOI] [PubMed] [Google Scholar]
- 18.Watkins S, McGeoch R, Lyne J, Steedman T, Good R, McLaughlin MJ, et al. Validation of magnetic resonance myocardial perfusion imaging with fractional flow reserve for the detection of significant coronary heart disease. Circulation 2009;120:2207–13 [DOI] [PubMed] [Google Scholar]
- 19.Zoghbi GJ, Htay T, Aqel R, Blackmon L, Heo J, Iskandrian AE. Effect of caffeine on ischemia detection by adenosine single-photon emission computed tomography perfusion imaging. J Am Coll Cardiol 2006;47:2296–302 [DOI] [PubMed] [Google Scholar]
- 20.Karamitsos TD, Ntusi NA, Francis JM, Holloway CJ, Myerson SG. Neubauer S. Feasibility and safety of high-dose adenosine perfusion cardiovascular magnetic resonance. J Cardiovasc Magn Reson 2010;12:66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Galla JM, Whitlow PL. Coronary chronic total occlusion. Cardiol Clin 2010;28:71–9 [DOI] [PubMed] [Google Scholar]
- 22.Heyne JP, Goernig M, Feger J, Kurrat C, Werner GS, Figulla HR, et al. Impact on adenosine stress cardiac magnetic resonance for recanalisation and follow up of chronic total coronary occlusions. Eur J Radiol 2007;63:384–90 [DOI] [PubMed] [Google Scholar]