Abstract
Objective
To evaluate volumetric changes of parotid glands (PGs) during intensity-modulated radiotherapy (IMRT) in head and neck cancer patients.
Methods
During IMRT all patients underwent kilovolt cone-beam CT (CBCT) scans to verify the set-up positioning in a protocol study. On each CBCT scan, the PGs were retrospectively contoured and evaluated with a dose–volume histogram.
Results
From February to June 2011, 10 patients were enrolled. 140 CBCT scans were registered (280 PGs): for each patient, a median of 14 CBCT scans were performed (range 14–16). At the start of radiation, the average volume for ipsilateral PGs (iPGs) was 18.77 ml (range 12.9–31.2 ml), whereas for contralateral PGs (cPGs) it was 16.63 ml (range 8.3–28.7 ml). At the last CBCT scan, the average volume loss was 43.5% and 44.0% for the iPG and cPG, respectively. When we analysed the percentage of volume loss, we observed that the volume decreased by linear regression (r2=0.92 for iPG; r2=0.91 for cPG), with an average volume loss rate of 1.5% per day for both PGs. During the third week of treatment the volume of both PGs reduced by 24–30%.
Conclusion
Our data show that, during IMRT, the shrinkage of PGs should be taken into account. A replan could be indicated in the third week of radiotherapy.
Radiotherapy (RT) has played an important role in the treatment of patients affected by head and neck cancer, despite the risk of side-effects. The introduction of high conformal techniques, such as intensity-modulated RT (IMRT), has increased the possibility of sparing the parotid glands (PGs), reducing the incidence of severe xerostomia compared with conformal RT [1]. During RT, the organs at risk (OARs) and the target change their position and/or volume, and this could modify the dosimetry of the planned radiation treatment: the OARs and target could receive a higher or lower dose, respectively [2-6]. Several studies have shown that the shrinkage of the PGs could alter the dose to the glands [2,7-9]; therefore, in selected patients, replanning is recommended during the IMRT course. In a recent analysis, Ricchetti et al [10] concluded that some OARs underwent volumetric reduction, but the PGs showed the major change, with implications for daily dose distribution. Nishimura et al [11] reported that the volume of the PGs decreased from 43.1 to 32.0 ml in the third week of a 4-week course of IMRT (p<0.001), and another study [12] highlighted that the volume loss of the PGs correlated with the radiation dose (p<0.001). To observe shrinkage of the PGs, image-guided RT (IGRT) was used because it allows changes to be made to correct set-up errors (systematic and random) and/or to take account of tissue changes, increasing the radiation dose to the target [13-20]. In our institution, a Trilogy® Varian System (Varian, Palo Alto, CA) with cone-beam CT (CBCT) and a Brain Lab Exact Track® (Brain Lab, Munich, Germany) were used to verify the set-up positioning.
The aim of this analysis was to evaluate the volumetric changes of PGs during a course of IMRT for head and neck carcinoma in patients enrolled in our prospective study to evaluate IGRT systems.
Methods and materials
Patients
Patients aged 18 years or older, with histologically proven head and neck cancer and treated with definitive IMRT, were enrolled in this study.
Immobilisation of the patients during treatment was achieved using a thermoplastic mask and the Type S-Fixator® (Civco, Orange City, IA). A treatment-planning CT was acquired in the treatment position (2.5 mm). Radiation Therapy Oncology Group guidelines were used to contour all structures. All IMRT the treatment-planning CTs were performed with the treatment planning system Eclipse® v. 8.6 (Varian Medical System).
IMRT total doses (5 days per week over 7 weeks) were as follows: 66–72 Gy to the macroscopic disease clinical target volume (CTV1); 60 Gy to the microscopic high-risk disease (CTV2); and 54–58 Gy to the microscopic low-risk disease (CTV3).
Each CTV was expanded by 5 mm to the corresponding planning target volume. Our IMRT approach involves a seven-field sliding window technique.
Every other day, during radiation all patients underwent kilovolt CBCT scans to verify the set-up positioning. A CBCT low-dose head model was used to generate images with “full-fan” acquisition, in which 360 projections are acquired over a gantry rotation of 200°. To reduce the dose to patients, clockwise and anticlockwise gantry rotation was used alternately [21]. CBCT images were obtained with a slice thickness of 2.5 mm and registered with the planning CT images [three-dimensional (3D)/3D match]. The position of each patient was adjusted based on the CBCT 3D/3D match.
On each CBCT scan, the PGs (right, left and both) were retrospectively contoured and evaluated with a dose–volume histogram. The PGs were contoured by a single observer (AF) and subsequently reviewed by another radiation oncologist (VF).
Statistics
For each CBCT scan during treatment and each patient, we analysed the absolute and the relative variation in the volume of the PGs. The average percentage changes in the volume of the PGs (right, left and both) during IMRT were described and used to analyse the overall data.
Results
Patients
From February to June 2011, 10 patients were analysed (Table 1). All patients completed IMRT, except for two: one patient died from another disease and missed four fractions, and the other patient did not receive the last fraction because of Grade 4 skin toxicity (the patient underwent radiochemotherapy with cisplatin and cetuximab).
Table 1. Patients' characteristics.
| Sex | Age (years) | Subsite | TN stage | Histology | Concurrent CT |
| F | 41 | Oral cavity | T4N0M0 | SCC | Yes |
| M | 46 | Tonsil | T4N2cM0 | SCC | Yes |
| F | 54 | Oral cavity | T4N2M0 | SCC | Yes |
| F | 60 | Oral cavity | T2N0M0 | SCC | Yes |
| M | 63 | Hypopharynx | T3N0M0 | SCC | Yes |
| M | 48 | Tonsil | T2N0M0 | SCC | Yes |
| M | 77 | Oropharynx | T3N1M0 | SCC | No |
| M | 77 | Oral cavity | T4N1M0 | SCC | No |
| M | 48 | Tonsil | T2N1M0 | SCC | Yes |
| M | 54 | Oral cavity | T3N0M0 | SCC | Yes |
F, female; M, male; SCC, squamous cell carcinoma.
Parotid gland volume changes
140 CBCT scans were registered: for each patient, a median of 14 scans were performed (range 14–16). 280 PGs were recontoured and evaluated.
The average mean dose for ipsilateral PG (iPG) and contralateral PG (cPG) was 33.0 Gy (range 24.9–36.0 Gy) and 31.0 Gy (range 23.9–37.0 Gy), respectively.
At the start of radiation, the average volume for the iPG was 18.77 ml (range 12.9–31.2 ml), whereas for the cPG it was 16.63 ml (range 8.3–28.7 ml). At the last CBCT scan, the average volumes were 10.6 ml (range 6.2–24.2 ml) and 9.3 ml (range 5.2–19.5 ml) for iPG and cPG, respectively.
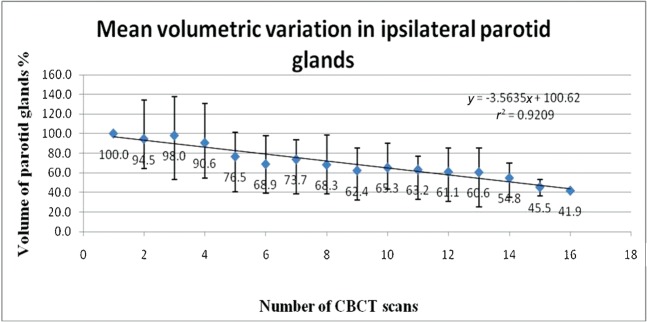
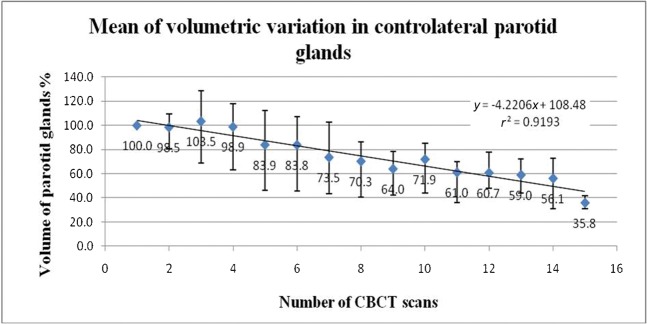
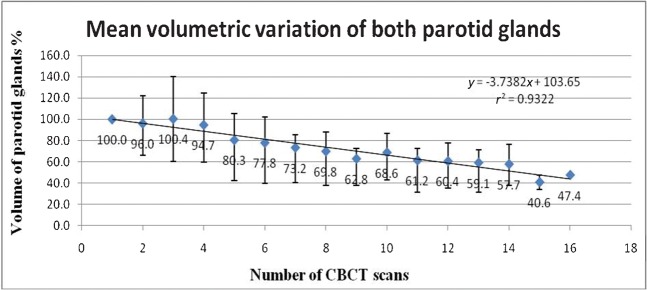
When we analysed the mean volumetric change for each PG, we observed that the volume decreased (Figure 1) by linear regression (Figure 2: r2=0.92 for iPG; Figure 3: r2=0.91 for cPG). The volume loss rate was 1.6% and 1.8% every day of treatment for iPG and cPG, respectively. The overall average mean volume for both PGs during IMRT is shown in Figure 4 (r2=0.93): the average volume loss rate was 1.5% per day. From the 10th to the 20th day of treatment, the volume of both PGs decreased by 15–30%.
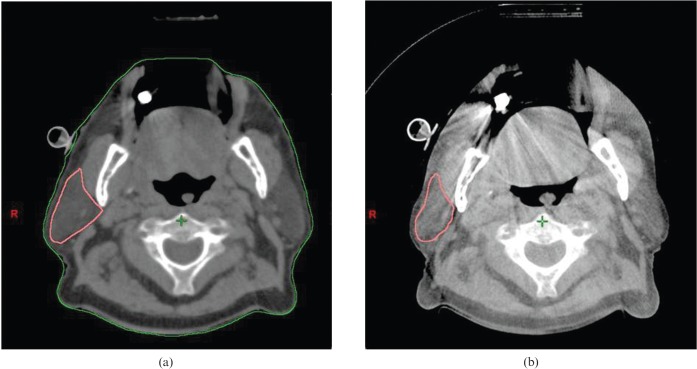
Figure 1.
An axial slice showing the right parotid gland on the (a) planning CT and on the (b) last cone-beam CT.
Figure 2.
Average volumetric variation in ipsilateral parotid glands. CBCT, cone-beam CT.
Figure 3.
Average volumetric variation in contralateral parotid glands. CBCT, cone-beam CT.
Figure 4.
Average volumetric variation in both parotid glands. CBCT, cone-beam CT.
Discussion
IMRT achieved an excellent dose distribution, especially in a concave-shaped target volume [22]. For patients with head and neck cancer, IMRT has shown a reduction in RT toxicity, and probably could improve survival [15,18]. The variation in volume or geometry of the target and OARs could increase the risk of missing the target or applying higher doses to the OARs. Several studies have documented significant volumetric change in selected OARs during RT for head and neck cancer, but the PGs showed the largest modifications in volume [3,10]. In a recent evaluation of 26 consecutive patients with head and neck cancer, the authors concluded that it is necessary to monitor the PGs during RT because their volumetric modifications are associated with an increase in radiation dose [10]. Another study on 10 oropharyngeal cancer patients reported a volume loss in the PGs with a medial shift of 3 mm and a change in the mean planned dose to both glands [12]. Nishimura et al [11] showed a significant decrease in the volume of the PGs during a course of RT and reported that the grade of xerostomia correlated with the initial volume of the PGs. Loo et al [23] reported a mean volume reduction for the iPG of 30.2% (range 17.1–55.8%) and for the cPG of 17.5% (range 15.6–48.5%). Despite more studies showing shrinkage of the PGs, it is not clear when a replan should be carried out. The aim of our study was to assess the volumetric change in the PGs during IMRT. To our knowledge, no studies have been published on the evaluation of PGs with CBCT. Although we evaluated a small series, we collected more data: our results showed a linear reduction in volume of the cPG and iPG and both PGs (r2=0.91, r2=0.92, r2=0.93, respectively), with a decrease per treatment day of 1.5% for both PGs. By the 20th day of treatment, the PGs had shrunk by 30% of the original volume. These data could support the hypothesis that, during the third week of RT, a check of the PG volume and/or a replan could be indicated.
Some authors showed a correlation between the mean dose to the PGs and volume loss for both PGs (especially for the iPG) (r2=0.4; p<0.001) [12]. Loo et al [23] in a recent evaluation of five cases showed a significant volume loss in both PGs without a correlation with radiation dose. Height et al [24] investigated the anatomical change in head and neck cancer and showed that both PGs (spared and unspared) decreased significantly in volume.
In our analysis, both PGs received a similar planned mean dose and we observed a volume loss in both PGs.
Several studies analysed the effects of PG shrinking and showed a gradual increase in the dose per fraction of the PG as a result of their volume loss and shift [12,23]: Loo et al [23] showed an increase in the cPG and iPG mean dose (average dose difference between planned and calculated of 7.3 Gy for the cPG and 7.6 Gy for the iPG). Castadot et al [25] analysed 10 head and neck cancer patients and observed that the delivered mean dose for both PGs increased compared with the planned mean dose owing to shrinkage of the PGs. Wu et al [26] reported the results of a replanning strategy in head and neck cancers and concluded that the shrinkage of target and some OARs did not result in significant dosimetric change, except for the PGs. This is consistent with our analysis; in fact, although we did not replan, we noted an increase in the global mean PG dose of approximately 3 Gy for each PG.
Conclusion
IGRT is a new and valid strategy to reduce side-effects and increase the dose to the target volume and, probably, increase survival. Evaluation of the volumetric change in the target and OARs is necessary to reduce toxicity, thereby tailoring the treatment. In head and neck cancer patients, the PGs show major changes during IMRT and our data, although limited (small series and the absence of replanning), showed that both PGs reduced in volume by approximately 1.5% per treatment day. Probably, a replan could be indicated on the third week of IMRT, when a volume loss of 24–30% is registered.
References
- 1.Saarilahti K, Kouri M, Collan J, Kangasmäki A, Atula T, Joensuu H, et al. Sparing of submandibular glands by intensity modulated radiotherapy in the treatment of head and neck cancer. Radiother Oncol 2006;78:270–5 [DOI] [PubMed] [Google Scholar]
- 2.Barker JL, Jr, Garden AS, Ang KK, O'Daniel JC, Wang H, Court LE, et al. Quantification of volumetric and geometric changes occurring during fractionated radiotherapy for head-and-neck cancer using an integrated CT/linear accelerator system. Int J Radiat Oncol Biol Phys 2004;59:960–70 [DOI] [PubMed] [Google Scholar]
- 3.Lee C, Langen KM, Lu W, Haimerl J, Schnarr E, Ruchala KJ, et al. Assessment of parotid gland dose changes during head and neck cancer radiotherapy using daily megavoltage computed tomography and deformable image registration. Int J Radiat Oncol Biol Phys 2008;71:1563–71 [DOI] [PubMed] [Google Scholar]
- 4.Han C, Chen YJ, Liu A, Schultheiss TE, Wong JY. Actual dose variation of parotid glands and spinal cord for nasopharyngeal cancer patients during radiotherapy. Int J Radiat Oncol Biol Phys 2008;70:1256–62 [DOI] [PubMed] [Google Scholar]
- 5.Rosenthal DI, Chambers MS, Fuller CD, Rebueno NC, Garcia J, Kies MS, et al. Beam path toxicities to non-target structures during intensity-modulated radiation therapy for head and neck cancer. Int J Radiat Oncol Biol Phys 2008;72:747–55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robar JL, Day A, Clancey J, Kelly R, Yewondwossen M, Hollenhorst H, et al. Spatial and dosimetric variability of organs at risk in head-and-neck intensity-modulated radiotherapy. Int J Radiat Oncol Biol Phys 2007;68:1121–30 [DOI] [PubMed] [Google Scholar]
- 7.Hansen EK, Bucci MK, Quivey JM, Weinberg V, Xia P. Repeat CT imaging and replanning during the course of IMRT for head-and-neck cancer. Int J Radiat Oncol Biol Phys 2006;64:355–62 [DOI] [PubMed] [Google Scholar]
- 8.Ballivy O, Parker W, Vuong T, Shenouda G, Patrocinio H. Impact of geometric uncertainties on the dose distribution during intensity modulated radiotherapy (IMRT) of head and neck cancer: the need for planning target volume (PTV) and planning organ at risk volume (PRV). Curr Oncol 2006;13:108–15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu Q, Chi Y, Chen PY, Krauss DJ, Yan D, Martinez A. Adaptive replanning strategies accounting for shrinkage in head and neck IMRT. Int J Radiat Oncol Biol Phys 2009;75:924–32 [DOI] [PubMed] [Google Scholar]
- 10.Ricchetti F, Wu B, McNutt T, Wong J, Forastiere A, Marur S, et al. Volumetric change of selected organs at risk during IMRT for oropharyngeal cancer. Int J Radiat Oncol Biol Phys 2011;80:161–8 [DOI] [PubMed] [Google Scholar]
- 11.Nishimura Y, Nakamatsu K, Shibata T, Kanamori S, Koike R, Okumura M, et al. Importance of the initial volume of parotid glands in xerostomia for patients with head and neck cancer treated with IMRT. Jpn J Clin Oncol 2005;35:375–9 [DOI] [PubMed] [Google Scholar]
- 12.Vásquez Osorio EM, Hoogeman MS, Al-Mamgani A, Teguh DN, Levendag PC, Heijmen BJ. Local anatomical changes in parotid and submandibular glands during radiotherapy for oropharynx cancer and correction with dose, studied in detail with non-rigid registration. Int J Radiat Oncol Biol Phys 2008;70:875–82 [DOI] [PubMed] [Google Scholar]
- 13.Kubicek GJ, Machtay M. New advances in high-technology radiotherapy for head and neck cancer. Hematol Oncol Clin North Am 2008;22:1165–80 [DOI] [PubMed] [Google Scholar]
- 14.Intensity Modulated Radiation Therapy Collaborative Working Group Intensity-modulated radiotherapy: current status and issues of interest. Int J Radiat Oncol Biol Phys 2001;51:880–914 [DOI] [PubMed] [Google Scholar]
- 15.Pow EH, Kwong DL, McMillan AS, Wong MC, Sham JS, Leung LH, et al. Xerostomia and quality of life after intensity-modulated radiotherapy vs. conventional radiotherapy for early-stage nasopharyngeal carcinoma: initial report on a randomized controlled clinical trial. Int J Radiat Oncol Biol Phys 2006;66:981–91 [DOI] [PubMed] [Google Scholar]
- 16.Xing L, Thorndyke B, Schreibmann E, Yang Y, Li TF, Kim GY, et al. Overview of image guided radiation therapy. Med Dosim 2006;31:91–112 [DOI] [PubMed] [Google Scholar]
- 17.Verellen D, Ridder MD, Linthout N, Tournel K, Soete G, Storme G. Innovations in image-guided radiotherapy. Nat Rev Cancer 2007;7:949–60 [DOI] [PubMed] [Google Scholar]
- 18.Donovan E, Bleakley N, Denholm E, Evans P, Gothard L, Hanson J, et al. for the Breast Technology Group Randomised trial of standard 2D radiotherapy (RT) versus intensity modulated radiotherapy (IMRT) in patients prescribed breast radiotherapy. Radiother Oncol 2007;82:254–64 [DOI] [PubMed] [Google Scholar]
- 19.Veldeman L, Madani I, Hulstaert F, De Meerleer G, Mareel M, De Neve W. Evidence behind use of intensity-modulated radiotherapy: a systematic review of comparative clinical studies. Lancet Oncol 2008;9:367–75 [DOI] [PubMed] [Google Scholar]
- 20.Nutting CM, Morden JP, Harrington KJ, Urbano TG, Bhide SA, Clark C, et al. Parotid-sparing intensity modulated versus conventional radiotherapy in head and neck cancer (PARSPORT): a phase 3 multicentre randomised controlled trial. Lancet Oncol 2011;12:127–36 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ding GX, Munro P, Pawlowski J, Malcom A, Coffey CW. Reducing radiation exposure to patients from Kv-CBCT imaging. Radiother Oncol 2010;97:585–92 [DOI] [PubMed] [Google Scholar]
- 22.Galvin JM, Ezzell G, Eisbrauch A, Yu C, Butler B, Xiao Y, et al. American Society for Therapeutic Radiology and Oncology; American Association of Physicists in Medicine. Implementing IMRT in clinical practice: a joint document of the American Society for Therapeutic Radiology and Oncology and the American Association of Physicists in Medicine. Int J Radiat Oncol Biol Phys 2004;58:1616–34 [DOI] [PubMed] [Google Scholar]
- 23.Loo H, Fairfoul J, Chakrabarti A, Dean JC, Benson RJ, Jefferies SJ, et al. Tumor shrinkage and contour change during radiotherapy increase the dose to organs at risk but not the target volumes for head and neck cancer patients treated on the tomotherapy HiArtTM System. Clin Oncol 2011;23:40–7 [DOI] [PubMed] [Google Scholar]
- 24.Height R, Khoo V, Lawford C, Cox J, Joon DL, Rolfo A, et al. The dosimetric consequences of anatomic changes in head and neck radiotherapy patients. J Med Imaging Radiat Oncol 2010;54:497–504 [DOI] [PubMed] [Google Scholar]
- 25.Castadot P, Geets X, Lee JA, Gregoire V. Adaptive functional image guided IMRT in pharyngo-laringeal squamous cell carcinoma: is the gain in dose distribution worth the effort? Radiother Oncol 2011;101:343–50 [DOI] [PubMed] [Google Scholar]
- 26.Wu Q, Chi Y, Chen PY, Krauss DJ, Yan D, Martinez A. Adaptive replanning strategies accounting for shrinkage in head and neck IMRT. Int J Radiat Oncol Biol Phys 2009;75:924–32 [DOI] [PubMed] [Google Scholar]