Abstract
The three currently marketed long-acting insulin analogs, glargine, detemir and insulin lispro protamine suspension (ILPS), represent the most significant advances in basal insulin supplementation since the 1940s and 1950s and the introduction of the intermediate-acting NPH (neutral protamine Hagedorn) insulin. As injection of NPH insulin lacks chronic maintenance of a steady-state low-level basal insulin during fasting periods, which can also expose patients to unpredictable nocturnal hypoglycemia, long-acting insulin analogs have been developed to overcome this important limitation of NPH insulin. ILPS is a protamine-based, intermediate-acting insulin formulation of the short-acting analog insulin lispro: its pharmacokinetic and pharmacodynamic characteristics are quite similar to the other basal insulin analogs glargine and detemir. In recent head-to-head randomized controlled trials of insulin-naïve patients with type 2 diabetes, ILPS achieved similar glycemic control compared with glargine or detemir. ILPS administered once daily is an effective and safe way to maintain a steady-state low-level basal insulin during night time, not dissimilar from that currently obtained with a one-day glargine or detemir administration.
Keywords: detemir, glargine, ILPS (insulin lispro protamine suspension), long-acting insulin analogs
Introduction
Diabetes mellitus is one of the most common chronic diseases in nearly all countries. In 2011 there were 366 million people with diabetes, and this is expected to rise to 552 million by 2030, rendering previous estimates very conservative [Whiting et al. 2011]. Diabetes is one of the main causes of cardiovascular disease, the most common cause of adult blindness, the leading cause of nontraumatic amputation in adults, and diabetic nephropathy is the main driver of renal dialysis [Centers for Disease Control and Prevention, 2009]. From 1980 through 2009, the number of adults in the USA aged 18–79 with newly diagnosed diabetes more than tripled from 493,000 in 1980 to more than 1.8 million in 2009 [Centers for Disease Control and Prevention, 2009]. Moreover, treatment of patients with diabetes and diabetic complications is estimated to cost over US$100 billion each year [Ray et al. 2005].
Tight glycemic control is recommended for all nonpregnant adults with diabetes to minimize the risk of long-term vascular complications [American Diabetes Association, 2012]. Lowering glycosylated hemoglobin A1c (HbA1c) to below or around 7% has been shown to reduce microvascular complications of diabetes, and if implemented soon after the diagnosis of diabetes is associated with long-term reduction in macrovascular disease. Therefore, a reasonable HbA1c goal for many nonpregnant adults is <7% [American Diabetes Association, 2012]. However, aggressive glycemic treatment to reach an HbA1c <7.0% may be inadvisable or impractical in some patients. Treatment must therefore be individualized over time to maintain an appropriate balance between the benefits and risk of good glycemic control, taking into account the specific features of the patient (e.g. the presence or absence of prior cardiovascular disease, duration of diabetes, age, life expectation, comorbidity, etc.) and the agents used (e.g. risk of hypoglycemia). So, more stringent A1C goals (such as ≤6.5%) may be appropriate for patients with short duration of diabetes, long life expectancy, and no significant CVD. On the other hand, less-stringent A1C goals (such as ≥8%) may be appropriate for patients with a history of severe hypoglycemia, limited life expectancy, advanced microvascular or macrovascular complications, extensive comorbid conditions, and longstanding diabetes.
Unfortunately, more than half of individuals with type 2 diabetes are still not at goal. Data from the National Committee for Quality Assurance showed that only about 40% of diabetic patients (both type 1 and type 2) were in good control (HbA1C <7%) in 2009 [National Committee for Quality Assurance, 2010]. In the real diabetic world of 114,249 Italian patients with type 2 diabetes, whose data were collected with electronic medical records at 86 diabetes clinics, 43.1% meet the <7% goal, 27.2% have HbA1c between 7% and 8%, and 29.7% have HbA1c ≥8% [Cimino et al. 2006].
These needs have led to a panoply of new oral antidiabetic drugs for the treatment of type 2 diabetes, and several other unique agents are now in development [Tahrani et al. 2011]. Ultimately, most patients will require insulin therapy. Although traditionally used as a final treatment option, insulin has been recommended as a second-line treatment after lifestyle changes and metformin fail to reach or maintain an HbA1c of <7% in type 2 diabetes [Nathan et al. 2009].
The need for insulin analogs
Insulin has been in use for nearly 90 years, mostly as a treatment to keep alive patients affected by the form we now call type 1 diabetes. Insulin is also increasingly used to treat patients with type 2 diabetes: about 28% of these patients are using insulin in the US [Centers for Disease Control and Prevention, 2007] and a similar percentage (30%) is reported in Italy [The AMD Annals 2009 Working Group, 2009]. However, reluctance to taking insulin among patients and resistance to prescribing insulin among healthcare providers may help explain, in part, why insulin therapy is often postponed in patients who could benefit from it [Karter et al. 2010]. Moreover, the risk of hypoglycemic episodes and weight gain, and the limiting pharmacokinetic and pharmacodynamic features of standard insulins [Hirsch, 2005], may have represented further concerns for delaying insulin therapy. It has been suggested that current uncertainty in medicine regarding diabetes and its treatment may be implicated in clinical inertia, currently defined as ‘failure of health care providers to initiate or intensify therapy when indicated’ [Giugliano and Esposito, 2011].
The chronic maintenance of a steady-state low-level basal insulin during fasting periods represents one major requirement for the appropriate regulation of glucose metabolism. This limitation of native insulin has fuelled the development of long-acting insulin analogs, with the hope of reducing the pharmacological variability of long-acting insulin preparations and simplifying optimal insulin titration in real-life clinical practice. There are currently three different long-acting insulin analogs (insulin glargine, insulin detemir and insulin lispro protamine suspension). Changes to the insulin molecule have focused on the B chain, away from receptor-binding elements. All insulin analogs have been developed through the substitution or addition of amino acids that result in changes to the charge and/or conformation of the insulin molecule at physiological pH.
Insulin lispro protamine suspension
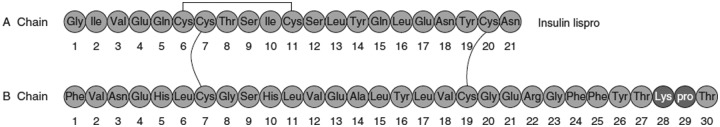
Insulin lispro protamine suspension (ILPS) is a protamine-based, intermediate-acting insulin formulation of the short-acting analog insulin lispro: Insulin lispro (LysB28, ProB29 human insulin) is formed by switching lysine and proline amino acids at positions B28 and B29 (Figure 1). ILPS has been predominantly used as the basal insulin component of currently marketed premixed biphasic formulations to obtain formulations of stable insulin mixtures suitable for 24-h coverage and the control of postprandial glucose concentration while limiting the number of daily injections. In addition to its use in premixed formulations with lispro, the proven stability of the cocrystallization of lispro with protamine in the long term [DeFelippis et al. 1998] determines a better reproducibility of the pharmacological effect. This has also led to the development of ILPS as insulin analog for basal coverage in diabetic patients. ILPS has recently been made available in Italy, Spain and Japan.
Figure 1.
The short-acting insulin analog insulin lispro (LysB28, ProB29 human insulin) is formed by switching lysine and proline amino acids at positions B28 and B29.
In patients with type 2 diabetes [Hompesch et al. 2009], the duration of glucose lowering activity of a single ILPS 0.8 U/kg dose was >23 h and did not differ from that observed with insulin glargine and insulin detemir. Compared with the other two types of insulin analogs, ILPS showed significantly greater glucose-lowering activity and earlier maximum pharmacodynamic response (based on glucose infusion rate). ILPS also exhibited dose-dependent increases in both pharmacokinetic and pharmacodynamic parameters across the dose range of 0.4–1.2 U/kg, consistent with the apparent dose-dependent increase in the mean estimate of duration of action. Another study [Ocheltree et al. 2010] showed that treatment with ILPS was associated with a lower pharmacodynamic intrasubject variability, a more rapid onset of action, greater glucose-lowering activity and greater exposure than that of glargine given at a single equivalent dose, although glargine showed a flatter glucose infusion rate (GIR) time profile.
Does ILPS have clinical advantages over neutral protamine Hagedorn insulin?
Neutral protamine Hagedorn (NPH) insulin often falls short of providing an appropriate basal insulin because of variable absorption, undesirable peaks in hypoglycemia and insufficient duration of action (including peaks and troughs in glucose excursions) [Bolli et al. 1999]. A recent meta-analysis of five open-label studies [Home et al. 2010] based on individual patient data comparing once-daily evening regimens of glargine and NPH in people with type 2 diabetes (2711 people, 1335 using glargine and 1376 NPH) found that the risk of nocturnal hypoglycemia was reduced approximately by half with glargine compared with NPH (odds ratio 0.44–0.52, p < 0.001). Apart from the theoretical consideration that long-acting insulin analogs with quite similar pharmacokinetic and pharmacodynamic characteristics are likely to share the same clinical efficacy (see below), there is also direct evidence for clinical advantages of ILPS over NPH.
Some studies compared the effects on glucose parameters of two different insulin lispro and ILPS premixed formulations (25/75) with those of regular insulin/NPH combinations in patients with type 2 diabetes. Compared with regular insulin/NPH 30/70, twice-daily administration of lispro/ILPS 25/75 resulted in improved post-prandial glycemia after the main meals and overall glycemic control, and in less nocturnal hypoglycemia, without an increase in exercise-induced hypoglycemia [Roach et al. 1999; Herz et al. 2002].
Two Italian uncontrolled clinical trials have examined patients with type 2 diabetes switched to ILPS from a previous treatment with NPH insulin. The first study [Settembrini and Piccolo, 2007] evaluated diabetic patients treated for more than 1 year with NPH insulin at bedtime plus regular human insulin, three times/day, and then switched to ILPS, at bedtime, plus either human regular insulin or lispro three times/day: the switching was associated with statistically significant reductions in HbA1c and fasting glucose in both groups at 3 months of follow up, and with a reduction in the incidence of hypoglycemic events, both symptomatic and asymptomatic.
The second study [Galeone et al. 2008] evaluated diabetic patients treated with bedtime NPH insulin and oral antidiabetic agents for at least 1 year, and then switched to bedtime ILPS at the same dose, without changing the oral diabetic therapy. At follow up of 3 and 6 months, significant reduction in HbA1c, fasting glucose and daily and nocturnal hypoglycemia were recorded. Although interesting, these results should be viewed in the context of uncontrolled clinical studies.
Comparison of ILPS with other long-acting analogs
In recent randomized controlled trials of insulin-naïve patients with type 2 diabetes (Table 1), ILPS achieved similar glycemic control compared with other basal insulin analogs [Esposito et al. 2008; Fogelfeld et al. 2010; Strojek et al. 2010; Arakaki et al. 2010]. The 24-week trial by Fogelfeld and colleagues compared ILPS versus detemir, both administered once or twice daily: ILPS at endpoint was noninferior to insulin detemir in HbA1c change from baseline and in glycemic variability [Fogelfeld et al. 2010]. Patients who received ILPS achieved a significantly lower endpoint HbA1c than those who received detemir with lower insulin doses, thereby indicating that insulin detemir is less potent than ILPS; however, they experienced greater hypoglycemia and weight gain. The differences in weight gain and in the incidence of hypoglycemic episodes were significant in total groups as well as in subgroups taking basal insulin twice daily, whereas patients taking one injection showed no significant difference in weight gain, insulin dose or in the incidence or rates of all hypoglycemias. A significant difference remained in the rates of nocturnal hypoglycemia (episodes/patient), although the incidence of nocturnal hypoglycemia did not differ. For patients treated once daily, both analogs achieved similar HbA1c reductions, and there was no significant difference in overall hypoglycemia (ILPS 65.2%, detemir 71.3% of patients).
Table 1.
Characteristics of the four randomized controlled trials evaluating ILPS versus comparators.
| Studies | Insulin analog | Number of patients | Length weeks | Design of the study | Mean age (years) | Male (%) | OADs | Naive | Start HbA1c | Efficacy HbA1c <7% | Hypoglycemia Events/pt/year | Weight gain (kg) |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Study arms | ||||||||||||
| Esposito et al. [2008] | ILPS | 55 | 36 | R, O, P | 54.9 | 52.7 | Met + Su | Yes | 8.8% | 62% | 7.5 | 2.4 |
| Fogelfeld et al. [2010] | ILPS | 223 | 24 | R, O, P | 56.3 | 50.7 | Su + Met | Yes | 8.8% | 34.9% | 21.5 | 1.88 |
| Strojek et al. [2010] | ILPS | 235 | 24 | R, O, P | 58 | 64 | Met + Su | Yes | 8.67% | 43.8% | 18.1 | 1.04 |
| Arakaki et al. [2010] | ILPS | 171 | 24 | R, O, P | 56 | NA | Met + Su + Ex | Yes | 8.2% | 53.7% | 16.3 | 0.27 |
| Comparator arms | ||||||||||||
| Esposito et al. [2008] | Glargine | 55 | 36 | R, O, P | 53.8 | 50.9 | Met + Su | Yes | 8.7% | 64% | 6.08 | 2.8 |
| Fogelfeld et al. [2010] | Detemir | 219 | 24 | R, O, P | 55.7 | 53.8 | Met + Su | Yes | 8.8% | 31.2% | 18.7 | 0.36 |
| Strojek et al. [2010] | Glargine | 236 | 24 | R, O, P | 57.3 | 62 | Met + Su | Yes | 8.67% | 41.2% | 22.9 | 1.07 |
| Arakaki et al. [2010] | Glargine | 168 | 24 | R, O, P | 56 | NA | Met + Su + Ex | Yes | 8.23% | 52.1% | 18.05 | 0.66 |
OAD, oral antidiabetic drug; R, randomized; O, open; P, parallel; Met, metformin; Su, sulfonylurea; Ex, exenatide; NA, not available; pt, patient.
The results of the study of Fogelfeld and colleagues [Fogelfeld et al. 2010] were somewhat similar to those of the study by Esposito and coworkers [Esposito et al. 2008], in which no significant difference was observed in hypoglycemic events between ILPS and insulin glargine groups. This study was the first to compare the efficacy and safety of ILPS and glargine in patients with type 2 diabetes and unsatisfactory glycemic control while taking one or more antidiabetic drugs. The results of this 36-week study showed a similar glycemic control (HbA1c, fasting plasma glucose levels, eight-points diurnal blood glucose profiles, continuous glucose-monitoring system) with the addition of ILPS or insulin glargine to oral regimens, with a comparable rate of hypoglycemia in the two groups. The average daily dose of ILPS was statistically lower than the glargine dose at endpoint.
The 24-week open-label trial by Strojek and colleagues [Strojek et al. 2010] compared ILPS once or twice daily versus glargine once daily. Glycemic control and overall incidence of hypoglycemia were similar. However, a significantly higher incidence of nocturnal hypoglycemia versus glargine was observed for patients injecting ILPS twice daily, but not for patients injecting ILPS once daily. These results suggest that in the case of once daily injection, ILPS achieves similar glycemic control to glargine or detemir, without increasing the risk of hypoglycemic episodes.
The noninferiority of ILPS versus insulin glargine (both given once daily at bedtime in addition to oral antidiabetic drugs and exenatide) on HbA1c at endpoint was confirmed in a recent 24-week study published as an abstract [Arakaki et al. 2010]. In this study, the effects on fasting plasma glucose and rates of overall and severe hypoglycemia also were comparable in the two groups, although the rate of nocturnal hypoglycemia was higher in ILPS group as compared with glargine groups (4.9 ± 8.4 episodes/patient/year versus 3.01 ± 7.2 episodes/patient/year, p = 0.004).
Finally, the efficacy and safety of ILPS has been compared versus insulin glargine once daily in a basal-bolus regimen [Koivisto et al. 2011]. A total of 383 insulin-treated type 2 diabetic patients were randomized to either ILPS plus lispro or glargine plus lispro in an open-label 24-week European study. Insulin doses were titrated to predefined blood glucose targets. The basal bolus regimen with ILPS once daily resulted in noninferior glycemic control compared with a similar regimen with glargine, without statistically significant or clinically relevant differences in hypoglycemia. No statistically significant or clinically relevant differences between groups were observed in the self-monitoring of blood glucose (SMBG) profile at week 24 and in hypoglycemia rates.
The reasons for a choice
A recent Cochrane review [Swinnen et al. 2011] examined four trials lasting 24–52 weeks involving 2250 people randomized to either insulin detemir or glargine. Insulin glargine was dosed once daily in the evening. Glycemic control, measured by absolute decrease of HbA1c from baseline and HbA1c equal to or less than 7% with or without hypoglycemia, did not differ significantly between treatment groups. Moreover, no significant differences in overall, nocturnal and severe hypoglycemia occurred between treatment groups.
Similarly, the results of the recent studies that compared ILPS with insulin detemir or insulin glargine in patients with type 2 diabetes show non-inferior efficacy results for ILPS versus comparators. ILPS was shown to be more efficacious in terms of HbA1c reduction from baseline than insulin detemir: on the other hand, in patients taking two ILPS injections per day there were more nocturnal hypoglycemic events, as compared with insulin detemir and glargine, and more weight gain, as compared with insulin detemir. All of this supports the usefulness of ILPS for the basal insulin coverage of type 2 diabetic patients no more responding to oral antidiabetic therapy, with an optimal usage as a once-daily (bedtime) injection in terms of balance between glucose-lowering efficacy (more than detemir), hypoglycemic risk (similar to detemir and glargine), daily dosage (lower than detemir and glargine) and body weight (similar to detemir and glargine). So, despite the similarities in the pharmacokinetic and pharmacodynamic profiles, ILPS differs from NPH insulin in clinical behavior, both in terms of effectiveness and safety.
As far as body weight is concerned, an increase in body weight seems an obligate effect of intensified insulin treatment in type 2 diabetes, and it has been quantified in an average annual increase of 4.3 ± 2.74 kg (95% confidence interval [CI] 4.32–4.38), with a correlation with intensity of treatment [Pontiroli et al. 2011]. This association has been quantified from 46 studies, including 14,250 patients treated for 12–52 weeks (mean 27.7 weeks). In a systematic review [Giugliano et al. 2011] of randomized controlled trials that evaluated the effect of insulin regimens (basal, biphasic, prandial and basal bolus) with insulin analogs in patients with type 2 diabetes, we identified 38 arms using basal insulin, with 17,588 patients: weight gain was 1.75 kg (95% CI 1.2–2.1). In particular, in 10 studies weight gain was ≤1 kg, in 18 studies was between 1 and 2 kg, and in the remaining 10 studies was >2 kg.
Conclusions
The three currently marketed long-acting insulin analogs, glargine, detemir and ILPS represent the most significant advances in ‘basal insulin’ supplementation since the 1940s and 1950s and introduction of the intermediate-acting NPH and lente insulin family, respectively. The long-acting insulin analogs are easy to initiate and titrate and can be used in different insulin regimens; however, effective glycemic control can only be achieved with optimal dosing and dose titration. Glargine and ILPS provide the added benefit of once-daily administration, whereas detemir can be used once or twice daily depending on individual needs.
Preliminary results of head-to-head comparisons between ILPS and other basal analogs show an equivalent glycemic control at endpoint, as expressed by change of HbA1c from baseline, without significant differences on weight when used once a day. These results are often linked with a reduced daily dosage when ILPS was administered once daily. Although the results from the current published literature and the preliminary data from some clinical trials show a slightly increased risk of mild diurnal and nocturnal hypoglycemia with ILPS as compared with competitors, this risk seems to be related to the percentage of patients upgrading from once- to twice-daily injections; moreover, the bedtime association of basal insulin analog with evening secretagogues (mainly a sulfonylurea) could have also contribute to the risk of hypo episodes in patients on higher daily dosages. These data from clinical experience are in line with the results from pharmacological studies, which indicate a dose-dependent increase of the pharmacological effect and suggest a once-daily schedule as the best option in clinical practice, in terms of balance between efficacy profile and hypoglycemic risk.
To sum up, ILPS at once daily administration is an effective and safe way to maintain a steady-state low-level basal insulin during night time, not dissimilar from that currently obtained with a one-day glargine administration at bedtime, with lower insulin doses. So, the ideal patient with type 2 diabetes who could benefit from ILPS therapy is a patient with an unsatisfactory glycemic control (HbA1c >7.5%) for at least 3–6 months, on at least two oral drugs (metformin plus a sulfonylurea or another) and who banned the evening secretagogue pill from their regimen when starting ILPS bedtime dose. This phenotypization of the ideal patient having success with ILPS at the lower risk for hypoglycemia and weight gain would help physicians to avoid exposure of type 2 diabetic patients to high glycemic levels over prolonged periods.
Footnotes
This research received no specific grant from any agency in the public, commercial, or not-for-profit sectors.
The authors declare no conflicts of interest in preparing this article
Contributor Information
Dario Giugliano, Department of Geriatrics and Metabolic Diseases, Second University of Naples, Piazza L. Miraglia 2, 80138 Naples, Italy.
Katherine Esposito, Department of Cardiothoracic and Respiratory Sciences, Second University of Naples, Naples, Italy.
References
- American Diabetes Association (2012) Standards of medical care in diabetes - 2012. Diabetes Care 35(Suppl. 1): S11–S63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arakaki R.F., Blevins T.C., Liljenquist D.R., Wise J.K., Jiang H.H., Schneider K.K., et al. (2010) Efficacy and safety of insulin lispro protamine suspension (ILPS) versus insulin glargine (G) added to oral antihyperglycaemic medications and exenatide in patients with type 2 diabetes. Diabetologia 53(Suppl. 1): S556 (abstract). [Google Scholar]
- Bolli G.B., Di Marchi R.D., Park G.D., Proamming S., Koivisto V.A. (1999) Insulin analogues and their potential in the management of diabetes mellitus. Diabetologia 42: 1151–1167 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2007) Atlanta: 2007 National Diabetes Fact Sheet. http://www.cdc.gov/diabetes/pubs/pdf/ndfs_2007.pdf
- Centers for Disease Control and Prevention (2009) Diabetes Data and Trends. http://www.cdc.gov/diabetes/statistics/complications_national.htm (accessed 4 February 2012).
- Cimino A., Giorda C., Meloncelli I., Nicolicci A., Pellegrini F., Rossi M.C., et al. (2006) AMD annals: quality indicators in diabetes care in Italy. http://ebookbrowse.com/2006-annali-amd-ita-pdf-d70659475, p. 30 (accessed 4 February 2012).
- DeFelippis M.R., Bakaysa D.L., Bell M.A., Heady M.A., Li S., Pye S., et al. (1998) Preparation and characterization of a cocrystalline suspension of [LysB28, ProB29]-human insulin analogue. J Pharm Sci 87: 170–176 [DOI] [PubMed] [Google Scholar]
- Esposito K., Ciotola M., Maiorino M.I., Di Palo C., Scognamiglio P., Gicchino M., et al. (2008) Addition of neutral protamine lispro insulin or insulin glargine to oral type 2 diabetes regimens for patients with suboptimal glycemic control: a randomized trial. Ann Intern Med 149: 531–539 [DOI] [PubMed] [Google Scholar]
- Fogelfeld L., Dharmalingam M., Robling K., Jones C., Swanson D., Jacober S. (2010) A randomized, treat-to-target trial comparing insulin lispro protamine suspension and insulin detemir in insulin-naive patients with Type 2 diabetes. Diabetes Med 27: 181–188 [DOI] [PubMed] [Google Scholar]
- Galeane F., Magiar A.V., Viti S. (2008) Valutazione del trattamento bed-time con insulin NPH e NPL nel diabetico tipo 2. CIC Edizioni Internazionali Roma, http://www.gruppocic.com, pp. 3–8
- Giugliano D., Esposito K. (2011) Clinical inertia as a clinical safeguard. JAMA 305: 1591–1592 [DOI] [PubMed] [Google Scholar]
- Giugliano D., Maiorino M.I., Bellastella G., Chiodini P., Esposito K. (2011) Treatment regimens with insulin analogues and haemoglobin A1c target of <7% in type 2 diabetes: a systematic review. Diabetes Res Clin Pract 92: 1–10 [DOI] [PubMed] [Google Scholar]
- Herz M., Profozic V., Arora V., Smircic-Duvnjak L., Koracevic I., Boras J. (2002) Effects of a fixed mixture of 25% insulin lispro and 75% NPL on plasma glucose during and after moderate physical exercise in patients with type 2 diabetes. Curr Med Res Opin 18: 188–193 [DOI] [PubMed] [Google Scholar]
- Hirsch I.B. (2005) Insulin analogues. N Engl J Med 352: 174–183 [DOI] [PubMed] [Google Scholar]
- Home P.D., Fritsche A., Schinzel S., Massi-Benedetti M. (2010) Meta-analysis of individual patient data to assess the risk of hypoglycaemia in people with type 2 diabetes using NPH insulin or insulin glargine. Diabetes Obes Metab 12: 772–779 [DOI] [PubMed] [Google Scholar]
- Hompesch M., Ocheltree S.M., Wondmagegnehu E.T., Morrow L.A., Kollmeier A.P., Campaigne B.N., et al. (2009) Pharmacokinetics and pharmacodynamics of insulin lispro protamine suspension compared with insulin glargine and insulin detemir in type 2 diabetes. Curr Med Res Opin 25: 2679–2687 [DOI] [PubMed] [Google Scholar]
- Karter A.J., Subramanian U., Saha C., Crosson J.C., Parker M.M., Swain B.E., et al. (2010) Barriers to insulin initiation: the translating research into action for diabetes insulin starts project. Diabetes Care 33: 733–735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koivisto V., Cleall S., Pontiroli A.E., Giugliano D. (2011) Comparison of insulin lispro protamine suspension versus insulin glargine once daily in basal-bolus therapies with insulin lispro in type 2 diabetes patients: a prospective randomized open-label trial. Diabetes Obes Metab 13: 1149–1157 [DOI] [PubMed] [Google Scholar]
- Nathan D.M., Buse J., Davidson M.B., Ferrannini E., Holman R.R., Sherwin R., et al. (2009) American diabetes association; European association for the study of diabetes. Management of hyperglycemia in type 2 diabetes: a consensus algorithm for the initiation and adjustment of therapy: a consensus statement from the American diabetes association and the European association for the study of diabetes. Diabetes Care 32: 193–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Committee for Quality Assurance (2010) The State of Health Care Quality 2010 Report. Washington, DC: National Committee for Quality Assurance; Available at: http://www.ncqa.org/portals/0/state%20of%20health%20care/2010/sohc%202010%20-%20full2.pdf (accessed February 2012). [Google Scholar]
- Ocheltree S.M., Hompesch M., Wondmagegnehu E.T., Morrow L., Win K., Jacober S.J. (2010) Comparison of pharmacodynamic intrasubject variability of insulin lispro protamine suspension and insulin glargine in subjects with type 1 diabetes. Eur J Endocrinol 163: 217–223 [DOI] [PubMed] [Google Scholar]
- Pontiroli A.E., Miele L., Morabito A. (2011) Increase of body weight during the first year of intensive insulin treatment in type 2 diabetes. Systematic review and meta-analysis. Diab Obes Metab 13: 1008–1019 [DOI] [PubMed] [Google Scholar]
- Ray J.A., Valentine W.J., Secnik K., Oglesby A.K., Cordony A., Gordois A., et al. (2005) Review of the cost of diabetes complications in Australia, Canada, France, Germany, Italy and Spain. Curr Med Res Opin 21: 1617–1629 [DOI] [PubMed] [Google Scholar]
- Roach P., Yue L., Arora V. (1999) Improved postprandial glycemic control during treatment with Humalog Mix25, a novel protamine-based insulin lispro formulation. Humalog Mix25 Study Group. Diabetes Care 22: 1258–1261 [DOI] [PubMed] [Google Scholar]
- Settembrini S., Piccolo G.P. (2007) Valutazione del compenso glicometabolico in una coorte di pazienti diabetici tipo 2 trattati con terapia insulinica plurifrazionata (3 somministrazioni di insulina umana regolare + NPL bedtime vs 3 somministrazioni di analogo lispro + NPL bedtime). CIC Edizioni Internazionali Roma, http://www.gruppocic.com, pp. 2-8
- Strojek K., Shi C., Carey M.A., Jacober S.J. (2010) Addition of insulin lispro protamine suspension or insulin glargine to oral type 2 diabetes regimens: a randomized trial. Diabetes Obes Metab 12: 916–922 [DOI] [PubMed] [Google Scholar]
- Swinnen S.G., Simon A.C., Holleman F., Hoekstra J.B., Devries J.H. (2011) Insulin detemir versus insulin glargine for type 2 diabetes mellitus. Cochrane Database Syst Rev 7: CD006383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tahrani A.A., Bailey C.J., Del Prato S., Barnett A.H. (2011) Management of type 2 diabetes: new and future developments in treatment. Lancet 378: 182–197 [DOI] [PubMed] [Google Scholar]
- The AMD Annals 2009 Working Group (2009) Longitudinal Analysis of Quality Indicators of Diabetes Care in Italy (2004–2007). Rome: Associazione Medici Diabetologi; Available at: http://www.infodiabetes.it/files/2009_annali_AMD_eng.pdf (accessed 4 February 2012). [Google Scholar]
- Whiting D.R., Guariguata L., Weil C., Shaw J. (2011) IDF Diabetes Atlas: Global estimates of the prevalence of diabetes for 2011 and 2030. Diabetes Res Clin Pract 94: 311–321 [DOI] [PubMed] [Google Scholar]