Abstract
Objective
The purpose of this study was to compare the diagnostic accuracy of time-resolved MR angiography (TR-MRA) with that of conventional venography for the detection and grading of ovarian venous reflux, which aid in the diagnosis of pelvic venous congestion.
Methods
We performed a retrospective analysis of 19 consecutive patients who underwent TR-MRA and conventional venography. The images were analysed by two radiologists in a randomised “blinded” manner. With the use of conventional venography as a gold standard, the images were reviewed to determine if differences in the detection and grading of ovarian venous reflux were seen between TR-MRA and conventional venography; the sensitivity, specificity and accuracy of TR-MRA compared with that of conventional venography were evaluated. The McNemar test was performed to determine the significance of any differences. Interobserver agreement was analysed using generalised κ statistics.
Results
There was no significant difference between TR-MRA and conventional venography for grading ovarian venous reflux (p>0.05). The sensitivity, specificity and diagnostic accuracy of TR-MRA were found to be 66.7%, 100% and 78.9%, and 75%, 100% and 84.2%, respectively, for the two observers. The weighted κ-values indicated excellent agreement between the two observers for grading ovarian venous reflux on TR-MRA (κ=0.894).
Conclusion
TR-MRA is an accurate method for accessing pelvic venous congestion.
Chronic pelvic pain is a common health problem among females, and this is characterised by non-cyclic pelvic pain lasting more than 6 months [1]. It has been reported that as many as 39.1% of females have had chronic pelvic pain at some time during their lives [2]. Pelvic congestion syndrome is defined as chronic pelvic pain caused by incompetent ovarian veins, with associated venous reflux and venous engorgement [3,4].
Conventional angiography is currently considered the gold standard for the detection of pelvic congestion syndrome [5]. However, this procedure is time-consuming and invasive, and it necessitates the use of ionising radiation. Several non-invasive techniques are used for the work-up of pelvic venous congestion, including sonography, CT and MRI [6-10]. Time-resolved MR angiography (TR-MRA) has been proven to be a quick and non-invasive technique that allows evaluation of the physiological blood flow [11-14].
There has been a study regarding the usefulness of TR-MRA for assessing ovarian venous reflux, but to the best of our knowledge [11] the correlation with conventional venography has not been used to access the result of TR-MRA for detecting ovarian venous reflux. The purpose of this study was to compare the diagnostic accuracy of TR-MRA with that of conventional venography for the detection and grading of ovarian venous reflux, which will help make the diagnosis of pelvic venous congestion.
Methods and materials
Patients
Our institutional review board approved this retrospective study and informed patient consent was waived. We performed a review of the clinical records of TR-MRA and conventional venography examinations that were performed from 1 January 2009 to 30 August 2009 for evaluating pelvic venous congestion. The criteria for inclusion in the study were a high degree of clinical suspicion of pelvic venous congestion because of chronic pelvic pain of at least 6 months' duration; patients had undergone both TR-MRA and conventional venography. In addition, the patients underwent conventional venography within 1 month after TR-MRA. The retrospective analysis included 19 patients (age range 27–61 years, mean age 42 years). They were all pre-menopausal females (17 parous and 2 non-parous).
Time-resolved MR angiography
MRI was performed on a 1.5 T system (Achieva 1.5 T, Philips Systems, Best, the Netherlands) using a SENSE body coil. All the patients were initially examined with a routine MRI protocol for the pelvis that included the axial, coronal and sagittal T2 weighted images, the axial T1 weighted images and the contrast-enhanced T1 weighted images.
T2 weighted fast spin echo (FSE) MRI was performed with the following parameters: repetition time (TR)/echo time (TE) 4000–4100/100 ms; a matrix of 340×340, a field of view of 22×22 cm, acquisition of two signals, a section thickness of 5 mm and a section gap of 1 mm. T1 weighted spin echo (SE) MRI was performed with the following parameters: a TR/TE of 300–450/10 ms, a flip angle of 90°, a matrix of 340×340, a field of view of 22×22 cm, acquisition of two signals, a section thickness of 5 mm and a section gap of 1 mm.
TR-MRA was acquired using the contrast-enhanced timing robust angiography (CENTRA) keyhole technique. The acquisition parameters of TR-MRA were the following: TR/TE of 5.5/1.5 ms, flip angle 35°, matrix 350×210, slices/slab 70, slice thickness 1.6 mm and field of view 40×40 cm. During shallow breathing, four phases (arterial, late arterial, venous and late venous) of imaging of the pelvis were performed in the coronal plane for 1–2 min after iv injection of 0.1 mmol kg–1 body weight of contrast medium (Dotarem, Guerbet S.A., Roissy, France) at a rate of 2 ml s–1, and this was followed by a 20 ml saline flush with a power injector. The acquisition time per phase was 15 s and the intervals between phases were 3 s. Timing for the TR-MRA was achieved through the use of a MR fluoroscopic bolus detection technique (BolusTrack; Philips Medical Systems). The scanning of the arterial phase was started after initial abdominal aortic enhancement at the renal artery level on the MR fluoroscopic images. The post-enhanced MR images for each phase were subtracted from the pre-contrast MR images, and then the subtracted MR images for each phase were used to generate MRA by using maximum intensity projection (MIP).
Venography and embolisation
The patients with chronic pelvic pain and a high degree of clinical suspicion for pelvic congestion underwent venographic evaluation for pelvic congestion with subsequent coil embolisation if it was indicated. Selective ovarian venography was performed via the transfemoral approach. With the patient in a supine position, venographic access was obtained with the Seldinger technique via the right femoral vein. The guidewire was advanced into the inferior vena cava and after placement of a 6-Fr introducer sheath and a 5-Fr Cobra catheter (Cook, Bloomington, IN) selective right ovarian venography was performed to evaluate the right ovarian vein using the Valsalva manoeuvre. After the right ovarian venography, the left ovarian vein was selectively catheterised and venography was performed.
An enlarged or incompetent ovarian vein was treated with transcatheter coil embolisation. However, we did not perform selective small collateral vein embolisations along the main ovarian vein. The indications for coil embolisation included dilatation of the ovarian vein (>5 mm), ovarian vein reflux into the pelvic cavity involving an incompetent valve, severe congestion of the pelvic venous plexus, significant stasis of contrast medium in the pelvic veins, abnormal filling of the pelvic veins across the midline and filling of vulvovaginal or thigh varicosities [15,16].
Among the 19 patients, 16 patients underwent left unilateral ovarian venous embolisation using coils. Three patients did not undergo ovarian venous embolisation because these patients had nutcracker syndrome, which requires surgery or endovascular stenting for alleviating symptoms. Embolisations were performed using an optimal size and number of coils (0.035 inch, 6–12 mm; Cook). After embolisation, repeat venography was performed to confirm occlusion of the ovarian vein as well as that of the concomitant parallel trunks.
Image analysis
Analysis of all the MR images was performed with a picture archiving and communications system (PACS) workstation monitor. Two experienced radiologists, each with more than 5 years of experience in the practice and interpretation of pelvic MR, independently evaluated both source images and volumetric MIP reconstructions of the TR-MRA. An experienced interventionalist with more than 5 years of experience in the field reviewed the conventional venography images. The conventional venography images were used as a reference standard. The observers were blinded to clinical history and the reports of the MRI and venography.
The images were reviewed to determine if differences in the detection and grading of ovarian venous reflux were seen between the TR-MRA and conventional venography. The grades of ovarian venous reflux were divided into two grades. Grade 1 reflux means the reflux was confined in the left ovarian vein and/or left parauterine veins. Grade 2 reflux means the reflux was found in the right ovarian vein, the left internal iliac vein and the right internal iliac vein, and varicosities of the vulva and thighs in addition to Grade 1 reflux. For cases with combined reflux, isolated treatment of the ovarian vein or conservative treatment can cause a poor clinical outcome [17]. However, bilateral ovarian and internal iliac vein embolisation provides improvement of the symptoms related to pelvic congestion syndrome without a significant change of ovarian function [15]. In patients with Grade 1 reflux, clinical symptoms are improved by ovarian vein embolisation only. However, in patients with Grade 2 reflux, embolisation of multiple venous channels is needed for relieving the symptoms related to pelvic congestion syndrome. Each reader indicated with arrows the presence of ovarian venous reflux and the digital images were saved on the workstation. We recorded the detected ovarian venous reflux on a data sheet on which the reflux site was listed (left ovarian vein, left parauterine plexus, right parauterine plexus, right ovarian vein, left internal iliac vein, right internal iliac vein, and varicosities of the vulva and thighs). The maximal diameters of the left ovarian veins and left parauterine veins were measured by one blinded radiologist. When there was more than one vein on the same side, the largest vein was measured.
Statistical analysis
The primary objective was to determine the diagnostic performance of TR-MRA for detecting ovarian venous reflux, with conventional venography as the reference standard. Statistical analysis was performed using the McNemar test to compare TR-MRA and conventional venography for assessing the ability of grading ovarian venous reflux. Probability values less than 0.05 were considered to be statistically significant. Separate determinations were made of the sensitivity, specificity and accuracy of TR-MRA, including 95% confidence intervals (CIs) derived from a generalised estimating equation analysis.
The sensitivity for correct grading of ovarian venous reflux was defined as the number of correctly identified cases of Grade 2 reflux evaluated on TR-MRA divided by the total number of cases of Grade 2 reflux evaluated on conventional venography. Specificity was defined as the number of cases of correctly identified Grade 1 reflux evaluated on TR-MRA divided by the total number of cases of Grade 1 reflux evaluated on conventional venography. Accuracy was defined as the number of correctly identified cases of Grade 1 and Grade 2 reflux evaluated on TR-MRA divided by the total number of cases of reflux evaluated on conventional venography. The data were analysed using a statistical software package (SPSS, v. 18, SPSS Inc., Chicago, IL).
Weighted κ statistics were calculated to assess the interobserver agreement for the grading of ovarian venous reflux. The level of agreement was defined as follows: κ-values of 0.00–0.40 indicated poor agreement, κ-values of 0.41–0.75 indicated good agreement and κ-values of 0.76–1.00 represented excellent agreement.
Results
The comparison between TR-MRA and conventional venography for grading ovarian venous reflux is shown in Table 1. In all 19 patients, left ovarian venous reflux was seen on both TR-MRA and conventional venography (Figures 1 and 2). On TR-MRA, left ovarian venous reflux was seen on the arterial phase and/or late arterial phase in all 19 patients. For both observers, there was no significant difference between TR-MRA and conventional venography for correctly grading the degree of ovarian venous reflux (p>0.05).
Table 1. Comparison between time-resolved MR angiography (TR-MRA) and conventional venography for grading of ovarian venous reflux.
| TR-MRA | Observer 1 |
Observer 2 |
||
| Conventional venography |
Conventional venography |
|||
| Grade 1 | Grade 2 | Grade 1 | Grade 2 | |
| Grade 1 | 7 | 4 | 7 | 3 |
| Grade 2 | 0 | 8 | 0 | 9 |
No significant difference was seen between TR-MRA and conventional venography for correct grading of ovarian venous reflux by two observers (p>0.05).
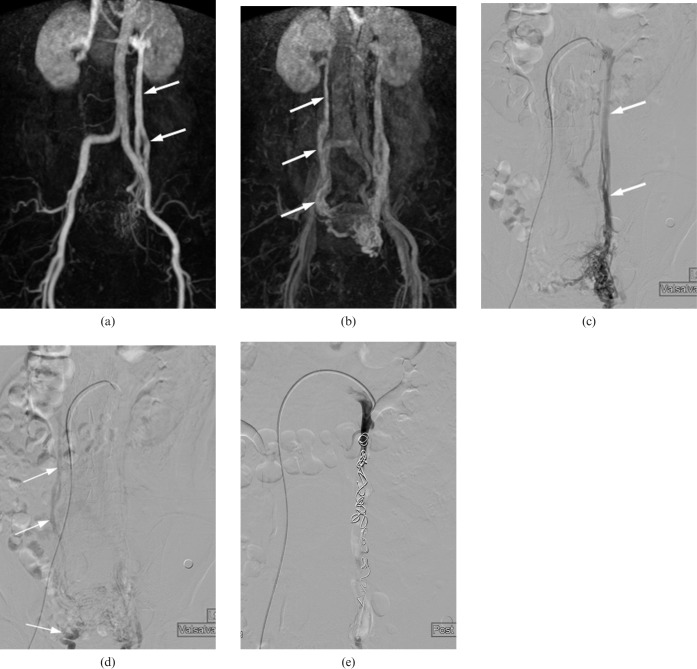
Figure 1.
A 61-year-old female with Grade 2 ovarian venous reflux. This case was correctly categorised as Grade 2 reflux on time-resolved MR angiography (TR-MRA). (a) Coronal maximum intensity projection image of TR-MRA obtained during the arterial phase shows retrograde opacificaton of contrast medium from the left renal vein to the left ovarian vein (arrows). (b) In the late arterial phase, there is dilatation of the right ovarian vein and right parauterine veins, and the right parauterine veins and right ovarian vein are opacified (arrows) owing to retrograde flow that crossed midline from left into right parauterine veins. (c, d) Selective left renal venography while performing the Valsalva manoeuvre shows the dilated left ovarian vein (thick arrows) and left parauterine veins. The right ovarian vein and right parauterine veins (thin arrows) are opacified owing to retrograde flow that crossed the midline from the left into the right parauterine plexus. (e) Transcatheter embolisation of the left ovarian vein was performed using multiple coils.
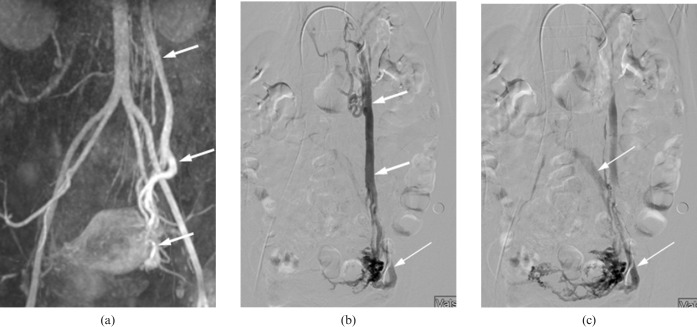
Figure 2.
A 41-year-old female with Grade 2 ovarian venous reflux. This case was incorrectly categorised as Grade 1 reflux on time-resolved MR angiography (TR-MRA). (a) Coronal maximum intensity projection image of TR-MRA obtained during the arterial phase shows retrograde opacificaton of contrast medium in the left ovarian vein and left parauterine veins (arrows). However, there is no evidence of opacification of the left internal iliac vein. (b,c) Selective left renal venography while performing the Valsalva manoeuvre shows the dilated left ovarian vein and left parauterine veins (thick arrows). The left internal iliac vein (thin arrows) is opacified owing to retrograde flow from the left parauterine varices.
The sensitivity, specificity and diagnostic accuracy of TR-MRA are listed in Table 2. The sensitivity, specificity and diagnostic accuracy of TR-MRA for grading ovarian venous reflux were found to be 66.7%, 100% and 78.9%, respectively, for observer 1 and 75%, 100% and 84.2%, respectively, for observer 2. In our study, TR-MRA showed a relatively high accuracy compared with venography (Figure 1). Of the 19 patients, 4 patients and 3 patients were incorrectly categorised by Observer 1 and Observer 2, respectively, as Grade 2 reflux to Grade 1 reflux with TR-MRA (Figure 2). There was no false-positive diagnosis of Grade 1 reflux to Grade 2 reflux on TR-MRA by both observers.
Table 2. Sensitivity, specificity and accuracy, and 95% confidence intervals (CIs) of time-resolved MR angiography (TR-MRA) for grading of ovarian venous reflux.
| Parameter | Observer 1 |
Observer2 |
||
| Value (%) | 95% CI | Value (%) | 95% CI | |
| Sensitivitya | 66.7 (8/12) | 34.9–90.1 | 75 (9/12) | 30.8–89.1 |
| Specificityb | 100 (7/7) | 59–100 | 100 (7/7) | 63.1–100 |
| Accuracyc | 78.9 (15/19) | 60–93.9 | 84.2 (16/19) | 60.4–96.6 |
Numbers in parentheses were used to calculate the percentages.
aSensitivity is the number of correctly identified cases of Grade 2 reflux on TR-MRA divided by the total number of cases of Grade 2 reflux on conventional venography.
bSpecificity is the number of correctly identified cases of Grade 1 reflux on TR-MRA divided by the total number of cases of Grade 1 reflux on conventional venography.
cAccuracy is the number of correctly identified cases of Grade 1 and 2 reflux on TR-MRA divided by the total number of cases of Grade 1 and 2 reflux on conventional venography.
The mean diameter of the left ovarian vein was 7.8±1.2 mm (range 5.2–9.7 mm) on TR-MRA and 9.2±1.7 mm (range 5.7–11.7 mm) on conventional venography. The mean diameter of the left parauterine veins was 4.7±0.7 mm (range 3.5–5.7 mm) on TR-MRA and 5.3±0.9 mm (range 3.4–6.7 mm) on conventional venography.
The weighted κ-values indicated excellent agreement between the two observers for grading ovarian venous reflux on TR-MRA (κ=0.894).
Discussion
The ovarian veins arise from the ovarian venous plexus, which has venous communications with the uterine plexus in the broad ligament. The ovarian veins join the inferior vena cava on the right side and the left renal vein on the left side. If there is incompetence of the ovarian veins, it leads to retrograde venous flow and progressive development of pelvic varicosities and dilatation of the ovarian and parauterine veins. Therefore, correct detection of ovarian vein reflux is important for the diagnosis of pelvic venous congestion and it may be crucial for determining which patients will respond to ovarian vein ligation or embolisation [11].
Several non-invasive modalities are used for the work-up of potential pelvic venous congestion, including sonogaphy, CT and MRI [6-10]. The sonographic appearance of pelvic venous congestion is multiple dilated veins around the ovary and uterus, reversed caudal blood flow in the ovarian veins, dilated arcuate veins crossing the uterine myometrium and polycystic changes of the ovary [6]. However, sonography does not readily show the ovarian veins. On the static CT and MR images, pelvic venous congestion was revealed as ovarian vein dilatation and early filling of the ovarian veins and dilated, tortuous, enhancing tubular structures near the ovaries and uterus [7,10,18]. However, the accurate determination of the direction of flow in the ovarian veins is difficult on the static CT and MR images.
TR-MRA has been proven to be a quick, non-invasive technique that allows visualisation of the blood flow dynamics. This technique has been shown to be highly sensitive for detecting pathology in a variety of blood vessels and body parts when compared with conventional angiography [11-14]. The findings of the present study are that TR-MRA is almost equal to conventional venography for detecting ovarian venous reflux and TR-MRA is well suited as a screening method for the initial evaluation of patients with suspected pelvic venous congestion [11]. In addition, TR-MRA may be more specific than conventional venography by virtue of its lack of disturbance of the normal physiological haemodynamics in the left renal vein and ovarian veins [11]. Kim et al [11] asserted that TR-MRA is a useful imaging technique for the detection of ovarian vein reflux, and it could become the gold standard for the evaluation of pelvic venous congestion and chronic pelvic pain. However, the correlation of TR-MRA with conventional venography for detecting ovarian vein reflux was not assessed in that study.
In our study, there was no significant difference between TR-MRA and conventional venography for grading the degree of ovarian venous reflux. The sensitivity, specificity and diagnostic accuracy of TR-MRA were found to be 66.7%, 100% and 78.9%, and 75%, 100% and 84.2%, respectively, for the two observers. Although the specificity for the diagnostic performance was higher, the sensitivity was lower. Four patients and three patients with Grade 2 ovarian venous reflux were incorrectly categorised as Grade 1 reflux according to TR-MRA by Observer 1 and Observer 2, respectively. The reasons for this result may be related to the difference in haemodynamics between TR-MRA and conventional venography. As seen on conventional venography, an incompetent ovarian vein is more dilated and more easily visible by artificially increasing the pressure of the left renal vein by selective injection of contrast medium into the left renal vein [11]. Therefore, conventional venography shows additional findings such as varicosities of the vulva and thighs.
In our study, retrograde ovarian venous reflux was seen on the arterial phase and/or late arterial phase on TR-MRA. Kim et al [11] reported that the average time to ovarian vein opacification after abdominal aortic enhancement on TR-MRA was 7–32 s (mean 15 s). Our results were similar to those of that previous study. In our study, the arterial and late arterial phases were finished within 35 s after abdominal aortic enhancement on TR-MRA. In these phases, opacification of the left ovarian vein and/or parauterine veins indicates ovarian venous reflux.
Ovarian venous reflux can be demonstrated with CT. On CT, opacification of the parauterine veins after ovarian vein opacification indicates contrast flow from the left ovarian vein to the parauterine vein [19]. The scanning delay time of the CT examination is 20 or 30 s for a single-detector helical scanner [20] and 65–95 s for an 8-detector scanner [19]. Although CT may demonstrate the retrograde ovarian vein flow and it may exclude other pelvic pathologies that may be the cause of chronic pelvic pain, combined pelvic MRI and TR-MRA provide dynamic imaging of the ovarian vein and combined pelvic MRI and TR-MRA can easily exclude other pelvic pathologies that may be the cause of chronic pelvic pain such as endometriosis, uterine myoma, pelvic inflammatory disease and ovarian cysts [11].
The normal range of diameters of competent left ovarian veins is between 3.2 mm and 3.6 mm [4,21,22]. The diameter of the ovarian veins in patients with pelvic congestion syndrome on sonography or CT is between 7 mm and 8 mm [6,9,10,20]. In our study, the mean diameter of the left ovarian vein was 7.8±1.2 mm (range 5.2–9.7 mm) on TR-MRA. Our results are similar to those of previous studies [9,10,20]. The mean diameter of the left ovarian vein was 9.2±1.7 mm (range 5.7–11.7 mm) on conventional venography in our study. The difference in the mean diameter of the left ovarian vein between TR-MRA and conventional venography is due to the pressure effect on the left ovarian vein by selective injection of contrast medium into the left renal vein and the radiographic magnification of conventional venography. Hiromura et al [19] reported that the mean diameter of the right and left parauterine veins on multidetector CT was 5.9±1.6 mm (range 4.3–8 mm) in patients with severe left ovarian venous reflux. In our study, the mean diameter of the left parauterine veins was 4.7±0.7 mm (range 3.5–5.7 mm) on TR-MRA and 5.3±0.9 mm (range 3.4–6.7 mm) on conventional venography. We suggest that the difference in the mean diameter of the parauterine veins between our study and the previous study [19] is related to the different degree of retrograde ovarian venous reflux between the two studies.
This study had a number of limitations that should be considered. First, the patient population was small and the study design was retrospective. Thus, further studies with larger sample sizes and prospective study will be necessary to more fully examine the usefulness of TR-MRA. Second, all 19 patients in our study were positive for reflux; therefore, it is impossible to know the specificity of TR-MRA for detecting ovarian venous reflux. As there were no negative cases in the sample, there is no way of knowing how frequently TR-MRA yields false-positive results. There was an inevitable referral bias because if ovarian venous reflux was not seen on TR-MRA, then we did not obtain conventional venography at our hospital. A control group would have been helpful as it is known that reflux is often present in asymptomatic patients. However, we did not use a control group in this study and this may be another limitation of this study. Finally, ovarian venous reflux by itself is not enough to make the diagnosis of pelvic venous congestion because reflux into the left ovarian vein and the associated parauterine veins is often seen in asymptomatic multiparous females [18,19]. However, we believe that our patients could be diagnosed as having pelvic congestion syndrome because our patients had chronic pelvic pain of at least 6 months' duration and they had no definite pelvic lesion such as adenomyosis, huge uterine myomas or endometriosis on pelvic MRI.
In conclusion, TR-MRA is a useful imaging technique for the detection and grading of ovarian venous reflux. Therefore, we believe that TR-MRA is an accurate method for accessing pelvic venous congestion.
References
- 1.Robinson JC. Chronic pelvic pain. Curr Opin Obstet Gynecol 1993;5:740–3 [PubMed] [Google Scholar]
- 2.Jamieson D, Steege J. The prevalence of dysmenorrhea, dyspareunia, pelvic pain, and irritable bowel syndrome in primary care practices. Obstet Gynecol 1996;87:55–8 [DOI] [PubMed] [Google Scholar]
- 3.Hobbs JT. The pelvic congestion syndrome. Br J Hosp Med 1990;43:200–6 [PubMed] [Google Scholar]
- 4.Beard RW. Diagnosis of pelvic varicosities in women with chronic pelvic pain. Lancet 1984;2:946–9 [DOI] [PubMed] [Google Scholar]
- 5.Ganeshan A, Upponi S, Hon LQ, Uthappa MC, Warakaulle DR, Uberoi R. Chronic pelvic pain due to pelvic congestion syndrome: the role of diagnostic and interventional radiology. Cardiovasc Intervent Radiol 2007;30:1105–11 [DOI] [PubMed] [Google Scholar]
- 6.Park SJ, Lim JW, Ko YT, Lee DH, Yoon Y, Oh JK, et al. Diagnosis of pelvic congestion syndrome using transabdominal and transvaginal sonography. AJR Am J Roentgenol 2004;182:683–8 [DOI] [PubMed] [Google Scholar]
- 7.Asciutto G, Mumme A, Marpe B, Koster O, Asciutto KC, Geier B. MR venography in the detection of pelvic congestion syndrome. Eur J Vasc Endovasc Surg 2008;36:491–6 [DOI] [PubMed] [Google Scholar]
- 8.Pagani JJ, Thomas LL, Bernardino ME. Computed tomographic manifestations of abdominal and pelvic venous collaterals. Radiology 1982;142:415–19 [DOI] [PubMed] [Google Scholar]
- 9.Coakley FV, Varghese SL, Hricak H. CT and MRI of pelvic varices in women. J Comput Assist Tomogr 1999;23:429–34 [DOI] [PubMed] [Google Scholar]
- 10.Rozenblit AM, Ricci ZL, Tuvia J, Amis ES., Jr Incompetent and dilated ovarian veins: a common CT finding in asymptomatic parous women. AJR Am J Roentgenol 2001;176:119–22 [DOI] [PubMed] [Google Scholar]
- 11.Kim CY, Miller MJ, Merkle EM. Time-resolved MR angiography as a useful sequence for assessment of ovarian vein reflux. AJR Am J Roentgenol 2009;193:W458–63 [DOI] [PubMed] [Google Scholar]
- 12.Kim CY, Mirza RA, Bryant JA, Whiting ED, Delong DM, Spritzer CE, et al. Central veins of the chest: evaluation with time-resolved MR angiography. Radiology 2008;247:558–66 [DOI] [PubMed] [Google Scholar]
- 13.Masunaga H, Takehara Y, Isoda H, Igarashi T, Sugiyama M, Isogai S, et al. Assessment of gadolinium-enhanced time-resolved three-dimensional MR angiography for evaluating renal artery stenosis. AJR Am J Roentgenol 2001;176:1213–19 [DOI] [PubMed] [Google Scholar]
- 14.Swan JS, Carroll TJ, Kennell TW, Heisey DM, Korosec FR, Frayne R, et al. Time resolved three-dimensional contrast-enhanced MR angiography of the peripheral vessels. Radiology 2002;225:43–52 [DOI] [PubMed] [Google Scholar]
- 15.Kim HS, Malhotra AD, Rowe PC, Lee JM, Venbrux AC. Embolotherapy for pelvic congestion syndrome: long-term results. J Vasc Interv Radiol 2006;17:289–97 [DOI] [PubMed] [Google Scholar]
- 16.Kwon SH, Oh JH, Ko KR, Park HC, Hur JY. Transcatheter ovarian vein embolization using coils for the treatment of pelvic congestion syndrome. Cardiovasc Intervent Radiol 2007;30:655–61 [DOI] [PubMed] [Google Scholar]
- 17.Asciutto G, Asciutto KC, Mumme A, Geier B. Pelvic venous incompetence: reflux patterns and treatment results. Eur J Vasc Endovasc Surg 2009;38:381–6 [DOI] [PubMed] [Google Scholar]
- 18.Nascimento AB, Mitchell DG, Holland G. Ovarian veins: magnetic resonance imaging findings in an easy asymptomatic population. J Magn Reson Imaging 2002;15:551–6 [DOI] [PubMed] [Google Scholar]
- 19.Hiromura T, Nishioka T, Nishioka S, Ikeda H, Tomita K. Reflux in the left ovarian vein: analysis of MDCT findings in asymptomatic women. AJR Am J Roentgenol 2004;183:1411–15 [DOI] [PubMed] [Google Scholar]
- 20.Desimpelaere JH, Seynaeve PC, Hagers YM, Appel BJ, Mortelmans LL. Pelvic congestion syndrome: demonstration and diagnosis by helical CT. Abdom Imaging 1999;24:100–2 [DOI] [PubMed] [Google Scholar]
- 21.Ahlberg NE, Bartley O, Chidekel N. Right and left gonadal veins: an anatomical and statistical study. Acta Radiol Diagn 1966;4:593–601 [DOI] [PubMed] [Google Scholar]
- 22.Giacchetto C, Catizone F, Cotroneo GB, Cavallaro V, Cammisuli F, Minutolo V, et al. Radiologic anatomy of the genital venous system in female patients with varicocele. Surg Gynecol Obstet 1989;169:403–7 [PubMed] [Google Scholar]