Abstract
A push for the use of evidence‐based medicine and evidence‐based practice patterns has permeated most health care disciplines. The use of evidence‐based practice in sports physical therapy may improve health care quality, reduce medical errors, help balance known benefits and risks, challenge views based on beliefs rather than evidence, and help to integrate patient preferences into decision‐making. In this era of health care utilization sports physical therapists are expected to integrate clinical experience with conscientious, explicit, and judicious use of research evidence in order to make clearly informed decisions in order to help maximize and optimize patient well‐being. One of the more common reasons for not using evidence in clinical practice is the perceived lack of skills and knowledge when searching for or appraising research. This clinical commentary was developed to educate the readership on what constitutes evidence‐based practice, and strategies used to seek evidence in the daily clinical practice of sports physical therapy.
Keywords: Evidence‐Based Medicine, Sports Physical Therapy, Rehabilitation
INTRODUCTION
The American Physical Therapy Association 2020 Vision Statement suggests that physical therapists and physical therapist assistants will render evidence‐based services throughout the continuum of care and improve quality of life for our society. This statement is in sharp contrast to what actually occurs in typical practice. According to Shuster and colleagues, 30‐40% of patients do not receive care according to current scientific evidence and about 20‐25% of care provided is not needed or is potentially harmful.1 A study of 321 physical therapists in England and Australia found that the basis for over 90% of each group's choice of treatment interventions reflected what was taught during their initial training despite more recent research and outcomes findings presented in the medical literature.2 Actually, research literature was ranked as least important as a basis for choosing treatment interventions and techniques, and ideas gleaned from review articles ranked higher. Jette and colleagues report that although most agree that evidence‐based practice (EBP) is important, far less make time to practice it due mainly to lack of time and lack of skills necessary to implement its use.3 Another serious problem faced by physical therapists is that rehabilitation journals may publish research articles with lower methodological quality, as described by Miller, ‐McKibbon and Haynes who found that only 19 of 179 journal articles published in four different physical therapy journals met standards of rigor as defined by the Hedges Project Criteria.4 Adding salt to our physical therapy wounds is the fact that many of these research articles do not even study clinical populations.5 Fortunately for physical therapists, this appears to be a more universal problem, and other professions such as orthopedic surgery and other medical specialties suffer from the same. The percentage of Level I studies published in the prestigious Journal of Bone and Joint Surgery has slowly increased from 4% to 21% between the years of 1975 and 2005.6 It is the hope of the authors that this manuscript will dispel some of the fears associated with using Evidence‐based medicine (EBM) in your day‐to‐day practice of sports physical therapy. Finding the evidence needed to guide and inform clinical practice is getting easier than ever before! The goal of this commentary is that the readership of IJSPT will have the necessary tools to practice using EBP. This commentary is designed to present key skills and tips in order to practice EBM in a clinical setting.
What is Evidence‐Based Medicine (EBM)/Practice (EBP)
EBM was developed due to a clear need to optimize quality of patient care. EBM has been touted as an effective series of mechanisms not only for improving health care quality, but also for reducing medical errors precipitated in part by clinical practice variation. In present day medical practices, clinicians are expected to integrate clinical experience with conscientious, explicit and judicious use of research evidence in order to make clearly informed decisions to help maximize and optimize patient well‐being. Although EBM has been a buzzword for some time now, many sports physical therapists are still not completely sure of how to integrate EBM into daily clinical practice and how to use it as a part of their continued professional growth. EBP is an approach to health care in which sports physical therapists use the best available evidence to make clinical decisions for individual patients during daily clinical practice. This article is the first of this special collection presented in the International Journal of Sports Physical Therapy (IJSPT) – A User Friendly Guide to Publishing in the International Journal of Sports Physical Therapy. This commentary will serve as an overview while others that follow will describe details about authorship and publishing in IJSPT.
Interest in EBM surged following the coining of the term published in JAMA in 1992.7 Sackett et al described EBM as “integration of the best research evidence with clinical expertise and patient values and circumstances to make clinical decisions”.8, p.71
What does this mean to us as sports physical therapists? Best research evidence means clinically relevant research sometimes from basic sciences of medicine, but especially from patient‐centered clinical research into the accuracy and precision of diagnostic tests (including the clinical examination), the power of prognostic markers, and the efficacy and safety of therapeutic, rehabilitation, and preventive strategies. The most updated clinical research does more than simply suggest new ways to diagnose pathology and approach treatments. It can often invalidate older ways of diagnosis and methods of treatment and replace them with more powerful, valid, or successful methods. Clinical expertise means the ability to use clinical skills and past experience to rapidly identify each athlete's unique health state and diagnosis, their individual risks and benefits associated with potential interventions, while skillfully integrating their personal values and expectations. Clinical expertise, personal to each physical therapist, is developed over time and requires exposure to variety in patient care, and ultimately is very hard to replace. It is clinical expertise that allows each physical therapist to apply new evidence from peer‐reviewed journals, symposia, and meetings. Each athlete is a unique individual with their own concerns, experiences, priorities and preferences. Patient values means the unique preferences, concerns and expectations each athletic patient brings to a clinical encounter. These must be integrated into clinical decisions if they are to serve the athlete. A relevant clinical decision must integrate the athlete's unique considerations into the decision‐making process.9 Patient circumstances means the athletic patient's individual clinical state and clinical setting.10
Although this concept is not entirely new it has seen resurgence since the early 1990's. In sports physical therapy, EBM should be based upon patient‐centered, clinically relevant research found in literature related to diagnostic tests, intervention techniques, preventive programs, and prognostic markers of sports related injuries. As a reader of the International Journal of Sports Physical Therapy, you already realize that this is a daunting task, as new evidence is continuously emerging. Evidence at any time can affect the use of or change thinking regarding commonly used and accepted methods of examination or treatment of musculoskeletal conditions. Therefore, what constitutes an acceptable method of treatment may change at any time. Reviewing and assimilating the abundance of evidence can be a daunting task as the volume of published literature continues to rise. There has been an explosion in the number of randomized controlled trials in physical therapy over the last 80 years. In 1929 there was only one randomized controlled trial related to physical therapy interventions published. This has jumped to roughly 12,000 randomized controlled trials in 2009.11 In a study of family physicians it was determined that clinical questions about patients care arose 3.2 times for every 10 patients seen, yet physicians did not seek an answer 64% of the time.12 According to Ely, most clinical questions don't get answered and most of the times that is because the physician does not want or have time to pursue the answer.12 The most common reason for not pursuing an answer was that after voicing some uncertainty, the doctor felt that a reasonable decision could be based on his or her current knowledge.
How to Use EBM in Sports Physical Therapy Practice
Sackett et al and others have proposed several steps that will be discussed in greater detail throughout this manuscript.8,10
-
1)
Convert the need for information (about prevention, diagnosis, prognosis, therapy, causation, etc.) into an answerable, clinically relevant question.
-
2)
Track down and search for best evidence with which to answer the question.
-
3)
Critically appraise the evidence for its validity (closeness to the truth), impact (size of the effect), and applicability (usefulness in our clinical practice).
-
4)
Integrate the critical appraisal with clinical expertise and with your patient's unique biology, values and circumstances.
-
5)
Evaluate effectiveness and efficiency in executing steps 1‐4 and seeking ways to improve upon them before next time.
Straus and colleagues have found that real world clinical incorporation of these steps is done in several fashions.10 In many instances the first four steps are done by clinicians, while the final step of evaluation of effectiveness is left out. Another common method is to skip steps 1‐3 and use a source of information that has already undergone review by another clinician. An example of this might be integrating findings from a systematic review or meta‐analysis, or evidence summaries that have been written or presented by others, without personal review. A final method is to follow recommendations of respected leaders in sports physical therapy. In reality most clinicians probably use all three of these methods of practicing EBM at one time or another depending on the condition that they are using it for. In select sports physical therapy encounters, going through all steps listed above is probably very prudent as you want to be as up to date as possible. An example might be the clinical usefulness of joint mobilization on a postoperative knee or shoulder that has become stiff. However, for a condition that is rarely seen such as acute rhabomyolysis the sports therapist may accept the recommendations that are received from other experts more experienced with this condition.
Defining a Clinical Question
Evidence‐based clinical questions should start and end with the athletic patient in mind. Clinical situations arise daily in the sports physical therapy clinic which requires asking a clinical question about which course of action is best. If the athlete has an unusual pathology or a condition that is rarely seen, the clinician may be uncertain of appropriate care. Without a doubt, in this case, there is a need for relevant information related to diagnosis, prognosis, or management of the condition(s). This may mean that evidence must be searched for. There may not always be an easily found protocol such as those for SLAP tears or anterior cruciate ligament reconstructions. For example, the therapist may suspect a deep venous thrombosis which may be a life threatening situation, or an athlete presents following a medial patellofemoral ligament reconstruction which is a novel procedure for the therapist. In these instances the therapist may not have an easy protocol “cookbook” to follow and will come to a point in the clinical decision‐making process where answerable questions need to be formulated. Questions that need to be asked may pertain to one or more of the following and evolve around care of the patient (Table 1).10
Table 1.
Central Issues in Clinical Work, Where Clinical Questions Arise.
|
Taken from: Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence‐Based medicine: How to Practice and Teach it. 4th ed. New York, NY: Churchill Livingstone; 2011 page 18. With permission.
Clinically based questions can come in two general forms: background or foreground questions. A background question is needed to understand the nature of an athlete's problem, a test, or a treatment. The essential components of a good background question are 1) a question root (who, what, where, when, how and why), and a verb. 2) A disorder, test, treatment, or other aspect of care. An example of several background questions relevant to sports physical therapy include:
-
–
How long does it take scar tissue to create limited motion in the knee following surgery?
-
–
What are common signs and symptoms of a superior labral tear?
-
–
What are the causes of shoulder internal impingement in an overhead athlete?
-
–
Is it possible to return to unrestricted pitching following ulnar collateral ligament reconstruction of the elbow?
A foreground question helps the clinician and athlete to make decisions about the specific management of their athletic condition or injury, and/or management of that problem. These questions are a little larger and have 4 essential components that can use the PICO format.10 The PICO acronym is described below, followed by several foreground questions that may be asked by a sports physical therapist.
-
1)
P: Patient, population, predicament, or problem. Information involves demographics such as age, sex and race. Other important information could include social situations, resources and patient values, and the clinical setting.
-
2)
I: Intervention, exposure, test, or other agent. What type of intervention is being considered? Is this a medication of some type or a form of diagnostic imaging such as radiograph or ultrasound imaging? Or is the intervention at this point a given special test the sports therapist is using to determine the pathology?
-
3)
C: Comparison, intervention, exposure, test, etc., if relevant. The treatment itself can only be compared with something else other than itself. The comparison may be with another medication, another form of imaging such as magnetic resonance imaging, to a current standardized treatment or to no treatment at all.
-
4)
O: Outcomes of clinical importance, including time when relevant. What would be the desired effect you would like to see? What effects are not wanted? Are there any side effects involved with this form of testing or treatment?
-
–
In adolescents following anterior cruciate ligament reconstruction, would the addition of neuromuscular electrical stimulation early in therapy result in better return of quadriceps motor control and, therefore, better graft stability?
-
–
Will the initiation of early passive range of motion result in improved subjective outcome scores compared to delayed range of motion for college‐aged pitchers with small undersurface rotator cuff tears?
As a sports physical therapist the amount of time that is spent using the two different types of questions will vary with your experience. Early in your career when you have limited clinical experience you may utilize an overabundance of background questions simply to better understand a given pathology. As you become more seasoned and have a general knowledge of most conditions you are more likely to ask foreground types of questions. This is by no means meant to imply that the seasoned clinician will not need to ever ask a background question or that a more novice clinician may not need to ask a foreground question. Each of these types of questions can be used by either clinician regardless of their level of experience.
Once a patient‐centered clinical question has been devised, it is important to plan a strategy for a search before jumping into the wide variety of sources of evidence that are available. The next section of this manuscript therefore will describe how to search for the best available evidence.
How to Search for Best Available Evidence
Searching for the best available evidence can be a daunting task without knowledge of efficient search strategies. As mentioned previously, the number of randomized controlled trials has grown exponentially, so much that a physical therapist who graduated in 1980 now has access to 25 times more randomized controlled trials about physical therapy treatment than when they graduated.13 Moreover, finding an article that meets basic criteria for quality and relevance among the throngs of available journals may be like looking for a needle in a haystack. McKibbon et al stated that the number of articles a clinician would need to read to find just one article that meets such basic criteria among the largest four general/family practice journals is between 107 and 226 articles.14
At the risk of sounding like the imperial authorities in Ray Bradbury's Fahrenheit 451, the harvesting of the best available evidence should begin by burning (or at least dismissing) all textbooks with the exception of the best of a new breed of them. In most texts, it's not possible to tell which information is current or supported by anything more than anecdotal evidence. Therefore, while some useful information about background questions may be found in texts, most are significantly suboptimal when attempting to find the best evidence‐based answers for clinical foreground questions.15 For example, textbooks may be able to accurately articulate that patients with patellofemoral pain syndrome often display reduced lower extremity muscle function; however, a 2011 study concerning patellofemoral pain syndrome is able to provide concrete evidence that a group of females with the condition generated 22% less hip abductor and 21% less hip external rotator force output on a hand‐held dynamometer than controls.16
Multiple online databases exist from which clinicians can search for evidence to support their practice. PubMed (http://www.ncbi.nlm.nih.gov/pubmed/), EBSCO (http://www.ebsco.com/), Ovid (http://www.ovid.com/), and Google Scholar (http://scholar.google.com/) are among the most popular. For the purpose of brevity, this manuscript will describe searching from PubMed. Moreover, the listed databases all have comprehensive “Help” tabs that explain how to search the respective databases in depth; therefore, the information here will focus on describing components of efficient searches for clinical research, assuming a reader with basic knowledge of online searching.
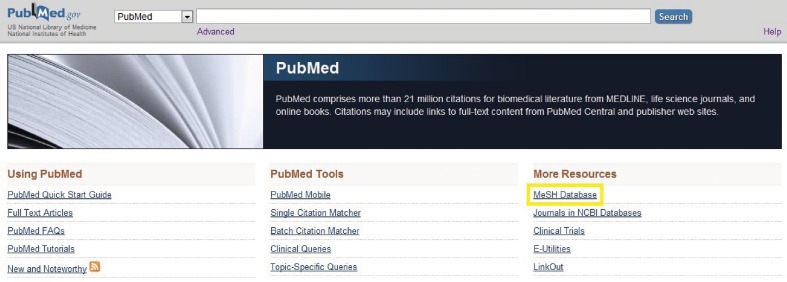
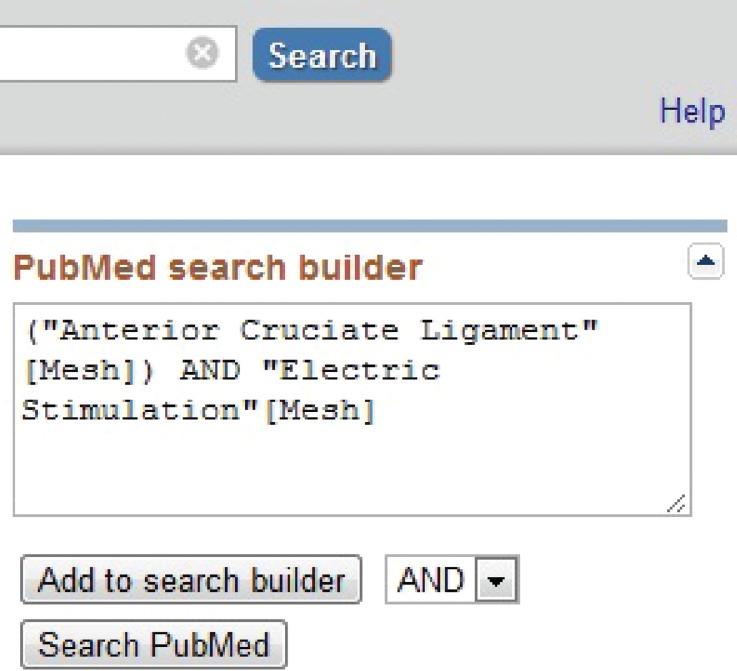
After developing a PICO question as described in the previous section, it is important to select the best words or phrases to use as search terms. Given the aforementioned PICO question, “In adolescents following anterior cruciate ligament reconstruction, would the addition of neuromuscular electrical stimulation early in therapy result in better return of quadriceps motor control and, therefore, better graft stability?,” the phrases “anterior cruciate ligament reconstruction” and “neuromuscular electrical stimulation” are essential to the query. The next step is to determine which words or phrases are most recognizable by the database. MeSH (Medical Subject Headings) is the vocabulary thesaurus used for indexing articles to PubMed (Figure 1) (http://www.ncbi.nlm.nih.gov/mesh). For example, the terms “ACL” and “neuromuscular electrical stimulation” are not recognized by the database and their use, therefore, would result in suboptimal search outcomes. “Anterior cruciate ligament” and “electric stimulation,” however, are recognized subject headings relevant to this example. Terms discovered within the MeSH database can be selected and automatically included in a search builder from which PubMed searches can be performed with the option of selecting the AND, OR, or NOT Boolean operators (Figure 2). The Boolean search operators define relationships between search terms and assist with providing more focused results than single search words or terms.
Figure 1.
The location of the MeSH link on PubMed's home page is indicated by the addition of the yellow highlighted rectangle. MeSH (Medical Subject Headings) is the vocabulary thesaurus used to index articles to PubMed.
Figure 2.
The textbox of the PubMed search builder within its MeSH database is shown. The dropdown box in the lower right hand corner can be used to select the AND, OR, or NOT Boolean operators.
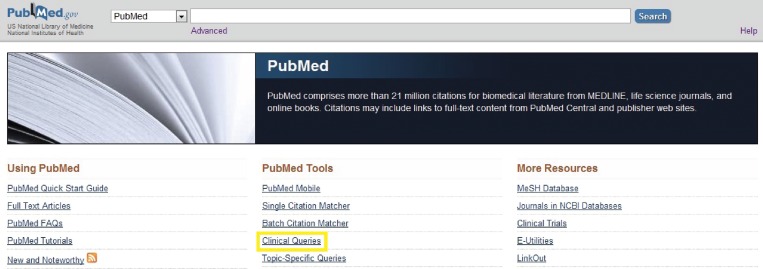
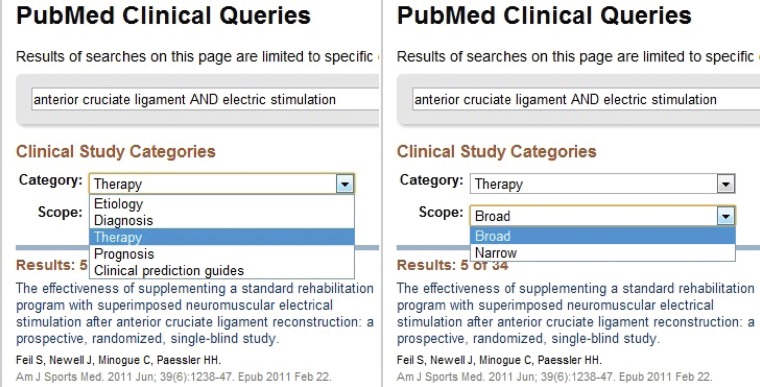
Another excellent launch pad for a search with relevant words or phrases is PubMed's Clinical Queries tool (Figure 3). Searches within Clinical Queries are able to limit results to specific clinical research areas. For example, search results can be filtered through the categories of Etiology, Diagnosis, Therapy, Prognosis, and Clinical prediction guides using a dropdown bar. Moreover, each Clinical Queries search can be further filtered with a Broad or Narrow scope with another dropdown bar (Figure 4). Narrow searches deliver clinical trials, randomized controlled trials, and systematic reviews. Broad searches deliver similar research with the inclusion of other review articles. The use of these filters results in a significantly more focused delivery of evidence than using the same terms to search from the PubMed home page. For example, searching “anterior cruciate ligament AND electric stimulation” from PubMed's home page delivered 67 results in September of 2012; whereas the same search using a Narrow scope filter in the Therapy category of Clinical Queries resulted in 23 relatively higher quality evidence more specific to therapeutic intervention.
Figure 3.
The location of the Clinical Queries link on PubMed's home page is indicated by the addition of the highlighted yellow rectangle. Searches within Clinical Queries are to able limit results to specific clinical research areas.
Figure 4.
Dropdown bars displaying the category and scope filters within PubMed's Clinical Queries tool are shown. Narrow searches deliver clinical trials, randomized controlled trials, and systematic reviews. Broad searches deliver similar research with the inclusion of other review articles.
Critically Appraising Evidence
Once evidence relevant to one's clinically‐oriented question is found, it must be critically appraised to determine its value and subsequent benefit to clinicians and patients. The Centre for Evidence Based Medicine describes a hierarchy of evidence with the use of numerical levels and letter grades to define the quality of each piece of clinical evidence (http://www.cebm.net/index.aspx?o=1025). Higher levels of study designs allow clinicians to have increased confidence in the conclusions drawn within the study. Levels described in the Therapy column of the Centre for Evidence Based Medicine's hierarchy are as follows (listed from best evidence to that in which clinicians can place least confidence): systematic reviews (SR) of randomized controlled trials (Level 1a); individual randomized controlled trial (1b); SR of cohort studies (2a); individual cohort studies (2b); SR of case‐control studies (3a); individual case control study (3b); case‐series (4); and expert opinion without explicit clinical appraisal, or based on physiology (5). These levels of evidence can sometimes be found within the online abstracts of articles, and they are now being noted in most respected journals, such as the International Journal of Sports Physical Therapy, within their respective articles.
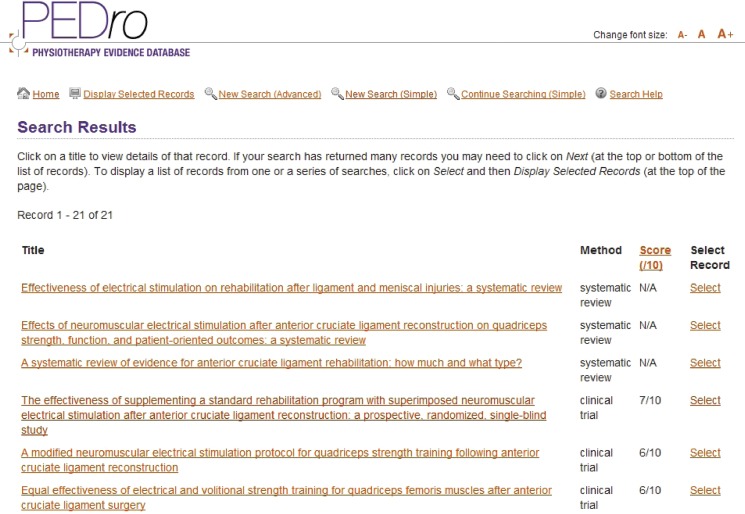
One efficient method for further determining the quality of clinical trial evidence is by using the PEDro score (http://www.pedro.org.au/english/downloads/pedro‐scale/) and/or the corresponding PEDro website database. PEDro is the Physiotherapy Evidence Database, a free database of over 22,000 trials, reviews, and guidelines with links to citation abstracts and full texts where possible ((http://www.pedro.org.au/). The PEDro database rates evidence with a score out of ten based on the following validity criteria of a research study: eligibility criteria specified; subjects randomly allocated to groups; allocation was concealed; homogeneity of groups; blinding of all subjects; blinding of all therapists administering treatment; blinding of all assessors who measured an outcome; measures of at least one outcome were obtained from more than 85% of the sample; all subjects received the treatment or control condition, otherwise there was an “intention to treat” analysis; the results of between‐group statistical comparisons are reported; and the study provides point and variability measures for at least one outcome (http://www.pedro.org.au/english/downloads/pedro‐scale/). Search results within PEDro will display relevant systematic reviews; however, scoring with the above criteria is not applicable to such reviews as it is to clinical trials (Figure 5).
Figure 5.
Search results are shown for “anterior cruciate ligament AND electric stimulation” within PEDro. PEDro scoring is not as applicable to systematic reviews as it is to clinical trials; nonetheless, they are listed first.
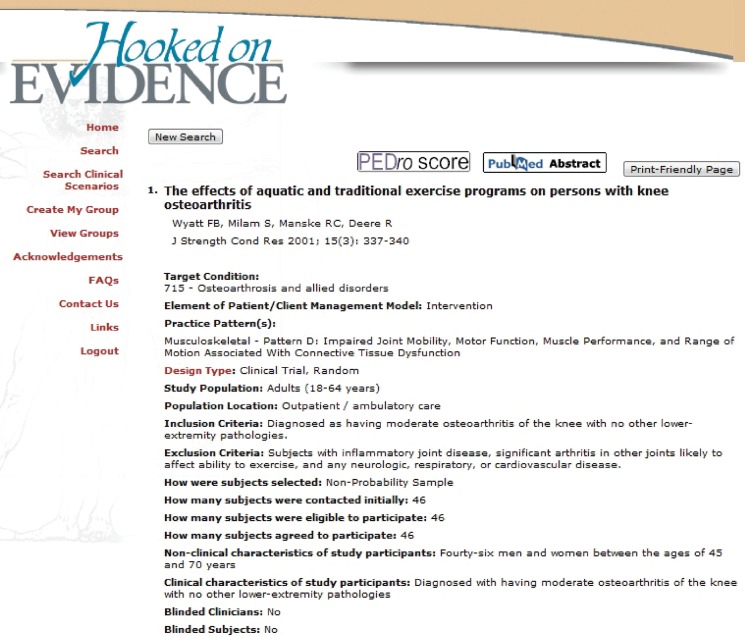
In the event that evidence is not yet appraised within PEDro, the presence of the aforementioned validity criteria can be determined by searching the full text of an article or turning to the American Physical Therapy Association's (APTA) growing database called “Hooked on Evidence” (http://www.hooked onevidence.com/). Hooked on Evidence aids in critically appraising evidence by dissecting study specifics and presenting them in an organized fashion. In addition to the majority of validity criteria rated by PEDro, Hooked on Evidence provides additional description of an article's study population and intervention specifics, as well as visual representations of study data. Moreover, if a study has been rated using the PEDro score, Hooked on Evidence provides a link to the scoring above the citation's title (Figure 6).
Figure 6.
The specifics of a clinical trial detailed by the American Physical Therapy Association's “Hooked on Evidence” is shown. Hooked on Evidence aids in critically appraising evidence by dissecting study specifics, presenting them in an organized fashion, and providing links to PEDro scoring when available.
An article's level within the research hierarchy, study purposes, compositions of participants, and measures of methodological quality are all important components to consider when critically appraising evidence.17 The use of PEDro scoring and APTA's Hooked on Evidence is extremely helpful for determining such components. It is only after critically appraising the research that a clinician can judge the amount of confidence he or she can have in the application of such evidence to clinical practice.
Integration and Application of Evidence with Sport Physical Therapy
Now that you have found information that you have determined to be valuable; meaning you have determined it was reliable, valid, clinically important information related to your given clinically‐oriented question, it is time to integrate this newly found information into the particular situation involving your athlete. This implies making decisions about how to apply the findings to treat the athlete sitting in front of us! The ability to fully integrate this best evidence with clinical experience into practice is twofold: (1) one must be comfortable and capable with integrating EBM into his or her practice, and (2) one must be able to understand and incorporate the patient's needs and wants to establish the best course to follow in terms of treatment and management.9
Remember that just because you have found information to be important does not mean it must be included in how you examine, evaluate, or treat your given patient. The information gained may not be right for your given case, patient, or client. As described in this article EBM should always be patient centered and in some instances information gained may not be able to be utilized. For example your search may indicate that in most patients with a given inflammatory condition treatment with xx brand of steroidal medication may be best in conjunction with physical rehabilitation. If you patient has an extreme allergy to that medication, despite high level evidence indicating efficacy with its use – this option is not going to work for you as it is contraindicated with this patient. What if in this same instance your patient has limited insurance and it does not cover the cost of the medication? The evidence that was discovered would not be applied in this instance, due to cost. The extreme importance of an athlete's perspectives, beliefs, expectations and goals cannot be given short thrift. By considering how your athlete thinks about the available options and their relative risks, benefits, harms, costs, and inconveniences when determining options through evidence and clinical expertise, the astute therapist engages in a shared decision making process.9 In these scenarios where the evidence points to treatments that are not viable for various reasons the sports physical therapist will have to draw on past experiences and use other methods of treatment for the patient in this scenario to improve. Using EBM the clinician must factor in patient preferences, cost, and convenience. By listening to your athletic patient to understand his or her personal situations and goals and working with your informed athlete to achieve a common ground on a treatment approach, you, as the sports physical therapist can deliver effective patient‐centered care.18
Make sure to use valuable resources to obtain your information not only opinion based guidelines that are not backed by science. These opinion based guidelines have been referred to as “BOGSAT's” because they were developed by a Bunch of Old Guys Sitting Around Talking.19 There are several resources that have been developed to help busy sports physical therapists to identify and integrate the best available research evidence with their clinical expertise. Clinical guidelines have been developed based on best available evidence and provide a good starting point for commonly encountered clinical scenarios. For example, the Journal of Orthopedic and Sports Physical Therapy has published clinical guidelines on heel pain – plantar fasciitis.20 Additionally, the American Physical Therapy Association (APTA) has developed PT Now which is a tool for APTA members to gain access to clinical practice guidelines relevant to physical therapist practice. PT Now is presently in early stages of development but has been working closely with the Sports Physical Therapy Section on development of practice guidelines that will be helpful for sports physical therapists. The PT Now website link is: http://www.ptnow.org/EBPLibrary/PracticeGuidelines.aspx
Another very important aspect of integration of evidence into practice is to share your findings with others. Teach other sports physical therapists what you have found with your searches. Allow others to learn what you have found. This can be done at a regularly scheduled meetings or in a more formal “journal club” type of format in which findings are passed out prior to the meeting so that members can review evidence beforehand in hopes that better discussions will be brought forward in valuable meeting time. Another way to help integrate evidence into practice is through attendance of continuing education meetings and workshops that are evidence‐based. Evidence does exist that demonstrates educational meetings alone or combined with other interventions, can improve professional practice and healthcare outcome for patients.21
Evaluating Performance of EBM
The integration and application of evidence with sports physical therapy is paramount considering a study done by McCluskey and Lovarini. These authors studied the extent to which practice behavior changed as a response to an evidence‐based education intervention. They concluded that EBP skills and knowledge improved markedly; however, changes in behavior were small.22 Such results emphasize the importance of establishing new routines and priorities around EBP, as well as the need to continually evaluate the performance of the EBP approach. Behavior change may take months or even years, but it's imperative in order to provide the best care to athletes.
Evaluation of performance in practicing EBM is essentially the process of answering questions such as the following:15
-
1.
Am I asking any well‐formulated questions?
-
2.
Am I becoming more efficient in my searching?
-
3.
Am I critically appraising evidence?
-
4.
Am I integrating critical appraisals into my practice?
-
5.
Have I done any audits of my diagnostic, therapeutic, or other performances, including measures of patient satisfaction?
Outcome measures such as the DASH (Disability of Arm, Shoulder, and Hand), LEFS (Lower Extremity Functional Scale), and Oswestry Low Back Pain Disability Questionnaire are helpful tools for assessing therapeutic performance. Interestingly, estimates suggest that only about 50% of physical therapists in the United States use standardized tools for measures of outcomes.23 A challenge for physical therapists and other health care professionals is to remain open and flexible to new ways of practicing. As part of a community, a movement of people who are exploring, discussing, sharing, and experiencing new understandings of how to heal and prime the human body, we need to remain open to change. Things that have been said, done, taught, and written may need to be revisited, rethought, and reworked. The things sports physical therapists are saying, doing, and writing today will likely need to be revisited, rethought, and reworked. The previously listed questions must be asked among sport physical therapy professionals in order to evaluate our performance in the art of evidence‐based practice.
CONCLUSIONS
A sound approach to sports physical therapy practice and clinical decision‐making is the role of all sports therapists. Practicing EBM will help the sports physical therapist deal with the increasingly insurmountable growth of medical literature that is published. Additionally, practicing EBM should allow clinicians an avenue for excellence and development in clinical practice. Clinician expertise and patient values are both valued components of the decision making process of EBM and EBP. Sports physical therapist can adopt EBM and EBP approaches in their clinic, but will face challenges with less‐than ideal evidence. The less than ideal evidence is changing due to excellent sports related physical therapy journal such as IJSPT, JOSPT, and due to efforts by the APTA with the promotion of PT Now and future sources to increase knowledge and awareness of the critical evidence available for therapists. We must all continue to work together in a goal toward developing evidence. Partnerships between researchers and clinicians will continue to help the lives of our patient athletes and achieve the goal of learning new, better, quicker, and more successful methods to return our athletes to their recreational or completive sports.
REFERENCES
- 1.Schuster M, McGlynn E, Brook RH. How good is the quality of health care in the United States? Milbank Q. 1998; 76:517–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Turner P, Whitfield TW. Physotherapists' use of evidence based practice: a cross‐national study. Physiother Res Int. 1997; 2(1):17–29 [DOI] [PubMed] [Google Scholar]
- 3.Jette DU, Bacon K, Batty C, et al. Evidence‐based practice: beliefs, attitudes, knowledge, and behaviors of physical therapists. Phys Ther. 2003; 83(9):786–805 [PubMed] [Google Scholar]
- 4.Miller PA, McKibbon KA, Haynes RB. A quantitative analysis of research publications in physical therapy journals. Phys Ther. 2003; 83:123–131 [PubMed] [Google Scholar]
- 5.Robertson VJ. A quantitative analysis of research in physical therapy. Phys Ther. 1995; 75:313–323 [DOI] [PubMed] [Google Scholar]
- 6.Hanzlik S, Mahabir RC, Baynosa RC, Khiabani KT. Levels of evidence in research published in The Journal of Bone and Joint Surgery (American Volume) over the last thirty years. J Bone Joint Surg Am. 2009; 91:425–428 [DOI] [PubMed] [Google Scholar]
- 7.Evidence‐Based Medicine Working Group. Evidence‐based medicine A new approach to teaching the practice of medicine. JAMA. 1992; 268:2420–2425 [DOI] [PubMed] [Google Scholar]
- 8.Sackett DL, Rosenburg WM, Gray JA, Haynes RB, Richardson WS. Evidence‐based medicine: what it is and it isn't. BJM. 1996; 312:71–72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Karlsson J, Marx RG, Nakamura N, Bhandari M. ISAKOS Scientific Committee Research Methods Handbook. A Practical Guide to Research: Design, Execution, and Publication. Arthroscopy. 2011; 27(4):S1–S112 [DOI] [PubMed] [Google Scholar]
- 10.Straus SE, Glasziou P, Richardson WS, Haynes RB. Evidence‐based medicine. How to practice and teach it. 4th ed. Churchill Livingstone, Philadelphia, 2011, pg. 1 [Google Scholar]
- 11.Maher C. PRISMA: helping to deliver information that physical therapists need. Phys Ther. 2009; 89(9):870–872 [DOI] [PubMed] [Google Scholar]
- 12.Ely JW, Osheroff JA, Ebell MH, et al. Analysis of questions asked by family doctors regarding patient care. BMJ. 1999; 319:358–361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Maher C. PRISMA: helping to deliver information that physical therapists need. Phys Ther. 2009; 89(9):870–872 [DOI] [PubMed] [Google Scholar]
- 14.McKibbon KA, Wilczynski NL, Haynes RB. What do evidence‐based secondary journals tell us about the publication of clinically important articles in primary healthcare journals? BMC Med. 2004;6(2):33doi:10.1186/1741‐7015‐2‐33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Straus SE, Richardson WS, Glasziou P, Haynes RB. Evidence‐based medicine. How to practice and teach it. 3rd ed. Churchill Livingstone, Philadelphia, 2005, pg. 32–33 [Google Scholar]
- 16.Bolgla LA, Malone TR, Umberger BR, Uhl TL. Comparison of hip and knee strength and neuromuscular activity in subjects with and without patellofemoral pain syndrome. Int J Sports Phys Ther. 2011; 6(4):285–96 [PMC free article] [PubMed] [Google Scholar]
- 17.Gutman SA. How to appraise research: elements of sound applied design. Am J Occup Ther. 2009; 63(2):123–5 [DOI] [PubMed] [Google Scholar]
- 18.Stewart M, Brown JB, Weston WW, McWilliam CL, Feeman TR. Patient‐Centered Medicine: Transforming the Clinical Method. Oxon, UK: Radcliffe Medical Press, 2003 [Google Scholar]
- 19.White B. Making evidence‐based medicine doable in everyday practice. Family Practice Management. 2004:51–58 [PubMed] [Google Scholar]
- 20.McPoil TG, Cornwall MW, Wukich DA, Irrgang JJ, Godges JJ, Martin RL. Heel pain‐plantar fasciitis. J Orthop Sports Phys Ther. 2008; 38(4): A1–A18 [DOI] [PubMed] [Google Scholar]
- 21.Forsetlund L, Biorndal A, Rashidan A, Jamtvedt G, O'Brien MA, Wolf F, Davis D, Odgaard‐Jensen J, Oxman AD. Continuing education meetings and workshops: effects on professional practice and health care outcomes. Cochrane Database Syst Rev. 2009;15(2). DOI:10.1002/14651858.CD003030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.McCluskey A, Lovarini M. Providing education on evidence‐based practice improved knowledge but did not change behaviour: a before and after study. BMC Med Educ. 2005;5:40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jette DU, Halbert J, Iverson C, Miceli E, Shah P. Use of standardized outcome measures in physical therapist practice: perceptions and applications. Phys Ther. 2009; 89(2):125–35 [DOI] [PubMed] [Google Scholar]