Abstract
Background
Overweight is among the major challenging health risk factors. It has been claimed that birth weight, being a critical indicator of prenatal developmental conditions, is related to long-term overweight risk. In order to check this important assumption of developmental and preventive medicine, we performed a systematic review and comprehensive meta-analysis.
Methods and Findings
Relevant studies published up to January 2011 that investigated the relation between birth weight and later risk of overweight were identified through literature searches using MEDLINE and EMBASE. For meta-analysis, 66 studies from 26 countries and five continents were identified to be eligible, including 643,902 persons aged 1 to 75 years. We constructed random-effects and fixed-effects models, performed subgroup-analyses, influence-analyses, assessed heterogeneity and publication bias, performed meta-regression analysis as well as analysis of confounder adjusted data. Meta-regression revealed a linear positive relationship between birth weight and later overweight risk (p<0.001). Low birth weight (<2,500 g) was found to be followed by a decreased risk of overweight (odds ratio (OR) = 0.67; 95% confidence interval (CI) 0.59–0.76). High birth weight (>4,000 g) was associated with increased risk of overweight (OR = 1.66; 95% CI 1.55–1.77). Results did not change significantly by using normal birth weight (2,500–4,000 g) as reference category (OR = 0.73, 95% CI 0.63–0.84, and OR = 1.60, 95% CI 1.45–1.77, respectively). Subgroup- and influence-analyses revealed no indication for bias/confounding. Adjusted estimates indicate a doubling of long-term overweight risk in high as compared to normal birth weight subjects (OR = 1.96, 95% CI 1.43–2.67).
Conclusions
Findings demonstrate that low birth weight is followed by a decreased long-term risk of overweight, while high birth weight predisposes for later overweight. Preventing in-utero overnutrition, e.g., by avoiding maternal overnutrition, overweight and/or diabetes during pregnancy, might therefore be a promising strategy of genuine overweight prevention, globally.
Introduction
Overweight is among the top challenging health problems at the beginning of the 21st century [1]. Prevalence has increased alarmingly, reaching epidemic levels in adults, adolescents, and even children in the US and globally [1]–[3]. Across the age spectrum, critical metabolic and cardiovascular morbidity (type 2 diabetes, hypertension, metabolic syndrome, coronary heart disease, stroke) is causally linked to obesity [2], [4], [5]. Cardiovascular and all-cause mortality are strongly related to overweight and obesity irrespective of age, sex, and ethnicity [6]–[9]. Therefore, measures of primary, genuine prevention are urgently needed.
For some years, the ‘fetal origins hypothesis’ on early causes of later diseases has become one of the most promising theoretical frameworks in medicine [10]–[12]. Especially, birth weight has been suggested and used as basic indicator to establish these highly influential concepts [10], [12], since it is decisively determined by the prenatal developmental conditions [13], [14]. However, one of the most important axioms in this context has not been tested globally so far. Although overweight is of central pathogenetic importance for metabolic, cardiovascular and general morbidity and mortality [2], [4], [5], no comprehensive analysis has investigated whether the risk of becoming overweight is related to birth weight in children, adolescents, and adults, i.e., for the long-term.
Therefore, we aimed to characterize this overall critical aspect of the ‘fetal origins’ approach by a systematic review and meta-analysis, substantially extending previous preliminary reviews [15]–[17].
Methods
Search strategy and selection criteria
Systematic review and meta-analysis were conducted according to the PRISMA statement for meta-analysis of observational studies (Text S1) [18], including the preparation of a protocol and analysis plan (Text S2). We performed a comprehensive literature search, including the databases MEDLINE and EMBASE (1966–January 2011), to identify studies that investigated the relation between birth weight and later risk of overweight. Searched terms were “birth weight”, “overweight”, “obesity” and “adiposity”, without language restrictions. Furthermore, we manually searched all references cited in original studies and all reviews identified. Authors were contacted if data, methods and/or parameter definitions provided from the respective studies remained unclear.
To be eligible for meta-analysis, a study had to fulfill the following criteria, defined a priori: 1) It had to be an original report on the relation between birth weight and risk of overweight. 2) Odds ratios (OR) and 95% confidence intervals (95% CI) (or data with which to calculate them) for risk of overweight in at least two strata of birth weight had to have been reported. All studies which reported the proportion of overweight or obese subjects in at least one age at follow up were included. We did not restrict to a particular definition of overweight/obesity as studies may have been published before currently accepted definitions were introduced [16]. The majority of studies used body mass index (BMI) as overweight criterion in childhood, adolescence as well as adulthood (80%).
From all eligible studies, data were abstracted in duplicate, using a standardized form. An independent reviewer confirmed all data entries.
Statistical analysis
Dichotomous comparisons
We extracted data on numbers of subjects with and without overweight above or below the cutoff value and calculated corresponding crude odds ratios and 95% confidence intervals. We constructed fixed-effects as well as random-effects models to estimate the pooled odds ratios for risk of overweight above vs. below the respective cutoff value across all studies.
Assessment of heterogeneity
By calculating the I2 according to Higgins et al [19], we assessed heterogeneity. Ranging from 0 to 100%, I2 is a direct measure of inconsistency of study results in a meta-analysis, with 0% indicating no inconsistency.
Influence analysis
Robustness of the pooled estimates was checked by influence analyses. Each of the studies was individually omitted from the data set, followed in each case by recalculation of the pooled estimate of the remaining studies.
Subgroup/Sensitivity analyses
To identify potential sources of heterogeneity and sources of bias, studies were stratified by study design and source of birth weight data to assess potential recall bias. Additionally, studies were stratified by publication language. To examine participation/selection bias, we stratified by extent of lost to follow-up. Further stratifications were made by geographic origin, age, overweight classification criterion, source of overweight data, gender distribution, gestational age and parental overweight (BMI>25 kg/m2). To assess the impact of parental socioeconomic status (SES), we stratified by the extent by which low SES was present in the study samples.
Publication bias
Publication bias was assessed by inspection of the funnel plot and formal testing for funnel plot asymmetry, using Begg's test and Egger's test.
Meta-regression
To explore the shape of the continuous relation between birth weight and later overweight risk, meta-regression technique was applied [20]. Accordingly, birth weight- specific odds ratios were related to the respective birth weight. Since birth weight was reported as categorical data with a certain range in the studies (per example, 2,000–2,500 g, 3,000–3,500 g etc.), median of the upper and lower limits of each category was assigned to the particular estimate in each study [21]. Estimates were plotted against respective birth weight as independent variable. After visual inspection, we primarily decided to use a linear regression model. Additionally, fractional polynomial regression was applied because it does not make an a priori assumption on shape of the curve. The family of second-order fractional polynomial models provides rich and flexible shapes of curves by choosing p = (p1,…,pm) as real-valued vector of fractional power from a predefined set [22]. All estimates were weighted by 1/variance.
Analysis of confounder-adjusted data
To perform meta-analysis of confounder-adjusted data we considered all studies which reported adjusted odds ratios for risk of overweight for the birth weight categories <2,500 g and/or >4,000 g. Resulting pooled odds ratios were based, however, on different reference categories, as defined by the authors themselves, and therefore not directly comparable to the pooled unadjusted odds ratios evaluated for <2,500 g vs. >2,500 g and >4,000 g vs. <4,000 g, respectively. To make pooled adjusted and unadjusted odds ratios more comparable, we therefore additionally calculated in all studies which provided adjusted data an unadjusted odds ratio that considered the reference category as used self-chosen by the authors for the adjusted odds ratios in the respective studies (bottom Tab. 1). Thereby, an orientating comparability of pooled adjusted vs. unadjusted odds ratios over all eligible studies was achieved [23]–[25].
Table 1. Birth weight and later risk of overweight: sensitivity and confounder analyses*.
| Category | Low birth weight Odds ratio (95% CI) | High birth weight Odds ratio (95% CI) |
| Number of studies | n = 30 | n = 45 |
| Study design | ||
| cohort studies | 0.67 (0.59−0.76) (n = 29) | 1.66 (1.56−1.78) (n = 40) |
| case-control studies | 0.17 (0.02−1.50) (n = 1) | 2.05 (1.51−2.78) (n = 5) |
| Geographic origin | ||
| Europe | 0.72 (0.54−0.95) (n = 11) | 1.63 (1.44−1.84) (n = 20) |
| North America | 0.76 (0.61−0.95) (n = 4) | 1.64 (1.43−1.88) (n = 7) |
| South America | 0.53 (0.42−0.68) (n = 10) | 1.69 (1.48−1.93) (n = 6) |
| Asia | 0.83 (0.48−1.42) (n = 4) | 1.75 (1.62−1.89) (n = 10) |
| Australia | 0.50 (0.32−0.77) (n = 1) | 2.23 (1.22−4.06) (n = 2) |
| Publication language | ||
| English | 0.67 (0.59−0.77) (n = 26) | 1.68 (1.57−1.80) (n = 38) |
| Non English | 0.63 (0.43−0.94) (n = 4) | 1.60 (1.30−1.97) (n = 7) |
| Age at follow up | ||
| 0–18 years | 0.60 (0.54−0.67) (n = 23) | 1.76 (1.65−1.87) (n = 37) |
| >18 years | 0.97 (0.79−1.20) (n = 7) | 1.40 (1.23−1.59) (n = 8) |
| Overweight classification criterion | ||
| BMI | 0.68 (0.60−0.78) (n = 25) | 1.63 (1.53−1.74) (n = 36) |
| Non BMI | 0.52 (0.24−1.11) (n = 5) | 2.26 (1.85−2.75) (n = 9) |
| Assessment of birth weight | ||
| registry | 0.74 (0.32−1.69) (n = 1) | 1.39 (0.88−2.19) (n = 2) |
| records/examination | 0.68 (0.57−0.81) (n = 14) | 1.72 (1.56−1.89) (n = 22) |
| interview/questionnaire | 0.65 (0.53−0.80) (n = 14) | 1.65 (1.48−1.83) (n = 18) |
| not reported | 0.17 (0.02−1.50) (n = 1) | 2.08 (0.69−6.19) (n = 3) |
| Assessment of overweight | ||
| records/examination | 0.63 (0.56−0.71) (n = 26) | 1.71 (1.61−1.82) (n = 39) |
| interview/questionnaire | 0.88 (0.70−1.11) (n = 4) | 1.45 (1.24−1.71) (n = 5) |
| not reported | - | 6.72 (1.45−31.0) (n = 1) |
| Gender distribution | ||
| ≤50% males | 0.59 (0.41−0.85) (n = 10) | 1.65 (1.43−1.91) (n = 18) |
| >50% males | 0.70 (0.62−0.78) (n = 18) | 1.71 (1.60−1.83) (n = 23) |
| not reported | 0.66 (0.52−0.84) (n = 2) | 1.68 (1.55−1.82) (n = 4) |
| Lost-to-follow up | ||
| ≤20% | 0.57 (0.46−0.70) (n = 11) | 1.72 (1.58−1.88) (n = 13) |
| >20% | 0.74 (0.61−0.89) (n = 17) | 1.65 (1.49−1.83) (n = 26) |
| not reported | 0.53 (0.23−1.22) (n = 2) | 1.80 (1.60−2.02) (n = 6) |
| Parental SES | ||
| low SES>30% of population | 0.71 (0.60−0.83) (n = 5) | 1.64 (1.47−1.18) (n = 7) |
| low SES≤30% of population | 0.58 (0.52−0.65) (n = 5) | 1.78 (1.63−1.94) (n = 9) |
| not reported | 0.70 (0.58−0.85) (n = 20) | 1.61 (1.45−1.79) (n = 29) |
| Gestational age | ||
| only term newborns | 0.59 (0.41−0.84) (n = 3) | 1.67 (1.44−1.94) (n = 9) |
| term and preterm newborns | 0.65 (0.57−0.74) (n = 6) | 1.70 (1.46−1.97) (n = 5) |
| not reported | 0.68 (0.56−0.82) (n = 21) | 1.66 (1.51−1.82) (n = 31) |
| Parental overweight | ||
| >30% of population | 0.69 (0.41−1.18) (n = 2) | 1.58 (1.29−1.94) (n = 6) |
| ≤30% of population | - | 1.73 (1.55−1.93) (n = 4) |
| not reported | 0.67 (0.58−0.76) (n = 28) | 1.66 (1.54−1.79) (n = 35) |
| Confounder-adjusted analyses | ||
| Studies with adjustments | ||
| unadjusted estimates | 0.50 (0.32−0.78) (n = 1) | 1.87 (1.56−2.25) (n = 16) |
| adjusted estimates | 0.51 (0.33−0.80) (n = 1) | 1.93 (1.56−2.38) (n = 16) |
| Studies without adjustments | 0.68 (0.60−0.77) (n = 29) | 1.68 (1.54−1.84) (n = 29) |
Abbreviation: BMI, body mass index; CI, confidence interval
random-effects model
Software
All calculations were performed with STATA, version 11.0, software (Stata Corp., College Station, TX, USA).
Ethics Statement
An ethics statement was not required for this work.
Results
Baseline characteristics of the studies
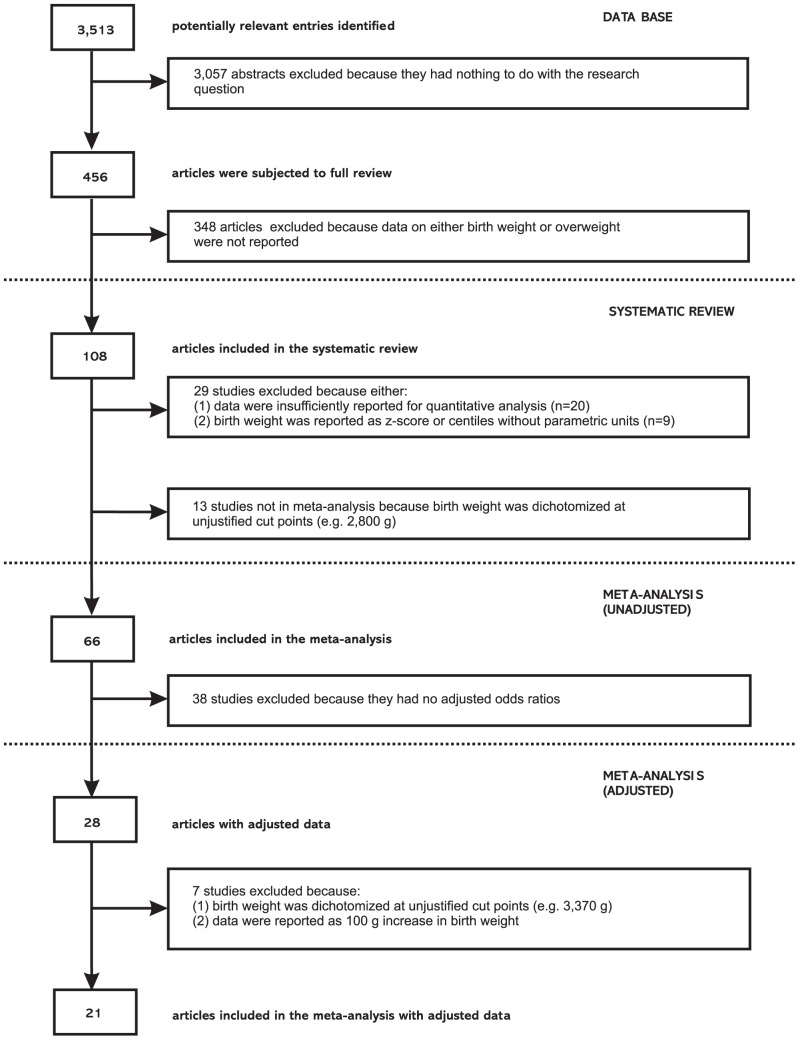
Course of the systematic review is illustrated in a flow diagram according to the PRISMA statement (Figure 1). From a total of 3,513 potentially relevant entries, 108 studies were identified which related birth weight to risk of later overweight [26]–[133]. They involved a total of 1,485,561 persons at six months to 79 years of age (for study characteristics see Table S1).
Figure 1. Flow diagram of selection process.
Course of systematic literature review on birth weight and risk of overweight later in life, 1966–January 2011.
In the systematic review, 94 of the 108 studies (87%) reported a positive relation between birth weight and later risk of overweight. In 7 studies (6.5%), no relation between birth weight and later risk of overweight was observed, while in 6 studies (5.6%) a U-shaped relation was found. Only one study (0.9%) reported an inverse relation between birth weight and later overweight risk.
For methodological reasons, 42 studies could not be included in the meta-analysis. Reasons for exclusion were firstly, data were insufficiently reported for quantitative analysis (n = 20). Secondly, birth weight was reported as z-score or centiles without units (n = 9) and thirdly, birth weight was dichotomized at unjustified cut points (n = 13) (see Figure 1). However, these excluded studies showed no relevant differences in general characteristics, e.g., distribution of geographic origin, age at follow up, assessment of overweight etc. Moreover, the observed relations between birth weight and later outcome did generally not differ from those observed in studies which could be included in the meta-analysis. Of the 42 excluded studies, 35 (83.4%) reported a positive relation between birth weight and later risk of overweight. In 3 studies (7.1%), no relation between birth weight and risk of later overweight was observed. A U-shaped relation was reported in 3 studies (7.1%) and only one study (2.4%) reported an inverse relation between birth weight and later overweight risk. These percentages were very similar to those observed in the studies which could be included into meta-analysis (see below).
For meta-analysis, 66 studies were identified to be eligible, including 58 cohort studies and eight studies with case-control-design [68]–[133], involving a total of 643,902 persons. Age of participants ranged from 1 to 75 years and the year of birth ranged from 1914–2004 (Table S1). Studies were performed in Asia, Australia, Europe, North America and South America. Study size varied ranging from 82 to 153,536 participants.
General estimates
Of the 66 studies eligible for meta-analysis 59 studies (89.4%) reported a positive relation between birth weight and later risk of overweight. In 4 studies (6.1%), no relation between birth weight and later risk of overweight was observed, whereas in 3 studies (4.5%) a U-shaped relation was detected. None of the studies reported an inverse relation between birth weight and later overweight risk.
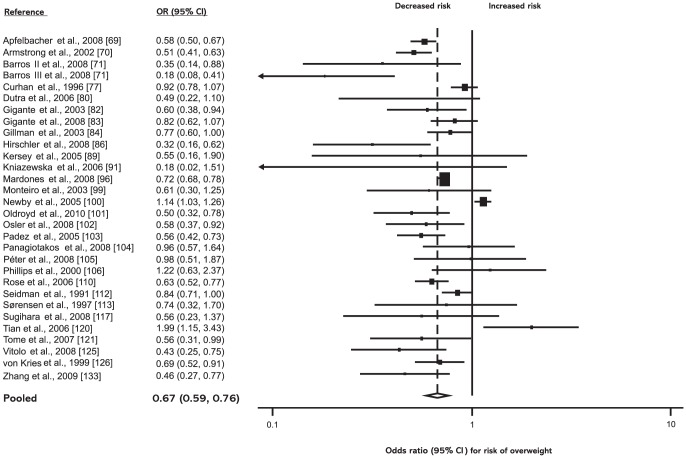
Low birth weight (<2,500 g) was found to be associated with a decreased risk of overweight in the random-effects model (OR = 0.67; 95% CI: 0.59–0.76) as well as in the fixed-effects model (OR = 0.75; 95% CI: 0.72–0.79; see Figure 2).
Figure 2. Low birth weight (<2,500 g) and subsequent risk of overweight.
ORs for overweight in subjects with birth weights <2,500 g as compared with subjects with birth weights ≥2,500 g. Studies are ordered alphabetically by first author. The point estimate (center of each black square) and the statistical size (proportional area of square) are represented. Horizontal lines indicate 95% confidence intervals. The pooled odds ratio (diamond) was calculated by means of a random effects model. OR, odds ratio; CI, confidence interval.
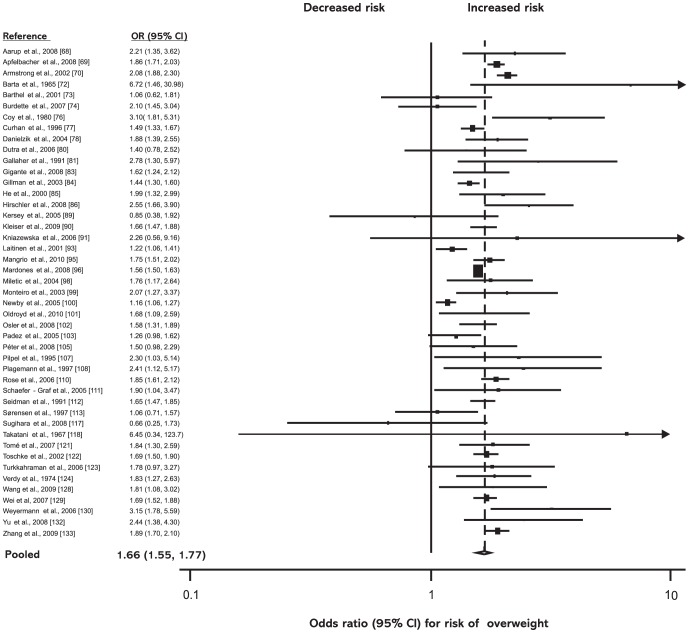
High birth weight (>4,000 g) was associated with increased risk of overweight in the random-effects model (OR = 1.66; 95% CI: 1.55–1.77) as well as in the fixed-effects model (OR = 1.61; 95% CI: 1.57–1.65; see Figure 3).
Figure 3. High birth weight (>4,000 g) and subsequent risk of overweight.
ORs for overweight in subjects with birth weights >4,000 g as compared with subjects with birth weights ≤4,000 g. Studies are ordered alphabetically by first author. The point estimate (center of each black square) and the statistical size (proportional area of square) are represented. Horizontal lines indicate 95% confidence intervals. The pooled odds ratio (diamond) was calculated by means of a random effects model. OR, odds ratio; CI, confidence interval.
Given these results, we repeated the dichotomous comparisons, now using “normal birth weight” (2,500–4,000 g) as reference category for all studies that gave data on both ends of the birth weight spectrum. The pooled estimate for low birth weight was 0.73 (95% CI: 0.63–0.84) and those for high birth weight was 1.60 (95% CI: 1.45–1.77; all random-effects model).
Influence analysis showed that the pooled estimates were robust. Omission of individual studies revealed that no single study had a particular influence on the pooled estimates, detected by pooled odds ratios ranging from 0.65 (95% CI: 0.57–0.73) to 0.68 (95% CI: 0.60–0.77) for low birth weight, and 1.64 (95% CI: 1.54–1.75) to 1.68 (95% CI: 1.58–1.78) for high birth weight.
Sensitivity/subgroup analyses
According to I2 [19], results were heterogeneous for both low birth weight (I2 = 93%) and high birth weight (I2 = 81%). To identify possible sources of heterogeneity and bias, we performed sensitivity/subgroup analyses (Table 1). Neither stratification by study design, nor by method of recording birth weight gave indication of recall bias. Geographic origin had no impact on the pooled estimates. Stratification by publication language also gave no indication for respective bias. Consideration of age revealed that the effect of high birth weight remained significant even in adulthood, whereas influence of low birth weight remained non-significant. Stratification by overweight classification criterion showed that studies which used non-BMI-based criteria, such as waist circumference (WC), waist-to-hip ratio (WHR) or waist-to-height ratio (WHtR), reported even stronger relations between birth weight and later overweight risk. Gender distribution had no impact on the pooled estimates. Furthermore, studies with higher lost to follow-up rates (>20%) had similar pooled estimates as those with low percentage of lost participants (≤20%). Surprisingly, a considerable number of studies did not account for gestational age, SES and/or parental body weight. However, even these potentially critical confounders had no significant impact on the overall results (Table 1).
Impact of publication bias
Neither for the relation between low birth weight and risk of overweight nor for that between high birth weight and later overweight risk evidence for publication bias was found, as indicated by visual inspection of funnel plots, proven by nonsignificant Begg's tests (low birth weight: p = 0.80; high birth weight: p = 0.45) and Egger's tests (low birth weight: p = 0.07; high birth weight: p = 0.23).
Shape of the continuous association between birth weight and risk of overweight
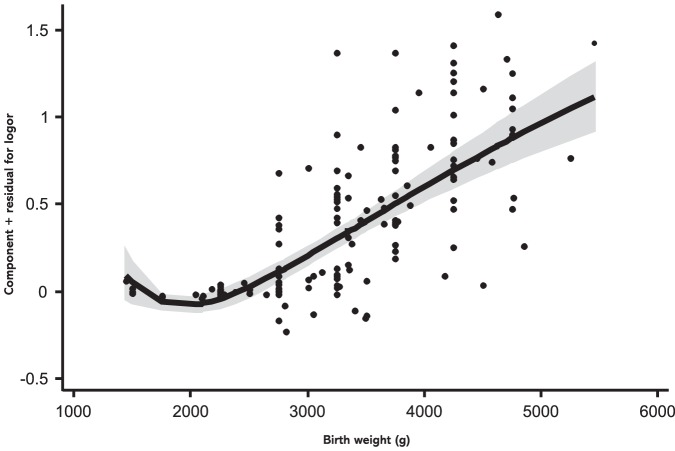
In a first step, we fitted a linear meta-regression model to the data, which revealed a significant positive linear relation between birth weight and subsequent overweight risk (b = 0.34×10−3 (0.28−0.40×10−3); p<0.001). To further explore the shape of the association, fractional polynomial regression was used. Figure 4 shows the shape of the curve for the continuous relation between birth weight and later risk of overweight, estimated by a second-order fractional polynomial regression model (b1 = 14.13 (9.27–19.00); b2 = −20.34 (−26.58−(−14.09)); p1 = −1; p2 = −0.5; p<0.001; inverse variance weighted). Over nearly the entire birth weight spectrum, birth weight was found to be linearly positively related to overweight risk. Risk does not further decrease below a birth weight of 1,500 g. Comparison of model fitness parameters showed that a linear regression model performed as good as the fractional polynomial model (p = 0.17 for comparison of deviance between both models).
Figure 4. Relationship between birth weight and risk of overweight.
Continuous relation between birth weight and later risk of overweight, calculated by fractional polynomial regression. Studies are represented by black dots. Grey shading indicates the 95% confidence interval around the fitted line. The model was estimated from a robust regression model based on second-order fractional polynomial (−1, −0.5) functions weighted by/variance.
Impact of confounders on strength of the association
Whereas only one study gave an adjusted estimate for low birth weight, in 16 studies confounder-adjusted estimates for risk of overweight after high birth weight were reported. Number and types of adjustments varied across the studies (Table S2). The pooled confounder-adjusted estimate for overweight after high birth weight was nearly the same as the pooled estimate of the unadjusted data from the same studies using the same reference category (Table 1). Fully adjusted estimates revealed a nearly doubled long-term overweight risk in individuals with high birth weight compared to normal birth weight subjects (OR = 1.96; 95% CI: 1.43–2.67). Weighted fractional polynomial regression of the confounder-adjusted data revealed very similar results as in the case of unadjusted data (b1 = 16.59 (9.55–23.64); b2 = −24.11 (−33.06 (−15.16)); p1 = −1; p2 = −0.5; p<0.001; inverse variance weighted).
Discussion
Over several years, increasing attention is given on early developmental origins of long-term diabetic, adipogenic, and cardiovascular disorders in terms of the metabolic syndrome [10], [11]. However, the direction and strength of relation between birth weight and long-term overweight risk has not been tested globally so far in a comprehensive manner. Therefore, we aimed to characterize this overall critical aspect of the ‘fetal origins’ approach by a respective meta-analysis, quantitatively as well as qualitatively substantially extending and proving previous preliminary reviews, statements, proposals etc. by our own group and others [15]–[17].
The data set and meta-analysis provided here is by far the largest one analyzed to date on this topic and the first to address the whole lifespan, provide confounder-adjusted estimates and incorporate global data i.e., including western, westernized as well as developing countries in Northern- and South America, Europe, Asia and Australia. Our analysis shows with high consistency that an increased birth weight (>4,000 g) may lead to a doubling of the long-term overweight risk, irrespective of geographic/ethnic origin, sex, socio-economic status, parental weight status etc.
In the context of the ‘small baby syndrome’ and the respective ‘fetal origins’ hypotheses [10]–[12], it has been claimed that low birth weight is a risk factor for cardiovascular diseases and type 2 diabetes, as tested by systematic reviews and meta-analyses with mixed results [134]–[138], as well as for the development of overweight/obesity, i.e., one of the most critical cardiometabolic risk determinants [5]–[7]. Interestingly, results of our meta-analysis do not support this claim. In contrast, across the birth weight spectrum a linear positive relation exists with later overweight risk. Only a small fraction of studies, analyzing probands with very low birth weight (VLBW; <1,500 g; n = 3 studies), found no further decrease of overweight risk at this very ‘left-handed’ side of the birth weight spectrum.
General concerns on our data and their interpretation might arise regarding the suitability of investigated parameters and/or the consideration of bias and/or confounding variables. For instance, it has increasingly been proposed that the effect of low birth weight on later health risks might rather result from increased (‘rapid’) neonatal weight gain/catch up growth [139]. This was regarded, unfortunately, in only five reports (4.6%; Table S3) [79], [109], [114], [115], [116], three of which [79], [115], [116] reported respectively adjusted data analyses. An ‘obesogenic’ effect of low birth weight was not observed in these unadjusted or adjusted studies. By contrast, all found an effect of high birth weight on later overweight risk, independently of early weight gain. Furthermore, although BMI has been established as routine parameter to identify overweight, it does not necessarily describe the cardiometabolically critical fat content and distribution [140]. Alternative measures, particularly reflecting abdominal obesity (waist circumference, waist-to-hip ratio, waist-to-height ratio), have been shown to be more accurate risk predictors [140]. Respective subgroup analyses revealed, however, that the relation between birth weight and later overweight risk was even strengthened when non-BMI related measures were applied. Also subgroup analyses considering gestational age, age at follow-up, geographic origin etc. showed no significant influence on the overall outcome. Moreover, pooled adjusted estimates were calculated considering the influence of confounders on the strength of the relation under investigation. However, they had no significant impact on the final outcome. Even parental weight status had only a marginal influence on the relation between birth weight and later overweight risk. This result appears to be of particular interest, since parental weight/overweight might represent contribution of genetic factors to the investigated relationship. Interestingly, it has been shown that none of the genetic obesity risk factors identified to date has a significant influence on birth weight [141], making respective confounding rather unlikely, as supported here.
Recently, Yu et al. [17] published a systematic review on the association between birth weight and downstream obesity, including 129,260 subjects from 33 studies, mainly originating from Asia (58%). Their meta-analysis involved 20 studies with a total of 42,863 subjects, most from China (15 studies; 88% of subjects). We analyzed a similar number of studies from Asia (n = 12) with a higher number of subjects from Asia (n = 140,734) as well as China (n = 103,411) in our meta-analysis. Interestingly, focussing on Asian/Chinese subjects Yu et al. [17] came to similar results as presented here: low birth weight was accompanied by decreased risk of obesity later on (OR = 0.61; 95% CI: 0.46–0.80), while high birth weight was associated with increased obesity risk (OR = 2.07; 95% CI: 1.91–2.24). Their analysis focused solely on obesity, with the meta-analysis only on children and adolescents including mainly Asian/Chinese subjects, studies and databases. A number of variables (e.g., geographic origin/ethnicity, gestational age, age at follow-up, parental weight etc.) were not considered and confounder adjusted estimates were not provided. Nevertheless, the observed trend in the relation under investigation was similar to those ascertained and described in our study. This appears to underline the global impact and reproducibility of the observed relationship and indicates that it is even relevant for Asian populations, characterized by a high frequency of relatively ‘low birth weight’ subjects but, simultaneously, continuous increase of ‘diabesity’ prevalence [142], [143].
Therefore, it must be noted that the provided data analyses should not be interpreted in terms of a ‘beneficial’ effect of a reduced birth weight. To the contrary, epidemiological, clinical as well as experimental observations have convincingly demonstrated long-term deleterious consequences in association with a decreased birth weight, especially concerning metabolic-syndrome-like disorders and diseases [10], [11]. Therefore, future studies should consider more precise measures of body composition, fat content and, especially, accompanying metabolic and hormonal alterations both at birth and later life to better understand pathophysiological links between altered prenatal nutritional and growth conditions and later overweight and ‘diabesity’ risk. Future studies should generally consider important variables in the relationship between fetal growth and later outcome, especially the potential impact of gestational age, maternal diseases during pregnancy, as well as neonatal nutrition, growth pattern and fat deposition. Finally, a slight trend has been observed here towards successively increasing risk of overweight in low birth weight subjects with increasing age, i.e., in adulthood (Table 1). Therefore, a ‘U-shaped’ curve, as it has been described regarding type 2 diabetes and hypertension [136], [134], with increasing age up to the elderly of the relation between birth weight and later risk of overweight, cannot be excluded from our data. Occasionally, pathophysiological causes and mechanisms of a latency of overweight manifestation in formerly low birth weight subjects remain to be evaluated.
Birth weight is essentially determined by the in-utero developmental conditions (13, 14), especially the materno-fetal food supply [144]–[146]. Accordingly, it appears important to notice that in parallel with the global ‘diabesity’ epidemics [2], [3]; the number of overweight and/or diabetic women at reproductive age has increased dramatically [147], [148]. Overweight and/or diabetes during pregnancy, however, lead to fetal overnutrition, often followed by increased birth weight, fatness and macrosomia at birth [144]–[146], [149], [150]. All of this has been shown to be preventable by adequate nutritional and metabolic management during pregnancy [151], [152]. With respect to our data of increased overweight risk in formerly macrosomic newborns, respective preventive measures may therefore not only improve the peripartal and perinatal outcome [151], [152], but even the long-term overweight risk and resulting disease dispositions. This prediction is in line with a number of epidemiological, clinical and experimental data which have shown an increased risk of overweight, obesity and diabetes in offspring of diabetic and/or obese pregnant women, even independent of or in addition to genetic dispositions [153]–[157]. Especially, fetal hyperglycemia/overnutrition leads to fetal B cell hyperplasia and hyperinsulinism, which have been shown to be preserved for the long term and subsequently may predispose to insulin resistance and a permanent obesity disposition [144]–[146], [158]–[161]. In general, mechanistic approaches speak in favour of epigenomic and/or microstructural long-term malprogramming of body weight regulatory systems by fetal overfeeding and accompanying hormonal disturbances during critical periods of fetal development, predisposing to increased overweight risk for the long-term [146], [154], [157]–[162].
Accordingly, prenatal life appears to be a ‘critical period’ [163], [164] of determination and, consequently, potential genuine prevention of long-term overweight predisposition and its critical co-morbidity [165]. Interestingly, high birth weight has also been described to be a risk factor for, e.g., type 2 diabetes, hypertension, childhood primary brain tumors and breast cancer [136], [134], [166], [167], all shown to be critically linked to overweight throughout life [2]–[4], [168].
Taken together, increased birth weight is reproducibly and independently linked to increased overweight risk later on, suggesting prenatal overfeeding as important risk factor which ‘programms’ a long-term obesity predisposition. In conclusion, avoiding in-utero overnutrition, especially by avoiding and/or adequately managing maternal overweight, overnutrition, increased weight gain and/or diabetes during pregnancy, appears to be a promising strategy to lower overweight risk for the long term, globally.
Supporting Information
PRISMA checklist.
(DOC)
Study protocol for systematic review and meta-analysis to determine the relation between birth weight and long-term overweight risk.
(DOC)
Characteristics of 108 studies included in the systematic review of birth weight and subsequent risk of overweight, 1966–January 2011.
(DOC)
Studies that adjusted for confounders in the meta-analysis on birth weight and subsequent risk of overweight, 1966-January 2011.
(DOC)
Studies that reported data on neonatal weight gain or infant growth in the meta-analysis on birth weight and subsequent risk of overweight, 1966-January 2011.
(DOC)
Funding Statement
This study was supported by grants of the the German Research Foundation (DFG: GRK 1208; PL 241/5-1) to Dr. Plagemann. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1. King D (2011) The future challenge of obesity. Lancet 378: 743–744. [DOI] [PubMed] [Google Scholar]
- 2. Mokdad AH, Ford ES, Bowman BA, Dietz WH, Vinicor F, et al. (2003) Prevalence of obesity, diabetes, and obesity related health risk factors, 2001. JAMA 289: 76–79. [DOI] [PubMed] [Google Scholar]
- 3. Ogden CL, Carroll MD, Curtin LR, Lamb MM, Flegal KM (2010) Prevalence of high body mass index in US children and adolescents, 2007–2008. JAMA 303: 242–249. [DOI] [PubMed] [Google Scholar]
- 4. Tirosh A, Shai I, Afek A, Dubnov-Raz G, Ayalon N, et al. (2011) Adolescent BMI trajectory and risk of diabetes versus coronary disease. N Engl J Med 364: 1315–1325. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Nordestgaard BG, Palmer TM, Benn M, Zacho J, Tybjaerg-Hansen A, et al. (2012) The effect of elevated body mass index on ischemic heart disease risk: causal estimates from a mendelian randomisation approach. PLoS Med 9: e1001212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Prospective studies collaboration (2009) Body mass index and cause-specific mortality in 900000 adults: collaborative analyses of 57 prospective studies. Lancet 373: 1083–1096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Berrington de Gonzalez A, Hartge P, Cerhan JR, Flint AJ, Hannan L, et al. (2010) Body-mass index and mortality among 1.46 million white adults. N Engl J Med 363: 2211–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, et al. (2010) Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med 362: 485–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Boggs DA, Rosenberg L, Cozier YC, Wise LA, Coogan PF, et al. (2011) General and abdominal obesity and risk of death among black women. N Engl J Med 365: 901–908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Barker DJ, Hales CN, Fall CHD, Osmond C, Phipps K, et al. (1993) Type 2 (non-insulin-dependent) diabetes mellitus, hypertension and hyperlipidaemia (syndrome X): relation to reduced fetal growth. Diabetologia 36: 62–67. [DOI] [PubMed] [Google Scholar]
- 11. Gluckman PD, Hanson MA, Cooper C, Thornburg KL (2008) Effect of in utero and early-life conditions on adult health and disease. N Engl J Med 359: 61–73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Hales CN, Barker DJ (2001) The thrifty phenotype hypothesis. Br Med Bull 60: 5–20. [DOI] [PubMed] [Google Scholar]
- 13. Brooks AA, Johnson MR, Steer PJ, Pawson ME, Abdalla HI (1995) Birth weight: nature or nurture? Early Hum Dev 42: 29–35. [DOI] [PubMed] [Google Scholar]
- 14. Lunde A, Melve KK, Gjessing HK, Skjaerven R, Irgens LM (2007) Genetic and environmental influences on birth weight, birth length, head circumference, and gestational age by use of population-based parent-offspring data. Am J Epidemiol 165: 734–741. [DOI] [PubMed] [Google Scholar]
- 15. Harder T, Schellong K, Stupin J, Dudenhausen JW, Plagemann A (2007) “Where is the evidence that low birthweight leads to obesity?” [letter]. Lancet 369: 1859. [DOI] [PubMed] [Google Scholar]
- 16. Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, et al. (2005) Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ 331: 929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Yu ZB, Han SP, Zhu GZ, Zhu C, Wang XJ, et al. (2011) Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obes Rev 12: 525–542. [DOI] [PubMed] [Google Scholar]
- 18. Moher D, Liberati A, Tetzlaff J, Altman DG (2009) The Prisma Group (2009) Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLoS Med 7: 1006–1012. [PMC free article] [PubMed] [Google Scholar]
- 19. Higgins JP, Thompson SG, Deeks JJ, Altman DG (2003) Measuring inconsistency in meta-analysis. BMJ 327: 557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Berlin JA, Longnecker MP, Greenland S (1993) Meta-analysis of epidemiologic dose-response data. Epidemiology 4: 218–228. [DOI] [PubMed] [Google Scholar]
- 21. Greenland S, Longnecker MP (1992) Methods for trend estimation from summarized dose-response data, with applications to meta-analysis. Am J Epidemiol 135: 1301–1308. [DOI] [PubMed] [Google Scholar]
- 22. Royston P, Ambler G, Sauerbrei W (1999) The use of fractional polynomials to model continuous risk variables in epidemiology. Int J Epidemiol 28: 964–974. [DOI] [PubMed] [Google Scholar]
- 23. Harder T, Roepke K, Diller N, Stechling Y, Dudenhausen JW, et al. (2009) Birth weight, early weight gain, and subsequent risk of type 1 diabetes: systematic review and meta-analysis. Am J Epidemiol 169: 1428–1436. [DOI] [PubMed] [Google Scholar]
- 24. Cardwell CR, Patterson CC (2009) Re: “Birth weight, early weight gain, and subsequent risk of type 1 diabetes” [letter]. Am J Epidemiol 170: 529–530. [DOI] [PubMed] [Google Scholar]
- 25. Harder T, Plagemann A (2009) “Authors' reply: Birth weight, early weight gain and subsequent risk of type 1 diabetes: systematic review and meta-analysis” [letter]. Am J Epidemiol 170: 530–531. [DOI] [PubMed] [Google Scholar]
- 26. Araújo CL, Hallal PC, Nader GA, Neutzling MB, deFátima Vieira M, et al. (2009) Effect of birth size and proportionality on BMI and skinfold thickness in early adolescence: prospective birth cohort study. Eur J Clin Nutr 63: 634–639. [DOI] [PubMed] [Google Scholar]
- 27. Binkin NJ, Yip R, Fleshood L, Trowbridge FL (1988) Birth weight and childhood growth. Pediatrics 82: 828–834. [PubMed] [Google Scholar]
- 28. Boney CM, Verma A, Tucker R, Vohr BR (2005) Metabolic syndrome in childhood: association with birth weight, maternal obesity, and gestational diabetes mellitus. Pediatrics 115: 290–296. [DOI] [PubMed] [Google Scholar]
- 29. Bouhours-Nouet N, Dufresne S, de Casson FB, Mathieu E, Douay O, et al. (2008) High birth weight and early postnatal weight gain protect obese children and adolescents from truncal adiposity and insulin resistance: metabolically healthy but obese subjects? Diabetes Care 31: 1031–1036. [DOI] [PubMed] [Google Scholar]
- 30. Celi F, Bini V, De Giorgi G, Molinari D, Faraoni F, et al. (2003) Epidemiology of overweight and obesity among school children and adolescents in three provinces of central Italy, 1993–2001: study of potential influencing variables. Eur J Clin Nutr 57: 1045–1051. [DOI] [PubMed] [Google Scholar]
- 31. Charney E, Goodman HC, McBride M, Lyon B, Pratt R (1976) Childhood antecedents of adult obesity. Do chubby infants become obese adults? N Engl J Med 295: 6–9. [DOI] [PubMed] [Google Scholar]
- 32. da Costa Ribeiro I, Taddei JAAC, Colugnatti F (2003) Obesity among children attending elementary public schools in São Paulo, Brazil: a case-control study. Public Health Nutr 6: 659–663. [DOI] [PubMed] [Google Scholar]
- 33. Drachler M de L, Macluf SP, Leite JC, Aerts DR, Giugliani ER, et al. (2003) Risk factors for overweight in children from Southern Brazil (Portuguese). Cad Saúde Pública 19: 1073–1081. [DOI] [PubMed] [Google Scholar]
- 34. de Moraes SA, Beltrán Rosas J, Mondini L, Freitas IC (2006) Prevalence of overweight and obesity, and associated factors in school children from urban area in Chilpancingo, Guerrero, Mexico, 2004 (Portuguese). Cad Saúde Pública 22: 1289–1301. [DOI] [PubMed] [Google Scholar]
- 35. Dieu HTT, Dibley MJ, Sibbritt D, Hanh TT (2007) Prevalence of overweight and obesity in preschool children and associated socio-demographic factors in Ho Chi Minh City, Vietnam. Int J Pediatr Obes 2: 40–50. [DOI] [PubMed] [Google Scholar]
- 36. Dubois L, Girard M (2006) Early determinants of overweight at 4.5 years in a population-based longitudinal study. Int J Obes 30: 610–617. [DOI] [PubMed] [Google Scholar]
- 37. Eriksson J, Forsén T, Tuomilehto J, Osmond C, Barker D (2001) Size at birth, childhood growth and obesity in adult life. Int J Obes 25: 735–740. [DOI] [PubMed] [Google Scholar]
- 38. Frye C, Heinrich J (2003) Trends and predictors of overweight and obesity in East German children. Int J Obes 27: 963–969. [DOI] [PubMed] [Google Scholar]
- 39. Fuiano N, Rapa A, Monzani A, Pietrobelli A, Diddi G, et al. (2008) Prevalence and risk factors for overweight and obesity in a population of Italian schoolchildren: a longitudinal study. J Endocrinol Invest 31: 979–984. [DOI] [PubMed] [Google Scholar]
- 40. Guimarães LV, de Azevedo Barros MB, Martins MSAS, Duarte EC (2006) Factors associated with overweight in schoolchildren (Portuguese). Rev Nutr 19: 5–17. [Google Scholar]
- 41. Hack M, Schluchter M, Cartar L, Rahman M, Cuttler L, et al. (2003) Growth of very low birth weight infants to age 20 years. Pediatrics 112 e: 30–38. [DOI] [PubMed] [Google Scholar]
- 42. Hawkins SS, Cole TJ (2009) Law C; Millennium Cohort Study Child Health Group (2009) An ecological systems approach to examining risk factors for early childhood overweight: findings from the UK Millennium Cohort Study. J Epidemiol Community Health 63: 147–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Hui LL, Nelson EA, Yu LM, Li AM, Fok TF (2003) Risk factors for childhood overweight in 6-7-y-old Hong Kong children. Int J Obes 27: 1411–1418. [DOI] [PubMed] [Google Scholar]
- 44. Koupil I, Toivanen P (2008) Social and early-life determinants of overweight and obesity in 18-year-old Swedish men. Int J Obes (Lond) 32: 73–81. [DOI] [PubMed] [Google Scholar]
- 45. Leong NM, Mignone LI, Newcomb PA, Titus-Ernstoff L, Baron JA, et al. (2003) Early life risk factors in cancer: the relation of birth weight to adult obesity. Int J Cancer 103: 789–791. [DOI] [PubMed] [Google Scholar]
- 46. Li C, Goran MI, Kaur H, Nollen N, Ahluwalia JS (2007) Developmental trajectories of overweight during childhood: role of early life factors. Obesity 15: 760–771. [DOI] [PubMed] [Google Scholar]
- 47. Locard E, Mamelle N, Billette A, Miginiac M, Munoz F, et al. (1992) Risk factors of obesity in a five year old population. Parental versus environmental factors. Int J Obes 16: 721–729. [PubMed] [Google Scholar]
- 48. Lundgren EM, Cnattingius S, Jonsson B, Tuvemo T (2003) Prediction of adult height and risk of overweight in females born small-for-gestational-age. Paediatr Perinat Epidemiol 17: 156–163. [DOI] [PubMed] [Google Scholar]
- 49. Maddah M (2009) Risk factors for overweight in urban and rural school girls in Iran: skipping breakfast and early menarche. Int J Cardiol 136: 235–238. [DOI] [PubMed] [Google Scholar]
- 50. Mazur A, Małecka-Tendera E, Klimek K (2003) Risk factors of obesity in primary school children from the Podkarpacie Region Part II. Obesity risk factors in girls (Polish). Pediatr Pol 78: 889–895. [Google Scholar]
- 51. Mazur A, Małecka-Tendera E, Klimek K (2003) Risk factors of obesity in primary school children from the Podkarpacie Region Part I. Obesity risk factors in boys. (Polish). Pediatr Pol 78: 881–888. [Google Scholar]
- 52. Mazur A, Klimek K, Telega G, Hejda G, Wdowiak L, et al. (2008) Risk factors for obesity development in school children from south-eastern Poland. Ann Agric Environ Med 15: 281–285. [PubMed] [Google Scholar]
- 53. Meas T, Deghmoun S, Armoogum P, Alberti C, Levy-Marchal C (2008) Consequences of being born small for gestational age on body composition: an 8-year follow-up study. J Clin Endocrinol Metab 93: 3804–3809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54. Mogan J (1986) Parental weight and its relation to infant feeding patterns and infant obesity. Int J Nurs Stud 23: 255–264. [DOI] [PubMed] [Google Scholar]
- 55. O'Callaghan MJ, Williams GM, Andersen MJ, Bor W, Najman JM (1997) Prediction of obesity in children at 5 years: a cohort study. J Paediatr Child Health 33: 311–316. [DOI] [PubMed] [Google Scholar]
- 56. Ochoa MC, Moreno-Aliaga MJ, Martínez-González MAM, Martínez JA, Marti A; GENOI Members (2007) Predictor factors for childhood obesity in a Spanish case-control study. Nutrition 23: 379–384. [DOI] [PubMed] [Google Scholar]
- 57. Olson CM, Strawderman MS, Dennison BA (2009) Maternal weight gain during pregnancy and child weight at age 3 years. Matern Child Health J 13: 839–846. [DOI] [PubMed] [Google Scholar]
- 58. Rugholm S, Baker JL, Olsen LW, Schack-Nielsen L, Bua J, et al. (2005) Stability of the association between birth weight and childhood overweight during the development of the obesity epidemic. Obes Res 13: 2187–2194. [DOI] [PubMed] [Google Scholar]
- 59. Savva SC, Tornaritis M, Chadjigeorgiou C, Kourides YA, Savva ME, et al. (2005) Prevalence and socio-demographic associations of undernutrition and obesity among preschool children in Cyprus. Eur J Clin Nutr 59: 1259–1265. [DOI] [PubMed] [Google Scholar]
- 60. Seidman DS, Laor A, Stevenson DK, Sivan E, Gale R, et al. (1998) Macrosomia does not predict overweight in late adolescence in infants of diabetic mothers. Acta Obstet Gynecol Scand 77: 58–62. [DOI] [PubMed] [Google Scholar]
- 61. Serra-Majem L, Bartrina JA, Pérez-Rodrigo C, Ribas-Barba L, Delgado-Rubio A (2006) Prevalence and determinants of obesity in Spanish children and young people. Br J Nutr 96: S67–72. [DOI] [PubMed] [Google Scholar]
- 62. Shehadeh N, Weitzer-Kish H, Shamir R, Shihab R, Weiss R (2008) Impact of early postnatal weight gain and feeding patterns on body mass index in adolescence. J Pediatr Endocrinol Metab 21: 9–15. [DOI] [PubMed] [Google Scholar]
- 63. Strufaldi MW, Silva EM, Franco MC, Puccini RF (2009) Blood pressure levels in childhood: probing the relative importance of birth weight and current size. Eur J Pediatr 168: 619–624. [DOI] [PubMed] [Google Scholar]
- 64. Sugimori H, Yoshida K, Miyakawa M, Izuno T, Kishimoto T, et al. (1997) Influence of behavioral and environmental factors on the development of obesity in three-year-old children. A case-control study based on Toyama Study. Environ Health Prev Med 2: 74–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Takahashi E, Yoshida K, Sugimori H, Miyakawa M, Izuno T, et al. (1999) Influence factors on the development of obesity in 3-year-old children based on the Toyama study. Prev Med 28: 293–296. [DOI] [PubMed] [Google Scholar]
- 66. Terry MB, Wei Y, Esserman D (2007) Maternal, birth, and early-life influences on adult body size in women. Am J Epidemiol 166: 5–13. [DOI] [PubMed] [Google Scholar]
- 67. Vohr BR, Lipsitt LP, Oh W (1980) Somatic growth of children of diabetic mothers with reference to birth size. J Pediatr 97: 196–199. [DOI] [PubMed] [Google Scholar]
- 68. Aarup M, Sokolowski I, Lous J (2008) The prevalence of obesity and overweight among 3 year-old children in the municipality of Aalborg and identification of risk factors (Danish). Ugeskr Laeger 170: 452–456. [PubMed] [Google Scholar]
- 69. Apfelbacher CJ, Loerbroks A, Cairns J, Behrendt H, Ring J, et al. (2008) Predictors of overweight and obesity in five to seven-year-old children in Germany: results from cross-sectional studies. BMC Public Health 8: 171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Armstrong J, Reilly JJ (2002) Child Health Information Team (2002) Breastfeeding and lowering the risk of childhood obesity. Lancet 359: 2003–2004. [DOI] [PubMed] [Google Scholar]
- 71. Barros AJ, Victora CG, Santos IS, Matijasevich A, Araújo Cl, et al. (2008) Infant malnutrition and obesity in three population-based birth cohort studies in Southern Brazil: trends and differences. Cad Saude Publica 24: S417–426. [DOI] [PubMed] [Google Scholar]
- 72. Barta L, Domján O (1965) Birthweight of obese and diabetic children. Acta Paediatr Acad Sci Hung 6: 163–170. [PubMed] [Google Scholar]
- 73. Barthel B, Cariou C, Lebas-Saison E, Momas I (2001) Prevalence of obesity in childhood: study in Paris elementary schools (French). Santé Publique 13: 7–15. [PubMed] [Google Scholar]
- 74. Burdette HL, Whitaker RC (2007) Differences by race and ethnicity in the relationship between breastfeeding and obesity in preschool children. Ethn Dis 17: 467–470. [PubMed] [Google Scholar]
- 75. Chen A, Pennell ML, Klebanoff MA, Rogan WJ, Longnecker MP (2006) Maternal smoking during pregnancy in relation to child overweight: follow-up to age 8 years. Int J Epidemiol 35: 121–130. [DOI] [PubMed] [Google Scholar]
- 76. Coy JF, Lewis IC, Mair CH, Longmore EA, Ratkowsky DA (1973) The growth of Tasmanian infants from birth to three years of age. Med J Aust 2: 12–18. [DOI] [PubMed] [Google Scholar]
- 77. Curhan GC, Willett WC, Rimm EB, Spiegelman D, Ascherio AL, et al. (1996) Birth weight and adult hypertension, diabetes mellitus, and obesity in US men. Circulation 94: 3246–3250. [DOI] [PubMed] [Google Scholar]
- 78. Danielzik S, Czerwinski-Mast M, Langnäse K, Dilba B, Müller MJ (2004) Parental overweight, socioeconomic status and high birth weight are the major determinants of overweight and obesity in 5-7 y-old children: baseline data of the Kiel Obesity Prevention Study (KOPS). Int J Obes 28: 1494–1502. [DOI] [PubMed] [Google Scholar]
- 79. Dennison BA, Edmunds LS, Stratton HH, Pruzek RM (2006) Rapid infant weight gain predicts childhood overweight. Obesity 14: 491–499. [DOI] [PubMed] [Google Scholar]
- 80. Dutra CL, Araújo CL, Bertoldi AD (2006) Prevalence of overweight in adolescents: a population-based study in a southern Brazilian city (Portuguese). Cad Saúde Pública 22: 151–162. [DOI] [PubMed] [Google Scholar]
- 81. Gallaher MM, Hauck FR, Yang-Oshida M, Serdula MK (1991) Obesity among mescalero preschool children. Association with maternal obesity and birth weight. Am J Dis Child 145: 1262–1265. [DOI] [PubMed] [Google Scholar]
- 82. Gigante DP, Victora CG, Araújo CLP, Barros FC (2003) Trends in the nutritional profile of children born in 1993 in Pelotas, Rio Grande do Sul, Brazil: Longitudinal analyses (Portuguese). Cad Saúde Pública 19: 141–147. [DOI] [PubMed] [Google Scholar]
- 83. Gigante DP, Minten GC, Horta BL, Barros FC, Victora CG (2008) [Nutritional evaluation follow-up of the 1982 birth cohort, Pelotas, Southern Brazil] (Portuguese). Rev Saude Publica 42: 60–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Gillman MW, Rifas-Shiman S, Berkey CS, Field AE, Colditz GA (2003) Maternal gestational diabetes, birth weight, and adolescent obesity. Pediatrics 111: 221–226. [DOI] [PubMed] [Google Scholar]
- 85. He Q, Ding ZY, Fong DY, Karlberg J (2000) Risk factors of obesity in preschool children in China: a population-based case-control study. Int J Obes 24: 1528–1536. [DOI] [PubMed] [Google Scholar]
- 86. Hirschler V, Bugna J, Roque M, Gilligan T, Gonzalez C (2008) Does low birth weight predict obesity/overweight and metabolic syndrome in elementary school children? Arch Med Res 39: 796–802. [DOI] [PubMed] [Google Scholar]
- 87. Hui LL, Nelson EA, Yu LM, Li AM, Fok TF (2003) Risk factors for childhood overweight in 6–7-y-old Hong Kong children. Int J Obes 27: 1411–1418. [DOI] [PubMed] [Google Scholar]
- 88. Kang HT, Ju YS, Park KH, Kwon YJ, Im HJ, et al. (2006) Study on the relationship between childhood obesity and various determinants, including socioeconomic factors, in an urban area (Korean). J Prev Med Pub Health 39: 371–378. [PubMed] [Google Scholar]
- 89. Kersey M, Lipton R, Sanchez-Rosado M, Kumar J, Thisted R (2005) Breast-feeding history and overweight in Latino preschoolers. Ambul Pediatr 5: 355–358. [DOI] [PubMed] [Google Scholar]
- 90. Kleiser C, Schaffrath Rosario A, Mensink BM G, Urban K, Bukowska C (2009) Potential determinants of obesity among children and adolescents in Germany: results from the cross-sectional KiGGS study. BMC Public Health 9: 46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Kniażewska M, Obuchowicz A, Żmudzińska-Kitczak J, Urban K, Bukowska C (2006) Assessment of association of birth weight and existence of hypertension in children and adolescents normostenic, obese or with metabolic syndrome. (Polish). Przegl Lek 63: 118–120. [PubMed] [Google Scholar]
- 92. Kromeyer-Hauschild K, Zellner K, Jaeger U, Hoyer H (1999) Prevalence of overweight and obesity among school children in Jena (Germany). Int J Obes 23: 1143–1150. [DOI] [PubMed] [Google Scholar]
- 93. Laitinen J, Power C, Jarvelin MR (2001) Family social class, maternal body mass index, childhood body mass index, and age of menarche as predictors of adult obesity. Am J Clin Nutr 74: 287–294. [DOI] [PubMed] [Google Scholar]
- 94. Maffeis C, Micciolo R, Must A, Zaffanello M, Pinelli L (1994) Parental and perinatal factors associated with childhood obesity in north-east Italy. Int J Obes 18: 301–305. [PubMed] [Google Scholar]
- 95. Mangrio E, Lindström M, Rosvall M (2010) Early life factors and being overweight at 4 years of age among children in Malmö, Sweden. BMC Public Health 10: 764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96. Mardones F, Villarroel L, Karzulovic L, Barja S, Arnaiz P (2008) Association of perinatal factors and obesity in 6- to 8-year-old Chilean children. Int J Epidemiol 37: 902–910. [DOI] [PubMed] [Google Scholar]
- 97. Mikulandra F, Grgurić J, Banović I, Perisa M, Zakanj Z (2000) The effect of high birth weight (4000 g or more) on weight and height of adult men and women. Coll Antropol 24: 133–136. [PubMed] [Google Scholar]
- 98. Miletić T, Mikulandra F, Stoini E, Anic J, Perisa M (2004) The relationship of birth weight and length to weight, height and body mass index in adult women. (Croatian). Gynaecol Perinatol 13: 13–5. [Google Scholar]
- 99. Monteiro POA, Victora CG, Barros FC, Monteiro LMA (2003) Birth size, early childhood growth, and adolescent obesity in a Brazilian birth cohort. Int J Obes 27: 1274–1282. [DOI] [PubMed] [Google Scholar]
- 100. Newby PK, Dickman PW, Adami HO, Wolk A (2005) Early anthropometric measures and reproductive factors as predictors of body mass index and obesity among older women. Int J Obes 29: 1084–1092. [DOI] [PubMed] [Google Scholar]
- 101. Oldroyd J, Renzaho A, Skouteris H (2010) Low and high birth weight as risk factors for obesity among 4 to 5-year-old Australian children: does gender matter? Eur J Pediatr 170: 899–906. [DOI] [PubMed] [Google Scholar]
- 102. Osler M, Lund R, Kriegbaum M, Andersen AM (2009) The influence of birth weight and body mass in early adulthood on early coronary heart disease risk among Danish men born in 1953. Eur J Epidemiol 24: 57–61. [DOI] [PubMed] [Google Scholar]
- 103. Padez C, Mourão I, Moreira P, Rosado V (2005) Prevalence and risk factors for overweight and obesity in Portuguese children. Acta Paediatr Int J Paediatr 94: 1550–1557. [DOI] [PubMed] [Google Scholar]
- 104. Panagiotakos DB, Papadimitriou A, Anthracopoulos MB, Konstantinidou M, Antonogeorgos G (2008) Birthweight, breast-feeding, parental weight and prevalence of obesity in schoolchildren aged 10-12 years, in Greece; the Physical Activity, Nutrition and Allergies in Children Examined in Athens (PANACEA) study. Pediatr Int 50: 563–568. [DOI] [PubMed] [Google Scholar]
- 105. Péter S, Bíró L, Németh A, Antal M (2008) Association between birth weight and childhood obesity in a Budapest metropolitan survey. (Hungarian). Orv Hetil. 149: 407–410. [DOI] [PubMed] [Google Scholar]
- 106. Phillips DIW, Young JB (2000) Birth weight, climate at birth and the risk of obesity in adult life. Int J Obes 24: 281–287. [DOI] [PubMed] [Google Scholar]
- 107. Pilpel D, Leer A, Phillip M (1995) Obesity among Jewish and Bedouin secondary school students in the Negev, Israel. Public Health Rev 23: 253–262. [PubMed] [Google Scholar]
- 108. Plagemann A, Harder T, Kohlhoff R, Rohde W, Dörner G (1997) Overweight and obesity in infants of mothers with long-term insulin-dependent diabetes or gestational diabetes. Int J Obes 21: 451–456. [DOI] [PubMed] [Google Scholar]
- 109. Reilly JJ, Armstrong J, Dorosty AR, Emmett PM, Ness A (2005) Early life risk factors for obesity in childhood: cohort study. BMJ 330: 1357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Rose D, Bodor JN (2006) Household food insecurity and overweight status in young school children: Results from the Early Childhood Longitudinal study. Pediatrics 117: 464–473. [DOI] [PubMed] [Google Scholar]
- 111. Schaefer-Graf UM, Pawliczak J, Passow D, Hartmann R, Rossi R (2005) Birth weight and parental BMI predict overweight in children from mothers with gestational diabetes. Diabetes Care. 28: 1745–1750. [DOI] [PubMed] [Google Scholar]
- 112. Seidman DS, Laor A, Gale R, Stevenson DK, Danon YL (1991) A longitudinal study of birth weight and being overweight in late adolescence. Am J Dis Child 145: 782–785. [PubMed] [Google Scholar]
- 113. Sørensen HT, Sabroe S, Rothman KJ, Gillman M, Fischer P, et al. (1997) Relation between weight and length at birth and body mass index in young adulthood: cohort study. BMJ 315: 1137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Stettler N, Bovet P, Shamlaye H, Zemel BS, Stallings VA, et al. (2002) Prevalence and risk factors for overweight and obesity in children from Seychelles, a country in rapid transition: the importance of early growth. Int J Obes 26: 214–219. [DOI] [PubMed] [Google Scholar]
- 115. Stettler N, Zemel BS, Kumanyika S, Stallings VA (2002) Infant weight gain and childhood overweight status in a multicenter, cohort study. Pediatrics 109: 194–199. [DOI] [PubMed] [Google Scholar]
- 116. Stettler N, Kumanyika SK, Katz SH, Zemel BS, Stallings VA (2003) Rapid weight gain during infancy and obesity in young adulthood in a cohort of African Americans. Am J Clin Nutr 77: 1374–1378. [DOI] [PubMed] [Google Scholar]
- 117. Sugihara S, Sasaki N, Amemiya S, Kohno H, Tanaka T (2008) Analysis of weight at birth and at diagnosis of childhood-onset type 2 diabetes mellitus in Japan. Pediatr Diabetes 9: 285–290. [DOI] [PubMed] [Google Scholar]
- 118. Takatani H, Okada T, Kaneda A (1967) Survey of infant obesity 3 years later. (Japanese). Nippon Shonika Gakkai Zasshi 71: 309–313. [PubMed] [Google Scholar]
- 119. Tene CE, Espinoza-Mejía MY, Silva-Rosales NA, Girón-Carrillo JL (2003) High birth weight as a risk factor for childhood obesity. (Spanish). Gac Med Mex 139: 15–20. [PubMed] [Google Scholar]
- 120. Tian JY, Cheng Q, Song XM, Li G, Jiang GX (2006) Birth weight and risk of type 2 diabetes, abdominal obesity and hypertension among Chinese adults. Eur J Endocrinol 155: 601–607. [DOI] [PubMed] [Google Scholar]
- 121. Tomé FS, Cardoso VC, Barbieri MA, Silva AA, Simões VM (2007) Are birth weight and maternal smoking during pregnancy associated with malnutrition and excess weight among school age children? Braz J Med Biol Res 40: 1221–1230. [DOI] [PubMed] [Google Scholar]
- 122. Toschke AM, Vignerova J, Lhotska L, Osancova K, Koletzko B, et al. (2002) Overweight and obesity in 6- to 14-year-old Czech children in 1991: protective effect of breast-feeding. J Pediatr 141: 764–769. [DOI] [PubMed] [Google Scholar]
- 123. Turkkahraman D, Bircan I, Tosun O, Saka O (2006) Prevalence and risk factors of obesity in school children in Antalya, Turkey. Saudi Med J 27: 1028–1033. [PubMed] [Google Scholar]
- 124. Verdy M, Gagnon MA, Caron D (1974) Birth weight and adult obesity in children of diabetic mothers. N Engl J Med 290: 576. [DOI] [PubMed] [Google Scholar]
- 125. Vitolo MR, Gama CM, Bortolini GA, Campagnolo PD, Drachler Mde L (2008) Some risk factors associated with overweight, stunting and wasting among children under 5 years old. J Pediatr (Rio J) 84: 251–257. [DOI] [PubMed] [Google Scholar]
- 126. von Kries R, Koletzko B, Sauerwald T, von Mutius E, Barnert D, et al. (1999) Breast feeding and obesity: cross sectional study. BMJ 319: 147–150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127. von Kries R, Toschke AM, Koletzko B, Slikker W (2002) Maternal smoking during pregnancy and childhood obesity. Am J Epidemiol 156: 954–961. [DOI] [PubMed] [Google Scholar]
- 128. Wang Y, Gao E, Wu J, Zhou J, Yang Q, et al. (2009) Fetal macrosomia and adolescence obesity: results from a longitudinal cohort study. Int J Obes 33: 923–928. [DOI] [PubMed] [Google Scholar]
- 129. Wei JN, Li HY, Sung FC, Lin CC, Chiang CC, et al. (2007) Birth weight correlates differently with cardiovascular risk factors in youth. Obesity 15: 1609–1616. [DOI] [PubMed] [Google Scholar]
- 130. Weyermann M, Rothenbacher D, Brenner H (2006) Duration of breastfeeding and risk of overweight in childhood: a prospective birth cohort study from Germany. Int J Obes 30: 1281–1287. [DOI] [PubMed] [Google Scholar]
- 131. Ylihärsilä H, Kajantie E, Osmond C, Forsén T, Barker DJ, et al. (2007) Birth size, adult body composition and muscle strength in later life. Int J Obes 31: 1392–1399. [DOI] [PubMed] [Google Scholar]
- 132. Yu Z, Sun JQ, Haas JD, Gu Y, Li Z, et al. (2008) Macrosomia is associated with high weight-for-height in children aged 1–3 years in Shanghai, China. Int J Obes 32: 55–60. [DOI] [PubMed] [Google Scholar]
- 133. Zhang X, Liu E, Tian Z, Wang W, Ye T, et al. (2009) High birth weight and overweight of obesity among Chinese children 3.6 years old. Preventive Medicine 49: 172–178. [DOI] [PubMed] [Google Scholar]
- 134. Huxley R, Neil A, Collins R (2002) Unravelling the fetal origins hypothesis: is there really an inverse association between birthweight and subsequent blood pressure? Lancet 360: 659–665. [DOI] [PubMed] [Google Scholar]
- 135. Huxley R, Owen CG, Whincup PH, Cook DG, Colman S, et al. (2004) Birth weight and subsequent cholesterol levels. Exploration of the “fetal origins” hypothesis. JAMA 292: 2755–2764. [DOI] [PubMed] [Google Scholar]
- 136. Harder T, Rodekamp E, Schellong K, Dudenhausen JW, Plagemann A (2007) Birth weight and subsequent risk of type 2 diabetes: a meta-analysis. Am J Epidemiol 165: 849–857. [DOI] [PubMed] [Google Scholar]
- 137. Whincup PH, Kaye SJ, Owen CG, Huxley R, Cook DG, et al. (2008) Birth weight and risk of type 2 diabetes. A systematic review. JAMA 300: 2886–2897. [DOI] [PubMed] [Google Scholar]
- 138. Plagemann A, Harder T (2009) Re: “Birth weight and risk of type 2 diabetes in adults” [letter]. JAMA 301: 1540–1541. [DOI] [PubMed] [Google Scholar]
- 139. Bhargava SK, Sachdev HS, Fall CHD, Osmond C, Lakshmy R, et al. (2004) Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med 350: 865–875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Lee CMY, Huxley RR, Wildman RP, Woodward M (2008) Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: a meta-analysis. J Clin Epidemiol 61: 646–653. [DOI] [PubMed] [Google Scholar]
- 141. Kilpeläinen TO, den Hoed M, Ong KK, Grøntved A, Brage S, et al. (2011) Obesity-susceptility loci have a limited influence on birth weight: a meta-analysis of up to 28,219 individuals. Am J Clin Nutr 93: 851–860. [DOI] [PubMed] [Google Scholar]
- 142. Hossain P, Kawar B, El Nahas M (2007) Obesity and diabetes in the developing world - a growing challenge. N Engl J Med 356: 213–215. [DOI] [PubMed] [Google Scholar]
- 143. Scully T (2012) Diabetes in numbers. Nature 485: S2–3. [DOI] [PubMed] [Google Scholar]
- 144.Freinkel N, Metzger BE (1979) Pregnancy as a tissue culture experience: the critical implications of maternal metabolism for fetal development. In: Pregnancy metabolism, diabetes, and the fetus. Ciba Foundation Symposium 63. Amsterdam: Excerpta Medica. pp 3–28. [DOI] [PubMed]
- 145. Freinkel N (1980) Of pregnancy and progeny. Diabetes 29: 1023–1035. [DOI] [PubMed] [Google Scholar]
- 146. Catalano P, Haughel-De Mouzon S (2011) Is it time to revisit the Pedersen hypothesis in the face of the obesity epidemic? Am J Obstet Gynecol 204: 479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Jovanovic L, Pettitt DJ (2001) Gestational diabetes mellitus. JAMA 286: 2516–2518. [DOI] [PubMed] [Google Scholar]
- 148. The HAPO study collaborative research group (2008) Hyperglycemia and adverse pregnancy outcomes. N Engl J Med 358: 1991–2002. [DOI] [PubMed] [Google Scholar]
- 149. Cedergren MI (2004) Maternal morbid obesity and the risk of adverse pregnancy outcome. Obstet Gynecol 103: 219–224. [DOI] [PubMed] [Google Scholar]
- 150. Sewell MF, Huston-Presley L, Super DM, Catalano P (2006) Increased neonatal fat mass, not lean body mass, is associated with maternal obesity. Am J Obstet Gynecol 195: 1100–1003. [DOI] [PubMed] [Google Scholar]
- 151. Crowther CA, Hiller JE, Moss JR, McPhee AJ, Jeffries WS, et al. (2005) Effect of treatment of gestational diabetes mellitus on pregnancy outcomes. N Engl J Med 352: 2477–2486. [DOI] [PubMed] [Google Scholar]
- 152. Landon MB, Spong CY, Thom E, Carpenter MW, Ramin SM, et al. (2009) A multicenter, randomized trial of treatment for mild gestational diabetes. N Engl J Med 361: 1339–1348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153. Pettitt DJ, Baird HR, Aleck KA, Bennett PH, Knowler WC (1983) Excessive obesity in offspring of Pima Indian women with diabetes during pregnancy. N Engl J Med 308: 242–245. [DOI] [PubMed] [Google Scholar]
- 154. Silverman BL, Metzger BE, Cho NH, Loeb CA (1995) Impaired glucose tolerance in adolescents offspring of diabetic mothers. Relationship to fetal hyperinsulinism. Diabetes Care 18: 611–617. [DOI] [PubMed] [Google Scholar]
- 155. Plagemann A, Harder T, Kohlhoff R, Rohde W, Dörner G (1997) Overweight and obesity in infants of mothers with long-term insulin-dependent diabetes or gestational diabetes. Int J Obes Relat Metab Disord 21: 451–456. [DOI] [PubMed] [Google Scholar]
- 156. Nelson SM, Matthews P, Poston L (2010) Maternal metabolism and obesity: modifiable determinants of pregnancy outcome. Hum Reprod Update 16: 255–275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157. Levin BE (2010) Developmental gene x environment interactions affecting systems regulating energy homeostasis and obesity. Front Neuroendocrinol 31: 270–283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158. Dörner G, Plagemann A (1994) Perinatal hyperinsulinism as possible predisposing factor for diabetes mellitus, obesity and enhanced cardiovascular risk in later life. Horm Metab Res 26: 213–221. [DOI] [PubMed] [Google Scholar]
- 159. Plagemann A (2008) A matter of insulin: Developmental programming of body weight regulation. J Mat Fet Med 21: 143–148. [DOI] [PubMed] [Google Scholar]
- 160. Van Assche FA, Holemans K, Aerts L (2001) Long-term consequences for offspring of diabetes during pregnancy. Br Med Bull 60: 173–182. [DOI] [PubMed] [Google Scholar]
- 161. Van Assche FA, Devlieger R, Harder T, Plagemann A (2010) Mitogenic effect of insulin and developmental programming. Diabetologia 53: 1243. [DOI] [PubMed] [Google Scholar]
- 162. Holemans K, Aerts L, Van Assche FA (1991) Evidence for an insulin resistance in the adult offspring of pregnant streptozotocin-diabetic rats. Diabetologia 34: 81–85. [DOI] [PubMed] [Google Scholar]
- 163. Stockard CR (1921) Developmental rate and structural expression: an experimental study of twins, “double monsters” and single deformities, and the interaction among embryonic organs during their origin and development. Am J Anat 28: 115–263. [Google Scholar]
- 164. Tzschentke B, Plagemann A (2006) Imprinting and critical periods in early development. World's Poult Sci J 62: 627–638. [Google Scholar]
- 165. Plagemann A, Harder T, Dudenhausen JW (2010) Re: “Childhood obesity, other cardiovascular risk factors, and premature death” [letter]. N Engl J Med 362: 1840–1841. [PubMed] [Google Scholar]
- 166. Harder T, Plagemann A, Harder A (2008) Birth weight and subsequent risk of childhood primary brain tumors: A meta-analysis. Am J Epidemiol 168: 366–373. [DOI] [PubMed] [Google Scholar]
- 167. Silva Idos S, De Stavola B (2008) McCormack V; Collaborative Group on Pre-Natal Risk Factors and Subsequent Risk of Breast Cancer (2008) Birth size and breast cancer risk: re-analysis of individual participant data from 32 studies. PLoS Med 5: e193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168. Ehemann C, Henly SJ, Ballard-Barbash R, Jacobs EJ, Schymura MJ, et al. (2012) Annual report to the nation on the status of cancer, 1975–2008, featuring cancers associated with excess weight and lack of sufficient physical activity. Cancer 118: 2338–2366. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
PRISMA checklist.
(DOC)
Study protocol for systematic review and meta-analysis to determine the relation between birth weight and long-term overweight risk.
(DOC)
Characteristics of 108 studies included in the systematic review of birth weight and subsequent risk of overweight, 1966–January 2011.
(DOC)
Studies that adjusted for confounders in the meta-analysis on birth weight and subsequent risk of overweight, 1966-January 2011.
(DOC)
Studies that reported data on neonatal weight gain or infant growth in the meta-analysis on birth weight and subsequent risk of overweight, 1966-January 2011.
(DOC)