Abstract
Hyponatremia is the most frequent electrolyte disorder and the syndrome of inappropriate antidiuretic hormone secretion (SIADH) accounts for approximately one-third of all cases. In the diagnosis of SIADH it is important to ascertain the euvolemic state of extracellular fluid volume, both clinically and by laboratory measurements. SIADH should be treated to cure symptoms. While this is undisputed in the presence of grave or advanced symptoms, the clinical role and the indications for treatment in the presence of mild to moderate symptoms are currently unclear. Therapeutic modalities include nonspecific measures and means (fluid restriction, hypertonic saline, urea, demeclocycline), with fluid restriction and hypertonic saline commonly used. Recently vasopressin receptor antagonists, called vaptans, have been introduced as specific and direct therapy of SIADH. Although clinical experience with vaptans is limited at this time, they appear advantageous to patients because there is no need for fluid restriction and the correction of hyponatremia can be achieved comfortably and within a short time. Vaptans also appear to be beneficial for physicians and staff because of their efficiency and reliability. The side effects are thirst, polydipsia and frequency of urination. In any therapy of chronic SIADH it is important to limit the daily increase of serum sodium to less than 8–10 mmol/liter because higher correction rates have been associated with osmotic demyelination. In the case of vaptan treatment, the first 24 h are critical for prevention of an overly rapid correction of hyponatremia and the serum sodium should be measured after 0, 6, 24 and 48 h of treatment. Discontinuation of any vaptan therapy for longer than 5 or 6 days should be monitored to prevent hyponatremic relapse. It may be necessary to taper the vaptan dose or restrict fluid intake or both.
Keywords: antidiuretic hormone, vaptans, hyponatremia, syndrome of inappropriate antidiuretic hormone secretion
Introduction
Routine measurements of the serum sodium concentration became available in the early 1950s. Since that time more than 5000 articles have been published analyzing hyponatremia in various ways. It was found that hyponatremia occurs in many different settings, that it has an incidence of between 4% and 15% in hospital patients and that it is the most frequent electrolyte disorder encountered [Anderson et al. 1985; Goldstein et al. 1983; Hoorn et al. 2006; Miller et al. 1995; Shea et al. 2008; Sherlock et al. 2009; Upadhyay et al. 2006]. Despite this, physicians did not have specific therapy for hyponatremia, until very recently. In the past 5 years, two vasopressin receptor antagonists (intravenous conivaptan; orally available tolvaptan) – collectively called vaptans – have been approved for clinical use in North America and Europe. Therefore hyponatremia and its management are reconsidered in this article. The discussion concentrates on the syndrome of inappropriate antidiuretic hormone secretion (SIADH), sometimes also called ‘Schwartz-Bartter syndrome’), which accounts for approximately one-third of all cases of hyponatremia [Anderson et al. 1985] and is a model abnormality for hyponatremia in general.
What is SIADH?
In a ground-breaking study, Schwartz et al. analyzed the phenomenon of severe hyponatremia in two older male patients under their care, both with advanced pulmonary and cerebral abnormalities – metastases in one patient and cerebromalacia in the other [Schwartz et al. 1957]. The authors were struck by the following features. In both patients, who incidentally had excellent renal function as judged by their high normal values of inulin clearance (120 ml/min) and p-aminohippurate clearance (650 ml/min), even large loads of hypertonic saline solution failed to correct the hyponatremia – except for some transient increase over a few hours – but were followed by quantitative excretion of the infused sodium within a day. Adrenal cortical function was normal and urinary sodium concentration never fell below 40 mmol/liter, except when the patient was on fluid and salt restriction at the same time. The patients’ urine never became maximally dilute (approximately 60–70 mOsm/kg); in fact urinary osmolality was higher than serum osmolality most of the time. Fluid restriction corrected the hyponatremia whereas a liberal fluid intake reintroduced it. These phenomena reminded the authors of features which could be produced by continuous administration of pitressin (a form of vasopressin) and water to normal subjects [Schwartz et al. 1957]. They concluded that ‘sustained inappropriate secretion of antidiuretic hormone’ was responsible for the disorder [Schwartz et al. 1957]. ‘Inappropriate’ was meant to describe the dissociation between antidiuretic hormone (ADH) and osmolality. The cause of this ADH secretion remained obscure [Schwartz et al. 1957].
In the 52 years since then, more details on SIADH – summarized by Ellison and Berl – have been uncovered but the original description and its interpretation have stood the test of time [Ellison and Berl, 2007]. There is now a long list of potential causes of SIADH – presented in Ellison and Berl – in addition to pulmonary carcinoma and brain metastases, including drugs (Table 1), a number of CNS disorders, pulmonary abnormalities, other malignancies, and idiopathic forms. Idiopathic forms appear to be frequent in older patients [Goldstein et al. 1983; Anpalahan, 2001]. The causes of inappropriate ADH are attributable either to paraneoplastic secretion or to ADH from the posterior pituitary and hypothalamus in response to other, so-called ‘nonosmotic’ stimuli [Schrier and Berl, 1975]. SIADH is now no longer a diagnosis merely of exclusion. Instead a well described set of criteria is available to establish the diagnosis affirmatively.
Table 1.
Drugs that may cause SIADH.
| Antidepressant agents (selective serotonin reuptake inhibitors, tricyclic antidepressants)’ |
| Carbamazepine, oxcarbazepine |
| Cyclophosphamide, ifosfamide |
| Hydrochlorothiazide, thiazides |
| Nonsteroidal anti-inflammatory drugs |
| Vincristine |
| Neuroleptic agents |
| Desmopressin (DDAVP, Ferring, Kiel, Germany), vasopressin |
| Oxytocin |
| Chlorpropamide |
| Clofibrate |
SIADH, syndrome of inappropriate antidiuretic hormone secretion.
The patterns of ADH in what seemed to be SIADH have also attracted attention. Several different observations have been made. First, the pattern of ADH secretion in SIADH may show variations that are independent of prevailing serum osmolality (type A) [Robertson, 2006], it may exhibit steady elevation regardless of serum osmolality (type B), or it may show a rather normal looking curve that is shifted to the left (type C, also termed ‘reset osmostat’) [Robertson, 2006; Hoorn et al. 2008]. The different patterns may not just be academic exercises. For example, when patients with reset osmostat (type C) have their hyponatremia corrected they can develop exceptional thirst and this in turn may become a therapeutic obstacle. However, patients with type C SIADH are able to suppress ADH secretion once they reach their left-shifted setpoint of osmolality; this will allow them to excrete water and hence their degree of hyponatremia will be limited to the value corresponding to the osmotic setpoint. The secretory patterns do not show any specific relationship to underlying pathology [Berl and Robertson, 2000].
Second, measurement of ADH in patients with SIADH receiving agents such as carbamazepine, cyclophosphamide or others [Gold et al. 1983] may yield low concentrations of ADH. This has been attributed to direct tubular actions of these drugs [de Braganca et al. 2010], resulting in enhancement of water reabsorption that is not exclusively mediated by ADH. In other words, such patients have typical features of SIADH, but they fail to exhibit inadequate ADH secretion.
Third, in scientific measurements of ADH obtained from patients with SIADH it was found that a small percentage showed no detectable antidiuretic hormone in the plasma. While one possible explanation for this may be related to technical limitations inherent in the available vasopressin assays, recent work has indicated another possible explanation. In some studies it was suggested that gain-of-function mutations of the renal hydro-osmotic vasopressin V-2 receptor exist in some patients, accounting for the clinical features of SIADH without ADH being instrumental in this abnormality [Decaux et al. 2007; Feldmann et al. 2005; Levtchenko and Monnens, 2010].
Lastly, the features of endocrine hyponatremia (as occurs in secondary adrenal insufficiency [Oelkers, 1989] and in advanced hypothyroidism) resemble those of SIADH. Yet both disorders are customarily discussed separately. One reason may be related to observations that intrarenal factors – in addition to vasopressin – are essential for their hyponatremia [Berl and Robertson, 2000]. Another aspect setting them apart is the approach to therapy: it should begin with treatment of the endocrine deficit rather than with measures directed at water metabolism.
Differential diagnosis of SIADH
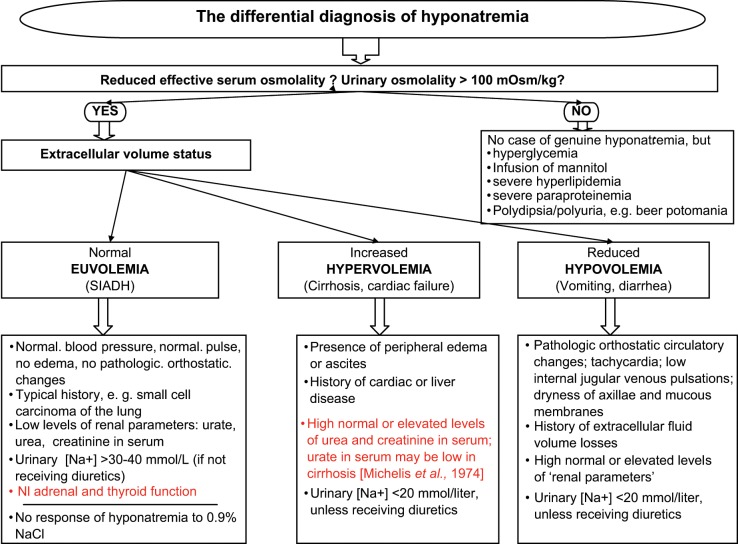
Recent publications have indicated that the diagnosis of SIADH is often missed or made erroneously [Fenske et al. 2010; Hoorn et al. 2006; Huda et al. 2006]. One should carefully follow the steps of differential diagnosis (Figure 1). Clinicians must resist the temptation to take shortcuts because this may result in misdiagnosis. If clinical circumstances dictate an urgent intervention despite available data being incomplete, clinicians should go ahead but review their working diagnosis as soon as all lab data have been reported back.
Figure 1.
Differential diagnosis of SIADH (syndrome of inappropriate antidiuretic hormone secretion).
As shown in Figure 1 and Table 2, it is important to demonstrate a reduced effective serum osmolality in a given hyponatremia to exclude the possibility of normo-osmolar or hyperosmolar hyponatremia. A common circumstance of hyperosmolar hyponatremia is hyperglycemia [Hillier et al. 1999]. Further comments are given in Figure 1 (‘Effective osmolality’ – referring to the parameter that the osmoreceptor appears to register – is measured serum osmolality minus approximately 5 mOsm/kg). A spot urinary osmolality greater than 100 mOsm/kg is considered evidence of the presence of ADH. In other words, patients with polydipsia alone have been described as having hyponatremia and urinary osmolality less than 100 mOsm/kg, but no demonstrable ADH, that is, no ‘SIADH’. In the next step the physical examination and past medical history are used to distinguish between extracellular euvolemia (SIADH), hypervolemia, or hypovolemia of the extracellular fluid volume (Figure 1). Finally the lab work mentioned in the lower sections of Figure 1 should be obtained fully and used to confirm the presence of euvolemia/ hyper-/hypovolemia as shown.
Table 2.
Diagnostic criteria of SIADH (adapted from [Ellison and Berl, 2007]).
| Hyponatremia < 135 mmol/liter together with decreased effective serum osmolality < 275 mOsm/kg |
| Spontaneous urinary osmolality > 100 mOsm/kg |
| Presence of a compatible clinical history, such as brain disorder, pulmonary disease, malignancy, typical drug |
| Absence of edematous disease (cardiac failure, liver cirrhosis, nephrotic syndrome) and of plasma volume depletion (i.e. absence of pathologic orthostatic changes, low internal jugular venous pulses, dryness of axillae) |
| Spontaneous urinary sodium concentration > 40 mmol/liter, unless taking diuretics or on a severe salt restriction |
| Normal adrenal and thyroid function |
| Plasma uric acid < 200 µmol/liter; fractional urate excretion > 12% (normal 5%) [Decaux et al. 1996; Fenske et al. 2008]; plasma urea < 4.5 mmol/liter; plasma creatinine (enzymatically) < 80 µmol/liter |
| Failure to correct hyponatremia by infusion of 0.9% NaCl |
| Successful correction of hyponatremia by fluid restriction |
SIADH, syndrome of inappropriate antidiuretic hormone secretion.
A rare differential diagnosis not mentioned in Figure 1 is cerebral salt wasting (CSW), a condition sometimes seen on neurosurgical wards [Brookes and Gould, 2003; Revilla-Pacheco et al. 2005; Tageja et al. 2009]. Its laboratory constellation resembles SIADH closely, although the spot urinary sodium concentration is usually much greater than 30–40 mmol/liter, sometimes exceeding 150 mmol/liter. Clinically, patients with CSW cannot be subjected to fluid restriction – it would lead to hypovolemia and a dangerous drop in blood pressure. Instead, patients with CSW require infusion of 0.9% or 3% NaCl to maintain blood pressure and circulation within acceptable limits. Cerebral salt wasting is often though not always a transient condition lasting no more than a few days [Lee et al. 2008] and seen in patients after cerebral hemorrhage or neurosurgical interventions.
In clinical practice the distinction between euvolemia and hypovolemia is sometimes more difficult than one would expect. In such situations it can be helpful to infuse 0.9 % NaCl, 0.5–1.0 liters over 12 h [Ellis, 1995], observing any alterations of the serum sodium and the urinary sodium. In euvolemic SIADH serum sodium will not change appreciably in response to 0.9% NaCl, but the urinary sodium will increase. Conversely, in hypovolemic hyponatremia the saline infusion will improve the serum sodium, leaving the urinary sodium more or less unchanged [Ellis, 1995]. A different type of clinical problem may arise from the combined occurrence of two etiologies of hyponatremia at the same time. For example, the patient with SIADH from small cell carcinoma of the lung may develop – in addition – a form of congestive cardiac failure. In such cases the findings (Figure 1) may not clearly conform to what is expected for euvolemia or to that for hypervolemia. If such hyponatremias require a diagnosis, for example to guide therapy, the clinician has to make a decision on what appears to be the leading pathology.
When should we treat hyponatremia? The role of symptoms
An important and interesting yet unclarified question concerns the indications for the treatment of hyponatremia. It is an important one because data indicate an association of general hyponatremia with increased morbidity and mortality [Asadollahi et al. 2006; Callahan et al. 2009; Gill et al. 2006; Heuman et al. 2004; Kim et al. 2008; Klein et al. 2005; Lee and Packer 1986; Waikar et al. 2009; Zilberberg et al. 2008], longer hospitalization [Gill et al. 2006; Wald et al. 2010], osteoporosis [Verbalis et al. 2009], and falls and fractures [Verbalis et al. 2009; Kinsella et al. 2010; Gankam-Kengne et al. 2008]. It is an interesting one because the recent availability of vaptans [Abraham et al. 2006; Berl et al. 2010; Gines et al. 2008; Schrier et al. 2006; Thibonnier et al. 2001; Velez et al. 2010] permits testing for a cause and effect relationship of these associations for the first time. It is an unclarified question since basically no prospective, randomized, controlled trials have been reported. Therapeutic recommendations are largely based on expert opinion [Fenske et al. 2010; Verbalis et al. 2007].
At the present time it is plausible and accepted that therapy should focus on symptoms and findings in hyponatremia [Adrogué, 2005] (Table 3) and not on an isolated low number on a lab slip. In some cases the symptoms or findings will be grave or advanced (Table 3) [Ellis, 1995] and the need for treatment will be obvious beyond any doubt.
Table 3.
Symptoms and findings in hyponatremia [Adrogué, 2005].
| Mild to moderate |
| Headache, lethargy, slowness, poor concentration, depressed mood, lack of attention, impaired memory, nausea, restlessness, instability of gait and falls, muscle cramps, tremor |
| Advanced |
| Confusion, disorientation, somnolence, vomiting, hallucinations, acute psychosis, limb weakness, dysarthria |
| Grave |
| Seizures, hemiplegia, severe somnolence, respiratory insufficiency, coma, death |
However, a much more common clinical situation is that of mild hyponatremia (arbitrarily defined as a serum sodium concentration of 128–134 mmol/liter), in which any associated symptoms may be modest, indistinct, and nonspecific. Many of these patients show symptoms such as forgetfulness, poor concentration, depressed mood, etc., but since they are often older patients the physician has great difficulty attributing the symptomatology to hyponatremia rather than to cerebral sclerosis, social depravation, clinical depression, poor general health, or similar common diagnoses. There are currently no bedside tests that would allow one to distinguish between hyponatremia and other etiologies causing such symptoms. This poses a frequent clinical dilemma. In my experience it is helpful in these cases to give a short trial of treatment to correct or improve hyponatremia. Patients’ symptomatology should be watched closely for any improvements – whether they become more alert and cooperative, concentrate better and are less confused, walk better and fall less, etc. – to appreciate the role of hyponatremia. They should be treated for 3 or 4 days using vaptan tablets or urea powder dissolved in orange juice (see below, section on treatment).
Not only are hyponatremic symptoms often nonspecific and indistinct, there are other cases of mild hyponatremia that seem to be asymptomatic altogether. Renneboog and colleagues studied apparently asymptomatic patients using neurocognitive measurements. The tests were performed twice, once in hyponatremia and then again after it had been corrected [Renneboog et al. 2006]. It was found that chronic ‘asymptomatic’ hyponatremia (126–128 mmol/liter) caused significant reduction (by 10–20%) in the ability to concentrate, memorize, and calculate. In addition, balance and stability of gait were significantly better in normonatremia than in hyponatremia [Renneboog et al. 2006]. This work suggests that ‘asymptomatic hyponatremia’ causes more changes than we realize [Decaux, 2006]. However, in the absence of prospective interventional studies, it does not help to answer the question of whether ‘asymptomatic’ hyponatremia should be treated – or simply observed.
Finally, the depth of any symptoms depends not only on the severity of a given hyponatremia but also on its duration. Acute hyponatremia, that is, lasting less than approximately 48 h, is generally much more symptomatic than chronic hyponatremia.
Treatment of SIADH using general and indirect means
The treatment of SIADH is largely based on expert opinion, not on randomized controlled trials. The agents used were commonly approved for other indications, not for hyponatremia. The only exception to this is vaptan treatment (see below).
A number of indirect modalities have been found helpful in SIADH (Table 4). Fluid restriction that causes a negative fluid balance will increase the serum sodium concentration. To this end daily water intake (oral, intravenous, and metabolic production) must be lowered beyond daily water losses (skin, respiratory tract, stool, urine). If the daily water intake amounts to 2 liters [Gross et al. 1988; Smith et al. 2004] with a fixed urinary osmolality between 350 and 500 mOsm/kg, a reduction of intake by 500 cm3/day may be sufficient to induce a negative water balance. However, if the daily water intake is 1,2 liters with a urinary osmolality of approximately 800 mOsm/kg this intake would be in the range of obligatory losses (skin approx. 400 cm3; respiratory tract approx. 400 cm3; stool approx. 200 cm3; 24 h urine approx. 600 cm3; to be diminished by metabolic water gain of approx. 400 cm3 yielding a total of 1.2 liters/day). In this situation the oral water intake would have to be reduced to 0.5–0.8 liters/day to generate a negative water balance. This may be difficult to tolerate.
Table 4.
Agents and means used in the treatment of SIADH.
| Indirect modalities |
| Fluid restriction |
| Treatment of underlying pathology |
| Hypertonic saline |
| Loop diuretics |
| Urea |
| Democlycline, lithium |
| Hemodialysis, CVVH, SLEDD |
| Direct modalities |
| Vaptan treatment |
CVVH, continuous veno-venous hemofiltration; SIADH, syndrome of inappropriate antidiuretic hormone secretion; SLEDD, slow, low-efficiency daily dialysis.
Some experts have recommended the urine/plasma electrolyte ratio (U-Na + U-K/P-Na) to guide any water restriction [Furst et al. 2000]. If urinary electrolytes are relatively high and the ratio is found to be at least 1.0 they recommend a minimal water intake or none at all, whereas with a ratio of up to 0.5 a water intake of 1 liter/day would amount to a useful water restriction. Although fluid restriction was helpful in the first patients described with SIADH [Schwartz et al. 1957] and is generally recommended [Berl and Robertson, 2000] in everyday practice it may be difficult to impose and frustrating to control.
Whenever possible, treatment of an underlying pathology of SIADH can be expected to correct hyponatremia. For example, if a drug such as hydrochlorothiazide or carbamazepine can be discontinued, or if a Legionella pneumonia causing SIADH is successfully treated, hyponatremia will disappear.
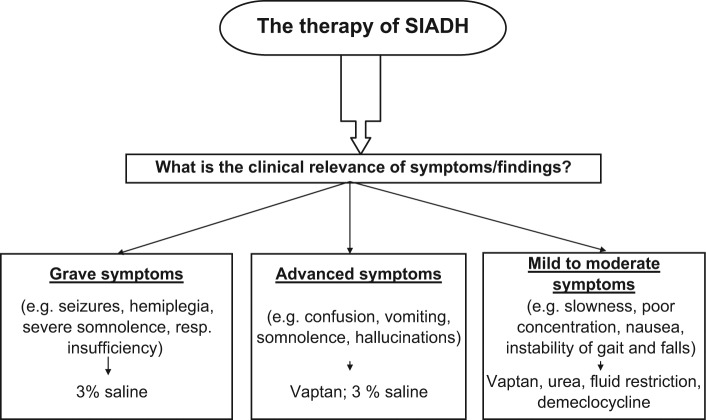
In certain situations (Figure 2) hypertonic saline is used to treat SIADH in hospital [Berl and Robertson, 2000; Mohmand et al. 2007; Sarnaik et al. 1991]. Although any infused NaCl in SIADH will eventually be excreted quantitatively [Schwartz et al. 1957], the kidney is unable to generate urinary sodium concentrations as high as those in 3% saline (>400 mmol/liter) and hence 3% NaCl will improve a given hyponatremia, albeit temporarily. The recommended dosage is 0.5–1.0 ml/kg body weight/h (3% saline) [Berl and Robertson, 2000]. This modality has drawbacks: it may increase the serum sodium too rapidly [Mohmand et al. 2007] and frequent controls are recommended; it may cause pulmonary edema and some experts give prophylactic loop diuretics [Ellison and Berl, 2007]; it cannot be given outside the hospital, that is, by the oral route, because it is impossible to take 20–30 g of NaCl/day in the form of capsules (80–120 capsules of 250 mg each); 3% saline may be unavailable on the drug market and one may have to prepared it oneself (e.g. addition of 91 ml of NaCl 10% to 360 ml of NaCl 0.9% results in 451 ml of NaCl 3%).
Figure 2.
Therapy of SIADH (syndrome of inappropriate antidiuretic hormone secretion).
Loop diuretics induce a copious water diuresis in SIADH [Decaux et al. 1981; Hantman et al. 1973]. Furosemide may be given orally or intravenously in a dosage as high as 10–40 mg/h, with or without replacement of any sodium lost by infusions of 3% saline. Although somewhat cumbersome, these regimens have been used successfully to treat SIADH [Decaux et al. 1981; Hantman et al. 1973].
Urea in dosages of 10–40 g/day results in osmotic diuresis and enhanced water excretion. Urea powder may be obtained from the pharmacy. This modality is very cost effective and has been used to correct hyponatremia in SIADH slowly, by 2–3 mmol/liter/day, a rate comparable to the effect of water restriction [Decaux, 2001; Soupart and Decaux, 2009]. An easy procedure is to dissolve 15–30 g of urea in a glass of orange juice and to administer two or three glasses a day after meals. The drawback of urea is its taste; not all patients will accept it.
Demeclocycline, an antibiotic (600–1200 mg/day), and lithium carbonate, an antidepressant (600–900 mg/day), may both cause nephrogenic diabetes insipidus. This effect has been used to treat the hyponatremia of SIADH [Forrest et al. 1978; Miller et al. 1980; Perks et al. 1979]. However, nephrogenic diabetes insipidus takes 2–4 days to come about, does not occur in all patients receiving these agents, may be associated with renal toxicity (in the case of lithium), and corrects hyponatremia rather slowly by 2–4 mmol/liter/day [Forrest et al. 1978 ]. These drugs are not currently used very often to correct hyponatremia.
In rare medical emergencies more commonly seen in cardiology in the context of hypervolemic severe hyponatremia rather than in SIADH, extracorporeal procedures such as continuous veno-venous hemofiltration (CVVH) and slow, low-efficiency daily dialysis (SLEDD) [Salahudeen et al. 2009] have been used to improve hyponatremia in a controlled manner. These methods are invasive and expensive. They are therefore reserved for exceptional circumstances.
Direct specific treatment of SIADH using vaptans
The modalities of treatment outlined in the previous section are either slow and of low efficiency (fluid restriction, urea, demeclocycline, lithium), unreliable (fluid restriction, demeclocycline, lithium), cumbersome (3% NaCl, loop diuretic, CVVH, SLEDD), or invasive (CVVH, SLEDD). There has been an unmet need for an easy, efficient, specific, titratable therapy for SIADH. Therefore the recent introduction of parenteral (conivaptan) and orally available (tolvaptan) antagonists to the renal V-2 vasopressin receptor – collectively called vaptans – has been considered a breakthrough [Abraham et al. 2006; Berl et al. 2010; Gines et al. 2008; Schrier et al. 2006; Thibonnier et al. 2001; Velez et al. 2010]. (Conivaptan is also an antagonist of the V-1 receptor.) Both agents are approved for the treatment of SIADH in Europe and North America, both have been demonstrated to possess high efficiency in the correction of hyponatremia, both have only minor side effects, and both are not cheap.
Conivaptan was originally developed as an oral preparation [Annane et al. 2009; Ghali et al. 2006] but is now available on the market as intravenous parenteral conivaptan [Velez et al. 2010; Zeltser et al. 2007]. Eligible patients are treated in hospital. An initial loading dose of 20 mg over 30 min is recommended. This is followed by a continuous infusion at a rate of 20 mg/day for up to 4 days. In the reported studies a daily fluid restriction of 1–2 liters was prescribed. This regimen increased the serum sodium from 121.7 to 129.2 mmol/liter within the first 24 h of treatment [Velez et al. 2010]. Lower serum sodium, lower blood urea nitrogen, and higher estimated glomerular filtration rate (eGFR) at baseline were correlated with a larger absolute increase in serum sodium at 24 h. The following adverse events have been noted: infusion site reactions, including thrombophlebitis, postural hypotension, hypotension, mild to moderate increases in blood urea nitrogen or creatinine, and significantly increased thirst [Zeltser et al. 2007]. Four of 42 patients corrected their hyponatremia too fast [Zeltser et al. 2007]. No osmotic demyelination was noted. Overall, conivaptan was judged to be an efficient treatment for hyponatremia of 117–128 mmol/liter, was well tolerated, and had few side effects.
Tolvaptan is available as a tablet, usually taken once a day in the morning [Schrier et al. 2006]. The recommended dosage for SIADH is 15–30 mg/day. Patients receiving tolvaptan should discontinue any previous fluid restriction and drink fluids freely though not excessively. The treatment should be initiated under close supervision by the hospital (as an outpatient or an inpatient) [Schrier et al. 2006]. When given in this way, tolvaptan increased serum sodium from approximately 128 to 136 mmol/liter within 4 days in one study [Schrier et al. 2006]. There is no published experience in patients with serum sodium values less than 120 mmol/liter, however I have personally witnessed cases of SIADH and serum sodium values of 110–120 mmol/liter responding well to the described regimen. Long-term treatment over 1–2 years was also effective and no tachyphylaxis occurred [Berl et al. 2010]. In a self-assessment health status questionnaire the correction of hyponatremia was associated with an improvement in the mental component of the questionnaire [Schrier et al. 2006]. The most common adverse events were thirst, dry mouth, and urinary frequency. Additional adverse events were constipation, nausea, dizziness, weakness, hyperglycemia, and urinary tract infection [Schrier et al. 2006]. An overly rapid correction rate of hyponatremia occurred in 4 of 223 patients [Schrier et al. 2006] and in the long-term study 1 of 111 patients reached hypernatremia. Overall tolvaptan was considered an effective agent that increased serum sodium concentrations in hyponatremia [Schrier et al. 2006] with an acceptable margin of safety [Berl et al. 2010]. It was not reported whether any patients did not respond to tolvaptan and what the cause of such circumstances may have been [Berl et al. 2010; Schrier et al. 2006].
Since the licensing of conivaptan and tolvaptan almost no new information has been published on the use of vaptans in everyday life outside studies [Velez et al. 2010]. In my opinion, vaptans (tolvaptan) represent a step forward for patients with SIADH. They no longer need fluid restriction, the correction of hyponatremia occurs efficiently and quickly, and hospitalization is shorter than with fluid restriction or demeclocycline. Tolvaptan may be continued in outpatients, although the extent and duration of such treatment are not clear. Vaptans (tolvaptan) are also beneficial to physicians treating SIADH. For the first time they have specific agents with predictable and titratable effects at their disposal. However, vaptans are not cheap. An algorithm on the treatment of SIADH is given in Figure 2.
The correction rate and the risk of osmotic demyelination
Central pontine myelinolysis is a pathological condition that has been known about since at least 1959. The clinical features of this syndrome consist of deterioration in the level of consciousness, quadriparesis, dysphagia, mutism, and eventually death [Tomlinson et al. 1976]. It was originally believed to occur as a result of alcoholism, malnutrition, malignancy, or cachexia. In 1976, Tomlinson and colleagues reported two middle-aged women with central pontine and extrapontine myelinolysis with no serious disease other than advanced hyponatremia (96 and 100 mmol/liter), corrected to normal natremia within 2 days, and hypokalemia could be pinpointed [Tomlinson et al. 1976]. Norenberg and colleagues described 12 patients with central pontine myelinolysis and suggested that a too rapid or excessive rise in serum sodium from a hyponatremic baseline was the cause of the disorder [Norenberg et al. 1982]. In their patients the serum sodium concentration had increased by more than 20 mmol/liter within 1–3 days, and most of the patients became mildly hypernatremic during the course of treatment.
Clinical observations have supported this view [Gutenstein, 2007; Sterns, 1987; Sterns et al. 1986, 1994; Tanneau et al. 1994]. Sterns and colleagues reported eight patients with diuretic induced chronic symptomatic hyponatremia, all of whom worsened after rapid correction of their hyponatremia (>12 mmol/liter/day) and developed a neurologic syndrome with pathologic findings of central pontine myelinolysis [Sterns et al. 1986]. In 50 patients with severe chronic hyponatremia corrected at a rate of less than 12 mmol/liter/day there were no neurologic sequelae [Sterns et al. 1986]. A review of the available literature at the time of the report, which recorded cases with diuretic induced hyponatremia and cases with SIADH, also suggested that a correction rate of less than 12 mmol/liter/day was critical to prevention of central pontine myelinolysis [Sterns et al. 1986], also termed ‘osmotic demyelination syndrome’. A survey of 56 hyponatremic cases (<105 mmol/liter) that had received medical care from members of the American Society of Nephrology confirmed these views. In the survey no neurologic complications were observed among patients corrected by less than 12 mmol/liter/day or less than 18 mmol/liter/48 h. Proton magnetic resonance spectroscopy work has demonstrated dramatic changes in cerebral osmolytes in hyponatremia and its correction and these changes may be related to osmotic demyelination [Videen et al. 1995]. In recent experimental work in SIADH-type hyponatremia in rats, minocycline – an inhibitor of microglial activation – was protective against osmotic demyelination [Gankam-Kengne et al. 2010; Kamel and Halperin 2010; Suzuki et al. 2010].
In summary, in symptomatic chronic hyponatremia of SIADH (i.e. hyponatremia lasting longer than 48 h) or in symptomatic hyponatremia of SIADH and unknown duration, most authorities recommend a slow correction rate of less than 0.5 mmol/liter/h and less than 8–10 mmol/liter/24 h with less than 18 mmol/liter/48 h [Ellis, 1995]. In these settings the presence of grave or advanced symptoms justifies the use of a correction rate of 1 mmol/liter/h for a few hours to improve symptoms, as long as the limits for total correction at 24 and 48 h are not exceeded. In patients with severe symptoms and acute SIADH-type hyponatremia (known to have lasted <48 h) a correction rate of 1–2 mmol/liter/h has been recommended to improve the symptoms, but the daily correction rate of 8–10 mmol/liter should still be kept [Adrogué and Madias, 2000; Palmer et al. 2003; Ayus et al. 1987].
Practical considerations of treatment
When saline is used to correct hyponatremia some physicians prefer to calculate the infusion rate needed. One method to accomplish this is provided by the Adrogué–Madias formula (Figure 3). The formula calculates the change in the serum sodium concentration that is expected to result from an infusion of saline solution. By comparing this total change in the serum sodium with the desired rate of correction per hour it is then possible to derive the hourly infusion rate. The formula may underestimate the change in serum sodium actually achieved and this applies to severe hyponatremia (<120 mmol/liter) in particular [Berl, 2007]. Therefore, it is advisable to follow the actual serum sodium closely, for example, every 3 h when infusing various concentrations of saline.
Figure 3.
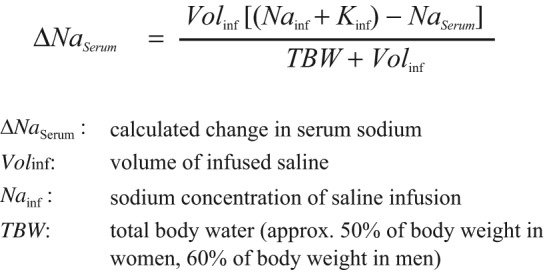
The Adrogué–Madias formula to calculate the change in the serum sodium that can be expected from a saline infusion.
When vaptans are used it is critical to monitor levels for the first 24 h to exclude a too rapid correction rate. Any fluid restriction should be discontinued and drinking encouraged. In my experience it is useful to obtain measurements of the serum sodium concentration at 0, 6, 24, and 48 h of treatment. Any increase in serum sodium of more than 6 mmol/liter by hour 6 of treatment is likely to result in a rise of more than 10 mmol/liter at hour 24. In such cases water should be given orally or intravenously (by infusion, e.g. of 5% dextrose in water (D5W)) at hour 6 of treatment to slow the rate of correction. There is the possibility of a too rapid correction rate in cases of severe hyponatremia (<<120 mmol/liter) and in those with a high eGFR at baseline. It may not always be necessary to continue treatment until a serum sodium concentration of 136 mmol/liter or higher has been achieved; in some patients symptoms will disappear at a serum sodium concentration of 130 mmol/liter.
Finally, discontinuation of therapy deserves attention. After perhaps 5 or 6 days of vaptan therapy the patient may have become used to an increased fluid intake, yet the underlying pathology of SIADH may be persistent. Any sudden discontinuation of a vaptan alone would then risk a relapse into – possibly severe – hyponatremia. To prevent this, natremia should be followed closely. Fluid restriction or a tapering of the vaptan dose (or both) should be used as required.
Footnotes
This review received no special grant from any funding agency in the public, commercial, or not-
Peter Gross has been an investigator in vaptan studies of Wyeth-Ayerst, Astellas, Sanofi and Otsuka. He has given presentations and been on an advisory board for Otsuka.
References
- Abraham W.T., Shamshirsaz A.A., McFann K., Oren R.M., Schrier R.W. (2006) AQuaretic effects of lixivaptan, an oral, non-peptide, selective V2 receptor vasopressin antagonist, in New York association functional class II and III chronic heart failure patients. J Am Coll Cardiol 47: 1615–1621 [DOI] [PubMed] [Google Scholar]
- Adrogué H.J. (2005) Consequences of inadequate management of hyponatremia. Am J Nephrol 25: 240–249 [DOI] [PubMed] [Google Scholar]
- Adrogué H.J., Madias N.E. (2000) Hyponatremia. N Engl J Med 342: 1581–1589 [DOI] [PubMed] [Google Scholar]
- Anderson R.Z., Chung H.M., Kluge R., Schrier R.W. (1985) Hyponatremia: a prospective analysis of its epidemiology and the pathogenetic role of vasopressin. Ann Intern Med 102: 164–168 [DOI] [PubMed] [Google Scholar]
- Annane D., Decaux G., Smith N. (2009) Efficacy and safety of oral conivaptan, a vasopressin-receptor antagonist, evaluated in a randomized, controlled trial in patients with euvolemic or hypervolemic hyponatremia. Am J Med Sci 337: 28–36 [DOI] [PubMed] [Google Scholar]
- Anpalahan M. (2001) Chronic idiopathic hyponatremia in older people due to syndrome of inappropriate antidiuretic hormone secretion (SIADH) possibly related to aging. J Am Geriatrics Soc 49: 788–792 [DOI] [PubMed] [Google Scholar]
- Asadollahi K., Beeching N., Gill G. (2006) Hyponatremia as a risk factor for hospital mortality. Q J Med 99: 877–880 [DOI] [PubMed] [Google Scholar]
- Ayus J.C., Krothapalli R.K., Arieff A.I. (1987) Treatment of symptomatic hyponatremia and its relation to brain damage: a prospective study. N Engl J Med 317: 1190–1195 [DOI] [PubMed] [Google Scholar]
- Berl T. (2007) The Adrogué–Madias formula revisited. Clin J Am Soc Nephrol 2: 1098–1099 [DOI] [PubMed] [Google Scholar]
- Berl T., Quittnat-Pelletier F., Verbalis G., Schrier R.W., Bichet D.G., Ouyang J., et al. (2010) Oral tolvaptan is safe and effective in chronic hyponatremia. J Am Soc Nephrol 21: 705–712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berl T., Robertson G.L. (2000) Pathophysiology of water metabolism. In: Brenner B.M. (ed.), The Kidney. Philadelphia: Saunders, pp; 866–924 [Google Scholar]
- Brookes M.J., Gould T.H. (2003) Cerebral salt wasting syndrome in meningoencephalitis: a case report. J Neurol Neurosurg Psychiatry 74: 277–282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callahan M.A., Do H.T., Caplan D.W., Yoon-Flannery K. (2009) Economic impact of hyponatremia in hospitalized patients: a retrospective cohort study. Postgrad Med 121: 186–191 [DOI] [PubMed] [Google Scholar]
- De Braganca A.C., Moyses Z.P., Magaldi A.Z. (2010) Carbamazepine can induce kidney water absorption by increasing AQuaporin-2 expression. Nephrol Dial Transplant 25: 3840–3845 [DOI] [PubMed] [Google Scholar]
- Decaux G. (2001) Long-term treatment of patients with inappropriate secretion of antidiuretic hormone by the vasopressin receptor antagonist conivaptan, urea, or furosemide. Am J Med 110: 582–584 [DOI] [PubMed] [Google Scholar]
- Decaux G. (2006) Is asymptomatic hyponatremia really asymptomatic? Am J Med 119: 79–82 [DOI] [PubMed] [Google Scholar]
- Decaux G., Namias B., Gulbis B., Soupart A. (1996) Evidence in hyponatremia related to inappropriate secretion of ADH that receptor stimulation contributes to the increase in renal uric acid clearance. J Am Soc Nephrol 7: 805–810 [DOI] [PubMed] [Google Scholar]
- Decaux G., Vandergheynst F., Bouko Y., Parma J., Vassart G., Vilain C. (2007) Nephrogenic syndrome of inappropriate antidiuresis in adults: high phenotypic variability in men and woman from a large pedigree. J Am Soc Nephrol 18: 606–612 [DOI] [PubMed] [Google Scholar]
- Decaux G., Waterlot Y., Genette F., Mockel J. (1981) Treatment of the syndrome of inappropriate secretion of antidiuretic hormone with furosemide. N Engl J Med 304: 329–330 [DOI] [PubMed] [Google Scholar]
- Ellis S.J. (1995) Severe hyponatremia: complications and treatment. Q J Med 88: 905–909 [PubMed] [Google Scholar]
- Ellison D.H., Berl T. (2007) The syndrome of inappropriate antidiuresis. N Engl J Med 356: 2064–2072 [DOI] [PubMed] [Google Scholar]
- Feldmann B.Z., Rosenthal S.M., Vargas G.A., Fenwick R.G., Huang E.A., Matsuda-Abedini M., et al. (2005) Nephrogenic syndrome of inappropriate antidiuresis. N Engl J Med 352: 1884–1890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fenske W., Maier S.K.G., Blechschmidt A., Allolio B., Störk S. (2010) Utility and limitations of the traditional diagnostic approach to hyponatremia: a diagnostic study. Am J Med 123: 652–657 [DOI] [PubMed] [Google Scholar]
- Fenske W., Störk S., Koschker A., Blechschmidt A., Lorenz D., Wortmann S. (2008) Value of fractional uric acid excretion in differential diagnosis of hyponatremic patients on diuretics. J Clin Endocrinol Metab 93: 2991–2997 [DOI] [PubMed] [Google Scholar]
- Forrest J.N., Cox M., Hong C., Morrison G., Bia M., Singer I. (1978) Superiority of demeclocycline over lithium in the treatment of chronic syndrome of inappropriate secretion of antidiuretic hormone. N Engl J Med 298: 173–177 [DOI] [PubMed] [Google Scholar]
- Furst H., Hallows K.R., Post J., Chen S., Kotzker W., Goldfarb S. (2000) The urine/plasma electrolyte ratio: a predictive guide to water restriction. Am J Med Sci 319: 240–244 [DOI] [PubMed] [Google Scholar]
- Gankam Kengne F., Andres C., Sattar L., Melot C., Decaux G. (2008) Mild hyponatremia and risk of fracture in ambulatory elderly. Q J Med 101: 583–588 [DOI] [PubMed] [Google Scholar]
- Gankam-Kengne F., Soupart A., Pochet R., Brion J.P., Decaux G. (2010) Minocycline protects against neurologic complications of rapid correction of hyponatremia. J Am Soc Nephrol 21: 2099–2108 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghali J.K., Koren M.J., Taylor J.R., Brooks-Asplund E., Fan K., Long W.A. (2006) Efficacy and safety of oral conivaptan: a V1A/V2 Vasopressin receptor antagonist, assessed in a randomized, placebo-controlled trial in patients with euvolemic or hypervolemic hyponatremia. J Clin Endocrinol Metab 91: 2145–2152 [DOI] [PubMed] [Google Scholar]
- Gill G., Huda B., Boyd A., Skagen K., Wilet D., Watson I. (2006) Characteristics and mortality of severe hyponatremia – a hospital-based study. Clin Endocrinol 65: 246–249 [DOI] [PubMed] [Google Scholar]
- Gines P., Wong F., Watson H., Milutinovic S., Arbol L.R., Olteanu D. (2008) Effects of satavaptan, a selective vasopressin V2 receptor antagonist, on ascites and serum sodium in cirrhosis with hyponatremia: a randomized trial. Hepatology 48: 204–213 [DOI] [PubMed] [Google Scholar]
- Gold P.W., Robertson G.L., Ballenger J.C., Kaye W., Chen J., Rubinow D.R., et al. (1983) Carbamazepine diminishes the sensitivity of the plasma arginine vasopressin response to osmotic stimulation. J Clin Endocrinol Metab 57: 952–957 [DOI] [PubMed] [Google Scholar]
- Goldstein C.S., Braunstein S., Goldfarb S. (1983) Idiopathic syndrome of inappropriate antidiuretic hormone secretion possibly related to advanced age. Ann Intern Med 99: 185–188 [DOI] [PubMed] [Google Scholar]
- Gross P., Ketteler M., Hausmann C., Reinhard C., Schömig A., Hackenthal E. (1988) Role of diuretics, hormonal derangements, and clinical setting of hyponatremia in medical patients. Klin Wochenschr 66: 662–669 [DOI] [PubMed] [Google Scholar]
- Gutenstein M. (2007) Osmotic myelinolysis syndrome after treatment of severe deamino arginine vasopressin-associated hyponatremia: pitfalls in emergency medicine. Emergency Med Australasia 19: 68–70 [DOI] [PubMed] [Google Scholar]
- Hantman D., Rossier B., Zahlman R., Schrier R. (1973) Rapid correction of hyponatremia in the syndrome of inappropriate secretion of antidiuretic hormone: an alternative treatment to hypertonic saline. Ann Intern Med 78: 870–875 [DOI] [PubMed] [Google Scholar]
- Heuman D.M., Abou-assi S.G., Habib A., Williams L.M., Stravitz R.T., Sanyal A.J., et al. (2004) Persistent ascites and low serum sodium identify patients with cirrhosis and low MELD scores who are at high risk for early death. Hepatology 40: 802–810 [DOI] [PubMed] [Google Scholar]
- Hillier T.A., Abbott R.D., Barrett E.J. (1999) Hyponatremia: evaluating the correction factor for hyperglycemia. Am J Med 106: 399–403 [DOI] [PubMed] [Google Scholar]
- Hoorn E.J., Lindemans J., Zietse R. (2006) Development of severe hyponatremia in hospitalized patients: treatment-related risk factors and inadequate management. Nephrol Dial Transplant 21: 70–76 [DOI] [PubMed] [Google Scholar]
- Hoorn E.J., Swart R.M., Westerink M., van den Dorpel M.A., Berghout A., Bakker J.J. (2008) Hyponatremia due to reset osmostat in dementia with Lewy bodies. J Am Geriatr Soc 56: 567–569 [DOI] [PubMed] [Google Scholar]
- Huda M.S.B., Boyd A., Skagen K., Wile D., van Heyningen C., Watson I., et al. (2006) Investigation and management of severe hyponatremia in a hospital setting. Postgrad Med J 82: 216–219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamel S., Halperin M.L. (2010) Managing overly rapid correction of chronic hyponatremia: an ounce of prevention or a pound of cure? Am Soc Nephrol 21: 2015–2016 [DOI] [PubMed] [Google Scholar]
- Kim W.R., Biggins S.W., Kremers W.D., Wiesner R.H., Kamath P.S., Benson J.T., et al. (2008) Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med 359: 1018–1026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinsella S., Moran S., Sullivan M.O., Molloy M.G.M., Eustace J.A. (2010) Hyponatremia independent of osteoporosis is associated with fracture occurrence. Clin J Am Soc Nephrol 5: 275–280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein L., O’Connor C.M., Leimberger J.D., Gattis-Stough W., Pina I.L., Felker G.M., et al. (2005) Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: results from the outcomes of a prospective trial of intravenous milrinone for exacerbations of chronic heart failure (OPTIME-CHF) study. Circulation 111: 2454–2460 [DOI] [PubMed] [Google Scholar]
- Lee P., Jones G.R.D., Center J.R. (2008) Successful treatment of adult cerebral salt wasting with fludrocortisone. Arch Int Med 168: 325–326 [DOI] [PubMed] [Google Scholar]
- Lee W.H., Packer M. (1986) Prognostic importance of serum sodium concentration and its modification by converting-enzyme inhibition in patients with severe chronic heart failure. Circulation 73: 257–267 [DOI] [PubMed] [Google Scholar]
- Levtchenko E.N., Monnens L.A.H. (2010) Nephrogenic syndrome of inappropriate antidiuresis. Nephrol Dial Transplant 25: 2839–2843 [DOI] [PubMed] [Google Scholar]
- Michelis M.F., Warms P.C., Fusco R.D., Davis B.D. (1974) Hypouricemia and hyperuricosuria in Laennec cirrhosis. Arch Int Med 134: 681–683 [PubMed] [Google Scholar]
- Miller P.D., Linas S.L., Schrier R.W. (1980) Plasma demeclocycline levels and nephrotoxicity. JAMA 243: 2513–2515 [PubMed] [Google Scholar]
- Miller M., Morley J.E., Rubenstein L.Z. (1995) Hyponatremia in a nursing home population. J Am Geriatr Soc 43: 1410–1413 [DOI] [PubMed] [Google Scholar]
- Mohmand H.K., Issa D., Ahmad Z., Cappuccio J.D., Kouides R.W., Sterns R.H. (2007) Hypertonic saline for hyponatremia: risk of inadvertent overcorrection. Clin J Am Soc Nephrol 2: 1110–1117 [DOI] [PubMed] [Google Scholar]
- Norenberg M.D., Leslie K.O., Robertson A.S. (1982) Association between rise in serum sodium and central pontine myelinolysis. Ann Neurol 11: 128–135 [DOI] [PubMed] [Google Scholar]
- Oelkers W. (1989) Hyponatremia and inappropriate secretion of vasopressin (antidiuretic hormone) in patients with hypopituitarism. New Engl J Med 321: 492–496 [DOI] [PubMed] [Google Scholar]
- Palmer B.F., Gates J.R., Lader M. (2003) Causes and management of hyponatremia. Ann Pharmacother 37: 1694–1702 [DOI] [PubMed] [Google Scholar]
- Perks W.H., Walters E.H., Tams I.P., Prowse K. (1979) Demeclocycline in the treatment of the syndrome of inappropriate secretion of antidiuretic hormone. Thorax 34: 324–327 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Renneboog B., Musch W., Vandemergel X., Manto M.U., Decaux G., Hon F. (2006) Mild chronic hyponatremia is associated with falls, unsteadiness, and attention deficits. Am J Med 119: 71.e1–71.e8 [DOI] [PubMed] [Google Scholar]
- Revilla-Pacheco F.R., Herrada-Pineda T., Loyo-Varela M., Modiano-Esquenazi M. (2005) Cerebral salt wasting syndrome in patients with aneurysmal subarachnoid hemorrhage. Neurological Research 27: 418–422 [DOI] [PubMed] [Google Scholar]
- Robertson G.L. (2006) Regulation of arginine vasopressin in the syndrome of inappropriate antidiuresis. Am J Med 119(7 Suppl. 1): 36–42 [DOI] [PubMed] [Google Scholar]
- Salahudeen A.K., Kumar V., Madan N., Xiao L., Lahoti A., Samuels J., et al. (2009) Sustained low efficiency dialysis in the continuous mode (C-SLED): dialysis efficacy, clinical outcomes, and survival predictors in critically I11 cancer patients. Clin J Am Soc Nephrol 4: 1338–1346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarnaik A.P., Meert K., Hackbarth R., Fleischmann L. (1991) Management of hyponatremic seizures in children with hypertonic saline: a safe and effective strategy. Crit Care Med 19: 758–762 [DOI] [PubMed] [Google Scholar]
- Schrier R.W., Berl T. (1975) Nonosmolar factors affecting renal water excretion. N Engl J Med 292: 141–145 [DOI] [PubMed] [Google Scholar]
- Schrier R.W., Gross P., Gheorghiade M., Berl T., Verbalis J.G., Czerwiec F.S., et al. (2006) Tolvaptan, a selective oral vasopressin V2-receptor antagonist, for hyponatremia. N Engl J Med 355: 2099–2112 [DOI] [PubMed] [Google Scholar]
- Schwartz W.B., Bennett W., Curelop S., Bartter F.C. (1957) Syndrome of renal sodium loss and hyponatremia probably resulting from inappropriate secretion of antidiuretic hormone. Am J Med 23: 529–542 [DOI] [PubMed] [Google Scholar]
- Shea A.M., Hammill B.G., Curtis L.H., Szczech L.A., Schulman K.A. (2008) Medical costs of abnormal serum sodium levels. J Am Soc Nephrol 19: 764–770 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherlock M., Sullivan E.O., Agha A., Behan L.A., Owens D., Finucane F., et al. (2009) Incidence and pathophysiology of severe hyponatremia in neurosurgical patients. Postgrad Med J 85: 171–175 [DOI] [PubMed] [Google Scholar]
- Smith D., Moore K., Tormey W., Baylis P.H., Thompson C.J. (2004) Downward resetting of the osmotic threshold for thirst in patients with SIADH. Am J Physiol Endocrinol Metab 287: E1019–E1023 [DOI] [PubMed] [Google Scholar]
- Soupart A., Decaux G. (2009) Efficacy and tolerance of vaptans compared to urea for longterm treatment of patients with SIADH. A prospective study. Acta Clin Belgica 563: 64–66 [Google Scholar]
- Sterns R.H. (1987) Severe symptomatic hyponatremia: treatment and outcome. Ann Intern Med 107: 656–664 [DOI] [PubMed] [Google Scholar]
- Sterns R.H., Cappuccio J.D., Silver S.M., Cohen E.P. (1994) Neurologic sequelae after treatment of severe hyponatremia: a multicenter perspective. J Am Soc Nephrol 4: 1522–1530 [DOI] [PubMed] [Google Scholar]
- Sterns R.H., Riggs J.E., Schochet S.S. (1986) Osmotic demyelination syndrome following correction of hyponatremia. N Engl J Med 314: 535–542 [DOI] [PubMed] [Google Scholar]
- Suzuki H., Sugimura Y., Iwama S., Suzuki H., Nobuaki O., Nasasaki H. (2010) Minocycline prevents osmotic demyelination syndrome by inhibiting the activation of microglia. J Am Soc Nephrol 21: 2090–2098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tageja N., Darden J., Brown L. (2009) Cervical spinal epidural abscess complicated with cerebral salt wasting. Southern Med J 102: 1279–1280 [DOI] [PubMed] [Google Scholar]
- Tanneau R.S., Henry A., Rouhart F., Bourbigot B., Caro B., Mocquard Y., et al. (1994) High incidence of neurologic complications following rapid correction of severe hyponatremia in polydipsic patients. J Clin Psychiatry 55: 349–354 [PubMed] [Google Scholar]
- Thibonnier M., Coles P., Thibonnier A., Shoham M. (2001) The basic and clinical pharmacology of nonpeptide vasopressin receptor antagonists. Annu Rev Pharmacol Toxicol 41: 175–202 [DOI] [PubMed] [Google Scholar]
- Tomlinson B.E., Pierides A.M., Bradley W.G. (1976) Central pontine myelinolysis. Q J Med 179: 373–386 [PubMed] [Google Scholar]
- Upadhyay A., Jaber B.L., Madias N.E. (2006) Incidence and prevalence of hyponatremia. Am J Med 119(7 Suppl. 1): 30–35 [DOI] [PubMed] [Google Scholar]
- Velez J.C.Q., Dopson S.J., Sanders D.S., Delay T.A., Arthur J.M. (2010) Intravenous conivaptan for the treatment of hyponatremia caused by the syndrome of inappropriate secretion of antidiuretic hormone in hospitalized patients: a single-centre experience. Nephrol Dial Transplant 25: 1524–1531 [DOI] [PubMed] [Google Scholar]
- Verbalis J.G., Barsony J., Sugimura Y., Tian Y., Adams D.J., Carter E.A., et al. (2009) Hyponatremia-induced osteoporosis. J Bone Miner Res 25: 554–563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verbalis J.G., Goldsmith S.R., Greenberg A., Schrier R.W., Sterns R.H. (2007) Hyponatremia treatment guidelines 2007: expert panel recommendation. Am J Med 120: 1–21 [DOI] [PubMed] [Google Scholar]
- Videen J.S., Michaelis T., Pinto P., Ross B.D. (1995) Human cerebral osmolytes during chronic hyponatremia. J Clin Invest 95: 788–793 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waikar S.S., Mount D.B., Curhan G.C. (2009) Mortality after hospitalization with mild, moderate, and severe hyponatremia. Am J Med 122: 857–865 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wald R., Jaber B.L., Price L.L., Upadhyay A., Madias N.E. (2010) Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med 170: 294–302 [DOI] [PubMed] [Google Scholar]
- Zeltser D., Rosansky S., van Rensburg H., Verbalis J.G., Smith N. (2007) Assessment of the efficacy and safety of intravenous conivaptan in euvolemic and hypervolemic hyponatremia. Am J Nephrol 27: 447–457 [DOI] [PubMed] [Google Scholar]
- Zilberberg M.D., Exuzides A., Spalding J., Foreman A., Graves Jones A., Colby C., et al. (2008) Epidemiology, clinical and economic outcomes of admission hyponatremia among hospitalized patients. Curr Med Res Opin 24: 1601–1608 [DOI] [PubMed] [Google Scholar]