Abstract
BACKGROUND
The order and magnitude of pathologic processes in Alzheimer’s disease are not well understood, partly because the disease develops over many years. Autosomal dominant Alzheimer’s disease has a predictable age at onset and provides an opportunity to determine the sequence and magnitude of pathologic changes that culminate in symptomatic disease.
METHODS
In this prospective, longitudinal study, we analyzed data from 128 participants who underwent baseline clinical and cognitive assessments, brain imaging, and cerebrospinal fluid (CSF) and blood tests. We used the participant’s age at baseline assessment and the parent’s age at the onset of symptoms of Alzheimer’s disease to calculate the estimated years from expected symptom onset (age of the participant minus parent’s age at symptom onset). We conducted cross-sectional analyses of baseline data in relation to estimated years from expected symptom onset in order to determine the relative order and magnitude of pathophysiological changes.
RESULTS
Concentrations of amyloid-beta (Aβ)42 in the CSF appeared to decline 25 years before expected symptom onset. Aβ deposition, as measured by positron-emission tomography with the use of Pittsburgh compound B, was detected 15 years before expected symptom onset. Increased concentrations of tau protein in the CSF and an increase in brain atrophy were detected 15 years before expected symptom onset. Cerebral hypometabolism and impaired episodic memory were observed 10 years before expected symptom onset. Global cognitive impairment, as measured by the Mini–Mental State Examination and the Clinical Dementia Rating scale, was detected 5 years before expected symptom onset, and patients met diagnostic criteria for dementia at an average of 3 years after expected symptom onset.
CONCLUSIONS
We found that autosomal dominant Alzheimer’s disease was associated with a series of pathophysiological changes over decades in CSF biochemical markers of Alzheimer’s disease, brain amyloid deposition, and brain metabolism as well as progressive cognitive impairment. Our results require confirmation with the use of longitudinal data and may not apply to patients with sporadic Alzheimer’s disease. (Funded by the National Institute on Aging and others; DIAN ClinicalTrials.gov number, NCT00869817.)
Alzheimer’s disease is the most common cause of dementia and is currently estimated to affect more than 5 million people in the United States, with an expected increase to 13 million by the year 2050. The typical clinical presentation is progressive loss of memory and cognitive function, ultimately leading to a loss of independence and causing a heavy personal toll on the patient and the family. The costs of care of patients with Alzheimer’s disease in 2010 were estimated at more than $172 billion in the United States, an annual cost that is predicted to increase to a trillion dollars by 2050 unless disease-modifying treatments are developed.1
Alzheimer’s disease has been hypothesized to begin decades before the first symptoms manifest. 2–4 Thus, longitudinal studies of Alzheimer’s disease biomarkers take many years to show the full pathologic cascade of events that lead to dementia. Furthermore, trials of disease-modifying treatment require large numbers of patients over extended periods owing to the slow progression of cognitive symptoms.5,6 Therefore, well-validated biomarkers of Alzheimer’s disease processes are needed to improve the design of clinical trials, develop more effective therapeutics, and offer the opportunity for prevention trials.7
On the basis of the amyloid hypothesis,8 amyloid-beta (Aβ) is currently the most common disease-modifying target. Recent research indicates that the targeting of amyloidosis in familial amyloid polyneuropathy improves clinical outcomes.9–11 However, the order and timing of amyloidosis and other Alzheimer’s disease processes that lead to clinical dementia are not well understood. We hypothesized that autosomal dominant Alzheimer’s disease and the more common late-onset Alzheimer’s disease12 have similar pathophysiological features. Although autosomal dominant Alzheimer’s disease accounts for a relatively small proportion (approximately 1%) of cases of Alzheimer’s disease, increasing evidence13 suggests that it overlaps with sporadic Alzheimer’s disease. Mutations in one of three genes (APP, PSEN1, and PSEN2) have been identified that cause alterations in Aβ processing and lead to Alzheimer’s disease with complete penetrance. The age at clinical onset of autosomal dominant Alzheimer’s disease is similar between generations14 and is affected mostly by the mutation type and background family genetics.15 We compared a wide range of pathophysiological markers between mutation carriers and noncarriers as a function of the parental age at onset in order to evaluate the cascade of events that lead to dementia. Clinical, cognitive, imaging, and biochemical measures were compared between mutation carriers and noncarriers in the first large international cohort of families with autosomal dominant Alzheimer’s disease.
METHODS
STUDY DESIGN
Participants at risk for carrying a mutation for autosomal dominant Alzheimer’s disease were enrolled in the Dominantly Inherited Alzheimer Network (DIAN) study at 1 of 10 sites. Each participant was a member of a pedigree with a known mutation for autosomal dominant Alzheimer’s disease. DIAN participants are assessed at baseline and in subsequent years with comprehensive clinical, cognitive, imaging, and biochemical assessments. Data from all 128 participants who were enrolled and who had completed baseline assessments between January 26, 2009, and the first data-cutoff point (April 28, 2011) went through quality-control checks and were included in the analysis (see the Methods section in the Supplementary Appendix, available with the full text of this article at NEJM.org). All participants provided written informed consent or assent with proxy consent. All study procedures were approved by the Washington University Human Research Protection Office and the local institutional review boards of the participating sites. All authors vouch for the accuracy of the data and the fidelity of the study to the protocol (available at NEJM.org).
CLINICAL ASSESSMENTS
Participants underwent clinical assessments of cognitive change with the use of the Clinical Dementia Rating (CDR)16 scale, with CDR 0 indicating normal cognitive function, CDR 0.5 very mild impairment, and CDR 1 mild impairment. The DIAN assessments ascertained family history of Alzheimer’s disease and medical history, and participants underwent a physical examination, including a neurologic evaluation (see the study protocol). Clinicians who performed the assessments were not aware of the mutation status of participants. The parental age at onset was determined by a semistructured interview in which family members were asked about the age of first progressive cognitive decline (Fig. S1 in the Supplementary Appendix). Clinical feedback was provided to participants if medically indicated. No other research data, including genetic status, were provided to research participants as part of the study.
NEUROPSYCHOLOGICAL TESTING
Participants underwent a comprehensive battery of neuropsychological tests, but results of only two tests are reported here because of space limitations; both tests are widely used in research on Alzheimer’s disease. The Mini–Mental State Examination (MMSE)17 is a measure of general cognitive function, with scores ranging from 0 (severe impairment) to 30 (no impairment). Story A from the Logical Memory subtest of the Wechsler Memory Scale–Revised18 is a measure of episodic memory. Participants recall as many details as they can from a short story containing 25 bits of information after it is read aloud by the examiner and again after a 30-minute delay, with scores ranging from 0 (no recall) to 25 (complete recall).
BRAIN IMAGING
Volumetric magnetic resonance imaging (MRI) was performed with the use of qualified 3-tesla scanners at each site; initial and ongoing quality control and matching between site scanners were performed according to the Alzheimer’s Disease Neuroimaging Initiative (ADNI) protocol.19 All images were reviewed for image quality and compliance with the acquisition protocol by the ADNI imaging core laboratories. The T1-weighted MRI scans from DIAN participants were processed through FreeSurfer (for details, see the Supplementary Appendix). Images obtained through positron-emission tomography (PET) with the use of fluorodeoxyglucose (FDG) and Pittsburgh compound B (PIB) (FDG-PET and PIB-PET, respectively) were then coregistered with individual MRI images for region-of-interest determination. For each FreeSurfer region of interest, the standardized uptake value ratio (SUVR) was calculated with the use of a hand-drawn reference region encompassing the brain stem. An increased PIB SUVR indicates increased binding to fibrillar amyloid, and a decreased FDG SUVR indicates decreased metabolism.
BIOCHEMICAL ANALYSIS
Cerebrospinal fluid (CSF) and blood were collected in the morning under fasting conditions by means of lumbar puncture and venipuncture, respectively. Samples were shipped on dry ice to the DIAN biomarker core laboratory. Concentrations in the CSF of Aβ1–42, total tau, and tau phosphorylated at threonine 181 were measured by immunoassay (INNOTEST β-Amyloid1–42 and INNO-BIA AlzBio3, Innogenetics), as were levels of plasma Aβ species (Aβ1–40, Aβ1–42, Aβx-40, and Aβx-42) (INNO-BIA Plasma Aβ Forms Multiplex Assay, Innogenetics). All values had to meet quality-control standards, including a coefficient of variation of 25% or less, kit “controls” within the expected range as defined by the manufacturer, and measurement consistency between plates of a common sample that was included in each run.
STATISTICAL ANALYSIS
The estimated years from expected symptom onset were calculated as the age of the participant at the time of the study assessment minus the age of the parent at symptom onset. For example, if the participant’s age was 35 years, and the parent’s age at onset was 45 years, then the estimated years from expected symptom onset would be −10. The parental age at the onset of clinical symptoms was determined by a semistructured interview with the use of all available historical data (Fig. S1 in the Supplementary Appendix). Clinical, cognitive, imaging, and biochemical measures were compared as a function of estimated years from expected symptom onset between mutation carriers and noncarriers. Statistical analyses (see the Supplementary Appendix for details) were conducted with the use of the PROC MIXED procedure in SAS software, version 9.3 (SAS Institute). With each marker treated as a continuous scale, a linear mixed model was used to model each marker as a function of estimated years from expected symptom onset, mutation status (carrier or noncarrier), and apolipoprotein E (APOE) status (positive or negative). Approximate Student’s t-test results derived from the model were used to determine whether marker values differed between mutation carriers and noncarriers at certain age points (Table S4 in the Supplementary Appendix), after adjustment for the correlation among family members. Values for individual participants were not displayed on graphs to protect the confidentiality of the mutation status of participants (e.g., a participant who did not know his or her mutation status could deduce it from individual values of estimated years from expected symptom onset). Figure 2 was generated with the same final models, with the use of the standardized difference between mutation carriers and noncarriers as a function of estimated years from expected symptom onset — that is, the predicted difference at each estimated year from expected symptom onset divided by the standard deviation for clinical, cognitive, imaging, and biochemical measures.
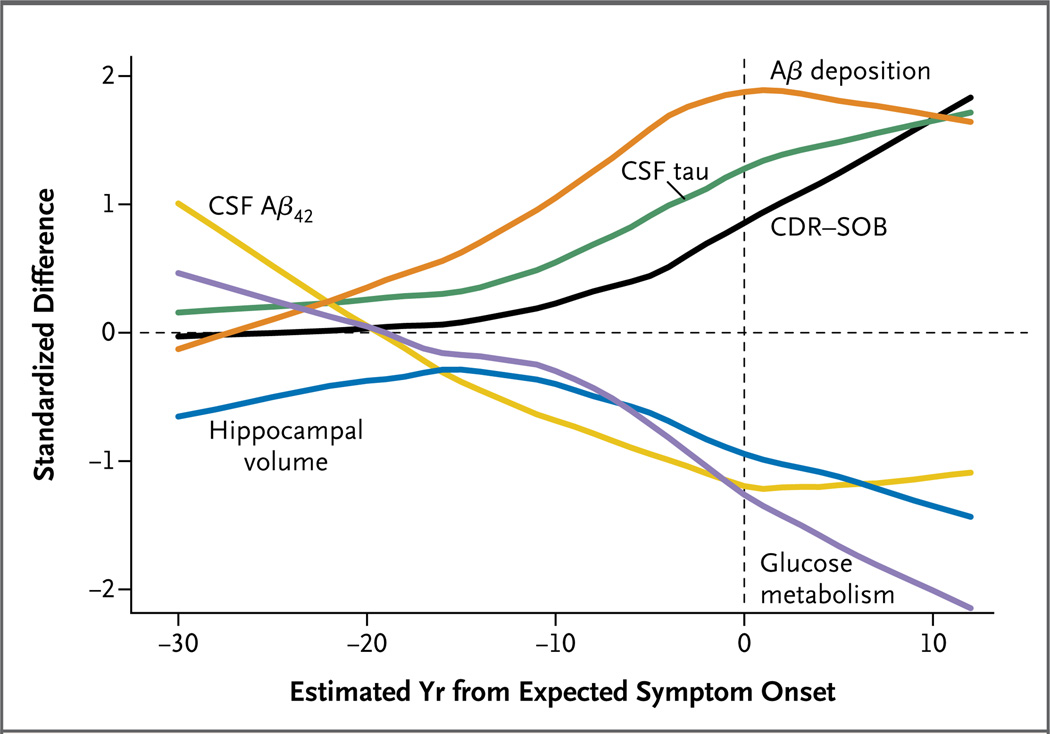
Figure 2. Comparison of Clinical, Cognitive, Structural, Metabolic, and Biochemical Changes as a Function of Estimated Years from Expected Symptom Onset.
The normalized differences between mutation carriers and noncarriers are shown versus estimated years from expected symptom onset and plotted with a fitted curve. The order of differences suggests decreasing Aβ42 in the CSF (CSF Aβ42), followed by fibrillar Aβ deposition, then increased tau in the CSF (CSF tau), followed by hippocampal atrophy and hypometabolism, with cognitive and clinical changes (as measured by the Clinical Dementia Rating–Sum of Boxes [CDR-SOB]) occurring later. Mild dementia (CDR 1) occurred an average of 3.3 years before expected symptom onset. 95% confidence interval bands are shown in Figure S2 in the Supplementary Appendix.
RESULTS
STUDY PARTICIPANTS
We analyzed 128 participants from the DIAN cohort (Table 1). The mutation types reflected the distribution of mutations described in the literature, with 40 PSEN1, 3 PSEN2, and 8 APP pedigrees.20 As expected with an autosomal dominant inheritance pattern, approximately 50% of the asymptomatic participants were mutation carriers. There were no significant differences in the presence of an APOE ε4 allele or sex between asymptomatic mutation carriers and noncarriers. The mean (±SD) age of parental onset of symptoms was 45.7±6.8 years. The DIAN parental age of symptom onset was correlated with the age of symptom onset for symptomatic offspring (Pearson correlation coefficient, 0.56; P<0.001).
Table 1.
Characteristics of the Study Participants.*
| Characteristic | Carriers (N = 88) |
Noncarriers (N = 40) |
P Value |
|---|---|---|---|
| Age — yr | 39.1±10.3 | 39.5±8.9 | 0.92 |
| Male sex — no. (%) | 36 (41) | 17 (42) | 0.85 |
| Education level — yr | 13.9±2.5 | 15.0±2.5 | 0.04 |
| Cognitive status — no. (%)† | |||
| Symptomatic | 43 (49) | 1 (2) | 0.29 |
| Asymptomatic | 45 (51) | 39 (98) | |
| Positive for apolipoprotein E ε4 allele — no. (%) | 22 (25) | 9 (22) | 0.69 |
Plus–minus values are means ±SD.
Participants were defined as asymptomatic if they had Cognitive Dementia Rating scores of 0 (no cognitive decline) and as symptomatic if they had scores greater than 0.
CLINICAL AND NEUROPSYCHOMETRIC FINDINGS
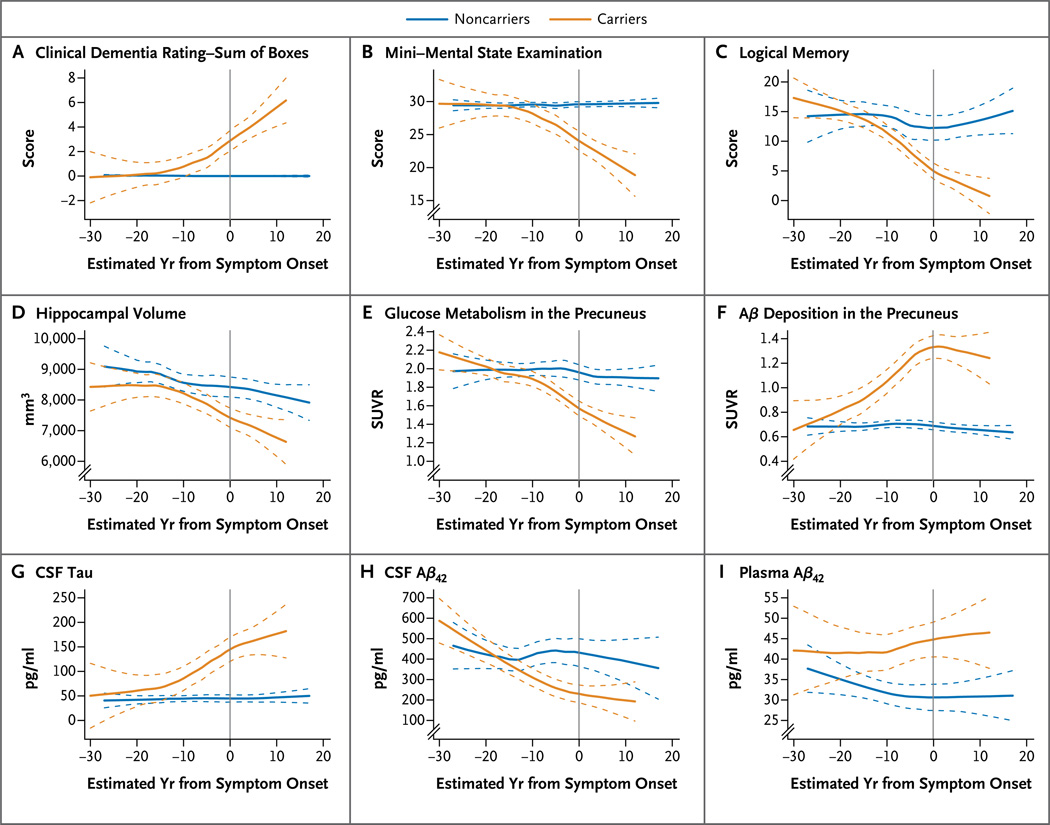
We measured clinical impairment with the use of the Clinical Dementia Rating–Sum of Boxes (CDR-SOB), with scores ranging from 0 (cognitive normality) to 18 (maximal cognitive impairment). Significant differences in CDR-SOB scores were detected between mutation carriers and noncarriers 5 years before expected symptom onset (Fig. 1A and Table 2). Noncarriers had stable CDR-SOB scores of 0 throughout the relative age range, whereas carriers had increasing CDR-SOB scores at higher values of estimated years from expected symptom onset. In this cohort, participants had a CDR rating of mild dementia (CDR 1) at a mean of 3.3±5.3 years after the parent’s age of symptom onset.
Figure 1. Cross-Sectional Analyses of Clinical, Cognitive, Structural, Metabolic, and Biochemical Changes in Autosomal Dominant Alzheimer’s Disease Mutation Carriers versus Noncarriers, According to Estimated Years from Expected Symptom Onset.
The clinical and cognitive measures of the Clinical Dementia Rating–Sum of Boxes (scores range from 0 [cognitive normality] to 18 [maximal cognitive impairment]) (Panel A), the Mini–Mental State Examination (scores range from 0 [severe impairment] to 30 [no impairment]) (Panel B), and the Logical Memory subtest of the Wechsler Memory Scale–Revised (scores range from 0 [no recall] to 25 [complete recall]) (Panel C) showed impaired ratings beginning approximately 5 to 10 years before expected symptom onset. MRI measures of hippocampal volume (Panel D) showed increased brain atrophy approximately 15 years before expected symptom onset. Decreases in cerebral glucose metabolism, as measured by positron-emission tomography (PET) with the use of fluorodeoxyglucose (Panel E), occurred approximately 10 years before expected symptom onset, and deposition of amyloid-beta (Aβ) in the precuneus, as measured by PET with the use of Pittsburgh compound B (Panel F), began approximately 15 to 20 years before expected symptom onset. In the cerebrospinal fluid (CSF), levels of tau protein (Panel G) increased beginning 10 to 15 years before expected symptom onset, and levels of Aβ42 (Panel H) decreased at least 15 years before expected symptom onset. Plasma Aβ42 levels were elevated throughout the range of estimated years from expected symptom onset (Panel I). Dashed lines represent 95% confidence intervals of the fitted curves. SUVR denotes standardized uptake value ratio.
Table 2.
Clinical, Cognitive, Imaging, and Biochemical Estimates in Mutation Carriers and Noncarriers.*
| Variable | Estimated Years from Expected Symptom Onset | |||||||
|---|---|---|---|---|---|---|---|---|
| −25 | −20 | −15 | −10 | −5 | 0 | 5 | 10 | |
| CDR-SOB score (no.)† | ||||||||
| Noncarriers | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Carriers | 0 | 0 | 0.2 | 0.7 | 1.5 | 2.6 | 4.0 | 5.7 |
| Difference | 0±2.2 | 0±1.4 | 0.2±1.1 | 0.7±1.1 | 1.5±1.1‡ | 2.6±1.1§ | 4.0±1.3§ | 5.7±1.7§ |
| MMSE score (no.)¶ | ||||||||
| Noncarriers | 29.4 | 29.5 | 29.5 | 29.5 | 29.6 | 29.6 | 29.6 | 29.7 |
| Carriers | 29.9 | 29.7 | 29.1 | 28.1 | 26.5 | 24.6 | 22.1 | 19.3 |
| Difference | 0.5±4.0 | 0.2±2.5 | −0.4±1.9 | −1.4±1.9 | −3.1±2.0‡ | −5.0±2.0§ | −7.5±2.2§ | −10.4±3.1§ |
| Logical Memory score (no.)‖ | ||||||||
| Noncarriers | 14.7 | 15.6 | 15.1 | 13.9 | 12.5 | 11.3 | 10.8 | 11.7 |
| Carriers | 16.3 | 15.9 | 14.1 | 11.4 | 8.3 | 5.2 | 2.8 | 1.4 |
| Difference | 1.6±4.2 | 0.3±2.7 | −1.0±2.0 | −2.5±2.0** | −4.2±2.2§ | −6.1±2.2§ | −8.0±2.5§ | −10.3±3.7§ |
| Aβ deposition in the precuneus (SUVR ratio)†† | ||||||||
| Noncarriers | 0.69 | 0.69 | 0.69 | 0.70 | 0.70 | 0.69 | 0.68 | 0.67 |
| Carriers | 0.71 | 0.76 | 0.9 | 1.08 | 1.24 | 1.36 | 1.38 | 1.24 |
| Difference | 0.02±0.28 | 0.07±0.17 | 0.21±0.15‡ | 0.38±0.13§ | 0.54±0.12§ | 0.67±0.15§ | 0.70±0.17§ | 0.57±0.21§ |
| Glucose metabolism in the precuneus (SUVR ratio)‡‡ | ||||||||
| Noncarriers | 2.06 | 2.04 | 2.01 | 1.99 | 1.97 | 1.95 | 1.92 | 1.90 |
| Carriers | 2.16 | 2.05 | 1.94 | 1.83 | 1.72 | 1.61 | 1.50 | 1.39 |
| Difference | 0.10±0.16 | 0.01±0.13 | −0.07±0.11 | −0.16±0.09§ | −0.25±0.08§ | −0.34±0.09§ | −0.42±0.12§ | −0.51±0.15§ |
| Total hippocampal volume (mm3) | ||||||||
| Noncarriers | 8999 | 8874 | 8748 | 8622 | 8497 | 8371 | 8245 | 8120 |
| Carriers | 8767 | 8511 | 8255 | 7999 | 7743 | 7486 | 7230 | 6974 |
| Difference | −232±675 | −363±548 | −493±442** | −623±370‡ | −754±356§ | −885±406§ | −1015±500§ | −1146±619§ |
| Aβ42 in the CSF (pg/ml) | ||||||||
| Noncarriers | 454 | 436 | 421 | 410 | 402 | 398 | 397 | 399 |
| Carriers | 532 | 433 | 352 | 289 | 245 | 218 | 210 | 219 |
| Difference | 78±149 | −3±97 | −69±82 | −121±85‡ | −157±88§ | −180±90§ | −187±107‡ | −180±155** |
| Tau in the CSF (pg/ml) | ||||||||
| Noncarriers | 39 | 41 | 42 | 44 | 45 | 47 | 48 | 50 |
| Carriers | 35 | 55 | 76 | 97 | 117 | 138 | 159 | 179 |
| Difference | −4±52 | 14±41 | 34±33** | 53±27§ | 72±27§ | 91±31§ | 111±39§ | 129±50§ |
| Plasma Aβ42 (pg/ml) | ||||||||
| Noncarriers | 37.0 | 34.8 | 33.1 | 31.7 | 30.8 | 30.3 | 30.2 | 30.5 |
| Carriers | 42.4 | 41.8 | 41.6 | 41.9 | 42.5 | 43.5 | 45.0 | 46.9 |
| Difference | 5.4±10.8 | 7.0±8.7 | 8.5±7.0** | 10.2±6.0‡ | 11.7±5.8§ | 13.2±6.8§ | 14.8±8.5§ | 16.4±10.5§ |
The timing of assessments was defined on the basis of the estimated years from expected symptom onset, calculated as the age of the participant at assessment minus the age of the parent at symptom onset. Estimates are reported with 95% confidence intervals for the difference between mutation carriers and noncarriers. Estimates were obtained with use of a mixed model that treated mutation status (noncarrier or carrier), estimated year from expected symptom onset (or higher-order term), and interactions between mutation status and estimated year from expected symptom onset as covariates regardless of the participant’s score on the Clinical Dementia Rating–Sum of Boxes (CDR-SOB) (Table S3 in the Supplementary Appendix). CSF denotes cerebrospinal fluid, and SUVR standardized uptake value ratio.
Scores on the CDR-SOB range from 0 (cognitive normality) to 18 (maximal cognitive impairment).
P<0.01.
P<0.001.
Scores on the Mini–Mental State Examination (MMSE) range from 0 (severe impairment) to 30 (no impairment). A score higher than 27 is considered normal.
Scores on the Logical Memory subtest of the Wechsler Memory Scale–Revised range from 0 (no recall) to 25 (complete recall).
P<0.05.
Deposition of amyloid-beta (Aβ) in the precuneus was measured by positron-emission tomography (PET) with the use of Pittsburgh compound B (PIB). A higher SUVR indicates greater binding of PIB to fibrillar amyloid.
Glucose metabolism in the precuneus was measured by PET with the use of fluorodeoxyglucose. A lower SUVR indicates lower metabolism.
Significant differences in MMSE scores between mutation carriers and noncarriers were detected at assessments performed 5 years before expected symptom onset; carriers had decreasing MMSE scores at higher values of estimated years from expected symptom onset (Fig. 1B). We found significant cognitive impairment in mutation carriers, as compared with noncarriers, in the delayed-recall portion of the Logical Memory test21 10 years before expected symptom onset (Table 2). Noncarriers remained stable in performance from 30 years before to 20 years after expected symptom onset (Fig. 1C).
BRAIN ATROPHY
MRI structural measures of hippocampal volume were compared between mutation carriers and noncarriers with the use of an a priori hypothesis of increased atrophy in mutation carriers. Increased atrophy of bilateral hippocampi was detected in mutation carriers 15 years before expected symptom onset (Table 2). As expected, there was an age-dependent decrease in hippocampal volumes in noncarriers (Fig. 1D).22
CEREBRAL GLUCOSE METABOLISM
FDG-PET measures of cerebral glucose use in the precuneus were compared with the use of an a priori hypothesis of decreased metabolism in mutation carriers to determine regional metabolic defects. The precuneus region, which is known to be an area of early deposition in both sporadic Alzheimer’s disease and autosomal dominant Alzheimer’s disease,4,23,24 was chosen for analysis of amyloid deposition. A significant decrease in cerebral metabolism in the precuneus was detected in mutation carriers 10 years before expected symptom onset (Fig. 1E and Table 2).
Aβ DEPOSITION
PIB-PET measures of fibrillar Aβ deposition25 in the precuneus were compared with the use of an a priori hypothesis of increased regional amounts of amyloid deposition in mutation carriers. There was no detectable amyloid deposition in noncarriers. All noncarriers had PIB-PET SUVR values of less than 0.88. As compared with noncarriers, mutation carriers had significant amyloid deposition in the precuneus 15 years before expected symptom onset (Fig. 1F and Table 2). The amount of amyloid deposition in mutation carriers increased as a function of estimated years from expected symptom onset at least until clinical symptom onset.
BIOCHEMICAL MEASURES
In mutation carriers, levels of tau in the CSF were increased 15 years before expected symptom onset (Fig. 1G and Table 2). Concentrations of Aβ42 in the CSF decreased as a function of estimated years from expected symptom onset and were pseudonormal at approximately 20 years before expected symptom onset, reaching low levels 10 years before expected symptom onset (Fig. 1H). The decrease by half in Aβ42 in the CSF and the increase in tau in the CSF were similar in magnitude to those typically observed in late-onset sporadic Alzheimer’s disease.26 Plasma Aβ42 levels were elevated in mutation carriers, as compared with noncarriers (Fig. 1I).
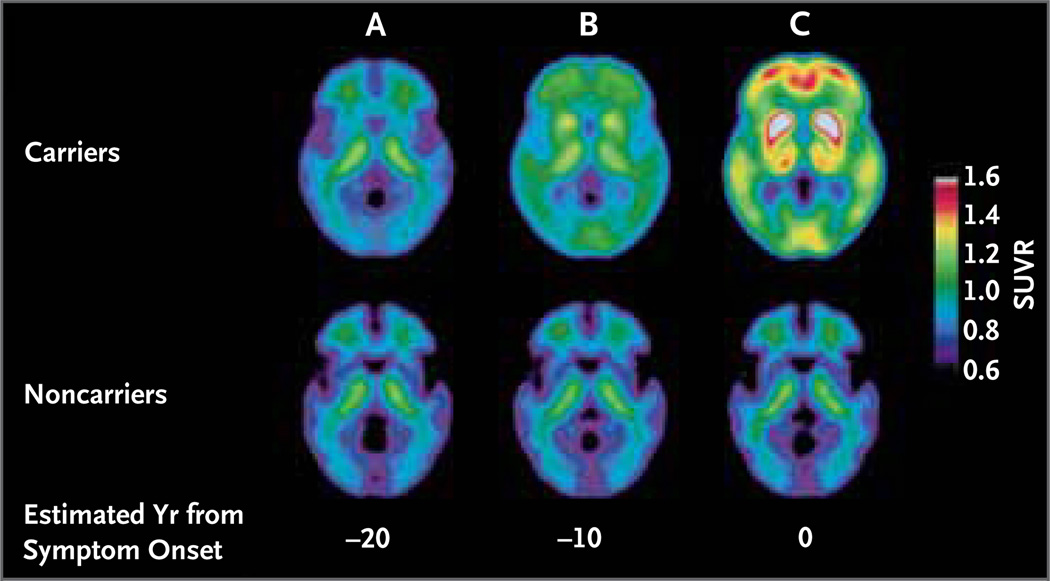
COMBINED MODEL
The order and rate of pathophysiological changes in autosomal dominant Alzheimer’s disease were estimated with the use of an analysis of the relationship among clinical, cognitive, imaging, and biochemical measures in the DIAN cohort (Fig. 2). Beginning 25 years before expected symptom onset, Aβ42 concentrations in the CSF in mutation carriers appeared to decline, as compared with those in noncarriers. Aβ deposition as measured by PIB-PET (Fig. 3; and see Video 1, available at NEJM.org) was detected at least 15 years before expected symptom onset (Table 2). Increases in levels of tau in the CSF and in brain atrophy were detected approximately 15 years before expected symptom onset, followed by cerebral hypometabolism and impaired episodic memory approximately 10 years before expected symptom onset and global cognitive impairment starting at 5 years before expected symptom onset.
Figure 3. Aβ Deposition in Autosomal Dominant Alzheimer’s Disease Years before Expected Clinical Symptoms.
Panel A compares the fibrillar Aβ deposition, as measured by PET with the use of Pittsburgh compound B (PIB), of the average of autosomal dominant Alzheimer’s disease mutation carriers and noncarriers 20 years before the estimated time of onset of symptoms. There was significant Aβ deposition in the caudate and cortex in mutation carriers more than 10 years before expected symptom onset, as compared with noncarriers (Panel B). Panel C shows additional Aβ deposition throughout the cortex and neostriatum at the estimated time of symptom onset. An increased SUVR indicates increased binding of PIB to fibrillar amyloid. The scale ranges from low SUVR values (bluer colors), indicating low amounts of amyloid, to high SUVR values (redder colors), indicating high amounts of amyloid.
DISCUSSION
Previous studies of autosomal dominant Alzheimer’s disease have showed hippocampal atrophy,27 fibrillar amyloidosis,28 and biochemical abnormalities in the CSF.29 With the establishment of DIAN, a worldwide network of autosomal dominant Alzheimer’s disease centers, we have estimated the timing and order of changes in autosomal dominant Alzheimer’s disease in a large cohort with the disease. Changes begin in the brain at least two decades before the estimated onset of clinical symptoms. With the use of estimates of years from expected symptom onset, the order and magnitude of changes indicate that genetic mutations cause increased Aβ42, which is followed by brain amyloidosis, tauopathy, brain atrophy, and decreased glucose metabolism. After these biologic changes, cognitive impairment can be detected, which culminates in clinical impairment and eventually dementia. These findings suggest that the diagnosis of clinical dementia is made late in the course of the biologic cascade of autosomal dominant Alzheimer’s disease.
The estimated year from expected symptom onset normalizes the stage of disease on the basis of the parental age of onset. Our findings suggest that once initiated, Alzheimer’s disease processes are likely independent of absolute age but rather depend on the start of processes such as Aβ misfolding and other modulating factors. Furthermore, other findings suggest that amyloid deposition probably occurs years or decades before dementia symptoms are manifest in sporadic Alzheimer’s disease.24 Previous cross-sectional studies in sporadic Alzheimer’s disease have suggested a series of changes that lead to clinical disease.2 Our results support the hypothesis of a pathophysiological cascade and suggest the possibility of a common pathophysiology between autosomal dominant Alzheimer’s disease and the much more common “sporadic” form.
A strength of this study is that it shows relative changes in Alzheimer’s disease processes that occur over a period of four decades. However, interpretations of the results are not certain, because the current analyses are based on cross-sectional data, which do not represent individual longitudinal changes. In addition, although many of our findings in autosomal dominant Alzheimer’s disease are similar to findings in sporadic Alzheimer’s disease, there were some differences. For example, trends for increased levels of Aβ42 in the CSF have not been reported in sporadic Alzheimer’s disease or autosomal dominant Alzheimer’s disease, although this trend was predicted in autosomal dominant Alzheimer’s disease, because familial Alzheimer’s disease mutations cause increased Aβ or Aβ42 production.30 Furthermore, unlike sporadic Alzheimer’s disease, autosomal dominant Alzheimer’s disease typically presents with early and pronounced PIB-PET signaling in the neostriatum.28 Although the findings of this study were largely based on PSEN1 mutations, a comparison with PSEN2 and APP mutations (Table S2 in the Supplementary Appendix) suggests no differences in results among the mutation gene types. Owing to the younger age of the cohort, the prevalence of confounders such as vascular risk factors was low (<15%) in this cohort and not significantly different between carriers and noncarriers. Although the clinical and pathologic phenotypes of dominantly inherited Alzheimer’s disease are similar to those of sporadic Alzheimer’s disease, the generalizability of the nature and sequence of brain changes in autosomal dominant Alzheimer’s disease remains to be determined for sporadic Alzheimer’s disease.
The definition of the timing and magnitude of pathophysiological changes associated with Alzheimer’s disease has implications for the development and implementation of diagnostic and predictive tests and the design of prevention trials. 31 For example, our data suggest that amyloid deposition will develop and be detectable in all persons with a mutation while still asymptomatic, whereas no noncarriers had positive scans for amyloid deposition. If autosomal dominant Alzheimer’s disease is similar to late-onset Alzheimer’s disease, this finding suggests that Alzheimer’s dementia will eventually develop in persons with positive scans for amyloid deposition. These findings suggest that the targeting of Aβ earlier in the course of the disease may provide better clinical outcomes than the treatment of mild to moderate dementia after substantial neuronal and synaptic loss has occurred.32
In summary, our findings indicate that the Alzheimer’s disease process begins more than 20 years before the clinical onset of dementia. Treatment and prevention trials can incorporate these pathophysiological changes to gauge the likelihood of future clinical success. Secondary prevention trials that are designed to prevent or delay cognitive and clinical impairment may ultimately test the amyloid hypothesis, just as the cholesterol hypothesis of heart disease was tested three decades ago.33
Supplementary Material
Acknowledgments
Supported by the National Institute on Aging and a private nonprofit foundation (see disclosure at NEJM.org).
We thank the participants and their families for their altruism; the DIAN research and support staff at each of the participating sites for their contributions to this study; and Martha Storandt for input and revisions to an earlier draft of the manuscript.
Appendix
The authors’ affiliations are as follows: the Departments of Neurology (R.J.B., A.M.F., D.M.H., A.S., V.B., A.O., K.M., J.C.M.), Biostatistics (C.X., X.X.), Psychiatry (A.G.), Radiology (T.L.S.B., D.S.M., T.M.B.), and Pathology and Immunology (N.J.C.), Washington University School of Medicine, St. Louis; University College London Institute of Neurology, London (N.C.F., M.N.R.); the Department of Neurosciences, University of California, San Diego, La Jolla (P.S.A.); the Department of Pathology and Laboratory Medicine, Indiana University School of Medicine, Indianapolis (B.G.); the Departments of Psychiatry (W.E.K.) and Neurology (W.E.K., E.M.), University of Pittsburgh School of Medicine, Pittsburgh; the Centre of Excellence for Alzheimer’s Disease Research and Care, Edith Cowan University, Joondalup, WA (R.N.M.), the Mental Health Research Institute, University of Melbourne, Melbourne, VIC (C.L.M.), and Neuroscience Research Australia and the School of Medical Sciences, University of New South Wales, Sydney (P.R.S.) — all in Australia; the Taub Institute for Research on Alzheimer’s Disease and the Aging Brain and the Department of Neurology, Columbia University College of Physicians and Surgeons, New York (R.M.); the Department of Neurology, David Geffen School of Medicine, University of California, Los Angeles, Los Angeles (J.M.R.); the Center for Alzheimer Research and Treatment and the Department of Neurology, Brigham and Women’s Hospital, Massachusetts General Hospital, and Harvard Medical School (R.A.S.) — all in Boston; and the Department of Neurology and the Memory and Aging Program, Butler Hospital, Warren Alpert Medical School of Brown University, Providence, RI (S.S.).
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
REFERENCES
- 1.Brookmeyer R, Evans DA, Hebert L, et al. National estimates of the prevalence of Alzheimer’s disease in the United States. Alzheimers Dement. 2011;7:61–73. doi: 10.1016/j.jalz.2010.11.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jack CR, Jr, Knopman DS, Jagust WJ, et al. Hypothetical model of dynamic biomarkers of the Alzheimer’s pathological cascade. Lancet Neurol. 2010;9:119–128. doi: 10.1016/S1474-4422(09)70299-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Price JL, Morris JC. Tangles and plaques in nondemented aging and “preclinical” Alzheimer’s disease. Ann Neurol. 1999;45:358–368. doi: 10.1002/1531-8249(199903)45:3<358::aid-ana12>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 4.Braak H, Braak E. Frequency of stages of Alzheimer-related lesions in different age categories. Neurobiol Aging. 1997;18:351–357. doi: 10.1016/s0197-4580(97)00056-0. [DOI] [PubMed] [Google Scholar]
- 5.Bapineuzumab in patients with mild to moderate Alzheimer’s disease (ApoE4 non-carrier) ClinicalTrials.gov. 2007 ( http://clinicaltrials.gov/ct2/show/NCT00574132).
- 6.Effect of LY2062430 on the progression of Alzheimer’s disease (EXPEDITION) ClinicalTrials.gov. 2009 ( http://clinicaltrials.gov/ct2/show/NCT00905372).
- 7.Bateman RJ, Aisen PS, De Strooper B, et al. Autosomal-dominant Alzheimer’s disease: a review and proposal for the prevention of Alzheimer’s disease. Alzheimers Res Ther. 2011;3:1. doi: 10.1186/alzrt59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hardy J, Selkoe DJ. The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics. Science. 2002;297:353–356. doi: 10.1126/science.1072994. [Erratum, Science 2002;297:2209.] [DOI] [PubMed] [Google Scholar]
- 9.Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349:583–596. doi: 10.1056/NEJMra023144. [DOI] [PubMed] [Google Scholar]
- 10.Summary of opinion (initial authorisation): Vyndaqel. London: European Medicines Agency; 2011. ( http://www.ema.europa.eu/ema/index.jsp?curl=pages/medicines/human/medicines/002294/smops/Positive/human_smop_000246.jsp&mid=WC0b01ac058001d127&murl=menus/medicines/medicines.jsp&jsenabled=true). [Google Scholar]
- 11.Johnson SM, Wiseman RL, Sekijima Y, Green NS, Adamski-Werner SL, Kelly JW. Native state kinetic stabilization as a strategy to ameliorate protein misfolding diseases: a focus on the transthyretin amyloidoses. Acc Chem Res. 2005;38:911–921. doi: 10.1021/ar020073i. [DOI] [PubMed] [Google Scholar]
- 12.Perrin RJ, Fagan AM, Holtzman DM. Multimodal techniques for diagnosis and prognosis of Alzheimer’s disease. Nature. 2009;461:916–922. doi: 10.1038/nature08538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cruchaga C, Chakraverty S, Mayo K, et al. Rare variants in APP, PSEN1 and PSEN2 increase risk for AD in late-onset Alzheimer’s disease families. PLoS One. 2012;7(2):e31039. doi: 10.1371/journal.pone.0031039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lopera F, Ardilla A, Martínez A, et al. Clinical features of early-onset Alzheimer disease in a large kindred with an E280A presenilin-1 mutation. JAMA. 1997;277:793–799. [PubMed] [Google Scholar]
- 15.Wijsman EM, Daw EW, Yu X, et al. APOE and other loci affect age-at-onset in Alzheimer’s disease families with PS2 mutation. Am J Med Genet B Neuropsychiatr Genet. 2005;132B:14–20. doi: 10.1002/ajmg.b.30087. [DOI] [PubMed] [Google Scholar]
- 16.Morris JC, Ernesto C, Schafer K, et al. Clinical dementia rating training and reliability in multicenter studies: the Alzheimer’s Disease Cooperative Study experience. Neurology. 1997;48:1508–1510. doi: 10.1212/wnl.48.6.1508. [DOI] [PubMed] [Google Scholar]
- 17.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state:” a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 18.Wechsler D. WMS-R: Wechsler Memory Scale–Revised: manual. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- 19.Mueller SG, Weiner MW, Thal LJ, et al. The Alzheimer’s disease neuroimaging initiative. Neuroimaging Clin N Am. 2005;15:869–877. doi: 10.1016/j.nic.2005.09.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Alzheimer Disease & Frontotemporal Dementia Mutation Database home page. 2011 ( http://www.molgen.ua.ac.be/ADMutations).
- 21.Morris JC, Weintraub S, Chui HC, et al. The Uniform Data Set (UDS): clinical and cognitive variables and descriptive data from Alzheimer Disease Centers. Alzheimer Dis Assoc Disord. 2006;20:210–216. doi: 10.1097/01.wad.0000213865.09806.92. [DOI] [PubMed] [Google Scholar]
- 22.Jack CR, Jr, Petersen RC, Xu YC, et al. Medial temporal atrophy on MRI in normal aging and very mild Alzheimer’s disease. Neurology. 1997;49:786–794. doi: 10.1212/wnl.49.3.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Minoshima S, Giordani B, Berent S, Frey KA, Foster NL, Kuhl DE. Metabolic reduction in the posterior cingulate cortex in very early Alzheimer’s disease. Ann Neurol. 1997;42:85–94. doi: 10.1002/ana.410420114. [DOI] [PubMed] [Google Scholar]
- 24.Mintun MA, Larossa GN, Sheline YI, et al. [11C]PIB in a nondemented population: potential antecedent marker of Alzheimer disease. Neurology. 2006;67:446–452. doi: 10.1212/01.wnl.0000228230.26044.a4. [DOI] [PubMed] [Google Scholar]
- 25.Klunk WE, Engler H, Nordberg A, et al. Imaging brain amyloid in Alzheimer’s disease with Pittsburgh Compound-B. Ann Neurol. 2004;55:306–319. doi: 10.1002/ana.20009. [DOI] [PubMed] [Google Scholar]
- 26.Fagan AM, Roe CM, Xiong C, Mintun MA, Morris JC, Holtzman DM. Cerebrospinal fluid tau/beta-amyloid(42) ratio as a prediction of cognitive decline in non-demented older adults. Arch Neurol. 2007;64:343–349. doi: 10.1001/archneur.64.3.noc60123. [DOI] [PubMed] [Google Scholar]
- 27.Ridha BH, Barnes J, Bartlett JW, et al. Tracking atrophy progression in familial Alzheimer’s disease: a serial MRI study. Lancet Neurol. 2006;5:828–834. doi: 10.1016/S1474-4422(06)70550-6. [DOI] [PubMed] [Google Scholar]
- 28.Klunk WE, Price JC, Mathis CA, et al. Amyloid deposition begins in the striatum of presenilin-1 mutation carriers from two unrelated pedigrees. J Neurosci. 2007;27:6174–6184. doi: 10.1523/JNEUROSCI.0730-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ringman JM, Younkin SG, Pratico D, et al. Biochemical markers in persons with preclinical familial Alzheimer disease. Neurology. 2008;71:85–92. doi: 10.1212/01.wnl.0000303973.71803.81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gómez-Isla T, Growdon WB, McNamara MJ, et al. The impact of different presenilin 1 and presenilin 2 mutations on amyloid deposition, neurofibrillary changes and neuronal loss in the familial Alzheimer’s disease brain: evidence for other phenotype-modifying factors. Brain. 1999;122:1709–1719. doi: 10.1093/brain/122.9.1709. [DOI] [PubMed] [Google Scholar]
- 31.Sperling RA, Aisen PS, Beckett LA, et al. Toward defining the preclinical stages of Alzheimer’s disease: recommendations from the National Institute on Aging–Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:280–292. doi: 10.1016/j.jalz.2011.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Price JL, Ko AI, Wade MJ, Tsou SK, McKeel DW, Morris JC. Neuron number in the entorhinal cortex and CA1 in preclinical Alzheimer disease. Arch Neurol. 2001;58:1395–1402. doi: 10.1001/archneur.58.9.1395. [DOI] [PubMed] [Google Scholar]
- 33.Yamamoto A, Sudo H, Endo A. Therapeutic effects of ML-236B in primary hypercholesterolemia. Atherosclerosis. 1980;35:259–266. doi: 10.1016/0021-9150(80)90124-0. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.