Abstract
Purpose
To identify through focus groups of visually impaired children and their parents, relevant content for a vision-targeted health-related quality of life questionnaire designed for children ages 6-12.
Methods
Six focus groups of children with vision impairment ages 6 -12 and six focus groups of their parents were conducted by trained facilitators using a guided script. Sessions were recorded, transcribed and coded per a standardized protocol for content analysis. Comments were placed in thematic categories and each coded as positive, negative or neutral.
Results
Twenty-four children (mean age 9.4 years) with vision impairment from a variety of causes and 23 parents participated. The child focus groups generated 1,163 comments, of which 52% (n=599) were negative, 12% (n=138) were neutral and 37% (n=426) were positive. The three most common topical areas among children were: glasses and adaptive equipment (18%), psychosocial (14%) and school (14%). The parent focus groups generated 1,952 comments of which 46% (n=895) were negative, 16% (n=323) were neutral and 38% (n=734) were positive. The three most common topical areas among parents were: school (21%), expectations or frustrations (14%) and psychosocial (13%).
Conclusions
Pediatric vision impairment has significant effects on health related quality of life, as reported by children with vision impairment and their parents in their own words. These findings will provide the content to guide construction of a survey instrument to assess vision-specific, health-related quality of life in children with vision impairment.
Keywords: low vision, quality of life, congenital nystagmus, albinism, pediatrics
Although children represent a small proportion of visually impaired or blind persons in the United States when compared to the older adult population, they represent a significant public health concern due to the number of life-years affected.1, 2 In 1996 it was estimated that the global financial cost of childhood blindness (defined according to the World Health Organization – best corrected vision of 20/400 or worse) in terms of loss of earning capacity is between US$6 trillion and $27 trillion, surpassing the cost of adult blindness1. Most of this loss occurs in high-income countries like the U.S. where the prevalence is lower, but children live longer and have greater earning capacities. In fact, only cataract ranks higher than childhood blindness on the global burden of eye disease when measured in disability adjusted life years.3 However, the implications of pediatric vision impairment on health-related quality of life (HRQoL) are not well understood.
The National Eye Institute Vision Function Questionnaire (NEI VFQ) is a widely used instrument designed to assess vision-specific HRQoL across a range of chronic eye diseases and low vision in the adult population.4-6 However, many items, for example those about driving or about staying home due to vision, do not apply to children. In addition, some content domains (e.g., school) particularly pertinent to children are not included. Thus, it is not ideally suited for use in children.
Development of HRQoL instruments for children is challenging.7 Developmental issues are probably the most significant when developing or choosing a HRQoL measure for children8 since developmental changes in attention, time perception, language ability, emotional processes and understanding of health and illness occur as a child matures. Children may also place differing levels of importance on areas of concern as they age, for example the visibility of their impairment to others may play different roles as they develop.9 Although an older child (e.g. teenager age ≥ 16 years old) might be able to validly and reliably respond to a HRQoL instrument developed for an adult population10, for the many reasons just discussed, a younger child’s responses on this same questionnaire are likely to be invalid and/or unreliable. Some HRQoL instruments for children developed for non-visual domains, have overcome this challenge with the use of age-specific formats.7
There has been increased interest in measuring HRQoL among children with vision impairment because the patient’s perspective is becoming increasingly important as an outcome measure in clinical trials in ophthalmology.11 Five instruments that assess the impact of visual conditions on children have been reported in the literature, however three of those address only the physical (visual ability) aspects of HRQoL. At a minimum, to assess HRQoL, physical, emotional and social domains should be addressed.7 The LV Prasad Vision Function Questionnaire was designed to assess functional vision problems (e.g. locating a ball, threading a needle) and is more appropriate for use in developing countries.12 This questionnaire does not address domains involving social, emotional or school functioning. The Effect of Youngsters’ Eyesight in Quality of Life instrument (EYE-Q) was developed and used to evaluate the effect of uveitis on visual function in children with juvenile rheumatoid arthritis.13 This instrument also focuses on function, asking questions about the level of difficulty required to complete 13 tasks. The Cardiff Visual Ability Questionnaire for Children14 also focuses on visual function, asking questions only about task difficulty.
Two instruments do address the all three domains of quality of life. The Children’s Vision Function Questionnaire (CVFQ)15 was designed for use in children less than 7 years of age. The content of sixty-one items were developed based on expert opinion and not from structured interviews or focus groups with the target population, namely visually impaired children or their proxies (e.g., parents). The CVFQ has been shown to be valid and reliable16 for its intended population, children < 7 years old. The content of the Impact of Vision Impairment for Children (IVI_C)17 was derived based on interviews and focus groups of parents and teachers of the visually impaired as well as children, however only children > 11 years old participated in their focus groups. The IVI_C has been shown to be psychometrically valid for Australian children ages 8 to 18.18 While both of these instruments (CVFQ and IVI_C) are useful, neither is optimal for those children in the 6 to 8 age range, and neither offers both a parent and child format. Thus, development of a new instrument is needed to fully understand the HRQoL of youngsters in the earliest stages of their formal education.
Our eventual goal is to develop a non condition-specific vision-targeted HRQoL instrument for use with visually impaired children ages 6 through 12 . Multiple forms will be developed, including child age-appropriate versions as well as a parent/guardian version. Such an instrument will be useful in measuring outcomes in studies evaluating rehabilitation approaches in children with low vision. Toward this goal, this study identifies the appropriate content for this instrument through the use of focus group and content methodology.
METHODS
Focus group participants were recruited from the Center for Low Vision Rehabilitation at the University of Alabama at Birmingham (UAB). Potential participants were identified by medical record review of all children seen in the prior 3 years who were ages 6 to 12 years old at the time of the review. Eligibility criteria were: aged 6 to 12 with organic vision impairment, best-corrected visual acuity between 20/40 and 20/800 in the better eye, inclusive, and no documentation of cognitive impairment in the clinical record. An initial letter of introduction to the project was mailed to the parents from their child’s optometrist (DKD). Parents were then contacted by phone to determine interest in participating in focus groups about childhood vision impairment. Interested parent/child pairs were scheduled for participation. Six child focus groups were conducted; 2 groups of children 6 to 7 years old, 2 groups of children 8-9 years old, and 2 groups of children 10-12 years old. There were also six parent focus groups conducted separately from the children’s groups in an adjacent room: at least one parent of each child was placed into a group to parallel the age group assignment of his/her child’s group. The lower age limit of 6 years old for the child’s groups was set since previous work has shown that younger children are typically not able to reliably participate in focus group exercises. 19, 20
This research followed the tenets of the Declaration of Helsinki, and Institutional Review Board approval at UAB was obtained. Written parental consent and child assent were obtained for all participants after the nature and possible consequences of the study were explained and prior to the start of the focus groups. The facilitator for the children’s focus groups was an experienced elementary school teacher with extensive training in conducting focus groups. A trained facilitator also led the parent groups. An assistant was present in each room to operate the audio recorders and help as needed. Two scripts covering the same topics (Table 1) were developed, one for the child groups and one for the parent groups. Questions in the script were open-ended and concluded with a final question offering the participants the opportunity to discuss areas not specifically queried. The content of the scripts are available at http://medicine.uab.edu/eyedoc/79227/.
Table 1.
Content areas for the semi-structured script.
| Domain | Content |
|---|---|
| General vision | Description of vision, comparison to friends, siblings |
| Mobility | Mobility in familiar and unfamiliar environments Use of white cane |
| School functioning | Feelings toward print size, use of large print books Use of assistive devices Reading |
| Social relations and activities | Ride a bike, play a sport Make friends Recognize faces Self-esteem |
| Self-care activities | Ability to dress self, brush teeth, bathe Pour a drink Identify coins |
| Treatment | Medications, surgeries Hopes for future treatments Spectacles |
| Family Impact | Parent worry, fear Time spent on doctors visits or other services Feelings toward discipline Future expectations |
The focus groups took place in late afternoon after the school day ended. For the child focus groups, children were informally introduced over a snack and chatted together prior to the start of the focus groups. Once the focus group discussion began, the facilitator laid the ground rules for participation (e.g. everything they have to say is important, it is okay to talk with each other as well as the facilitator, but one person at a time may speak). In the parent focus groups, after the facilitator laid out the ground rules, the parents were asked to introduce themselves and to share a few words about something they did that was fun recently. Child focus groups lasted 60 minutes or less, while parent groups lasted up to 80 minutes.
Audio recordings from all groups were transcribed word for word by a professional transcriptionist; the participant providing each comment was identified by first name in the transcript. Data were summarized using well-established methods discussed by Holsti21 and used to develop the NEI-VFQ 5, the NEI-RQL, 22 and the Low Luminance Questionnaire 23. During a first-pass reading of the transcript, major themes were identified. The major themes were operationally defined in order to create categories that were both mutually exclusive and exhaustive. Coding rules were written so that comments could only fit into one category. During a second pass of the data, items were categorized as positive (activity can be done adequately, pleasant comments were made or expression of a positive affect), neutral (no affective tone detected, factual statements unrelated to disability) or negative (being limited or having difficulties with activities, or any negative emotion or thought associated with vision). A second experienced coder categorized approximately15% of the comments using the same coding rules as the primary coder. Disagreements between coders were resolved by referring back to the coding guidelines and discussion. Cohen’s κ 24 was calculated for both the child and parent focus groups to assess inter-rater reliability. A κ of 0.60 was predetermined to be acceptable.25
RESULTS
Six focus groups were conducted with children with vision impairment and six focus groups were conducted with their parents. A total of 24 children and 23 parents participated. Group sizes ranged from 3 to 6 persons. Participants were 91.5% white and 8.5% African American. The average age of the children was 9.4 ± 1.96 years. The majority of participating parents were female (82.6%) while the majority of child participants were male (62.5%). There were a wide variety of diagnoses for the children’s vision impairment as well as a range of best-corrected visual acuity (Table 2). Inter-rater agreement in coding the transcripts was excellent (κ=0.87 for child focus groups and κ= 0.79 for parent focus groups).
Table 2.
Ocular diagnosis and visual acuity of participants in child focus groups.
| Age | Primary Ocular Diagnosis | Nystagmus | Best Corrected VA OD |
Best Corrected VA OS |
|---|---|---|---|---|
| 6 years, 4 months | Rod Cone Dystrophy | present | 20/80 | 20/64 |
| 6 years, 7 months | Optic Nerve Hypoplasia | present | 20/80 | 20/252 |
| 6 years, 9 months | Optic Nerve Hypoplasia | present | NLP | 20/60 |
| 7 years, 2 months | Congenital Nystagmus | present | 20/80 | 20/80 |
| 7 years, 4 months | Oculocutaneous Albinism | present | 20/277 | 20/277 |
| 8 years, 5 months | Congenital Nystagmus | present | 20/80 | 20/80 |
| 8 years, 1 month | Congenital Nystagmus | present | 20/80 | 20/60 |
| 8 years, 10 months | Oculocutaneous Albinism | present | 20/303 | 20/241 |
| 8 years, 10 months | Optic atropy | absent | 20/200 | 20/200 |
| 8 years, 3 months | Achromatopsia | present | 20/200 | 20/200 |
| 8 years, 7 months | Oculocutaneous Albinism | present | 20/200 | 20/200 |
| 8 years, 7 months | Oculocutaneous Albinism | present | 20/200 | 20/200 |
| 9 years, 11 months | Congenital Nystagmus | present | 20/150 | 20/100 |
| 9 years, 2 months | Retinitis Pigmentosa | absent | 20/80 | 20/80 |
| 9 years, 3 months | Cone Rod Dystrophy | absent | 20/160 | 20/160 |
| 9 years, 3 months | Retinopathy of Prematurity | present | 20/400 | 20/400 |
| 11 years, 1 month | Dominant Optic Atrophy | absent | 20/150 | 20/150 |
| 11 years, 2 months | Optic Nerve Hypoplasia | present | 20/100 | 20/80 |
| 11 years, 8 months | Aniridia | present | 20/200 | 20/200 |
| 12 years | Congenital Nystagmus | present | 20/200 | 20/200 |
| 12 years | Oculocutaneous Albinism | present | 20/200 | 20/400 |
| 12 years, 1 month | Achromatopsia | present | 20/100 | 20/80 |
| 12 years, 3 months | Congenital Nystagmus | present | 20/40 | 20/50 |
| 12 years, 4 months | Retinitis Pigmentosa | absent | 20/200 | 20/70 |
VA OD = visual acuity right eye
VA OS = visual acuity left eye
Child Focus Groups
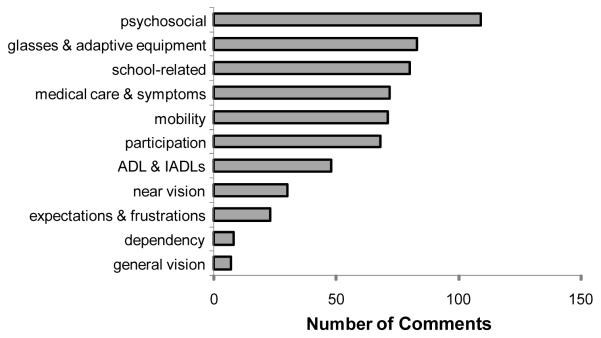
Overall, the child focus groups generated 1,163 comments, of which 52% (n=599) were negative, 12% (n=138) were neutral and 37% (n=426) were positive (Figure 1). Frequency distribution of the comments can be found in Table 3, while ranking of the negative (problem) comments by category can be seen in Figure 2.
Figure 1.
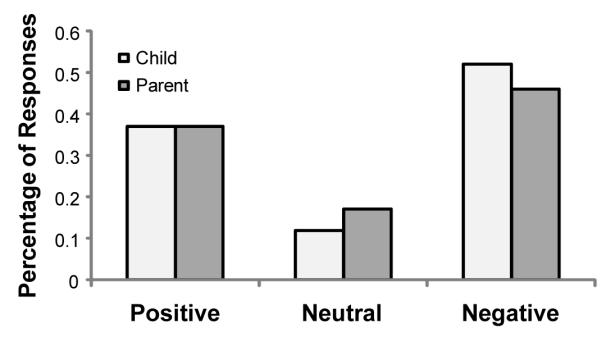
Percentage of positive, neutral and negative comments made during child (grey bars) and parent (black bars) focus groups.
Table 3.
Frequency of negative (problem), neutral and positive comments within each content category.
| Content Category (listed alphabetically) |
Child Focus Groups | Parent Focus Groups | ||||||
|---|---|---|---|---|---|---|---|---|
|
| ||||||||
| Negative | Neutral | Positive | Total | Negative | Neutral | Positive | Total | |
| ADL & IADLs | 48 | 8 | 30 | 86 | 28 | 11 | 20 | 59 |
| Dependency | 8 | 6 | 10 | 24 | 9 | 1 | 12 | 22 |
| Expectations & Frustrations | 23 | 11 | 24 | 58 | 145 | 35 | 96 | 276 |
| General Vision | 7 | 27 | 32 | 66 | 96 | 37 | 65 | 198 |
| Glasses & Adaptive Equipment | 83 | 37 | 94 | 214 | 70 | 52 | 105 | 227 |
| Medical Care & Symptoms | 72 | 22 | 19 | 113 | 94 | 64 | 44 | 202 |
| Mobility | 71 | 0 | 56 | 127 | 69 | 5 | 88 | 162 |
| Near Vision | 30 | 2 | 15 | 47 | 16 | 3 | 7 | 26 |
| Participation | 68 | 4 | 29 | 101 | 56 | 21 | 32 | 109 |
| Psychosocial | 109 | 4 | 53 | 166 | 118 | 21 | 122 | 261 |
| School-Related | 80 | 17 | 64 | 161 | 194 | 73 | 143 | 410 |
ADL & IADLs = activities of daily living and instrumental activities of daily living.
Figure 2.
Distribution of negative (problem) comments from child focus groups.
Glasses and adaptive equipment were the most frequently discussed topics during the child focus groups, ranking first in frequency for positive comments and second for negative comments. Typical positive comments from the children’s focus groups included: “I got this thing called an easel, it’s helpin’ me a lot” or “When I’m usin’ the CCTV I get really relaxed and kind a like usin’ it. It’s really fun”. Typical negative comments pertained to glasses and included: “I wanna get contacts because the nose part hurts and you have to keep up with them” or “I hate wearing glasses”.
Psychosocial comments were the second most frequent during the child focus groups and had the highest percentage of negative comments (66%). These negative comments accounted for almost one fifth (18.2%) of all negative comments mentioned. Examples from the child focus groups include: “It’s kind of weird when people look at my eyes. They’re like what’s wrong with your eyes, stop doin’ that, and I can’t because I have albinism”, “everybody makes fun of me” and “when I make friends I don’t tell them I have bad vision until the middle of the year”.
School-related topics ranked third overall in the child focus groups. Comments were nearly evenly split between negative and positive/neutral comments. Examples of negative comments include: “I can tell that I can’t see things because people at my class can just open a book, a chapter book and read it and I have, I can’t see the words when I try to do that” and “I couldn’t see the words so I couldn’t practice with my class and it was really hard.” Positive comments included statements like “she does my textbook because my textbook is biggest and everyone can see it and it’s really neat how um I get to use these big textbooks” and “sometimes he [the teacher] helps me by telling, saying what he wrote or sometimes he will write it bigger so I can read it.”
The top three areas with respect to frequency accounted for 47% of all comments among the children. The remaining areas, from most common to least common were: mobility, medical care and associated symptoms, participation, activities of daily living, general vision, expectations and frustrations, near vision and dependency. Comments about general vision had by far the lowest proportion of negative comments (10.6%) while participation in social and recreational or sporting activities had the greatest proportion of negative comments (67%).
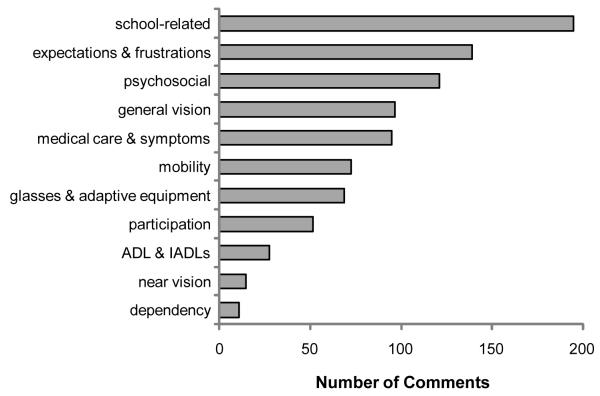
Parent Focus Groups
Parent focus groups generated 1,952 comments of which 45.9% (n=895) were negative, 16.6% (n=323) were neutral and 37.6% (n=734) were positive (Figure 1). Frequency distribution of the comments can be found in Table 3, while ranking of the negative (problem) comments by category can be seen in Figure 3.
Figure 3.
Distribution of negative (problem) comments from parent focus groups.
School-related comments ranked first in frequency among parent focus groups, accounting for 21.1% of all comments. Roughly half (47.3%) were negative. Typical negative statements included: “we had a second grade teacher that told us that she was wasting her time teaching my child because he was visually impaired “ or “if they are writing on the board, if they use a yellow marker, there’s not enough contrast. He struggles with that.” Whereas positive comments often related to accommodations: “This year, he does all his work independent, it’s amazing. And the differences are they are giving him enlarged things, he’s using a scanner, read software and just things like that that are working for him” or “They have enlarged anything and they have done anything that I’ve asked them to do.”
The second most common topic was expectations and frustrations. The comments were almost evenly split between negative and positive/neutral. Frustrations typically centered around a lack of a cure for their ocular condition, such as: “I wish they could transplant new nerves cause see that’s our child’s problem mainly is the nerves are dead” or “His is, it gets progressively worse so you know I have to stress every, you know, is it going to be worse this year?” Positive comments centered around hope: “My family has always hoped for a cure. Um, we, we believe in prayer and that’s one of the, the big things that gets us through” and “it always amazes me that everywhere I go, I find out something new that will help my son.”
Psychosocial comments were the third most common type. In the parent groups they were approximately evenly split between positive and negative comments. Positive comments often mentioned siblings or close friends being helpful: “He was in kindergarten through the fifth grade with his same group and there were a lot of his friends that realized his vision problem and knew what it was and they helped him accommodate” or “My oldest is very good with (child’s name) as far as vision. I mean, he always wants, every time we’re anywhere, he wants to make sure that (child’s name) can see.” Negative comments were most frequently about other children teasing their child. For example: “they’ll say stuff like what’s wrong, retard, can’t you catch the ball, you know cause he just can’t see it and a lot of the kids don’t even realize he has a visual problem so, you know” or “we’ve had a lot of teasing because of her eyes, the nystagmus, and our girls have pure white hair so they are just extremely different and so yeah, that’s been a real struggle.”
The top three areas with respect to frequency accounted for 48.5% of all comments among the parents. The remaining areas, from most common to least common were: glasses and adaptive equipment, medical care and associated symptoms, general vision, mobility, participation, activities of daily living, dependency and near vision. Near vision had the highest percentage of negative comments (68%) and glasses and adaptive equipment had the least (31%).
DISCUSSION
The focus group process identified the relevant content areas for development of a vision-targeted questionnaire on pediatric HRQoL. Although focus groups have been conducted for older children with vision impairment (ages 11-18)17 this work represents the first focus groups of younger (ages 6 to 12) children with vision impairment. It is also the first time that parent/child dyads have participated in this type of research. Proxy reporting of quality of life has been shown to have serious limitations. One meta-analytic study looked at 119 studies for the consistency between informant reports on behavioral and emotional problems in pediatric subjects. The correlation between informants playing similar roles (e.g. pairs of parents or pairs of teachers) was 0.60, whereas the correlation between different types of informants (e.g. parent and teacher) was only 0.28. However, children’s self-report had the lowest correlation (0.22) with those of informants.26 There are many explanations for this discordance including lack of knowledge on the informant’s part, the relationship between child and informant, denial, provision of socially desirable answers and the informants own biases and personal problems.27 By obtaining both the parent and child perspectives from members of the same family, we gained a broader understanding of the perspectives of these two groups on the same topics. Additionally, since we plan to develop both parent proxy and child report formats for this new questionnaire, this work has generated much information about parents and children discuss these topics in their own words.
School is an important aspect of life for all children, so it is not surprising that much of the discussion centered on school. The comments were nearly evenly split between negative and positive/neutral. This may in large part be due to there being considerable disparity in educational services received by the children participating in our study. In the geographic area where our study was based, fewer services are available for children attending schools in more rural areas, as compared to urban and suburban areas. Parents and children receiving more assistance in terms of specialized teaching and/or adaptive equipment in the school setting were more likely to make positive comments. Our analysis revealed that school-related issues will be an important domain to include in a vision-targeted HRQoL instrument for visually impaired children since it is such an integral part of a child’s life. Given the long-term implications of education on employment and the link between employment and quality of life, education (school) is an essential domain for a HRQoL instrument for visually impaired children. Previous research has shown that only about 25% of people ≥ 16 years old with vision loss were in the workforce in 2010.28 Understanding the vision-targeted quality of life issues related to education may enable strategies to be developed to increase employability.
With regard to psychosocial comments, children frequently noted that they were excluded or picked on by peers due to their appearance (e.g., glasses, nystagmus, hypopigmentation). Children’s negative comments on psychosocial issues were 2-fold more common than that of their positive comments. However, interestingly parents comments were evenly split between positive and negative, perhaps suggesting that the personal emotional burden of vision impairment expressed by visually impaired children may be more prominent in their everyday life than parents believe or are able to discuss in a group setting. Many children reported episodes of being a victim of verbal bullying and often expressed feelings of helplessness; a few reported episodes or fear of physical bullying. There have been no published studies concerning bullying of children with vision impairment, however, studies have shown that children with other disabilities are targets for bullying.29, 30 While parents in our groups noted that their child may be teased or left out because of their vision, they also reported that having a good peer support network is critical, and that friends and siblings were typically accommodating. These comments provide guidance for development of questions to further explore this important area.
None of the available vision-targeted pediatric HRQoL questionnaires delve into physical symptoms, associated with vision impairment. Our focus groups show that this area is of significant concern to both parents and children. Positive comments in this domain typically represented an appreciation for the eye care they received as well as acknowledgement that the burden of receiving the care was low (most reported only 2-3 eye doctor visits per year). However, medical care and condition-associated symptoms ranked 4th and 5th in terms of the number of negative comments generated in the child and parent focus groups, respectively. Visual fatigue and reading-associated headaches severe enough to limit productivity were the source of many negative comments. While practitioners specializing in providing low vision care commonly hear these complaints, they are not reported as symptoms of eye conditions causing pediatric vision impairment in the literature. Such symptoms, when present, would clearly have a negative impact on HRQoL and merit further exploration.
Although children and parents reported some instrumental activity of daily living difficulties, it is difficult to determine whether these reflect typical childhood difficulties (e.g., pouring liquid), or have greater significance in visually impaired children. This emphasizes the importance of age-appropriate surveys. One version of the survey is not likely to be able to encompass the entire age range studied in our focus groups. One well-studied generic pediatric quality of life instrument31 utilizes 3 age-specific child self-report forms (ages 5-7, 8-12, 13-18) and 4 age-specific parent proxy forms (ages 2-4, 5-7, 8-12, 13-18). Development of questions covering this domain will likely require age-specific topic areas.
A significant strength of this research is that it examined the perspective of children ages 6 to 12 years old with vision impairment in a focus group setting where they could express their perspectives in their own words. Our data represents the youngest sample of children with vision impairment studied using focus groups. These results confirm those of Ronen32 that showed that children as young as 6 years of age can meaningfully participate in focus groups. An additional strength is that we examined both parent and child perspectives using parent-child dyads rather than unrelated pairs. Given that there are limitations with parent proxy responses, having the perspective of the dyad will enable us to generate questions that reflect both perspectives. A limitation is that we used a convenience sample for our participants, and as such they may not be representative of all children with vision impairment; however this is a common approach in focus group studies on vision impairment and eye disease. 4, 23, 33 None of the children in our study had profound vision impairment. However, the vast majority of children with vision impairment have visual acuity in the range we studied. In a prior study, we found that 70.5% of children enrolled in a school for the blind and visually impaired had visual acuity of 20/400 or better.34
These focus groups achieved our primary objective of providing rich information for developing a child self-report and parent proxy-report questionnaire regarding the impact of pediatric vision impairment on quality of life. There was a wide distribution of responses across the categories. Splitting the responses into positive/negative or neutral categories provided information about the types of comments and will help to frame questions and appropriate response categories in the item generation phase of questionnaire development. No category was overwhelmingly positive or negative suggesting that the development of appropriate response scales will be critically important in the development of a vision-targeted HRQoL instrument for children. This study lays the content groundwork for the development of items and response scales for a vision-targeted HRQoL for visually impaired children, which will then be evaluated and refined so that it is appropriate for use in intervention evaluation studies for children with low vision.
ACKNOWLEDGEMENTS
National Institutes of Health Grants K23EY018864 and R21EY16801; EyeSight Foundation of Alabama; Research to Prevent Blindness; Able Trust.
Footnotes
The authors declare no conflicts of interest.
This work was presented in part (parent focus groups only) as a poster at the ARVO Annual Meeting in Fort Lauderdale, 2011. Both the parent and child focus groups were presented as a poster at the American Academy of Optometry Annual Meeting in Boston, MA, November 2011.
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Rahi JS, Gilbert CE, Foster A, Minassian D. Measuring the burden of childhood blindness. Br J Ophthalmol. 1999;83:387–8. doi: 10.1136/bjo.83.4.387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Adams PF, Hendershot GE, Marano MA. Current estimates from the National Health Interview Survey, 1996. Vital Health Stat. 1999;10:1–203. [PubMed] [Google Scholar]
- 3.Gilbert C, Foster A. Childhood blindness in the context of VISION 2020--the right to sight. Bull World Health Organ. 2001;79:227–32. [PMC free article] [PubMed] [Google Scholar]
- 4.Mangione CM, Berry S, Spritzer K, Janz NK, Klein R, Owsley C, Lee PP. Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire: results from focus groups with visually impaired persons. Arch Ophthalmol. 1998;116:227–33. doi: 10.1001/archopht.116.2.227. [DOI] [PubMed] [Google Scholar]
- 5.Mangione CM, Lee PP, Pitts J, Gutierrez P, Berry S, Hays RD. Psychometric properties of the National Eye Institute Visual Function Questionnaire (NEI-VFQ). NEI-VFQ Field Test Investigators. Arch Ophthalmol. 1998;116:1496–504. doi: 10.1001/archopht.116.11.1496. [DOI] [PubMed] [Google Scholar]
- 6.Mangione CM, Lee PP, Gutierrez PR, Spritzer K, Berry S, Hays RD. Development of the 25-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 2001;119:1050–8. doi: 10.1001/archopht.119.7.1050. [DOI] [PubMed] [Google Scholar]
- 7.Koot HM. The study of quality of life: concepts and methods. In: Koot HM, Wallander JL, editors. Quality of Life in Child and Adolescent Illness: Concepts, Methods, and Findings. Brunner-Routledge; New York: 2001. pp. 3–22. [Google Scholar]
- 8.Eiser C. Growing Up with a Chronic Disease: the Impact on Children and Their Families. Jessica Kingsley Publishers; London: 1993. [Google Scholar]
- 9.French DJ, Christie MJ, Sowden AJ. The reproducibility of the Childhood Asthma Questionnaires: measures of quality of life for children with asthma aged 4-16 years. Qual Life Res. 1994;3:215–24. doi: 10.1007/BF00435387. [DOI] [PubMed] [Google Scholar]
- 10.Juniper EF, Guyatt GH, Feeny DH, Griffith LE, Ferrie PJ. Minimum skills required by children to complete health-related quality of life instruments for asthma: comparison of measurement properties. Eur Respir J. 1997;10:2285–94. doi: 10.1183/09031936.97.10102285. [DOI] [PubMed] [Google Scholar]
- 11.Mangione C, Lee PP, Hays RD. Measurement of visual functioning and health-related quality of life in eye disease and cataract surgery. In: Spiker B, editor. Quality of Life and Pharmacoeconomics in Clinical Trials. 2nd ed Lippincott-Raven; Philadelphia: 1996. pp. 1045–51. [Google Scholar]
- 12.Gothwal VK, Lovie-Kitchin JE, Nutheti R. The development of the LV Prasad-Functional Vision Questionnaire: a measure of functional vision performance of visually impaired children. Invest Ophthalmol Vis Sci. 2003;44:4131–9. doi: 10.1167/iovs.02-1238. [DOI] [PubMed] [Google Scholar]
- 13.Angeles-Han ST, Griffin KW, Lehman TJ, Rutledge JR, Lyman S, Nguyen JT, Harrison MJ. The importance of visual function in the quality of life of children with uveitis. J Aapos. 2010;14:163–8. doi: 10.1016/j.jaapos.2009.12.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Khadka J, Ryan B, Margrain TH, Court H, Woodhouse JM. Development of the 25-item Cardiff Visual Ability Questionnaire for Children (CVAQC) Br J Ophthalmol. 2010;94:730–5. doi: 10.1136/bjo.2009.171181. [DOI] [PubMed] [Google Scholar]
- 15.Felius J, Stager DR, Sr., Berry PM, Fawcett SL, Stager DR, Jr., Salomao SR, Berezovsky A, Birch EE. Development of an instrument to assess vision-related quality of life in young children. Am J Ophthalmol. 2004;138:362–72. doi: 10.1016/j.ajo.2004.05.010. [DOI] [PubMed] [Google Scholar]
- 16.Birch EE, Cheng CS, Felius J. Validity and reliability of the Children’s Visual Function Questionnaire (CVFQ) J Aapos. 2007;11:473–9. doi: 10.1016/j.jaapos.2007.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cochrane G, Lamoureux E, Keeffe J. Defining the content for a new quality of life questionnaire for students with low vision (the Impact of Vision Impairment on Children: IVI_C) Ophthalmic Epidemiol. 2008;15:114–20. doi: 10.1080/09286580701772029. [DOI] [PubMed] [Google Scholar]
- 18.Cochrane GM, Marella M, Keeffe JE, Lamoureux EL. The Impact of Vision Impairment for Children (IVI_C): validation of a vision-specific pediatric quality-of-life questionnaire using Rasch analysis. Invest Ophthalmol Vis Sci. 2011;52:1632–40. doi: 10.1167/iovs.10-6079. [DOI] [PubMed] [Google Scholar]
- 19.Ronen GM, Rosenbaum P, Law M, Streiner DL. Health-related quality of life in childhood disorders: a modified focus group technique to involve children. Qual Life Res. 2001;10:71–9. doi: 10.1023/a:1016659917227. [DOI] [PubMed] [Google Scholar]
- 20.Peterson-Sweeney K. The use of focus groups in pediatric and adolescent research. J Pediatr Health Care. 2005;19:104–10. doi: 10.1016/j.pedhc.2004.08.006. [DOI] [PubMed] [Google Scholar]
- 21.Holsti OR. Content Analysis for the Social Sciences and Humanities. Addison-Wesley Pub. Co.; Reading, MA: 1969. [Google Scholar]
- 22.Hays RD, Mangione CM, Ellwein L, Lindblad AS, Spritzer KL, McDonnell PJ. Psychometric properties of the National Eye Institute-Refractive Error Quality of Life instrument. Ophthalmology. 2003;110:2292–301. doi: 10.1016/j.ophtha.2002.07.001. [DOI] [PubMed] [Google Scholar]
- 23.Owsley C, McGwin G, Jr., Scilley K, Kallies K. Development of a questionnaire to assess vision problems under low luminance in age-related maculopathy. Invest Ophthalmol Vis Sci. 2006;47:528–35. doi: 10.1167/iovs.05-1222. [DOI] [PubMed] [Google Scholar]
- 24.Cohen J. A coefficient of agreement for nominal scales. Educ Psychol Meas. 1960;20:37–46. [Google Scholar]
- 25.Barlow DH, Hersen M. Single Case Experimental Designs: Strategies for Studying Behavior Change. 2nd ed Pergamon Press; New York: 1984. [Google Scholar]
- 26.Achenbach TM, McConaughy SH, Howell CT. Child/adolescent behavioral and emotional problems: implications of cross-informant correlations for situational specificity. Psychol Bull. 1987;101:213–32. [PubMed] [Google Scholar]
- 27.Wallander JL, Schmitt M, Koot HM. Quality of life measurement in children and adolescents: issues, instruments, and applications. J Clin Psychol. 2001;57:571–85. doi: 10.1002/jclp.1029. [DOI] [PubMed] [Google Scholar]
- 28.American Federation for the Blind [Accessed: April 3, 2012];Interpreting Bureau of Labor Statitics Employment Data. 2010 [updated January 2012]. Available at: www.afb.org/Section.asp?SectionID=15&SubTopicID=177.
- 29.Flint SW, Morton RC. Bullying and children with disabilities. J Instruct Psychol. 2004;31:330–3. [Google Scholar]
- 30.Norwich B, Kelly N. Pupils’ views on inclusion: moderate learning difficulties and bullying in mainstream and special schools. Br Educ Res J. 2004;30:43–65. doi: 10.1348/0007099041552297. [DOI] [PubMed] [Google Scholar]
- 31.Varni JW, Seid M, Kurtin PS. PedsQL 4.0: reliability and validity of the Pediatric Quality of Life Inventory version 4.0 generic core scales in healthy and patient populations. Med Care. 2001;39:800–12. doi: 10.1097/00005650-200108000-00006. [DOI] [PubMed] [Google Scholar]
- 32.Ronen GM, Rosenbaum P, Law M, Streiner DL. Health-related quality of life in childhood disorders: a modified focus group technique to involve children. Qual Life Res. 2001;10:71–9. doi: 10.1023/a:1016659917227. [DOI] [PubMed] [Google Scholar]
- 33.Owsley C, McGwin G, Scilley K, Girkin CA, Phillips JM, Searcey K. Perceived barriers to care and attitudes about vision and eye care: focus groups with older African Americans and eye care providers. Invest Ophthalmol Vis Sci. 2006;47:2797–802. doi: 10.1167/iovs.06-0107. [DOI] [PubMed] [Google Scholar]
- 34.DeCarlo DK, Nowakowski R. Causes of visual impairment among students at the Alabama School for the Blind. J Am Optom Assoc. 1999;70:647–52. [PubMed] [Google Scholar]