Abstract
Posttraumatic stress disorder (PTSD) commonly co-occurs with alcohol dependence (AD) and negatively affects treatment outcomes. Trauma-related negative affect enhances substance craving in laboratory cue-reactivity studies of AD individuals, but the role of positive affect has not been established. In this study, 108 AD treatment-seeking adults with current PTSD and AD were presented with four counterbalanced trials consisting of an audio cue (personalized trauma or neutral script) followed by a beverage cue (alcohol or water). Results revealed alcohol cues increased positive and negative affect, and positive affective responses explained significant incremental variance in self-reported craving and salivation, but only when cues were accompanied by neutral not trauma imagery. Ambivalent (high negative and positive) responses were associated with strongest craving. Findings advance the conceptualization of craving in individuals with PTSD-AD and highlight the importance of independently assessing positive and negative affective responses to cues in individuals with co-occurring PTSD-AD.
Keywords: PTSD, alcohol abuse, craving, approach-avoidance, cue reactivity, salivation
Researchers, clinicians, and policy makers have been increasingly attentive to the issue of posttraumatic stress disorder (PTSD) and substance use disorder (SUD) comorbidity. Between 20% and 40% of individuals seeking treatment for alcohol and drug use disorders meet current diagnostic criteria for PTSD (e.g., Dansky, Roitzsch, Brady, & Saladin, 1997; Reynolds et al., 2005). Lifetime prevalence rates of PTSD in this population range from 30% to 52% (Back et al., 2000; Reynolds et al., 2005). Alcohol and drug users with PTSD present a more complicated clinical picture and experience poorer treatment outcomes, such that individuals with PTSD improve less in SUD treatment programs, relapse more quickly on discharge, and experience additional difficulties compared with individuals with SUD alone (e.g., poorer occupational functioning, poorer physical health and greater likelihood of overdose; Brown, Stout, & Mueller, 1999; Norman, Tate, Anderson, & Brown, 2007; Ouimette, Finney, & Moos, 1999; Read, Brown, & Kahler, 2004).
PTSD is characterized by experiences of heightened negative affect, as well as constant efforts to manage and/or avoid such states (e.g., Beckham et al., 2000). At least two theoretical models suggest that negative affect plays a pivotal role in the maintenance of PTSD-SUD comorbidity (see Stewart & Conrod, 2003, for review). The self-medication hypothesis proposes that individuals with PTSD drink to relieve distress evoked by traumatic memories (Khantzian, 1997). The mutual maintenance hypothesis, a bidirectional model, suggests that substance use may also interfere with natural resolution of trauma-related distress, and that PTSD symptoms may negatively affect substance use symptoms (Brown, Stout, & Gannon-Rowley, 1998). Consistent with these models, alcohol-dependent individuals report increased alcohol craving in response to stress cues and negative mood induction paradigms (e.g., Fox, Bergquist, Hong, & Sinha, 2007; Rubonis et al., 1994). Similarly, individuals with comorbid PTSD and alcohol dependence (AD) evidence increased self-reported alcohol craving and salivary responding in response to trauma cues, even when no alcohol cue is present (e.g., Coffey et al., 2010), with these responses being dampened after distress elicited by traumatic memories is reduced through repeated exposure to the traumatic memory (Coffey, Stasiewicz, Hughes, & Brimo, 2006). Conversely, exposure to alcohol and drug cues has also been shown to increase negative affect in cuereactivity paradigms. For example, among recently abstinent alcohol-dependent individuals, alcohol cue-elicited craving is related to increases in subjective and physiological anxiety and fear (Fox et al., 2007). Individuals with AD also tend to report increased guilt on exposure to alcohol-related cues (Cooney, Gillespie, Baker, & Kaplan, 1987). Thus, trauma-related negative affect induces craving among SUD individuals, and exposure to drug and alcohol cues in turn exacerbates negative affect.
Although cue-reactivity paradigms have predominantly focused on negative affect, positive affect may also be important to consider. Researchers are moving toward a multidimensional conceptualization of craving that includes alcohol approach and avoidance motivations (Anton, 1999; Breiner, Stritzke, & Lang, 1999; McEvoy, Stritzke, French, Lang, & Ketterman, 2004; Stritzke, Breiner, Curtin, & Lang, 2004; Stritzke, McEvoy, Wheat, Dyer, & French, 2007). From this perspective, anticipated positive (e.g., pleasure, stress relief) and negative (e.g., hangover, interpersonal difficulties) consequences simultaneously attract and deter an individual from drinking (Breiner et al., 1999). Cognitive models of cravings suggest that individuals in treatment for SUD are particularly vulnerable to what are termed abstinence promotion cravings, which are characterized by ambivalence about use (Tiffany, 1990). Essentially, when a SUD individual is confronted by a cue (e.g., beer in the grocery store) he or she experiences conflicting approach (e.g., positive outcome expectancies) and avoidance (e.g., desire to remain sober) impulses that are subjectively experienced as craving (Stritzke et al., 2007; Tiffany, 1990). The ambivalence model (e.g., Breiner et al., 1999) predicts urges to drink to be strongest when positive responses to alcohol are high and negative responses are low (i.e., pure approach motives). Cravings are theoretically weaker when negative responses are high and positive responses are low (i.e., pure avoidance) and when positive and negative responses are low (i.e., indifference). Ambivalence, characterized by strong positive and negative responses, is theorized to be a middle ground between these poles. These models emphasize the importance of examining multidimensional, orthogonal responses to drug and alcohol cues. Despite this, the role of positive affect in craving has not been well established using cue-reactivity paradigms. Fox and colleagues (2007) found that alcohol-dependent individuals reacted to alcohol cue-elicited craving with decreases in positive affect. However, related literature suggests that positive affect, as well as positive outcome expectancies, correspond with increased levels of craving (Johnson & Fromme, 1994; Litt, Cooney, & Morse, 2000). Consistent with this, positive affective stimuli increase alcohol craving in non-treatment-seeking alcoholics (Mason, Light, Escher, & Drobes, 2008). Furthermore, increases in self-reported positive affect following alcohol cue exposure also have been demonstrated among regular, nonabstinent social drinkers (Kambouropoulos & Rock, 2010; Kambouropoulos & Staiger, 2004). The results of these few studies notwithstanding, no studies to our knowledge have investigated the impact of alcohol cue presentation on positive affect among PTSD-SUD individuals. Given the complexity of these individuals’ drinking patterns and motivations, research examining the effects of alcohol cues on positive affect among SUD individuals with PTSD may help advance our conceptualization of craving and decision making about drinking in this population. Examining affective responses in the context of alcohol and trauma cues will be particularly important in this respect.
The relationship between affective ambivalence and craving also requires further study. Ambivalence models of cravings focus on conflicting approach and avoidance inclinations. Affective responses to cues are not directly addressed by these models, but they may influence and/or reflect these motivational dispositions. Indeed, affective ambivalence has been examined in the context of several facets of desire and desire-related behavior (e.g., chocolate consumption, sexual arousal; Hormes & Rozin, 2011; Peterson & Janssen, 2007). Simultaneous positive and negative affective responses to cues have received inadequate attention in alcohol craving research, however, and no studies have examined how these affective responses relate to the ambivalence model. Extension of this model to affect suggests that positive and negative affective responses to cues should be associated with variations in alcohol craving.
Present Study
Ultimately, understanding affective responses to alcohol and trauma cues will be critical to advancing our conceptualization of co-occurring PTSD and AD. Thus, the first aim of the current study was to examine affective responses to alcohol and trauma cues in treatment-seeking individuals with concurrent PTSD and AD. Toward this aim, alcohol-dependent substance abuse treatment seekers with PTSD were presented with alcohol or water in vivo cues, combined with personalized trauma and neutral imagery cues. Alcohol craving, along with positive and negative affect, was measured in response to each cue combination. It was hypothesized that (a) the combined trauma script-alcohol cue would correspond with the highest levels of alcohol craving and negative affect compared with the other cue combinations and (b) alcohol cues would elicit higher levels of positive affect compared with the neutral (i.e., water) cue combinations.
The second aim was to examine the relationship between cue-elicited affect and alcohol craving. PTSD-related negative affect is known to be a strong predictor of SUD craving. However, recent models of cravings highlight the importance of examining multidimensional, orthogonal responses to cues. As such, craving may be better understood as a function of positive and negative affect. Accordingly, we hypothesized that increases in positive affect would be related to increases in craving, above and beyond variance accounted for by increases in negative affect.
The final aim of the current study was to examine cue-elicited alcohol craving as a function of response types defined by the ambivalence model of craving. This model implies that urges to drink occur in a multidimensional space, with stronger urges occurring in the context of either pure approach (i.e., high positive, low negative) or ambivalent (i.e., high positive, high negative) responses. Extending this model to affective responses, we examined how patterns in affective responsivity related to cue-elicited craving. Participants’ affective reactions to cues were classified as “positive” (high positive/low negative), “negative” (low positive/high negative), “ambivalent” (high positive/high negative), or “indifferent” (low positive/low negative). It was hypothesized that cue-elicited cravings would be strongest among “positive” and “ambivalent” affective responders.
Method
Participants
Participants were 108 adults (50 women) meeting Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV; American Psychiatric Association, 1994) criteria for current AD and PTSD who were recruited from a community residential chemical dependency treatment facility as a part of a larger, ongoing study. Participants were required to report at least one heavy drinking day in the past 60 days. To eliminate acute effects of intoxication or withdrawal, participants were also required to be alcohol and drug free for at least 4 days immediately preceding the cue-reactivity assessment. Exclusion criteria included meeting diagnostic criteria for a psychotic disorder, currently experiencing a manic episode, or current use of benzodiazapines or other medications that could interfere with cue-elicited craving or salivation (e.g., naltrexone, tricyclic antidepressants, anticholinergic medication; see Table 1 for demographics).
Table 1.
Mean (SD) Participant and Trauma Characteristics (N = 108)
| Age | 33.77 (10.24) |
| Gender | |
| Female | 46% |
| Race | |
| White | 81% |
| Black/African American | 18% |
| Other | 2% |
| Education | |
| ≤12th | 13% |
| High school diploma | 29% |
| Post high school | 43% |
| ≥4-year degree | 16% |
| Employmenta | |
| Full-time | 22% |
| Part-time | 8% |
| Unemployed | 48% |
| Homemaker | 6% |
| Student | 7% |
| Retired | 1% |
| Current co-occurring drug use disorders | |
| Cocaine use disorder | 50% |
| Amphetamine use disorder | 25% |
| Marijuana use disorder | 33% |
| Sedative use disorder | 37% |
| Opiate use disorder | 43% |
| Hallucinogen use disorder | 3% |
| Any co-occurring drug use disorder | 80% |
| Current comorbid psychiatric conditions | |
| Mood disorder | 80% |
| Other anxiety disorder | 74% |
| Anorexia or Bulimia Nervosa | 4% |
| Clinician-Administered PTSD Scale total score | 79.20 (17.57) |
| Impact of Event Scale–Revised total score | 51.47 (15.08) |
| Alcohol Dependence Scale | 25.64 (9.55) |
| Days since last drink of alcohol | 18.06 (11.79) |
Note: PTSD = posttraumatic stress disorder.
Employment status prior to entering treatment.
Measures
Screening
The PTSD Checklist (PCL; Weathers, Litz, Herman, Huska, & Keane, 1993), a reliable, valid, and widely used PTSD screening tool (e.g., Blanchard, Jones-Alexander, Buckley, & Forneris, 1996), and the Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente, & Grant, 1993), a 10-item self-report screening measure for alcohol problems that was developed by the World Health Organization, were used to screen prospective participants. Individuals whose scores were ≥44 on the PCL (Blanchard et al., 1996) and ≥8 on the AUDIT (Babor, de la Fuente, Saunders, & Grant, 1992) were scheduled for a comprehensive assessment.
Diagnosis
The Computerized Diagnostic Interview Schedule (C-DIS; Robins et al., 2000) was used to diagnose SUDs. The C-DIS is a computerized version of the Diagnostic Interview Schedule (DIS), which is a structured clinical interview for the assessment of DSM-IV Axis I disorders. It has demonstrated sound psychometric properties in the diagnosis of substance abuse and dependence (e.g., Vandiver & Sher, 1991).
The National Women’s Study (NWS) PTSD Module (Resnick, 1996), as adapted by Dansky, Bryne, and Brady (1999), was used to establish PTSD Criterion A events. The NWS-PTSD module is a structured interview based on the DIS. This module has been frequently used with populations consisting of men and women (e.g., Coffey et al., 2006; Saladin et al., 2003) and has demonstrated good reliability and concurrent validity (Resnick, Kilpatrick, Dansky, Saunders, & Best, 1993).
The Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995) is a structured clinical interview that was used in the current study to diagnose current (past month) PTSD symptoms for all Criterion A events combined. The CAPS is considered the “gold standard” for PTSD assessment (Weathers, Keane, & Davidson, 2001).
The Mini-International Neuropsychiatric Interview (MINI; Sheehan et al., 1998), a commonly used structured diagnostic interview, was used to assess diagnostic criteria for common mood, eating, and anxiety disorders, with the exception of PTSD and SUDs.
Self-report
The Impact of Event Scale-Revised (IES-R; Weiss & Marmar, 1997) is a widely used measure of the three DSM-IV PTSD symptom clusters (intrusion, avoidance, and arousal). The IES-R has demonstrated sound reliability and validity (e.g., Creamer, Bell, & Failla, 2003) and was used in the current study to assess PTSD symptoms specific to the target trauma used in the individualized trauma script.
The Alcohol Dependence Scale (ADS; Skinner & Horn, 1984) measures alcohol-related problems and symptoms, including withdrawal symptoms, tolerance, impaired control over drinking, and alcohol-seeking behavior. It displays solid psychometric properties (e.g., Drake, McHugo, & Biesanz, 1995).
Cue reactivity
The Positive and Negative Affect Scale (PANAS; Watson, Clark, & Tellegen, 1988) is a 20-item self-report scale that measures positive and negative affect. Each item is rated from 1 = very slightly or not at all to 5 = extremely. Items are summed to provide totals ranging from 10 to 50 for positive and negative affect. The PANAS has demonstrated sound psychometric properties (Crawford & Henry, 2004; Watson et al., 1988) and was used in the current study to measure affective responses to trauma and alcohol cue combinations.
Self-reported cue-elicited alcohol craving was assessed with three Likert-type scale items (Kozlowski, Pillitteri, Sweeney, Whitfield, & Graham, 1996). Participants rated three statements: (a) “I crave a drink right now,” (b) “I have a desire for a drink right now,” and (c) “I want a drink right now,” on a 0 to 10 Likert-type scale following each cue-combination trial. Items demonstrated high internal consistency (α = .97 following NN [neutral imagery cue followed by a neutral cue] condition) and were averaged to produce a single craving score.
Salivary flow
was used as a physiological measure of cue-elicited craving. This method is described fully by Monti and colleagues (1987). In brief, three preweighed dental cotton rolls were inserted under the tongue and between the inner check and lower gum on each side of the mouth and weighed again following the presentation of each cue combination. Magnitude of salivation was calculated by subtracting the pretrial weight from the posttrial weight.
Procedure
Assessment session
Prospective participants with scores above the cutoffs on the AUDIT and PCL were invited to complete an assessment session. At the assessment session, participants completed an Institutional Review Board (IRB)-approved, documented informed consent procedure. Participants who consented to participate then completed the C-DIS, NWS-PTSD module, CAPS, MINI, IES-R, and ADS to fully assess inclusion and exclusion criteria. Most participants had experienced multiple traumatic events. Therefore, following the recommendations of Weathers and Keane (1999), it was not required that their PTSD symptoms be associated with a single traumatic event on the CAPS. Instead, participants could relate each PTSD symptom to one or more traumatic events that fulfilled Criterion A for PTSD.
If eligible, participants were next asked to describe their worst traumatic event using multiple sensory dimensions (i.e., physical sensations, thoughts, emotions, olfactory sensations, visual details, and avoided activities and events), which provided information for a 60-s audiotaped narrative to be used in their laboratory session. They were then scheduled for a laboratory session within the next week and asked to maintain abstinence from alcohol and illicit drugs for 4 days prior to the laboratory session.
Laboratory session
To control for diurnal variations that may affect cue reactivity, laboratory sessions were scheduled between 1:00 p.m. and 3:00 p.m. On arrival for the laboratory session, participants were asked to remove any gum and were given a urine drug screen (UDS; Instant Technologies, Inc., Norfolk, Virginia) to assess recent drug use. Expired air samples were analyzed (Alco-sensor IV, Intoximeters, Inc., St. Louis, Missouri) to assess current alcohol intoxication. Participants who reported or tested positive for the metabolites of cocaine, opiates, benzodiazapines, amphetamines, methamphetamine, oxycodone, propoxyphene, barbiturates, and 3,4-methylenedioxymethamphetamine (MDMA) were rescheduled. However, participants who tested positive for Tetrahydrocannabinol (THC) and reported marijuana use in the past 30 days, but not the past 4 days, were allowed to participate in the laboratory session due to the long half-life of THC. Participants were then seated in a sound attenuated experimental room and provided detailed instructions of the laboratory procedure.
This laboratory procedure has been described in detail elsewhere (Coffey et al., 2010). Briefly, participants were presented four counterbalanced imagery in vivo cue combinations (i.e., trauma imagery cue followed by an alcohol cue [TA], trauma imagery cue followed by a neutral cue [TN], neutral imagery cue followed by an alcohol cue [NA], and NN). The trauma imagery cue was a 60-s narrative description of the participant’s subjectively rated worst traumatic event, the alcohol cue was their preferred alcoholic beverage, and the neutral cues were a 60-s narrative about changing a light bulb and a bottle of water. Prior to the presentation of these cue combinations, participants were led through a practice trial using an NN combination. Dental cotton rolls were inserted into participants’ mouths and they were instructed to close their eyes and listen to the narrative. Following the imagery presentation, the experimenter placed the beverage cue in front of the participant, and they were instructed to open their eyes and continue imagining the scene described in the narrative as vividly as possible for 2 min. Immediately following the 3-min imaginal in vivo cue exposure, the dental cotton rolls were removed and participants were instructed to complete self-report measures (i.e., craving and PANAS). Following the practice trial, this procedure was repeated for the four cue combinations (i.e., TA, TN, NA, NN). Participants provided a final craving rating at the end of the session to assure their safety on dismissal; a clinical psychologist was available to assist any distressed participants.
Analyses
Aim 1: Responses to alcohol and trauma cues
Repeated-measures ANOVA was used to examine differences among the four cue-combination trials on positive and negative affect (i.e., PANAS) and craving (i.e., self-report and salivary response). Statistically significant omnibus Fs were investigated with paired-samples t tests.
Aim 2: Cue-elicited affect and craving
To examine the relationship between cue-elicited alcohol craving and affect, change scores were first calculated to isolate the specific effects caused by the addition of alcohol cues. These change scores were calculated by subtracting affect or craving ratings administered after the neutral trials from the same measure administered after the alcohol trials. For example, two positive affect change scores were calculated for each person, one as the difference between NA and NN trials (NA-NN; representing affective responses to alcohol cues outside a trauma context) and another as the difference between TA and TN trials (TA-TN; representing affective responses to adding alcohol cues to trauma cues). Because the raw PANAS scores range from 10 to 50, these change scores could potentially range from +40 (indicating extreme increase in affect following cue presentation) to −40 (indicating extreme decrease in affect). Two negative affect, self-report craving and salivation change scores were calculated for each person in the same fashion. Four hierarchical multiple regression analyses were used to examine the incremental utility of adding positive affect (Step 2) to negative affect (Step 1) in the prediction of cue-elicited cravings (self-report and salivation).
Aim 3: Ambivalence model response types and cue-elicited craving
To examine how cue-elicited affect maps on to the ambivalence model of cravings, participants were classified into one of four responder types based on their positive and negative affect scores. First, individuals demonstrating an increase in positive affect from neutral to alcohol cue presentation trials (i.e., NA-NN) were designated “high positive”; individuals demonstrating either a decrease or no change in positive affect were classed as “low positive.” Participants were labeled as either “high negative” or “low negative” in the same manner. These labels were used to classify participants into one of the four ambivalence model responder types: “positive” (high positive/low negative), “negative” (low positive/high negative), “ambivalent” (high positive/high negative), and “indifferent” (low positive/low negative).
Repeated-measures ANOVA was used to examine differences between the four responder types and change in craving (self-report and salivary response) associated with adding alcohol cues to neutral cues (i.e., NA-NN). Statistically significant omnibus Fs were investigated with independent-samples t tests. Because group sizes were quite unequal for these analyses, conservative Scheffé tests were applied to limit Type 1 error. To examine whether results differed in the context of trauma cues, categorization and ANOVAs were repeated using affective responses to alcohol in trauma trials (i.e., TA-TN).
Results
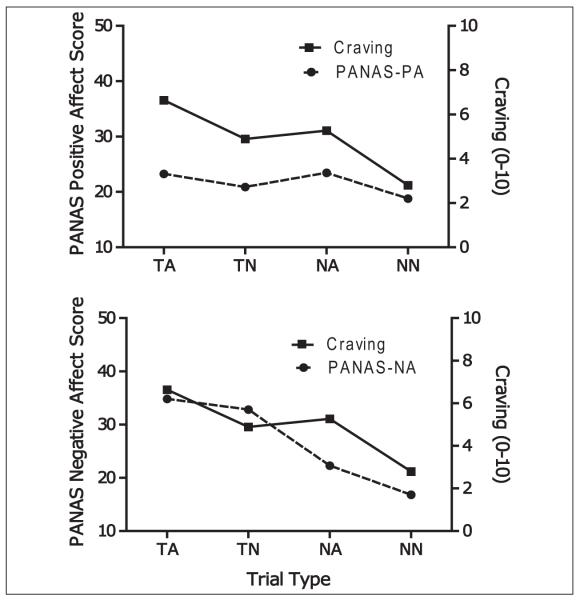
Means, standard deviations, and between-trial effect sizes for negative affect, positive affect, and craving are presented in Table 2; see Figure 1 for graphic presentation. No gender, education, employment, or ethnicity differences were found on PANAS scores or alcohol craving during the cue-reactivity paradigm.
Table 2.
Raw Means (SDs) and Between-Trial Effect Sizes (d) of Participants’ (N = 108) Ratings and Salivary Responding Following Each Cue-Combination Trial
| Trial |
Ms and SDs |
|||
|---|---|---|---|---|
| Positive affect | Negative affect | Craving | Salivation | |
| TA | 23.21 (7.10) | 34.81 (9.00) | 6.64 (3.37) | 1.55 (1.48) |
| TN | 20.81 (6.73) | 32.91 (9.63) | 4.90 (3.39) | 1.09 (1.07) |
| NA | 23.43 (7.70) | 22.27 (8.94) | 5.28 (3.33) | 1.25 (1.35) |
| NN | 18.79 (7.28) | 16.83 (7.43) | 2.80 (2.73) | 0.89 (0.76) |
|
| ||||
| Trial differences | Between-trial effect sizes | |||
|
| ||||
| TA-TN | 0.34 | 0.21 | 0.52 | 0.34 |
| TA-NA | −0.03 | 1.40 | 0.41 | 0.20 |
| TA-NN | 0.62 | 2.19 | 1.26 | 0.59 |
| TN-NA | −0.35 | 1.13 | −0.11 | −0.14 |
| TN-NN | 0.30 | 1.87 | 0.69 | 0.23 |
| NA-NN | 0.62 | 0.66 | 0.80 | 0.37 |
Note: TA = trauma-image/in vivo alcohol cue, TN = trauma-image/in vivo neutral cue, NA = neutral-image/in vivo alcohol cue, NN = neutral-image/in vivo neutral cue.
Small effect size (d) = 0.2, medium effect size = 0.5, large effect size = 0.8.
Figure 1.
Cue-elicited affect and self-report craving means
Aim 1: Responses to Alcohol and Trauma Cues
Negative affect
A significant main effect was found for trial, F(3, 321) = 172.71, p < .001, ηp2 = .62. Post hoc tests revealed the TA trial elicited significantly more negative affect than the TN (p = .004), NA (p < .001), and NN trials (p < .001). The TN trial elicited significantly greater negative affect than the NA (p < .001) and NN trials (p < .001). Last, the NA trial elicited significantly greater negative affect than the NN trial (p < .001).
Positive affect
A significant main effect was found for trial, F(3, 321) = 17.30, p < .001, ηp2 = .14. Post hoc analysis of the trial types revealed that the TA and NA trials elicited higher levels of positive affect than the TN and NN trials, all ps < .001. The TA and NA trials elicited equivalent levels of positive affect (p = .80), whereas the TN trials elicited significantly greater positive affect than the NN trial (p = .01).
To examine whether the TN increased positive affect over NN as a function oof PANAS positive affect scale items potentially tapping anxious arousal (“alert,” “attentive,” “active”), analyses were repeated after removing these three items. Consistent with this explanation, a significant main effect was found for trial, F(3, 321) = 19.05, p < .001, ηp2 = .15. Post hoc analysis of the trial types revealed that the NA trials elicited higher levels of positive affect than all other trials, including TA, ps < .01, ds > .26. The TA trial elicited higher levels of positive affect than TN and NN, ps < .01, ds > .41. The TN and NN trials were no longer significantly different, p = .47, d = .09.
Self-reported craving
Results from the self-report craving measure were similar to the PANAS findings. First, a significant main effect was found for trial, F(3, 321) = 91.71, p < .001, ηp2 = .46. Post hoc analysis of the trial types revealed that the TA trial produced higher craving than the TN, the NA, and the NN trials (all ps < .001). The TN trial produced higher craving than the NN trial (p < .001) but did not differ statistically from the NA trial (p = .12). The NA trial produced higher craving ratings than the NN trial (p < .001).
Salivation
Analyses of salivation showed congruent effects. A significant main effect was found for trial, F(3, 318) = 19.31, p < .001, ηp2 = .15. Post hoc analysis of the trial types revealed that the TA trial produced greater salivation than the TN, NA, and the NN trials (all ps < .001). The TN trial produced greater salivary response than the NN trial (p < .001) but differed only marginally from the NA trial (p = .07). The NA trial produced more salivation than the NN trial (p < .001).
Aim 2: Cue-Elicited Affect and Craving
Correlation and multiple regression analyses were conducted to examine the relationship between affective responses to cues and alcohol cue-elicited craving. Increases in self-reported craving associated with adding alcohol cues to neutral cues (NA-NN) correlated with an increase in negative (r = .34, p < .001) and positive affect (r = .23, p = .02); increases in craving associated with adding alcohol cues to trauma cues (TA-TN) was also associated with an increase in negative (r = .25, p = .01) and positive affect (r = .19, p = .049). Increases in salivation associated with the addition of alcohol cues to neutral cues correlated with increases in positive affective responses (r = .20, p = .04) but was unrelated to change in negative affect (r = .06, p = .51). Increases in salivation associated with the addition of alcohol cues to trauma cues were unrelated to affective changes of either valence (rs < .09, ps > .45).
Correlations between subjective craving and salivary responsivity to alcohol cues were not significant, either in the context of neutral cues (NA-NN; r = .15, p = .11) or trauma cues (TA-TN; r = .10, p = .31). Within modality, there was only a marginally significant relationship between subjective craving reactivity to alcohol cues in the context of neutral versus trauma cues, r = .18, p = .07. Salivary responses to alcohol were more consistent, with NA-NN and TA-TN reactivity correlating at r = .45, p < .001.
Self-reported craving
The full model accounted for 15% of variance in craving score change from the NN to NA condition, F(2, 105) = 9.25, p < .001. Change in negative affect from NN to NA accounted for 12% of variance at Step 1 of the model, β = .34, p < .001. Change in positive affect from NN to NA accounted for an additional 3% of variance at Step 2 of the model, β = .19, p = .04.
With regard to difference in craving scores between the TA and TN conditions, the full model accounted for 8% of variance in craving score change from the TN to TA condition, F(2, 105) = 4.80, p = .01. Change in negative affect from TN to TA accounted for 6% of variance at Step 1 of the model, β = .25, p < .001. Change in positive affect from TN to TA did not explain any additional variance at Step 2 of the model, β = .15, p = .11.
Salivation
When examining salivary responses to the addition of alcohol cues to neutral cues (i.e., NA-NN), the full model accounted for 4% of variance in salivation change from the NN to NA condition but did not reach statistical significance, F(2, 104) = 2.19, p = .12. Change in negative affect from NN to NA was unrelated to change in salivation at Step 1 of the model, β = .06, p = .51. However, change in positive affect explained significant incremental variance at Step 2, r2 change = .04, β = .19, p = .05.
With regard to difference in salivation scores between the TA and TN conditions, the full model accounted for 0.6% of variance in salivation score change from TN to TA and was not statistically significant, F(2, 105) = 0.292, p = .75. Change in negative and positive affect did not account for variation in salivary responding at either step of the model, βs < .08, ps >.45.
Aim 3: Ambivalence Model Response Types and Cue-Elicited Craving
Means, standard deviations, and between-group effect sizes comparing cueelicited cravings among individuals classified as “positive,” “negative,” “ambivalent,” or “indifferent” affective responders are presented in Table 3.
Table 3.
Affective Response Types: Means (SDs) and Between-Group Effect Sizes (d) of Cue-Elicited Change in Craving and Salivary Responding
| Groups |
Ms and SDs |
|||||
|---|---|---|---|---|---|---|
| NA-NN |
TA-TN |
|||||
| n | Self-report craving |
Salivation | n | Self-report craving |
Salivation | |
| Positive | 20 | 1.33 (1.85)a | 0.46 (0.78)a | 24 | 1.64 (1.68)a,b | 0.38 (0.64)a |
| Ambivalent | 56 | 3.37 (2.34)b | 0.38 (0.87)a | 40 | 2.35 (2.05)b | 0.45 (0.91)a |
| Indifferent | 9 | 0.81 (0.72)a | 0.00 (0.43)a | 21 | 0.76 (1.38)a | 0.30 (0.89)a |
| Negative | 23 | 1.97 (1.98)a,b | 0.18 (0.41)a | 23 | 1.67 (2.43)a,b | 0.57 (1.00)a |
|
| ||||||
| Group differences |
Between-group effect sizes | |||||
|
| ||||||
| Ambivalent– positive |
0.93 | −0.10 | 0.38 | 0.09 | ||
| Ambivalent– negative |
0.63 | 0.26 | 0.31 | −0.13 | ||
| Ambivalent– indifferent |
1.18 | 0.47 | 0.87 | 0.17 | ||
| Positive– negative |
−0.34 | 0.47 | −0.01 | −0.23 | ||
| Positive– indifferent |
0.34 | 0.69 | 0.58 | 0.11 | ||
| Negative– indifferent |
0.69 | 0.45 | 0.47 | 0.29 | ||
Note: NA-NN reflects change in response from NN (neutral-image/in vivo neutral cue) to NA (neutral-image/in vivo alcohol cue) trial. TA-TN reflects change in response from TN (traumaimage/in vivo neutral cue) to TA (trauma-image/in vivo alcohol cue) trial. Means sharing similar superscripts do not differ significantly based on Scheffé corrections. Small effect size (d) = 0.2, medium effect size = 0.5, large effect size = 0.8.
Homogeneous subgroups comparing the four responder types for each dependent variable (i.e., comparison of means within same vertical column).
Homogeneous subgroups comparing the four responder types for each dependent variable (i.e., comparison of means within same vertical column).
Self-reported craving
For changes in self-reported craving associated with adding alcohol to neutral cues (NA-NN), a significant main effect was found for affective responder classification, F(3, 104) =7.69, p<.001, ηp2 = .18. Post hoc Scheffé tests revealed that “ambivalent” responders reported significantly greater cue-elicited increases in craving than individuals classified as “positive” (p = .004) or “indifferent” (p = .01) and marginally greater craving than those classified as “negative” responders (p = .07). Individuals classified as “positive,” “negative,” or “indifferent” did not report significantly different cue-elicited changes in craving, ps > .58.
When adding alcohol to trauma cues (TA-TN), there were again significant differences between affective responder classifications, F(3, 104) =3.08, p =.03, ηp2 = .08. Post hoc Scheffé tests revealed that “ambivalent” responders reported significantly greater cue-elicited increases in craving than individuals classified as “indifferent” (p = .03). There were no other statistically significant group differences, ps > .42.
Salivation
There were no statistically significant differences among the four responder groups when adding alcohol to neutral cues (NA-NN), F(3, 104) = 1.11, p = .35, ηp2 = .03, or when adding alcohol to trauma cues (TA-TN), F(3, 104) = 0.38, p = .77, ηp2 = .01.
Discussion
Responses to Alcohol and Trauma Cues
The first goal of the present study was to investigate affective responses to alcohol and trauma cues among individuals with PTSD and AD. First, it was hypothesized that the combined trauma image-alcohol cue (TA trials) would increase negative affect and craving more than any other cue condition. Consistent with this hypothesis, trauma cues (TA and TN) elicited the strongest negative affect, with the greatest distress occurring following presentation of trauma and alcohol cues together (TA trials). Together, this evidence indicates a potential additive effect whereby trauma and alcohol cues trigger stronger negative affect in individuals with PTSD-AD than either cue alone. This builds on previous work demonstrating a relationship between cueelicited craving and increases in guilt, anxiety, and fear in alcohol-dependent individuals (Cooney et al., 1987; Fox et al., 2007). Consistent with the cuereactivity literature (see Carter & Tiffany, 1999), trauma and alcohol cues also produced moderate to large increases in self-reported craving and salivation. Craving was highest when trauma and alcohol cues were presented together, relative to when either type of cue was presented alongside a neutral counterpart (i.e., TA > TN and NA). This finding is in line with previous work indicating that negative affective states trigger urges to drink (Cannon et al., 1992; Fox et al., 2007; Rubonis et al., 1994). Taken together, the present results provide support for a model whereby negative affect, exposure to drug/alcohol and trauma cues, and craving mutually encourage one another. This process is consistent with bidirectional conceptualizations of concurrent PTSD-SUD (Brown et al., 1998).
Second, it was hypothesized that alcohol cues would elicit increases in positive affect. This hypothesis was also supported, given that the trauma script-alcohol and neutral script-alcohol conditions (TA and NA) were associated with the greatest levels of positive affect. This effect was most obvious when trials involving alcohol were compared with neutral-neutral cue conditions (i.e., TA and NA > NN; medium effect sizes), but small effects were also observed between the trauma script-alcohol and trauma script-neutral cues (i.e., TA > TN). These findings replicate and extend past research demonstrating cue-elicited positive affect among normative social drinkers (Kambouropoulos & Rock, 2010; Kambouropoulos & Staiger, 2004) within a treatment-seeking PTSD-AD sample. The finding that alcohol cues increase positive affect even in the context of trauma imagery is novel and underscores the reinforcing properties of alcohol-seeking behavior. This may be an important mechanism underlying the maintenance of alcohol use among highly distressed populations.
Trauma cues also elicited more positive affect than neutral script cues (i.e., TN > NN), but this effect disappeared once three PANAS-PA items overlapping with anxious arousal (“alert,” “attentive,” “active”) were removed. Thus, trauma cues do not appear to appreciably increase positive affect. Future work examining affective responses to trauma may wish to account for this measurement effect or supplement with alternative assessment modalities (e.g., facial electromyography responses).
Cue-Elicited Affect and Craving
The second aim of the current study was to examine the relationship between cue-elicited affect and craving. Previous research, as well as available data, indicates that increases in negative affect are associated with increased craving. However, given the paucity of research on positive affect in this population, as well as models highlighting the importance of appetitive responses in craving (e.g., Breiner et al., 1999; Stritzke et al., 2007; Tiffany, 1990), the role of positive affect in craving, above and beyond that of negative affect, was of particular interest. As hypothesized, when examining the addition of alcohol to neutral cues (i.e., NA-NN responses), positive affect explained a significant proportion of variance in self-reported craving and salivation responses, over and above that already accounted for by negative affect. Together, these results underscore the importance of positive and negative affective responses in understanding cue-elicited alcohol craving. In fact, this is the first evidence to our knowledge that cue-elicited positive affect explains incremental variance in alcohol cravings among individuals with comorbid PTSD and AD. This work complements multidimensional models of cravings as well as literature indicating relationships among positive affect, outcome expectancies, and craving in alcohol users without comorbid PTSD (Johnson & Fromme, 1994; Litt et al., 2000).
When examining alcohol cue-elicited craving in the context of trauma cues (i.e., TA-TN responses), negative affect was positively correlated with craving, a finding consistently demonstrated in previous work (Coffey et al., 2002; Coffey et al., 2006; Saladin et al., 2003). However, positive affect did not explain a significant proportion of variance in self-reported craving over and above that accounted for by negative affect in the presence of trauma cues. Similarly, neither positive nor negative affective responses were associated with cue-elicited salivation in this context. The discrepant findings between the NA-NN and TA-TN findings are intriguing and underscore the importance of examining cravings from a multidimensional perspective. Specifically, the relative importance of positive or negative affect in SUD may vary depending on contextual factors. When triggered by traumatic memories, distress may be the strongest determinant of alcohol use among individuals with PTSD and AD. However, in a neutral environment, feeling distressed or happy may trigger drinking. Treatments for individuals with PTSD-AD may need to address these different pathways to use.
Ambivalence Model Response Types and Cue-Elicited Craving
Our final study goal was to examine the relationship between cue-elicited affect and cravings as an extension of the ambivalence model of cravings. Partially consistent with the hypotheses, participants classified as “ambivalent” affective responders (i.e., demonstrating increases in positive and negative affect in response to cues) reported significantly greater increases in self-reported craving than individuals classified as “positive” (increases in positive but not negative affect) or “indifferent” (no increases in either affect valence) and marginally greater increases in craving than “negative” responders (increases in negative but not positive affect). There were no group differences in salivary responses.
These results are generally consistent with models of cravings that point to the role of conflicting positive and negative responses in the subjective experience of craving (Stritzke et al., 2007; Tiffany, 1990). It is possible, however, that positive and negative affect in response to alcohol and trauma cues do not reflect pure approach and avoidance motivations, given that individuals classified as “positive” did not evidence relatively stronger cravings. Affective ambivalence may instead relate to craving and subsequent motivation to drink as a function of the greater affective intensity, more generally, as present in the “ambivalent” class of responders. Alternatively, as initial euphoric responses to drug cues have been shown to give way to increasing levels of irritability and frustration over time (O’Brien, Ehrman, & Ternes, 1986; see Stasiewicz & Maisto, 1993, for discussion), craving could also be higher among “ambivalent” responders as a function of frustration. Although this is one of the first studies to examine affective ambivalence in substance use cravings, it builds on some preliminary work examining the role of affective ambivalence in desire for food and sex (e.g., Hormes & Rozin, 2011; Peterson & Janssen, 2007).
Limitations
Several limitations of the current work are worth noting. First, no diagnostic control group was used. As such, although results shed light on affective responses to drug and alcohol cues, it cannot be concluded that these effects are unique to individuals with PTSD and AD. Individuals with comorbid SUD and depression, for example, may display similar response patterns. Comparison with nonclinical and alternative clinical groups would clarify the specificity of results. Second, the sample comprises individuals from a residential SUD treatment facility. People who are seeking treatment may experience different affective responses to cues and may arguably be less ambivalent about their use than substance users in the general population. In addition, although participants completed the laboratory session less than a week after being admitted into the treatment program, they may already have learned new coping strategies that influenced their affective responses to cues. Thus, results may not generalize to nontreatment seekers. Third, although the present study examines positive and negative affect as an extension of the ambivalence model of cravings, several constructs that are important to these models (e.g., expectations about the effects of use, motivation, cognition, and actual drinking behavior; Breiner et al., 1999) were not assessed. Future laboratory work examining affective ambivalence would benefit from the inclusion of explicit self-report and behavioral measures of approach and avoidance motivation, such as the Approach and Avoidance of Alcohol Questionnaire (McEvoy et al., 2004). Finally, self-reported craving and affective ratings were collected within the same assessment period of the laboratory study, and therefore, it is unclear whether affect promoted craving, whether the reverse was true, or whether bidirectional influences existed. Future work using diverse study designs could help determine the interrelations among these variables.
Conclusions and Future Directions
Understanding affective responses to alcohol and trauma cues will be an important step toward advancing conceptual models of concurrent PTSD-AD, particularly as it relates to craving. The present study demonstrates that exposure to alcohol cues among treatment-seeking individuals with comorbid PTSD and AD increases positive and negative affect in addition to self-reported craving and salivation. Negative affective responses to alcohol cues correlated significantly with self-reported craving in the context of neutral and trauma cues. A novel finding was that positive affective responses explained significant incremental variance in self-reported craving and salivation when cues were accompanied by neutral, but not trauma imagery. Consistent with this, participants classified as “ambivalent” affective responders reported the greatest cue-elicited increases in cravings, particularly in the context of neutral imagery cues. Overall, findings highlight the importance of independently assessing positive and negative affective responses to cues in understanding the complexity of cravings in individuals with comorbid PTSD and AD. Results are consistent with multidimensional conceptualizations of cravings and encourage greater consideration of the rewarding elements of drinking and the importance of resolving ambivalence in the treatment of SUDs (Breiner et al., 1999; Miller & Rollnick, 1991). Increasing awareness of affective responses to cues and developing targeted strategies to cope with cravings in different emotional contexts may be a valuable area for further research and intervention.
Acknowledgments
The authors wish to thank M. Trost Friedler, Jackie Lampley, and the staff and patients of Harbor House Recovery Center for their cooperation on this study. They also wish to thank Robert C. Schlauch for his helpful comments on an earlier draft of this manuscript.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported, in part, by National Institute on Alcohol Abuse and Alcoholism Grant R01AA016816 (PI: Coffey).
Biography
Elizabeth Nosen is a Ph.D. student in Clinical Psychology at the University of British Columbia and is currently completing her predoctoral internship at the University of Mississippi Medical Center and G.V. (Sonny) Montgomery VA Medical Center. Her research interests focus on cognitive and emotion regulation processes in anxiety and substance use disorders.
Yael I. Nillni is a Ph.D. student in Clinical Psychology at the University of Vermont and is currently completing her predoctoral internship at the University of Mississippi Medical Center and G.V. (Sonny) Montgomery VA Medical Center. Her primary research interests are in the identification of sex-specific mechanisms involved in the etiology and/or maintenance of anxiety and mood disorders.
Erin C. Berenz received her Ph.D. in Clinical Psychology from the University of Vermont. She is currently a postdoctoral fellow at the Virginia Institute for Psychiatric and Behavioral Genetics at Virginia Commonwealth University. Her primary research interests are in the areas of posttraumatic stress disorder and co-occurring substance use disorders.
Julie A. Schumacher received her Ph.D. in Clinical Psychology from the State University of New York at Stony Brook. She is currently an Associate Professor of Psychiatry at the University of Mississippi Medical Center. Her primary research interests are in the areas of drug and alcohol abuse and violent behavior.
Paul R. Stasiewicz received his Ph.D. in Clinical Psychology from The State University of New York at Binghamton. He is currently a Research Scientist at the University at Buffalo’s Research Institute on Addictions. His research interests include learning-based processes of addiction and the application of basic behavioral processes to the development of new clinical interventions.
Scott F. Coffey received his Ph.D. in Clinical Psychology from the University of Mississippi. He is Professor and Director of the Division of Psychology in the Department of Psychiatry and Human Behavior at the University of Mississippi Medical Center. His research interests include substance use disorders, posttraumatic stress disorder (PTSD), the co-occurrence of PTSD and substance abuse, cue reactivity, psychotherapy treatment development, and impulsivity.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Anton RF. What is craving? Models and implications for treatment. Alcohol Research & Health. 1999;23:165–173. [PMC free article] [PubMed] [Google Scholar]
- Babor TF, de la Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for use in primary care (WHO Publication No. 92.4) World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- Back S, Dansky BS, Coffey SF, Saladin ME, Sonne S, Brady KT. Cocaine dependence with and without posttraumatic stress disorder: A comparison of substance use, trauma history and psychiatric comorbidity. American Journal on Addictions. 2000;9:51–62. doi: 10.1080/10550490050172227. doi:10.1080/10550490050172227. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Barefoot JC, Fairbank JA, Helms MJ, Haney TL, Davidson JR. Ambulatory cardiovascular activity in Vietnam combat veterans with and without posttraumatic stress disorder. Journal of Consulting and Clinical Psychology. 2000;68:269–276. doi: 10.1037//0022-006x.68.2.269. doi:10.1037/0022-006X.68.2.269. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered PTSD Scale. Journal of Traumatic Stress. 1995;8:75–90. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behaviour Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Breiner MJ, Stritzke WGK, Lang AR. Approaching avoidance: A step essential to the understanding of craving. Alcohol Research & Health. 1999;23:197–206. [PMC free article] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Gannon-Rowley J. Substance use disorder-PTSD comorbidity: Patients perceptions of symptom interplay and treatment issues. Journal of Substance Abuse Treatment. 1998;15:445–448. doi: 10.1016/s0740-5472(97)00286-9. doi:10.1016/s0740-5472(97)00286-9. [DOI] [PubMed] [Google Scholar]
- Brown PJ, Stout RL, Mueller T. Substance use disorder and posttraumatic stress disorder comorbidity: Addiction and psychiatric treatment rates. Psychology of Addictive Behaviors. 1999;13:115–122. doi:10.1037/0893-164X.13.2.115. [Google Scholar]
- Cannon DS, Rubin A, Keefe CK, Black JL, Leeka JK, Phillips LA. Affective correlates of alcohol and cocaine use. Addictive Behaviors. 1992;17:517–524. doi: 10.1016/0306-4603(92)90061-y. doi:10.1016/0306-4603(92)90061-y. [DOI] [PubMed] [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94:327–340. doi:10.1046/j.1360-0443.1999.9433273.x. [PubMed] [Google Scholar]
- Coffey SF, Saladin ME, Drobes DJ, Brady KT, Dansky BS, Kilpatrick DG. Trauma and substance cue reactivity in individuals with comorbid posttraumatic stress disorder and cocaine or alcohol dependence. Drug and Alcohol Dependence. 2002;65:115–127. doi: 10.1016/s0376-8716(01)00157-0. doi:10.1016/s0376-8716(01)00157-0. [DOI] [PubMed] [Google Scholar]
- Coffey SF, Schumacher JA, Stasiewicz PR, Henslee AM, Baillie LE, Landy N. Craving and physiological reactivity to trauma and alcohol cues in posttraumatic stress disorder and alcohol dependence. Experimental and Clinical Psychopharmacology. 2010;18:340–349. doi: 10.1037/a0019790. doi:10.1037/a0019790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coffey SF, Stasiewicz PR, Hughes PM, Brimo ML. Trauma-Focused imaginal exposure for individuals with comorbid posttraumatic stress disorder and alcohol dependence: Revealing mechanisms of alcohol craving in a cue reactivity paradigm. Psychology of Addictive Behaviors. 2006;20:425–435. doi: 10.1037/0893-164X.20.4.425. doi:10.1037/0893-164x.20.4.425. [DOI] [PubMed] [Google Scholar]
- Cooney NL, Gillespie RA, Baker LH, Kaplan RF. Cognitive changes after alcohol cue exposure. Journal of Consulting and Clinical Psychology. 1987;55:150–155. doi: 10.1037//0022-006x.55.2.150. doi: 10.1037/0022-006X.55.2.150. [DOI] [PubMed] [Google Scholar]
- Crawford JR, Henry JD. The Positive and Negative Affect Schedule (PANAS): Construct validity, measurement properties and normative data in a large non-clinical sample. British Journal of Clinical Psychology. 2004;43:245–265. doi: 10.1348/0144665031752934. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale-Revised. Behaviour Research and Therapy. 2003;41:1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Dansky BS, Bryne CA, Brady KT. Intimate violence and post-traumatic stress disorder among individuals with cocaine dependence. American journal of drug and alcohol abuse. 1999;25:257–268. doi: 10.1081/ada-100101859. [DOI] [PubMed] [Google Scholar]
- Dansky BS, Roitzsch JC, Brady KT, Saladin ME. Posttraumatic stress disorder and substance abuse: Use of research in a clinical setting. Journal of Traumatic Stress. 1997;10:141–148. doi: 10.1023/a:1024872800683. doi:10.1023/A:1024872800683. [DOI] [PubMed] [Google Scholar]
- Drake RE, McHugo GJ, Biesanz JC. The test-retest reliability of standardized instruments among homeless persons with substance use disorders. Journal of Studies on Alcohol. 1995;56:161–167. doi: 10.15288/jsa.1995.56.161. [DOI] [PubMed] [Google Scholar]
- Fox HC, Bergquist KL, Hong K-I, Sinha R. Stress-induced and alcohol cue-induced craving in recently abstinent alcohol-dependent individuals. Alcoholism: Clinical & Experimental Research. 2007;31:395–403. doi: 10.1111/j.1530-0277.2006.00320.x. doi:10.1111/j.1530-0277.2006.00320.x. [DOI] [PubMed] [Google Scholar]
- Hormes JM, Rozin P. The temporal dynamics of ambivalence: Changes in positive and negative affect in relation to consumption of an emotionally charged food. Eating Behaviors. 2011;12:219–221. doi: 10.1016/j.eatbeh.2011.02.001. doi: 10.1016/j.eatbeh.2011.02.001. [DOI] [PubMed] [Google Scholar]
- Johnson CN, Fromme K. An experimental test of affect, subjective craving, and alcohol outcome expectancies as motivators of young adult drinking. Addictive Behaviors. 1994;19:631–641. doi: 10.1016/0306-4603(94)90018-3. doi:10.1016/0306-4603(94)90018-3. [DOI] [PubMed] [Google Scholar]
- Kambouropoulos N, Rock A. Extraversion and altered state of awareness predict alcohol cue-reactivity. Journal of Individual Differences. 2010;31(2010):178–184. [Google Scholar]
- Kambouropoulos N, Staiger PK. Reactivity to alcohol-related cues: Relationship among cue type, motivational processes, and personality. Psychology of Addictive Behaviors. 2004;18:275–283. doi: 10.1037/0893-164X.18.3.275. doi:10.1037/0893-164x.18.3.275. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ. The self-medication hypothesis of substance use disorders: A reconsideration and recent applications. Harvard Review of Psychiatry. 1997;4:231–244. doi: 10.3109/10673229709030550. doi:10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Kozlowski LT, Pillitteri JL, Sweeney CT, Whitfield KE, Graham JW. Asking questions about urges or cravings for cigarettes. Psychology of Addictive Behaviors. 1996;10:248–260. [Google Scholar]
- Litt MD, Cooney NL, Morse P. Reactivity to alcohol-related stimuli in the laboratory and in the field: Predictors of craving in treated alcoholics. Addiction. 2000;95:889–900. doi: 10.1046/j.1360-0443.2000.9568896.x. doi:10.1046/j.1360-0443.2000.9568896.x. [DOI] [PubMed] [Google Scholar]
- Mason BJ, Light JM, Escher T, Drobes DJ. Effect of positive and negative affective stimuli and beverage cues on measures of craving in non treatment-seeking alcoholics. Psychopharmacology. 2008;200:141–150. doi: 10.1007/s00213-008-1192-x. doi:10.1007/ s00213-008-1192-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEvoy PM, Stritzke WGK, French DJ, Lang AR, Ketterman RL. Comparison of three models of alcohol craving in young adults: A cross-validation. Addiction. 2004;99:482–497. doi: 10.1111/j.1360-0443.2004.00714.x. doi:10.1111/j.1360-0443.2004.00714.x. [DOI] [PubMed] [Google Scholar]
- Miller W, Rollnick S. Motivational Interviewing: Preparing people for change. Guilford; New York, NY: 1991. [Google Scholar]
- Monti PM, Binkoff JA, Abrams DB, Zwick WR, Nirenberg TD, Liepman MR. Reactivity to alcoholics and non-alcoholics to drinking cues. Journal of Abnormal Psychology. 1987;96:122–126. doi: 10.1037//0021-843x.96.2.122. [DOI] [PubMed] [Google Scholar]
- Norman SB, Tate SR, Anderson KG, Brown SA. Do trauma history and PTSD symptoms influence addiction relapse context? Drug and Alcohol Dependence. 2007;90:89–96. doi: 10.1016/j.drugalcdep.2007.03.002. doi:10.1016/j.drugalcdep.2007.03.002. [DOI] [PubMed] [Google Scholar]
- O’Brien CP, Ehrman RN, Ternes JW. Classical conditioning in human opioid dependence. In: Goldberg SR, Stolerman IP, editors. Behavioral analysis of drug dependence. Academic Press; Orlando, FL: 1986. pp. 329–356. [Google Scholar]
- Ouimette PC, Finney JW, Moos RH. Two-year posttreatment functioning and coping of substance abuse patients with posttraumatic stress disorder. Psychology of Addictive Behaviors. 1999;13:105–114. doi:10.1037/0893-164X.13.2.105. [Google Scholar]
- Peterson ZD, Janssen E. Ambivalent affect and sexual response: The impact of co-occurring positive and negative emotions on subjective and physiological sexual responses to erotic stimuli. Archives of Sexual Behavior. 2007;36:793–807. doi: 10.1007/s10508-006-9145-0. doi:10.1007/s10508-006-9145-0. [DOI] [PubMed] [Google Scholar]
- Read JP, Brown PJ, Kahler CW. Substance use and posttraumatic stress disorders: Symptom interplay and effects on outcome. Addictive Behaviors. 2004;29:1665–1672. doi: 10.1016/j.addbeh.2004.02.061. doi:10.1016/j.addbeh.2004.02.061. [DOI] [PubMed] [Google Scholar]
- Resnick H. Psychometric review of National Women’s Study (NWS) Event History-PTSD Module. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Sidran Press; Lutherville, MD: 1996. pp. 214–217. [Google Scholar]
- Resnick HS, Kilpatrick DG, Dansky BS, Saunders BE, Best CL. Prevalence of civilian trauma and posttraumatic stress disorder in a representative national sample of women. Journal of Consulting and Clinical Psychology. 1993;61:984–991. doi: 10.1037//0022-006x.61.6.984. [DOI] [PubMed] [Google Scholar]
- Reynolds M, Mezey G, Chapman M, Wheeler M, Drummond C, Baldacchino A. Co-morbid post-traumatic stress disorder in a substance misusing clinical population. Drug and Alcohol Dependence. 2005;77:251–258. doi: 10.1016/j.drugalcdep.2004.08.017. doi:10.1016/j.drugalcdep.2004.08.017. [DOI] [PubMed] [Google Scholar]
- Robins LN, Cottler LB, Bucholz KK, Compton WM, North CS, Rourke KM. Diagnostic Interview Schedule for the DSM-IV (DIS-IV) Washington University; St. Louis, MO: 2000. [Google Scholar]
- Rubonis AV, Colby SM, Monti PM, Rohsenow DJ, Gulliver SB, Sirota AD. Alcohol cue reactivity and mood induction in male and female alcoholics. Journal of Studies on Alcohol. 1994;55:487–494. doi: 10.15288/jsa.1994.55.487. [DOI] [PubMed] [Google Scholar]
- Saladin ME, Drobes DJ, Coffey SF, Dansky BS, Brady KT, Kilpatrick DG. PTSD symptom severity as a predictor of cue-elicited drug craving in victims of violent crime. Addictive Behaviors. 2003;28:1611–1629. doi: 10.1016/j.addbeh.2003.08.037. doi:10.1016/j. addbeh.2003.08.037. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier V, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (MINI): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59:22–23. [PubMed] [Google Scholar]
- Skinner HA, Horn JL. Alcohol Dependence Scale: Users guide. Addiction Research Foundation; Toronto, Canada: 1984. [Google Scholar]
- Stasiewicz PR, Maisto SA. Two-factor avoidance theory: The role of negative affect in the maintenance of substance use and substance use disorder. Behavior Therapy. 1993;24:337–356. doi:10.1016/s0005-7894(05)80210-2. [Google Scholar]
- Stewart SH, Conrod PJ. Psychosocial models of functional associations between posttraumatic stress disorder and substance use disorder. In: Ouimette P, Brown PJ, editors. Trauma and substance abuse: Causes, consequences, and treatment of comorbid disorders. American Psychological Association; Washington, DC: 2003. pp. 29–55. [Google Scholar]
- Stritzke WGK, Breiner MJ, Curtin JJ, Lang AR. Assessment of substance cue reactivity: Advances in reliability, specificity, and validity. Psychology of Addictive Behaviors. 2004;18:148–159. doi: 10.1037/0893-164X.18.2.148. doi:10.1037/0893-164x.18.2.148. [DOI] [PubMed] [Google Scholar]
- Stritzke WG, McEvoy PM, Wheat LR, Dyer KR, French DJ. The Yin and Yang of indulgence and restraint: The ambivalence model of craving. In: O’Neal PW, editor. Motivation of Health Behavior. Nova Science; New York, NY: 2007. pp. 31–47. [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior: Role of automatic and nonautomatic processes. Psychological Review. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. doi:10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Vandiver T, Sher KJ. Temporal stability of the diagnostic interview schedule. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1991;3:277–281. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS Scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD Checklist (PCL): Reliability, validity, and diagnostic utility; Paper presented at the Annual Convention of the International Society for Traumatic Stress Studies; San Antonio, TX. 1993. [Google Scholar]
- Weathers FW, Keane TM. Psychological assessment of traumatized adults. In: Saigh PA, Bremner JG, editors. Posttraumatic stress disorder: A comprehensive text. Allyn & Bacon; Boston, MA: 1999. pp. 219–247. [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD Scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale-Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. Guilford; New York, NY: 1997. pp. 399–411. [Google Scholar]