Abstract
Objectives
This study aimed to clarify the number and cause of incidental findings detected on positron emission tomography (PET)/CT in patients undergoing investigation for presumed lung cancer.
Methods
The scan reports from PET/CT studies performed for patients with lung cancer under National Institute for Clinical Evidence guidelines from January 2006 until March 2008 were retrospectively reviewed. Incidental findings were followed up by a combination of case note review, clinician feedback, colonoscopy database, histopathology and follow-up imaging.
Results
818 patients were investigated for lung cancer in the study period. 197 incidental findings were found in 175 (21%) patients. The subsequent investigation of 108 lesions confirmed a pathological correlation in 71 (66%) cases. A second primary malignancy was found in 10 patients within the bowel (6), breast (2), tongue (1) and stomach (1). A pre-malignant lesion was confirmed in 25 cases (24 large bowel tubulovillous adenomas and a follicular thyroid lesion). A further 41 (5%) benign abnormalities were detected at multiple sites; the thyroid gland was the single most frequently affected site (14 abnormalities). There were 36 (4.4%) false-positive reported findings, including 17 in the region of the pharynx and larynx and 12 within the large bowel.
Conclusions
Overall, 9.2% of patients with suspected or known lung cancer having PET/CT had a confirmed incidental finding. A malignant or pre-malignant lesion was found in 1.2% and 3.0%, respectively. These were mostly located within the gastrointestinal tract. The majority of false-positive incidental findings were located in the larynx and pharynx. Uptake in these regions is unlikely to be significant in the absence of a CT morphological correlation.
The Department of Health and National Institute of Clinical Excellence (NICE) guidelines advise that 18-fludeoxyglucose (FDG) positron emission tomography (PET) should be used to differentiate between benign and malignant lung lesions where anatomical imaging or biopsy are inconclusive or biopsy is contraindicated and for staging of non-small cell lung cancer prior to radical treatment [1,2]. The PET/CT North Scheme is a 5-year UK government-awarded contract whose key objective is to provide an improved diagnosis for cancer patients leading to improvements in quality of care in the north of England. This is expected to generate approximately 48 000 National Health Service (NHS) PET/CT scans over the lifetime of the contract and to assist in the integration of a new diagnostic speciality in the UK [3]. During routine reporting of PET/CT scans, it is common to find areas of increased FDG uptake that are unlikely to be related to the neoplasm for which the patient is being scanned [4-13]. These findings cause delays in the management of the primary malignancy because they require further investigation. Therefore, incidental findings tend to be unpopular with the referring clinicians.
The aims of this study were to assess the frequency and significance of incidental findings reported on PET/CT scans in patients investigated for lung cancer to gain insight into the relevance of these findings, to reassure referring clinicians and to improve reporting accuracy.
Methods and materials
A retrospective analysis of PET/CT scans referred to the Sheffield Teaching Hospital NHS Trust between January 2006 and March 2008 was carried out. Patients imaged in accordance with NICE guidelines for the investigation of lung cancer were included in the study. All patients were scanned from the skull base to the thighs with 350 MBq of FDG in conjunction with non-contrast low dose CT. The scans were dual reported by consultant radiologists. The scan reports were reviewed and any incidental findings recorded. An incidental finding was defined as either a significant area of FDG uptake at a site where the uptake was unlikely to be related to the primary neoplasm, but could represent significant pathology, or an abnormality on the CT component of the PET/CT scan that was not evident on the initial diagnostic CT scan. Infective changes detected within the thorax that had developed since the diagnostic CT scan were excluded from this study. A combination of case note review, clinician feedback, the colonoscopy database, histopathology reports and follow-up imaging were used to clarify the aetiology and significance of the reported coincidental findings. Where unexpected findings were not investigated, similar methods were used to determine why further investigation had not been performed. This study was submitted to our Clinical Effectiveness Unit and accepted as service review, and no ethical approval was required.
Results
A total of 1158 patients underwent PET/CT imaging during the study period. 818 patients were investigated according to the NICE lung guidelines and 197 incidental findings were identified in 175 (21%) patients (Table 1). The age of patients with incidental findings ranged from 43 to 89 years (mean, 70.1 years; 98 males and 77 females.) Of the 197 incidental findings, 108 were investigated further. In 71 cases this confirmed an abnormality, and in 37 cases no abnormality was found. 71 of the incidents were not investigated: 49 cases had advanced lung cancer or were deceased and 22 were reported as probably physiological uptake, and for 18 information regarding further follow-up could not be found. 196 of the incidental findings were FDG avid. Only one abnormality did not take up FDG and was identified from the CT scan performed in conjunction with the PET/CT scan.
Table 1. Summary of unexpected findings by site, outcome of investigation and reasons for absence of investigation.
| Site of incidental finding | Total cases | Number investigated | Results of investigation (number) | Reason for no investigation |
| Large bowel | 84 | 49 | 37 (76%) abnormal: | Physiological uptake (7) |
| Tubulovillous adenoma (23) | Advanced disease/deceased (20) | |||
| Diverticular disease (5) | Reason unknown (7) | |||
| Adenocarcinoma (4) | ||||
| Hyperplastic polyp (1) | ||||
| Inflammatory (1) | ||||
| Lymphoid tissue (1) | ||||
| Annular lesion (1) | ||||
| Multiple polyps (1) | ||||
| 12 (24%) normal colonoscopy | ||||
| Pharynx | 24 | 12 | 2 (17%) abnormal: | Advanced disease (6) |
| Tonsillitis (1) | Physiological uptake (3) | |||
| Tongue carcinoma (1) | Reason unknown (3) | |||
| 10 (83%) normal | ||||
| Larynx and hypopharynx | 18 | 7 | 2 (28.5%) vocal cord palsy | Physiological uptake (7) |
| 5 (71.5%) normal | Advanced disease (4) | |||
| Thyroid | 27 | 18 | 15 (83%) abnormal: | Advanced disease (6) |
| Multinodular goitre (10) | Reason unknown (3) | |||
| Follicular thyroid lesion (1) | ||||
| Thyroid nodule (1) | ||||
| Atrophic gland (1) | ||||
| Thyroiditis (2) | ||||
| 3 (17%) normal | ||||
| Oesophagus and stomach | 7 | 5 | 1 (20%) abnormal: | Advanced disease (1) |
| Gastro-oesophageal carcinoma | Reason unknown (1) | |||
| 4 (80%) normal | ||||
| Small bowel | 6 | 2 | 1 (50%) carcinoid | Advanced disease (3) |
| 1 (50%) normal | Physiological (1) | |||
| Breast | 6 | 3 | 2 (67%) abnormal: | Advanced disease/deceased (3) |
| Breast carcinoma (2) | Advanced disease/deceased (3) | |||
| 1 (33%) recent surgery for benign disease | ||||
| Other miscellaneous sites | 25 | 11 | 9 (82%) abnormal: | Advanced disease/deceased (7) |
| Pituitary adenoma (2) | Most likely physiological (4) | |||
| Warthin's tumour (2) | Reason unknown (3) | |||
| Benign mucinous ovarian tumour (1) | ||||
| Haemorrhagic ovarian cyst (1) | ||||
| Spinal cord meningioma (1) | ||||
| Cholecystitis (1) | ||||
| Inguinal hernia (1) | ||||
| 2 (18%) normal | ||||
| Parotid biopsy—normal (1) | ||||
| Adrenal mass resolved on follow-up CT (1) |
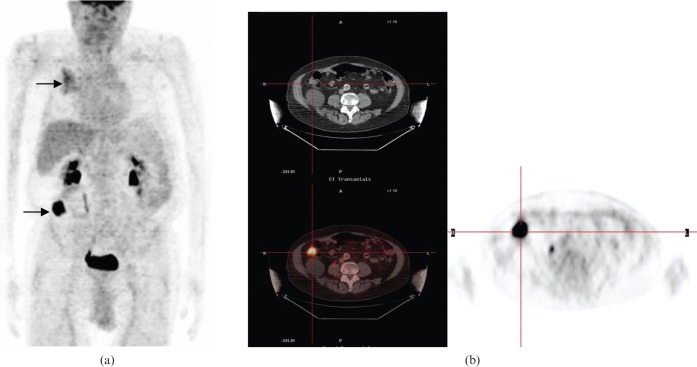
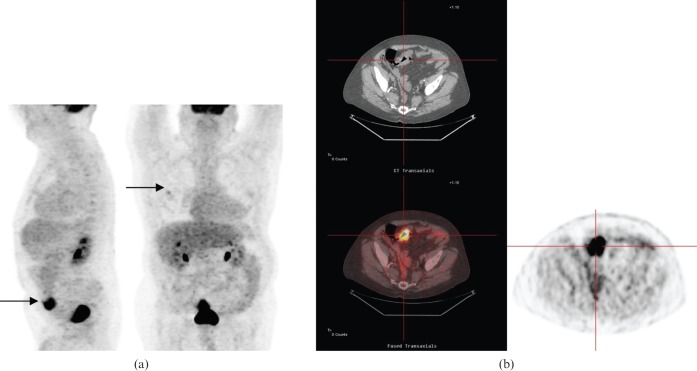
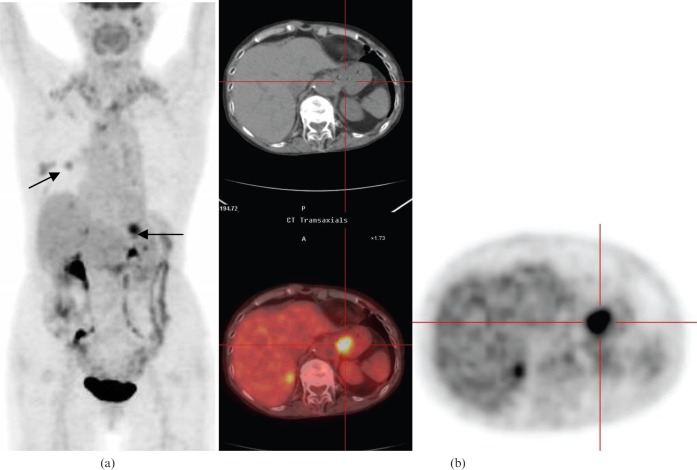
Among the 197 unexpected findings, 84 (43%) were found in the large bowel, of which 24 were associated with a mass on the CT component. 49 of these abnormalities were investigated by colonoscopy, which revealed an abnormality in 37 cases. The incidental FDG uptake corresponded to a range of abnormalities: 23 tubulovillous adenomas, 5 diverticular disease, 4 adenocarcinomas, 1 hyperplastic polyp, 1 inflammatory lesion (unspecified), 1 lymphoid tissue, 1 annular lesion (probable carcinoma, no histology) and 1 multiple polyps without confirmed histology (Figures 1 and 2). The colonoscopy was normal in 12 of the cases investigated. Of the remaining 34 incidental bowel findings not investigated, 7 were reported as probable physiological uptake but with clinical correlation advised, 20 had advanced disease or were deceased and for 7 the reason for no further investigation was unknown.
Figure 1.
85-year-old male imaged for suspected lung cancer. (a) Coronal positron emission tomography (PET) scan shows positive hypermetabolic focus corresponding to the right upper lobe mass (upper arrow) and an unexpected intense caecal focus (lower arrow). (b) Transverse PET/CT scan shows intense tracer uptake within the caecum that mapped onto a soft-tissue mass. Colonoscopy and biopsy revealed caecal adenocarcinoma.
Figure 2.
60-year-old male investigated for lung nodule. (a) Coronal positron emission tomography (PET) scan shows a right upper lobe nodule (upper arrow) and the sagittal image shows incidental 18-fludeoxyglucose uptake in the sigmoid colon (lower arrow). (b) Transaxial PET/CT revealed intense focus within the sigmoid colon, which when investigated was found to be a sigmoid adenocarcinoma.
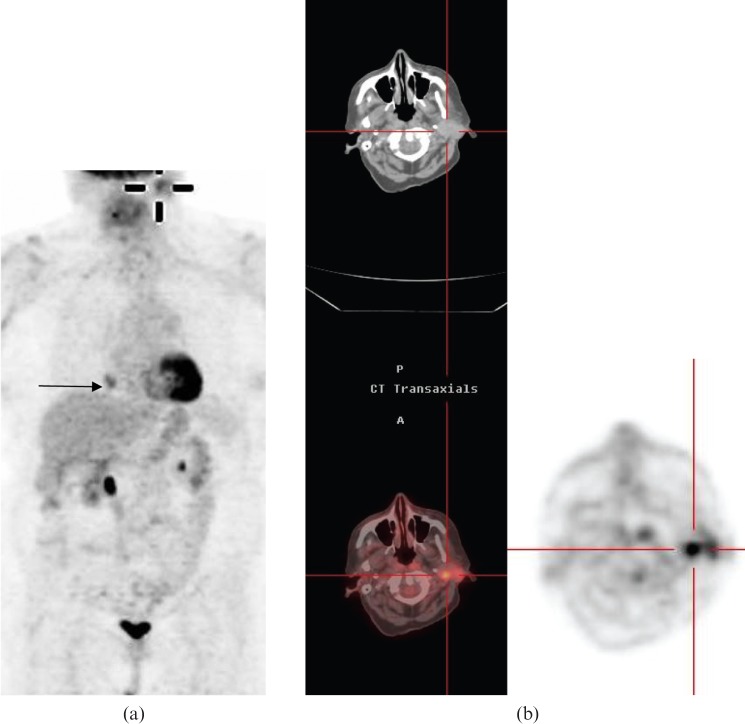
24 unexpected findings were reported within the pharynx, of which 4 were associated with an abnormality on the CT component. 12 patients were further investigated, 3 by MRI and the remainder by direct visualisation. No abnormality was seen in 10 cases. One patient underwent a tonsillectomy but the tonsil was histologically normal. There were two abnormal findings. One patient was diagnosed with tonsillitis (Figure 3). The second patient had an area of intense focal FDG uptake within the tongue. The initial biopsy of this region showed no abnormality; however, the patient represented 3 months later with an enlarged mass lesion of the tongue that was confirmed as a squamous cell carcinoma on repeat biopsy (Figure 4).
Figure 3.
53-year-old male scanned to assess the resectability of a known squamous cell carcinoma. (a) Coronal positron emission tomography (PET) scan shows a right hilar lung mass (lower arrow) and unexpected oropharyngeal 18-fludeoxyglucose (FDG) tracer uptake (upper arrow). (b) Transaxial PET/CT shows intense FDG uptake within a soft-tissue mass within the left side of the oropharynx. Follow-up examination revealed tonsillitis.
Figure 4.
Evaluation of a solitary pulmonary nodule in a 69-year-old male. (a) Sagittal positron emission tomography (PET) scan shows a hypermetabolic solitary lung nodule (lower arrow) and unexpected focus of uptake in the oral cavity (upper arrow). (b) Axial PET/CT images initially reported as abnormal tongue uptake suspicious for malignancy. However, there was no discernable mass on the CT component and tongue biopsy was normal. (c) Follow-up CT for lung nodule assessment after a 3-month interval showed an incidental large tongue mass. Squamous cell carcinoma of tongue confirmed after repeat biopsy.
Within the larynx and hypopharynx there were 18 unexpected findings and 2 were associated with a mass on the CT component. Seven patients were investigated further; two were found to have vocal cord palsy and no abnormality was detected in the remaining five patients. 11 cases were not investigated; 7 were reported as most probably physiological but clinical correlation was advised and 4 patients had advanced disease.
27 patients had abnormal findings within the thyroid. The FDG uptake was described as focal in 15 cases and diffuse in 4. Ultrasound was performed in 18 patients and the final diagnosis for the FDG uptake was as follows: 10 multinodular goitres, 1 Category III follicular thyroid lesion, 1 thyroid nodule, 1 atrophic gland, 2 cases of thyroiditis and 3 normal glands. The imaging findings prompted a fine-needle aspiration in only one patient. No confirmed malignancy was found. The remaining nine patients were not investigated; six had advanced disease and in three patients the reason was unknown.
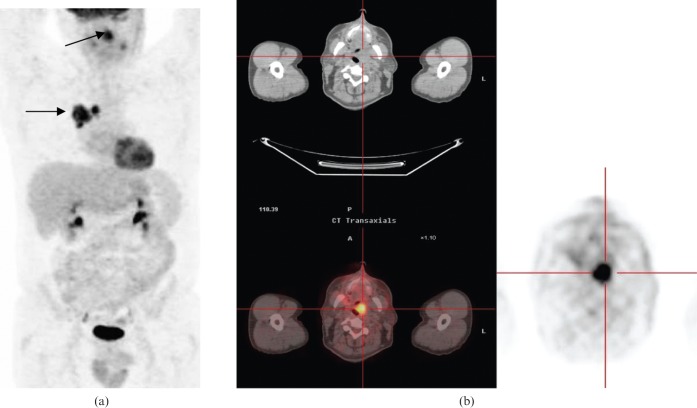
Seven patients had an abnormality in the oesophagus or stomach. Upper gastrointestinal endoscopy was carried out in five patients; four were normal and one patient had a gastro-oesophageal carcinoma (Figure 5). Two patients were not investigated; one patient had advanced disease and the reason for the remaining patient was unknown.
Figure 5.
80-year-old female investigated for an incidentally found lung nodule. (a) Coronal positron emission tomography (PET) scan shows right middle lobe nodule (top arrow) and unexpected hypermetabolic focus within the stomach (bottom arrow). (b) Transaxial PET/CT images show very intense and very focal stomach uptake. Oesophagogastroscopy and biopsy identified a gastro-oesophageal junction adenocarcinoma.
There were six unexpected findings reported in relation to the small bowel. However, four of these were not investigated owing to end-stage disease. Of the two patients investigated, one underwent capsule endoscopy and contrast-enhanced abdominal CT imaging that was normal and in the other case carcinoid disease was detected in the abdominal nodes.
Six patients had an abnormality reported within the breast. Further investigation of three of these cases detected two breast carcinomas. The increased FDG uptake in the third patient was secondary to recent surgery for benign disease, but this information had not been stated on the request card and was unknown at the time the report was issued. The remaining three patients were not investigated owing to advanced disease.
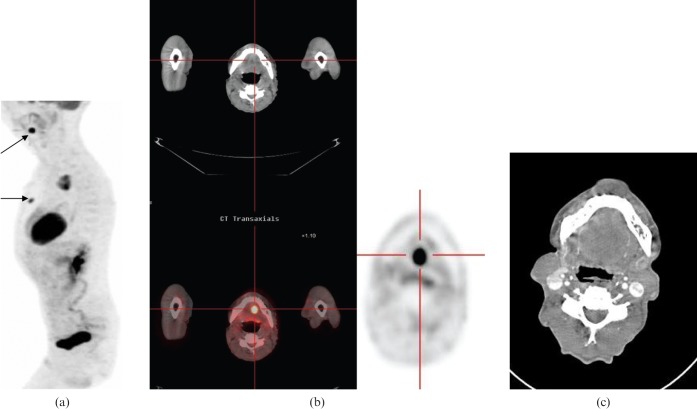
Finally, 11 of the remaining 25 patients were investigated for more unusual sites of increased FDG uptake. There were three cases of focal-increased FDG uptake within the parotid gland; all had an ultrasound-guided biopsy. This confirmed Warthin's tumour in two cases and no abnormality was found in the third patient (Figure 6). The PET/CT scan detected two pituitary adenomas. In retrospect, the clinicians were aware of one of these lesions but the relevant information was not included on the request card. The second adenoma was a true incidental finding and remained stable on follow-up imaging. There were two ovary/adnexal lesions. One of these lesions was later diagnosed as a benign mucinous tumour and the second was due to a haemorrhagic ovarian cyst. A further adrenal mass detected on one PET/CT scan had resolved on follow-up. Finally, there were single cases each of a spinal cord meningioma confirmed on a subsequent MRI scan, cholecystitis confirmed by ultrasound and an inguinal hernia confirmed with clinical examination. The remaining 14 incidental findings were not investigated: 1 patient was deceased, 6 had advanced disease, 4 were reported as most probably physiological uptake in the following sites: axilla, mandible, parotid and the skin on the lower abdominal wall, and in 3 cases the reason for not investigating was unknown.
Figure 6.
Scans in a 79-year-old female for evaluation of a solitary pulmonary nodule. (a) Coronal positron emission tomography (PET) scan shows a right lower lobe nodule (lower arrow) and unexpected left parotid uptake (as highlighted). (b) Transaxial PET/CT shows intense tracer within a left parotid mass. Subsequent ultrasound guided biopsy revealed a Warthin's tumour.
Therefore, an additional malignancy was confirmed in 1.2% and a pre-malignant lesion was identified in 3% of the study population. A coincidental benign lesion was found in 5% and no abnormality was identified as a cause of the hypermetabolic focus reported on PET/CT scan in a further 4.4%.
Discussion
As PET/CT imaging becomes more widely available, reporting radiologists are encountering a large number of incidental findings. The emphasis the reporter places on an incidental finding will influence further management, as does the stage of the primary cancer and the patient's comorbidity. Many clinicians are uncertain of the relevance of the reported unexpected findings and require guidance relating to their importance and the need for further investigation. All malignancies should be discussed at local site-specific multidisciplinary team meetings (MDTs). Increasingly, a PET/CT-trained radiologist can provide advice on the probable significance of such findings in conjunction with the clinical context.
An incidental finding was detected in 21% of the patients in our study. The incidental uptake was investigated in 55% of cases and an abnormality was detected in 66% of the cases that were investigated. Overall, an incidental finding was confirmed in 9.2% of patients undergoing PET/CT imaging (this percentage is likely to have been higher had all incidental findings been investigated). A confirmed malignant or pre-malignant lesion was found in 4.2% of patients and the false-positive rate was 4.4%. A large proportion of the reported incidental findings were not further evaluated, largely owing to the limited perceived benefit to the patient in relation to the stage of the primary malignancy. The number of incidental findings in our study is much greater than that reported in other studies. Ishimori et al [10] reported 79 incidental findings in 1912 patients (4.1%), of whom 22 (1.2%) had a confirmed malignancy. There were only 10 (0.5%) false-positive findings and in 8 cases (0.4%) the PET positive lesion was considered benign. The mean patient age was 58.9±13.9 years. A further study by Agress et al [5] reviewed a series of 1750 PET/CT scans performed for a wide range of indications and found 58 unexpected findings in 53 patients (3.1%). Histology was obtained for 42 hypermetabolic foci in 37 patients. There were 30 malignant or pre-malignant lesions (1.7% of total investigated), 3 false positives (0.2%) and 9 benign lesions (0.5%). The increased proportion of confirmed incidental findings in our study may be related to the greater mean age of the patients in our study, although the age of the population and the different distribution of primary malignancies under investigation in the Agress et al study was not stated.
Lardinois et al [7] performed a prospective study to assess the incidence and nature of solitary extrapulmonary FDG accumulations in 350 patients undergoing PET/CT scans for the investigation of non-small cell lung cancer. Solitary extrapulmonary accumulations (SEPA) were detected in 72 patients (21%). 69 SEPAs were further investigated: 54% were due to a solitary non-small cell lung cancer metastasis (NSCLC) and 46% were unrelated to the primary malignancy, i.e. 13% had an unexpected coincidental finding. A second malignancy or recurrence of a previously diagnosed primary malignancy was found in 1.7% of the study group (6 cases), and in a further 7.4% (26 cases) the uptake was secondary to benign or inflammatory lesions. Overall, an unexpected incidental finding not related to the NSCLC was found in 9.1% of patients investigated. These figures are similar in magnitude to our study.
The commonest site for incidental findings was within the large bowel. Having a “hot spot” correlated with a high risk of having a significant abnormality. In our study, a malignant or pre-malignant abnormality was detected in 76% of those undergoing colonoscopy. A confirmed abnormality was more likely if the focal FDG-avid area corresponded with a reported CT scan abnormality. Surprisingly, the confirmed rate of abnormality was not that different between the two groups: 80% with CT scan abnormality and 73% with no reported CT scan abnormality. The predominance of tubulovillous adenomas in our study is concordant with the findings of many studies [4,5,7-10], although no bowel polyps were identified in the paper by Ishimori et al [10]. The rate of incidental large bowel findings in these studies varied from 1.3% to 3% in those investigated. This was much lower than the 10.2% in our study. However, in patients in whom the hypermetabolic focus was investigated, the rate of a confirmed abnormality varied from 46% to 80%. The confirmed pathology rate in our study was 76% in those patients investigated, suggesting that the reported findings were likely to be real and not simply a reflection of an overcall of bowel pathology. Again, this may be related to the mean age of our patient population. PET/CT is more accurate than PET alone, as shown in reported series and literature from American centres, which often scan for a wider range of pathologies.
In our practice, the frequent detection of a bowel abnormality resulted in treatment delay of the primary bronchogenic carcinoma. In response to this, a rapid referral, the investigation mechanism, was set up within our trust. The colorectal surgical team had noted the high pick-up rate of pathological findings in patients referred for colonoscopy for investigation of a PET-detected abnormal bowel focus and agreed that patients fit enough for further investigation could be referred directly for colonoscopy without prior review in the surgical clinic. Requests were sent by e-mail or fax directly to the colorectal cancer MDT co-ordinator and colonoscopy was booked within 5 working days. This referral pathway has sped up the investigation of bowel abnormalities detected coincidentally significantly.
The second highest rate of incidental findings was within the pharynx and larynx, where most of the patients investigated were found to have no abnormality. Areas of raised FDG uptake within the head and neck region, particularly the pharynx, are very common owing to the large amount of lymphoid tissue found. In addition, the anatomy of the region is complex and not very clearly defined on the low dose, unenhanced CT scan performed as part of the PET/CT scan. Furthermore, the uptake is frequently slightly asymmetric and a limited history is usually provided regarding relevant head and neck surgery, e.g. unilateral tonsillectomy, even in patients referred for the investigation of a suspected occult head and neck primary malignancy. Considerable experience is required in the interpretation of these findings.
There are not many studies published in the literature examining this issue. Heusner et al [14] examined the intensity and symmetry of FDG uptake at 4 sites (Waldeyer's ring, oral floor, larynx and thyroid) in 590 patients without a head or neck malignancy, inflammation or a correlating morphological lesion on a fully diagnostic CT scan to determine whether the increased FDG uptake indicated the development of a head and neck malignancy. Increased FDG uptake was present in one of the sites of interest in 60% of cases. In approximately 17%, the uptake was asymmetric and could be associated with a standardised uptake value as high as 7.2. No malignancy was ultimately found within this group after an average 2.5 years of follow-up. Two malignancies were diagnosed in patients with symmetric raised uptake with a maximum standardised uptake value (SUV) of 3.7. The study concluded that elevated, asymmetric head and neck FDG accumulation without a correlating morphological lesion is found frequently and does not predict cancer development. This paper illustrates the difficulty of predicting the significance of increased FDG uptake in the head and neck region.
The high rate of incidental findings within this region in the current study are partly related to the reporters' relative inexperience at the commencement of the regional PET/CT service (at this time the principal reporting radiologists had 3 and 1 years' experience of PET reporting, respectively. Feedback was obtained regarding the low pick-up rate of abnormalities from the pharyngeal “unexpected” findings at a regional educational lung cancer event at which the clinicians were invited to bring interesting PET/CT cases for discussion. This feedback proved invaluable and highlights the importance of two-way interaction between the PET/CT reporters and referring clinicians. The rate of reported unexpected findings within the head and neck region has dropped substantially.
Incidental FDG uptake within the thyroid gland is reported in 1.1–4% of patients investigated by PET/CT [11-13,15]. This is comparable to the rate of 3.3% of patients in the current study. However, most reports indicated that investigation of these lesions detects malignancy, mostly primary thyroid cancer, in 26.7–52% of cases. Of note is that histological confirmation of FDG-avid thyroid focus is obtained in a small proportion of the identified cases only and there may have been a bias in selecting patients with more concerning features for further investigation. There was no confirmed malignancy in our study. One criticism of our study is that only a single biopsy was performed out of the 18 cases referred for ultrasound. However, all the ultrasound scans were performed by 2 experienced consultant radiologists with an interest in thyroid disease who did not find a distinct focal suspicious abnormality worthy of biopsy in the remaining 17 cases. In contrast to other studies, Heusner et al [14] detected FDG uptake in the thyroid gland in 31% of patients, mostly symmetric, but there was not a single case of confirmed thyroid malignancy. This study concluded that, for populations in which thyroid goitre is endemic, FDG uptake by the thyroid is common and not associated with thyroid cancer. This study was performed in Germany which, similar to the UK, has a low prevalence of thyroid cancer.
Several studies conclude that focal FDG thyroid uptake, especially in the presence of a CT correlate, is associated with an increased risk of malignancy [12,13]. Symmetrical FDG uptake in the thyroid gland is a feature of benign disease and most frequently related to thyroiditis. There are conflicting reports on the use of the SUV value in differentiating between benign and malignant disease. However, it appears that there is a considerable overlap is the range of values measured in the two conditions and that the SUV values should be used with caution [11,12,15].
There are several limitations of this study. The study was performed retrospectively and it was not possible to obtain feedback data on all patients included in the study. Many patients were not suitable for further investigation or the importance of an unexpected finding was limited owing to the advanced stage of the patient's lung cancer. The study spanned numerous referral centres and the initial referrer could not always be identified. In many instances the MDT discussion was not documented and the precise reason for the lack of further investigation could only be surmised.
Clinicians are frequently uncertain how to deal with reported unexpected findings. It is vital that referring clinicians are encouraged to provide all relevant clinical information. Referrers may need guidance with regard to this as they may be unaware of the normal patterns of FDG uptake in the body and how this may be affected by previous therapies. In addition, it is important that clinicians reporting PET/CT state clearly the probable significance of coincidental findings and the need for further investigation. The availability of selected images highlighting the area of interest along with the written report and discussion at MDT meetings should be encouraged. Of course, the importance of additional findings should be considered in the clinical context of the patient's prognosis and the impact of additional diagnoses on subsequent management.
Conclusion
Unexpected findings in patients having PET/CT imaging for the investigation of lung cancer are common, but the requirement for further investigation should be considered in the light of the probable significance of the finding relative to the stage of the primary malignancy. The majority of incidental findings are located within the bowel, and colonoscopy will confirm a pathological lesion in most cases. A rapid referral pathway for the investigation of bowel lesions is advised to minimise delay in the treatment of the primary carcinoma. Intense and asymmetric FDG uptake in the region of the larynx and pharynx is frequently present and is unlikely to signify malignant disease in the absence of a CT morphological correlate. The absence of a confirmed malignant thyroid lesion in our study is at odds with most papers in the literature and may reflect the low prevalence of thyroid malignancy within the UK.
References
- 1.National Institute for Health and Clinical Excellence. The diagnosis and treatment of lung cancer [updated 2005; cited August 2009]. Available from: http://www.nice.org.uk/nicemedia/pdf/cg024fullguideline.pdf.
- 2.Department of Health. A framework for development of PET services in England (2005) [cited August 2009]. Available at: http://webarchive.nationalarchives.gov.uk/+/www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4121030.pdf.
- 3.Alliance Medical group. PET/CT North scheme [cited September 2009]. Available from: http://www.alliancemedical.eu.com/newsitem/display1.htm.
- 4.Gutman F, Alberini J, Wartski M, Vilain D, LeStanc E, Sarandi F, et al. Incidental colonic lesions found at PET/CT. Am J Roentgenol 2005;185:495–500 [DOI] [PubMed] [Google Scholar]
- 5.Agress H, Cooper BZ. Detection of clinically unexpected malignant and premalignant tumours at PET. Radiology 2004;230:417–22 [DOI] [PubMed] [Google Scholar]
- 6.Zhuang H, Hickeson M, Chacko TK, Duarte PS, Nakhoda KZ, Feng QI, et al. Incidental detection of colon cancer by FDG positron emission tomography in patients examined for pulmonary nodules. Clinical Nucl Med 2002;27:628–32 [DOI] [PubMed] [Google Scholar]
- 7.Lardinois D, Weder W, Roudas M, von Schulthess GK, Tutic M, Moch H, et al. Etiology of solitary extrapulmonary positron emission tomography and computed tomography findings in patients with lung cancer. J Clin Oncol 2005;23:6846–53 [DOI] [PubMed] [Google Scholar]
- 8.Kamel EM, Thumshirn M, Truninger K, Schiesser M, Fried M, Padberg B, et al. Significance of incidental FDG accumulations in the gastrointestinal tract in PET/CT: correlation with endoscopic and histopathologic results. J Nucl Med 2004;45:1804–10 [PubMed] [Google Scholar]
- 9.Israel O, Yefremov N, Bar-Shalom R, Kagana O, Frenkel A, Keidar Z, et al. PET/CT detection of unexpected gastrointestinal foci of 18 FDG uptake: incidence, localisation patterns and clinical significance. J Nucl Med 2005;46:758–62 [PubMed] [Google Scholar]
- 10.Ishimori T, Patel PV, Wahl RL. Detection of unexpected additional primary malignancies with PET/CT. J Nucl Med 2005;46:752–7 [PubMed] [Google Scholar]
- 11.Bogsrud TV, Karantanis D, Nathan MA, Mullan BP, Wiseman GA, Collins D, et al. The value of quantifying 18F-FDG uptake in thyroid nodules found incidentally on whole-body PET/CT. Nucl Med Commun 2007;28:373–81 [DOI] [PubMed] [Google Scholar]
- 12.Choi JY, Lee K, Kim H, Shim Y, Kwon OJ, Park K, et al. Focal thyroid lesions incidentally identified by integrated 18F-FDG PET/CT: clinical significance and improved characterisation. J Nucl Med 2006;47:609–15 [PubMed] [Google Scholar]
- 13.Are C, Hsu JF, Schoder H, Shah JP, Larson S, Shaha A. FDG-PET detected thyroid incidentalomas: need for further investigation? Ann Surg Oncol 2006;14:239–47 [DOI] [PubMed] [Google Scholar]
- 14.Heusner A, Hahn S, Hamami M, Forsting M, Kogel S, Bockisch A, et al. Incidental head and neck 18F-FDG uptake on PET/CT without corresponding morphological lesion: early predictor of cancer development? Eur J Nucl Med Mol Imaging 2009;36:1397–406 [DOI] [PubMed] [Google Scholar]
- 15.Kang K, Kim S, Kang H, Lee E, Sim J, Lee I, et al. Prevalence and risk of cancer of focal thyroid incidentaloma identified by 18F-flurodeoxyglucose positron emission tomography for metastasis evaluation and cancer screening in healthy subjects. J Clin Endo Meta 2003;88:4100–4 [DOI] [PubMed] [Google Scholar]