Abstract
Background
Abnormal sleep duration, either long or short, is associated with disease risk and mortality. Little information is available on sleep duration and its correlates among Chinese women.
Methods
Using information collected from 68,832 women who participated in the Shanghai Women’s Health Study (SWHS), we evaluated sleep duration and its correlations with sociodemographic and lifestyle factors, health status, and anthropometric measurements and their indexes using polynomial logistic regression.
Results
The mean age of the study population was 59.6 years (SD=9.0; range: 44.6–79.9 years) at time of sleep duration assessment. Approximately 80% of women reported sleeping 6–8 hours per day, 11.5% slept five hours or less, and 8.7% slept nine hours or more. As expected, age was the strongest predictor for sleep duration and was negatively correlated with sleep duration. In general, sleep duration was positively associated with energy intake, intakes of total meat and fruits, body mass index (BMI), waist-hip ratio (WHR), and waist circumference (WC) after adjustment for age and other factors. Both short and long sleep duration were negatively associated with education level, family income, and leisure-time physical activity and positively associated with number of live births, history of night shift work, and certain chronic diseases, compared to sleep duration around seven hours/day (6.5–7.4 hours/day). Short sleep duration was related to tea consumption and passive smoking. Long sleep duration was related to menopausal status and marital status.
Conclusions
In this large, population-based study, we found that sleep duration among middle-aged and elderly Chinese women was associated with several sociodemographic and lifestyle factors and with disease status. The main limitation of the study is the cross-sectional design that does not allow us to draw any causal inference. However, this study provides information for future investigation into the nature of these associations so that recommendations can be developed to reduce sleep problems in middle-aged and elderly Chinese women. It also provides important information on potential confounders for investigation of sleep duration on health outcomes in this population.
Keywords: Sleep duration, socio-economic factor, lifestyle, health status, BMI, correlation, Chinese
INTRODUCTION
Duration of sleep is an important parameter in predicting not only the quality of sleep, but also quality of life, health status, and longevity [1–3]. Demographic characteristics such as race, age and gender, lifestyle, and health status have been previously shown to be associated with sleep duration [4]. Sleep duration and its correlates are known to vary from country to country [5].
Socioeconomic status indicators, including marital status, financial strain, education level, menopausal status, and history of night-shift work, have previously been related to sleep duration [6–7]. Other lifestyle factors have also been related to sleep duration among women, although the evidence is inconsistent. Smoking has been related to both short and long duration of sleep among Iranian women [8], but it was negatively related to sleep duration in England [9]. Total fat intake was associated with short sleep duration among post-menopausal women in the United States [10] and China [11], whereas energy intake was found to be unrelated to sleep duration among Greek women [12]. Recently, many studies have focused on the relationship between sleep and obesity and have shown that short sleep duration was associated with weight gain or obesity [13–15], while a study in Spain reported no association of sleep duration with waist circumference [16]. In addition, in a large US cohort study of adults aged 30–102 years, BMI was found to have a U-shaped relationship to sleep duration in women [17]. More importantly, sleep duration has been shown to relate to incidence and mortality from cancer and other common diseases, such as hypertension, diabetes, and coronary heart disease [18–21].
Despite abundant literature on sleep duration and its correlates in various populations, little information is available on sleep duration and its correlates among women in China. Using data from a population-based cohort study, we evaluated sleep duration and its correlates among middle-aged and elderly women in urban China. Our study did not provide any information about the directions and complexity of causal pathways from relations of sleep duration and various health factors. Therefore further cohort studies should be granted in this field.
METHODS
Participants
Included in current analysis were participants of the Shanghai Women’s Health Study (SWHS), a population-based prospective cohort study of women aged 40–70 years at baseline survey and conducted in seven urban communities of Shanghai, China. Details of the SWHS survey have been reported elsewhere [22]. Briefly, study enrollment took place between 1997 and 2000 with an overall response rate of 92.3%. Biennial in-person follow-up of all living cohort members was conducted by in-person interview from 2000 to 2002, 2002 to 2004, and 2004 to 2006 with response rates of 99.8%, 98.7%, and 95.2%, respectively. The study was approved by the relevant institutional review boards for human research in China and the United States and written, informed consent was obtained from all participants.
Data collection
A structured questionnaire was used at the baseline survey to collect information on socioeconomic status, living conditions, history of chronic disease, physical activity, family history, reproductive history, supplement intake, including vitamins and calcium, dietary habits, and anthropometric measurements. The follow-up surveys collected information on history of night-shift work, passive smoking, and occurrence of cancer and other chronic diseases, as well as survival status. Information on dietary intake, menopausal status, physical activity, and other lifestyle factors were updated at the follow-up surveys. History of night-shift work was defined as starting work after 10 PM at least three times per month for one year or longer. Dietary intake was assessed using a validated food frequency questionnaire (FFQ). For each food or food group, participants were asked how frequently (daily, weekly, monthly, yearly, or never) they consumed the food or food groups over the preceding year, followed by a question on the amount consumed in liang (1 liang=50g) per unit of time. The Chinese Food Composition Tables published in 2002 was used to estimate energy intake (kcal/day) and nutrients consumption based on information obtained from the FFQ. Anthropometric measurements, including height, weight, and circumferences of waist and hip, were taken at the baseline survey by trained interviewers. BMI was calculated as weight in kilograms divided by the square of height in meters, and WHR was calculated as waist circumference divided by hip circumference.
At the third follow-up, approximately four years after study enrollment, information on sleep duration was collected based on the following question: “In the past two years, how many hours did you sleep each day (including sleeping during the day and night, but not including time if you woke up between two periods of sleep)?” Participants reported their sleep duration and fractional-hour responses were rounded off at interview (e.g., seven hours represented responses from 6.5 hours and 7.4 hours). Among 69,775 participants who completed the third follow-up survey, we excluded 943 who did not provide sleep information. The remaining 68,832 participants were included in the current analysis.
Statistical analyses
Sleep duration each day was classified into seven categories: ≤four hours, five hours, six hours, seven hours, eight hours, nine hours, and ≥10 hours. Educational attainment level was divided into four categories: elementary school or under, middle school, high school, and college or above. Occupational status was categorized into four groups: professional, clerical, manual laborer, and housewife. Annual family income was reported in four categories: <10,000 yuan, 10,000–19,999 yuan, 20,000–29,999 yuan, and ≥30,000 yuan. A dichotomous variable was created for self-reported night-shift work history, Passive smoking, tea consumption, vitamin supplement, disease history (yes/no) and marital status: married or living together vs. single (not married, widowed, divorced, or separated). Number of live births was categorized into three groups: none or one, two, and ≥three. Hours spent watching television per day were classified into four groups: ≤two, three, four, ≥five. Dietary intake (total energy intake [kcal/day] and intakes of total meat [g/day], fruits [g/day], and vegetables [g/day]) and anthropometric measurements and their indexes (WC, BMI, and WHR) were all divided into quartiles. For the current analyses, data on education level, occupational status, family income, marital status, number of live births, and hours spent watching TV were collected at the baseline survey. Information for other variables were collected during follow-up surveys to minimize the interval of data collection between sleep duration assessment.
Variation of sleep duration by sociodemographic factors, lifestyle factors, and health status were adjusted for age at sleep duration assessment, i.e., time at the third follow-up, in a continuous scale. Odds ratios (ORs) for each sleep duration compared with the reference group (seven hours/day) and associated 95% confidence intervals (CIs) were calculated by using polynomial logistic regression models adjusted for potential confounders. We chose the sleep duration of seven hours/day as the reference group in the analysis because average sleep duration was 7.0 hours/day in our study. Variables were included in the multivariate analysis if they were related to sleep duration with adjustment for age (P<0.05) and if they were associated with sleep duration in the literature. In the analysis of lifestyle factors, we adjusted for the following covariates: education level, occupational status, history of night-shift work, family income, menopausal status, marital status, and number of live births. In analyses evaluating associations with health status and anthropometric measurements, the model was further adjusted for physical activity, passive smoking (exposure to smoking at home or at work), tea consumption, energy intake, hours spent watching TV per day, and vitamin supplement intake. Categorical variables were treated as continuous variables to obtain P-values for trend tests. P-values for all tests were two-tailed with a significance level of P <0.05. All analyses were performed using SAS statistical software (version 9.2; SAS Institute Inc. NC).
RESULTS
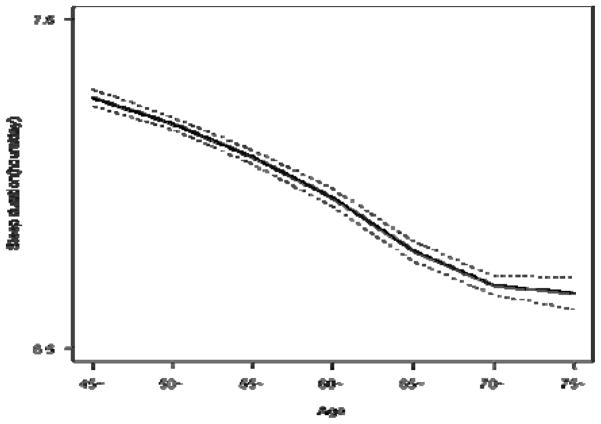
Table 1 presents selected characteristics of participants in the study. The average sleep duration was 7.0 hours in our study population. Approximately 80% of study participants reported daily sleep duration between six and eight hours, 11.5% reported short sleep duration (≤ five hours/day), and 8.7% reported long sleep duration (≥nine hours/day ). The mean age was 59.6 (SD=9.0). Among participants, 58% of them had low education levels and half of them had a family income under 20,000 yuans/year. Most of them were married and were in the post-menopausal stage. Figure 1 depicts the relations between age and sleep duration (hours/day). As expected, age was inversely correlated with sleep duration.
Table 1.
Selected characteristics of participants in the Shanghai Women’s Health Study.
| Characteristics | Statistics |
|---|---|
| Age at the third follow-up (years, x̄ ± SD) | 59.59±9.04 |
| BMI (x̄ ± SD) a,d | 24.02±3.42 |
| WHR ((x̄ ± SD) a | 0.81±0.05 |
| Waist circumference (cm, x̄ ± SD) a | 77.87±8.77 |
| Energy intake (kcal, x̄ ± SD)b | 1601.25±386.15 |
| Education level (%) a | |
| Middle school or under | 58.18 |
| High school or above | 41.42 |
| Family income (%, yuan) a | |
| <20,000 | 54.28 |
| ≥20,000 | 45.72 |
| Occupational status (%) a | |
| Professional | 28.50 |
| Clerical | 20.70 |
| Manual Laborer | 50.46 |
| Housewife | 0.34 |
| Exercise participation (%) d | 38.85 |
| History of night-shift work (%) c | 26.53 |
| Married (%) a | 89.16 |
| Post-menopausal status (%) d | 75.42 |
| Sleep duration (%) c | |
| <6 hours/day | 11.50 |
| 6–8 hours/day | 79.76 |
| >8 hours/day | 8.74 |
Data from baseline survey.
Data from the first follow-up.
Data from the second follow-up.
Data from the third follow-up.
Figure 1.
Means and 95% confidence intervals of sleep duration (hours/day) in each 5-year age group in the Shanghai Women’s Health Study
Table 2 presents associations between sleep duration and selected demographic characteristics. Age, occupation, history of night-shift work, and number of live births were associated with increased ORs for short sleep duration. Age showed the strongest correlation, with women aged 70 years or older having a 3-fold higher OR (OR=3.6, 95% CI=3.0–4.2) for sleep duration≤four hours, compared with women aged less than 50 years. Housewives had an about two-fold increased OR for short sleep duration compared with women who had professional jobs. Age, marriage, and menopausal status were associated with decreased ORs for long sleep duration, while occupation, history of night shift work, and number of live births were associated with increased ORs for long sleep duration. Education level and family income were inversely associated with both short and long sleep duration. Interestingly, there was no association between age and sleep duration among women aged 70 years or older.
Table 2.
Associations of sociodemographic characteristics and sleep duration (hours/day) using 7 hours/day as a reference, the Shanghai Women’s Health Study*.
| Duration<=4 Hr. (N=2011) | Duration=5 Hr. (N=5904) | Duration=6 Hr. (N=15627) | Duration=8 Hr. (N=20029) | Duration=9 Hr. (N=3751) | Duration>=10 Hr. (N=2268) | |
|---|---|---|---|---|---|---|
| Age at the third follow-up (years) | ||||||
| 44–49 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 50–59 | 0.94 (0.79–1.11) | 1.11 (1.00–1.23) | 1.09 (1.02–1.16) | 0.89 (0.84–0.94) | 0.88 (0.80–0.97) | 0.66 (0.58–0.74) |
| 60–69 | 1.81 (1.53–2.14) | 1.72 (1.54–1.91) | 1.39 (1.30–2.50) | 0.74 (0.69–0.79) | 0.77 (0.69–0.87) | 0.55 (0.47–0.63) |
| 70- | 3.58 (3.04–4.22) | 2.89 (2.61–3.21) | 1.86 (1.73–2.02) | 0.71 (0.66–0.76) | 0.91 (0.80–1.02) | 0.95 (0.83–1.08) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | 0.023 | 0.399 |
| Education level a | ||||||
| Elementary or under | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Middle school | 0.62 (0.54–0.71) | 0.83 (0.75–0.91) | 0.93 (0.86–1.00) | 0.93 (0.87–1.00) | 0.80 (0.71–0.91) | 0.65 (0.56–0.75) |
| High school | 0.40 (0.35–0.47) | 0.68 (0.61–0.74) | 0.87 (0.81–0.94) | 0.87 (0.81–0.94) | 0.70 (0.62–0.80) | 0.45 (0.39–0.52) |
| College or above | 0.29 (0.24–0.35) | 0.54 (0.48–0.60) | 0.80 (0.74–0.86) | 0.81 (0.75–0.87) | 0.61 (0.54–0.70) | 0.23 (0.18–0.28) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Occupational status a | ||||||
| Professional | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Clerical | 1.70 (1.47–1.97) | 1.31 (1.20–1.44) | 1.04 (0.98–1.10) | 1.04 (0.98–1.10) | 1.13 (1.02–1.25) | 1.96 (1.71–2.25) |
| Manual Laborer | 1.91 (1.63–2.15) | 1.51 (1.41–1.63) | 1.11 (1.05–1.16) | 1.11 (1.06–1.16) | 1.26 (1.16–1.37) | 2.22 (1.97–2.50) |
| Housewife | 3.35 (1.89–5.91) | 2.07 (1.31–3.26) | 1.35 (0.92–1.99) | 1.10 (0.72–1.67) | 2.04 (1.13–3.67) | 5.73 (3.25–10.1) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| History of night-shift work c | ||||||
| Never | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Ever | 1.48 (1.34–1.64) | 1.26 (1.18–1.34) | 1.10 (1.05–1.16) | 1.02 (0.97–1.07) | 1.04 (0.96–1.13) | 1.22 (1.11–1.35) |
| Family income (yuan) a | ||||||
| <10,000 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 10,000–20,000 | 0.77 (0.68–0.87) | 0.92 (0.84–1.00) | 0.94 (0.89–1.01) | 0.95 (0.89–1.01) | 0.92 (0.82–1.02) | 0.73 (0.65–0.82) |
| 20,000–30,000 | 0.56 (0.48–0.64) | 0.77 (0.70–0.84) | 0.88 (0.82–0.94) | 0.92 (0.87–0.98) | 0.86 (0.77–0.96) | 0.52 (0.46–0.60) |
| >30,000 | 0.52 (0.46–0.60) | 0.69 (0.62–0.76) | 0.82 (0.76–0.88) | 0.86 (0.80–0.92) | 0.76 (0.67–0.86) | 0.39 (0.33–0.45) |
| P for trend | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
| Married a | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.95 (0.83–1.10) | 0.91 (0.83–1.00) | 0.96 (0.90–1.03) | 0.99 (0.93–1.06) | 0.94 (0.84–1.06) | 0.72 (0.63–0.83) |
| Menopausal statusd | ||||||
| Premenopausal | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Postmenopausal | 0.95 (0.80–1.17) | 0.97 (0.87–1.07) | 1.03 (0.96–1.09) | 0.90 (0.85–0.95) | 0.77 (0.70–0.85) | 0.57 (0.50–0.65) |
| No. of live births a | ||||||
| 0–1 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 2 | 0.99 (0.86–1.15) | 1.07 (0.97–1.16) | 1.02 (0.95–1.09) | 1.00 (0.94–1.06) | 0.97 (0.87–1.08) | 1.03 (0.89–1.18) |
| ≥ 3 | 1.62 (1.37–1.92) | 1.39 (1.24–1.55) | 1.13 (1.04–1.23) | 1.15 (1.06–1.25) | 1.27 (1.10–1.47) | 2.04 (1.70–2.45) |
| P for trend | <0.001 | <0.001 | 0.008 | 0.003 | 0.005 | <0.001 |
Odds ratios and 95% confidence intervals were estimated using multinomial logistic regression adjusting for continuous age at the third follow-up.
Data from the baseline survey.
Data from the second follow-up.
Data from the third follow-up.
Table 3 presents associations between sleep duration and lifestyle factors. Exercise was negatively related with both short and long sleep duration. Tea consumption, energy, and intake of fruit were inversely associated with short sleep duration. Passive smoking, and spending more than five hours per day watching TV were positively associated with short sleep duration. Different association patterns were observed for long duration of sleep. Time spent watching TV, tea consumption, intakes of meat, fruits, and vegetables, and total energy intake were not related to long sleep duration, whereas vitamin supplement users were less likely to report long sleep duration.
Table 3.
Associations of lifestyle factors and sleep duration (hours/day) using 7 hours/day as a reference, the Shanghai Women’s Health Study*.
| Duration<=4 Hr. (N=2011) | Duration=5 Hr. (N=5904) | Duration=6 Hr. (N=15627) | Duration=8 Hr. (N=20029) | Duration=9 Hr. (N=3751) | Duration>=10 Hr. (N=2268) | |
|---|---|---|---|---|---|---|
| Exercise participation d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.84 (0.76–0.92) | 0.94 (0.88–1.00) | 0.96 (0.92–1.00) | 0.96 (0.92–1.00) | 1.00 (0.93–1.08) | 0.75 (0.68–0.83) |
| Physical activity (hours/week) d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 0.1–6.9 | 0.90 (0.79–1.02) | 0.96 (0.89–1.04) | 0.96 (0.90–1.02) | 0.96 (0.91–1.02) | 1.02 (0.92–1.12) | 0.74 (0.65–0.85) |
| ≥ 7.0 | 0.79 (0.70–0.89) | 0.92 (0.86–0.99) | 0.96 (0.91–1.01) | 0.96 (0.91–1.01) | 0.99 (0.91–1.09) | 0.76 (0.67–0.85) |
| P for trend | <0.001 | 0.028 | 0.077 | 0.087 | 0.961 | <0.001 |
| Passive smoking b | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.16 (1.03–1.30) | 1.05 (0.98–1.13) | 1.04 (0.99–1.10) | 0.96 (0.92–1.02) | 0.90 (0.83–0.99) | 0.96 (0.86–1.07) |
| Tea consumption b | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 0.73 (0.65–0.82) | 0.80 (0.74–0.85) | 0.89 (0.85–0.93) | 1.06 (1.02–1.11) | 1.02 (0.95–1.11) | 1.06 (0.96–1.17) |
| Time spent watching TV a | ||||||
| ≤ 2 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 3 | 0.93 (0.82–1.05) | 0.96 (0.89–1.05) | 1.00 (0.94–1.06) | 0.97 (0.92–1.03) | 0.94 (0.86–1.04) | 0.90 (0.80–1.02) |
| 4 | 0.90 (0.79–1.03) | 1.02 (0.94–1.11) | 1.03 (0.97–1.09) | 0.97 (0.92–1.03) | 0.92 (0.83–1.01) | 0.94 (0.83–1.07) |
| ≥ 5 | 1.11 (0.98–1.27) | 1.19 (1.09–1.29) | 1.12 (1.05–1.19) | 1.00 (0.94–1.05) | 0.91 (0.82–1.00) | 1.09 (0.96–1.23) |
| P for trend | 0.211 | <0.001 | <0.001 | 0.765 | 0.043 | 0.200 |
| Vitamin supplement use b | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.10 (0.99–1.22) | 1.05 (0.98–1.12) | 1.01 (0.97–1.06) | 0.88 (0.84–0.92) | 0.89 (0.82–0.96) | 0.80 (0.73–0.89) |
| Energy intake (kcal/day) b | ||||||
| <1339.13 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 1339.13- | 0.88 (0.78–1.00) | 0.96 (0.89–1.04) | 0.99 (0.93–1.05) | 1.01 (0.95–1.07) | 0.96 (0.87–1.06) | 0.99 (0.87–1.11) |
| 1566.45- | 0.86 (0.75–0.97) | 0.93 (0.86–1.01) | 0.94 (0.89–1.00) | 1.00 (0.94–1.05) | 1.05 (0.95–1.15) | 0.84 (0.74–0.95) |
| ≥1823.35 | 0.87 (0.76–0.99) | 0.94 (0.86–1.02) | 0.94 (0.88–0.99) | 1.05 (0.99–1.11) | 1.13 (1.02–1.05) | 1.12 (1.00–1.27) |
| P for trend | 0.002 | 0.002 | <0.001 | 0.028 | 0.007 | 0.152 |
| Total meat intake (g/day) b | ||||||
| <62.00 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 62.00- | 0.91 (0.80–1.03) | 1.00 (0.92–1.08) | 1.04 (0.98–1.11) | 0.93 (0.88–0.99) | 0.99 (0.89–1.09) | 0.88 (0.78–1.00) |
| 95.51- | 0.88 (0.78–1.00) | 0.98 (0.90–1.06) | 0.97 (0.91–1.02) | 0.97 (0.92–1.02) | 1.05 (0.95–1.16) | 0.91 (0.80–1.03) |
| ≥ 140.94 | 0.97 (0.85–1.11) | 0.98 (0.90–1.07) | 0.99 (0.93–1.05) | 1.01 (0.96–1.07) | 1.11 (1.01–1.23) | 1.08 (0.96–1.22) |
| P for trend | 0.130 | 0.054 | 0.062 | 0.136 | 0.040 | 0.148 |
| Total vegetable intake (g/day)b | ||||||
| <188.80 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 188.80- | 0.89 (0.78–1.01) | 0.96 (0.88–1.04) | 0.96 (0.91–1.02) | 0.96 (0.91–1.01) | 0.94 (0.85–1.04) | 0.87 (0.77–0.99) |
| 278.12- | 0.89 (0.79–1.02) | 1.01 (0.93–1.09) | 0.95 (0.90–1.01) | 0.96 (0.91–1.01) | 1.01 (0.91–1.11) | 0.90 (0.79–1.01) |
| ≥394.95 | 1.00 (0.88–1.13) | 1.04 (0.96–1.13) | 0.97 (0.91–1.03) | 0.99 (0.93–1.04) | 1.08 (0.98–1.19) | 1.01 (0.90–1.14) |
| P for trend | 0.376 | 0.899 | 0.047 | 0.853 | 0.085 | 0.619 |
| Total fruit intake (g/day) b | ||||||
| <114.51 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 114.51- | 0.91 (0.80–1.03) | 0.96 (0.89–1.04) | 0.96 (0.91–1.02) | 0.93 (0.88–0.98) | 1.04 (0.94–1.15) | 0.80 (0.71–0.90) |
| 198.81- | 0.77 (0.67–0.88) | 0.90 (0.83–0.98) | 0.96 (0.90–1.02) | 0.97 (0.91–1.02) | 1.05 (0.95–1.16) | 0.83 (0.73–0.94) |
| ≥293.91 | 0.98 (0.86–1.12) | 0.88 (0.81–0.96) | 0.95 (0.89–1.01) | 0.99 (0.94–1.05) | 1.12 (1.01–1.23) | 1.02 (0.91–1.15) |
| P for trend | 0.046 | <0.001 | 0.007 | 0.546 | 0.056 | 0.638 |
Odds ratios and 95% confidence intervals were estimated using multinomial logistic regression adjusted for age at the third follow-up, education level, occupational status, history of night-shift work, annual income, menopausal status, marital status, and number of live births.
Data from the baseline survey.
Data from the first follow-up.
Data from the third follow-up.
Table 4 presents relationships between sleep duration and health conditions and anthropometric measurements. There were U-shaped associations between prevalence of hypertension, coronary disease, stroke, diabetes, hyperlipidemia, fatty liver, cancer, and bone fracture and sleep duration. Gout, asthma, and chronic bronchitis were only correlated with short sleep duration. Participants who had higher measurements for BMI, WHR, or WC were less likely to have short sleep duration and more likely to have long sleep duration. We conducted additional analyses stratified by age and found no modification of the associations presented in Tables 2 to 4 (data not shown).
Table 4.
Associations of health conditions and anthropometric measurements and sleep duration (hours/day) using 7 hours/day as a reference, the Shanghai Women’s Health Study*.
| Duration<=4 Hr. (N=2011) | Duration=5 Hr. (N=5904) | Duration=6 Hr. (N=15627) | Duration=8 Hr. (N=20029) | Duration=9 Hr. (N=3751) | Duration>=10 Hr. (N=2268) | |
|---|---|---|---|---|---|---|
| Hypertension a,b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.19 (1.07–1.32) | 1.05 (0.98–1.12) | 1.03 (0.98–1.08) | 1.04 (1.00–1.09) | 1.10 (1.01–1.18) | 1.17 (1.06–1.29) |
| Coronarya,b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.46 (1.26–1.70) | 1.28 (1.15–1.43) | 1.11 (1.02–1.21) | 0.95 (0.86–1.03) | 1.07 (0.92–1.25) | 1.41 (1.19–1.67) |
| Strokea,b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.75 (1.49–2.07) | 1.37 (1.21–1.55) | 1.16 (1.05–1.29) | 1.05 (0.94–1.17) | 1.07 (0.89–1.29) | 1.88 (1.56–2.27) |
| Diabetes a,b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.22 (1.05–1.42) | 1.18 (1.07–1.31) | 1.05 (0.96–1.13) | 1.17 (1.08–1.26) | 1.17 (1.02–1.33) | 1.68 (1.45–1.95) |
| Goutd | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.81 (1.21–2.70) | 1.44 (1.07–1.95) | 1.21 (0.94–1.56) | 0.96 (0.74–1.26) | 1.16 (0.75–1.80) | 1.49 (0.92–2.41) |
| Hyperlipidemia d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.65 (1.45–1.87) | 1.50 (1.37–1.63) | 1.15 (1.07–1.22) | 0.97 (0.91–1.04) | 1.10 (0.99–1.24) | 1.24 (1.08–1.43) |
| Fatty liver d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.58 (1.38–1.80) | 1.30 (1.19–1.42) | 1.12 (1.04–1.19) | 1.07 (1.00–1.14) | 1.16 (1.04–1.30) | 1.29 (1.12–1.48) |
| Chronic bronchitis a | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.40 (1.19–1.64) | 1.43 (1.29–1.59) | 1.21 (1.11–1.31) | 0.99 (0.91–1.08) | 1.12 (0.98–1.30) | 0.86 (0.71–1.05) |
| Asthmaa | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.73 (1.31–2.29) | 1.53 (1.26–1.87) | 1.32 (1.13–1.53) | 1.07 (0.92–1.25) | 1.04 (0.80–1.36) | 1.16 (0.84–1.59) |
| Personal history of cancer b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.58 (1.32–1.89) | 1.12 (0.99–1.27) | 1.14 (1.05–1.25) | 0.96 (0.89–1.05) | 1.02 (0.88–1.18) | 1.42 (1.20–1.67) |
| Bone fracture b,c,d | ||||||
| No | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| Yes | 1.50 (1.30–1.73) | 1.31 (1.19–1.45) | 1.13 (1.05–1.22) | 1.06 (0.99–1.15) | 1.04 (0.92–1.19) | 1.22 (1.04–1.42) |
| Body measurements | ||||||
| BMI (kg/m2) a,d | ||||||
| <21.64 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 21.64- | 0.86 (0.74–0.98) | 0.86 (0.79–0.94) | 0.91 (0.86–0.97) | 0.98 (0.92–1.04) | 1.00 (0.91–1.11) | 0.89 (0.78–1.02) |
| 23.73- | 0.80 (0.70–0.92) | 0.82 (0.75–0.90) | 0.93 (0.88–0.99) | 1.05 (0.99–1.12) | 1.00 (0.90–1.11) | 1.04 (0.91–1.19) |
| ≥ 26.09 | 0.78 (0.68–0.89) | 0.81 (0.74–0.89) | 0.94 (0.88–1.00) | 1.09 (1.02–1.16) | 1.07 (0.96–1.19) | 1.34 (1.17–1.52) |
| P for trend | <0.001 | <0.001 | 0.111 | 0.001 | 0.274 | <0.001 |
| WHR a | ||||||
| <0.77 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 0.77- | 0.98 (0.85–1.13) | 0.94 (0.86–1.03) | 1.00 (0.94–1.06) | 1.01 (0.96–1.07) | 1.07 (0.96–1.18) | 1.05 (0.92–1.20) |
| 0.81- | 0.84 (0.72–0.98) | 0.92 (0.83–1.01) | 1.00 (0.93–1.07) | 1.06 (0.99–1.12) | 1.10 (0.98–1.23) | 1.12 (0.96–1.29) |
| ≥ 0.84 | 0.94 (0.81–1.09) | 0.90 (0.82–0.98) | 1.00 (0.93–1.07) | 1.12 (1.05–1.19) | 1.20 (1.08–1.34) | 1.44 (1.25–1.65) |
| P for trend | 0.235 | <0.017 | 0.919 | <0.001 | 0.001 | <0.001 |
| WC (cm) a | ||||||
| <72 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 | 1.0 |
| 72- | 0.82 (0.70–0.95) | 0.85 (0.77–0.93) | 0.99 (0.93–1.06) | 1.01 (0.95–1.08) | 1.02 (0.92–1.14) | 0.92 (0.80–1.06) |
| 77- | 0.79 (0.68–0.91) | 0.88 (0.81–0.96) | 0.96 (0.90–1.03) | 1.04 (0.98–1.11) | 1.04 (0.93–1.15) | 1.00 (0.87–1.15) |
| ≥ 83 | 0.83 (0.72–0.95) | 0.81 (0.74–0.89) | 1.01 (0.95–1.08) | 1.11 (1.04–1.18) | 1.18 (1.06–1.31) | 1.50 (1.32–1.72) |
| P for trend | 0.014 | <0.001 | 0.946 | <0.001 | 0.004 | <0.001 |
Odds ratios and 95% confidence intervals were estimated using multinomial logistic regression adjusted for age at the third follow-up, education level, occupational status, history of night-shift work, annual income, menopausal status, marital status, number of live births, physical activity, passive smoking, tea consumption, energy intake, time spent watching TV, and vitamin supplement use.
Data from baseline survey.
Data from the first follow-up.
Data from the second follow-up.
Data from the third follow-up.
DISCUSSION
In this cohort of women aged 44.6–79.9 years living in urban Shanghai, we found that 79.8% of women slept about six-eight hours per day, 11.5% slept five hours or less, and 8.7% slept nine hours or more. These statistics are similar to those reported in Krueger’s study of 110,441 people in America, in which 8.5% of them slept 9 or more hours [23]. As expected, we found that age was the most significant predictor and was inversely correlated with sleep duration. Several sociodemographic factors, lifestyle factors, medical conditions, and anthropometric measurements were found to be correlated with either short or long sleep duration. To our knowledge, this is the first study to comprehensively evaluate sleep duration and its correlates in a population-based study of middle-aged and older Chinese women.
A finding of negative correlation between age and sleep duration in our study was consistent with previous studies showing that changes in sleep quality and quantity accompany aging [24]. In a meta-analysis of 65 studies involving 3,577 subjects aged 5–102 years, it was found that both total sleep duration and sleep efficiency decreased with age because of increase with age of time awake after sleep onset or sleep latency [25]. Lauderdale and colleagues reported that age was inversely related with time in bed and sleep duration among the 699 participants of the Coronary Artery Risk Development in Young Adults (CARDIA) study [26]. However, in the National Health Interview Survey (NHISs) of 71,455 participants aged 18 years and above, Fang and colleagues found that sleep duration was positively associated with age [27]. This association was also found by Magee et al. among middle aged and elderly Australians [28]. But in the Whitehall II study in France an association between age and sleep duration was found only in male participants [29]. Krueger and colleagues reported that ORs for long sleep duration were highest among both the youngest and oldest individuals and were lowest among those aged 45 years [23]. These inconsistent results may be due to different ethnic and cultural influences or lifestyles. Further studies are required to investigate these influences on association between age and sleep duration.
In our study, we found that sleep duration was associated with several lifestyle factors and these findings are, in general, consistent with prior research findings [26,30]. We found that short sleep duration was inversely associated with tea consumption. This finding is comparable to findings of a French study in which habitual consumption of up to seven cups of coffee per day was not associated with decreased duration of sleep, although caffeine in both tea and coffee is known to have sleep-reducing effects [31]. A possible explanation for our finding and the finding from the French study is the development of a tolerance to the sleep-reducing effects of caffeine, since the women in these studies were habitual consumers of tea or coffee [32]. This result expressed that tea consumption is one of the correlates of sleep duration in Chinese women. Further study on the association between sleep duration and tea consumption is necessary to get causal inference. In the US Nurses’ Health Study, night-shift workers were found to sleep less [33]. Ohayon and colleagues reported that regular night-shift workers and those who worked night shifts regularly but on a rotating schedule reported short sleep duration (<six hours), with significant ORs of 1.7 and 1.9, respectively [34]. Data from our study support the finding mentioned above. Night-shift work may disrupt the body’s circadian rhythm and has a wide range of health impacts on night-shift workers [35], since a long history of night-shift work may induce sleep disorders. Previous studies have shown that exercises such as Tai Chi increased sleep duration [36] and that women who were physically active slept longer than sedentary women [37], which is similar to our finding that exercise (including Tai Chi) appeared to improve sleep duration among participants with short sleep duration. In our study, 30% of participants regularly used nutritional supplements, including multi-vitamins. Vitamin users were more likely to sleep less than non-users of vitamins. Lichstein also found that use of a multi-vitamin or multiple single vitamins was associated with poorer sleep maintenance in a survey of 772 participants in the US [38]. A plausible explanation for this association is reverse causation – that is, women with insomnia or poor health took vitamin supplements to improve their sleep quality.
Total energy intake and total fruit intake were associated with long sleep duration and were inversely associated with short sleep duration, while intakes of total meat and vegetables were not associated with sleep duration in our study. Our results are similar to Shi and colleagues’ study conducted in China, which indicated that total energy intake is positively correlated with self-reported sleep duration [11]. However, a negative correlation between actigraphic sleep duration and energy intake was found among post-menopausal women in the US [10] and no relation was found among Greek women [12]. Many studies have investigated the association between sleep duration and obesity but the results were inconsistent. In our study, high body mass index (BMI), waist-hip ratio (WHR), and waist circumference (WC) were associated with long sleep duration after adjustment for energy intake and other confounders. In a cohort study evaluating cancer risk in Japan, short sleep duration was associated with lower BMI [39]. Other studies have reported no association [5, 40–41], a U-shaped association [17,42], or an inverse association [43–44] between sleep duration and BMI or other anthropometric measurements. Interestingly, in America, several studies reported that short sleep duration is a risk factor for obesity in children, adolescents, and adults in both cross-sectional studies and cohort studies [45–47]. A recent study in America, which included 56,507 observations in patients aged 18–85 years in the US National Health Interview Survey during 2005–2006, reported that short sleep is strongly associated with obesity after adjusting for individual characteristics, health behaviors, family environment, and census region [48]. Sleep is a complicated physical process. The low rate of obesity and lack of morbid obesity in our study population may result in different association patterns between sleep duration and BMI compared to studies in Anerica. In addition, the relation between sleep duration and BMI could be reciprocal. Thus, further physiologic studies are warranted to better understand the effect of sleep duration on weight regulation, especially among different countries.
Impaired ability to initiate, maintain, and ultimately achieve good quality, optimal sleep may be a marker of increased mortality and neurocognitive dysfunction in the elderly [49]. Our study revealed that many chronic diseases, such as hypertension, diabetes, and coronary heart disease, were positively associated with short and long sleep duration. Tuomilehto and colleagues reported that both short and long sleep duration were associated with diabetes and serum levels of lipids and lipoproteins [21]. Increasing sleep duration was associated with lower breast cancer risk among Chinese women in Singapore [18], but with a higher risk among American women [19]. Short and long sleep duration have been associated with not only incidence, but also mortality from cardiovascular disease in various countries [20,50]. Sleep duration has been related to overall mortality in numerous prospective studies [3–4,35].
Advantages of our study include its large size, population-based design, and comprehensive assessment of a wide range of lifestyle factors and health conditions. However, there are also some limitations to consider. 1) Sleep duration is a complex physical process that is strongly influenced by many factors, such as psychology, sleeping habits, sleep disorders, sleep medication, and type and severity of disease and associated treatments. These unmeasured factors could confound the associations under study. 2) Current study is more likely to be a cross-sectional design that does not allow us to draw any causal inference. Therefore, future prospective studies should be applied to confirm the association between exposures and sleep duration. 3) In our study population, most women practice exercise, including Tai Chi, outdoors in the early morning. It is likely that these women would have more exposure to daylight. But we did not collect the information on when women went to bed and got up in the morning and, therefore, can’t access the influence of daylight exposure on sleep duration. 4) Sleep duration was derived from a self-reported questionnaire item without investigating questionnaire reliability or objective sleep patterns, which may also have introduced bias. Lauderdale and colleagues reported a moderate correlation between self-reported sleep duration and actigraph-measures of sleep duration of 0.47 [51]. Categorizing sleep duration in the data analysis would reduce bias in association estimates.
In conclusion, we evaluated sleep duration and its correlates in middle-aged and elderly Chinese women participating in a population-based cohort study and found that age is the strongest predictor of sleep duration in this population. Less than optimal sociodemographics, an unhealthy lifestyle and poor health conditions were related to short and long sleep duration. Obesity was associated with long sleep duration. These findings provide important information for future investigation of the causes of sleep duration and sleep quality, as well as sleep-health risk associations.
Acknowledgments
Our study was supported by research grants R37 CA070867 from the National Institutes of Health. All authors in this study have no financial conflicts of interest.
Footnotes
All authors in this study have no financial conflicts of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Groeger JA, Zijlstra FR, Dijk DJ. Sleep quantity, sleep difficulties and their perceived consequences in a representative sample of some 2000 British adults. J Sleep Res. 2004;13:359–71. doi: 10.1111/j.1365-2869.2004.00418.x. [DOI] [PubMed] [Google Scholar]
- 2.Parish JM. Sleep-related problems in common medical conditions. Chest. 2009;135:563–72. doi: 10.1378/chest.08-0934. [DOI] [PubMed] [Google Scholar]
- 3.Patel SR, Ayas NT, Malhotra MR, White DP, Schernhammer ES, Speizer FE, et al. A prospective study of sleep duration and mortality risk in women. Sleep. 2004;27:440–4. doi: 10.1093/sleep/27.3.440. [DOI] [PubMed] [Google Scholar]
- 4.Kripke DF, Jean-Louis G, Elliott JA, Klauber MR, Rex KM, Tuunainen A, et al. Ethnicity, sleep, mood, and illumination in postmenopausal women. BMC Psychiatry. 2004;4:8. doi: 10.1186/1471-244X-4-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ohayon MM. Interactions between sleep normative data and sociocultural characteristics in the elderly. J Psychosom Res. 2004;56:479–86. doi: 10.1016/j.psychores.2004.04.365. [DOI] [PubMed] [Google Scholar]
- 6.Kalleinen N, Polo-Kantola P, Himanen SL, Alhola P, Joutsen A, Urrila AS, et al. Sleep and the menopause - do postmenopausal women experience worse sleep than premenopausal women? Menopause Int. 2008;14:97–104. doi: 10.1258/mi.2008.008013. [DOI] [PubMed] [Google Scholar]
- 7.Sudo N, Ohtsuka R. Sleep patterns and sleep disorders among female shift workers in a computer factory of Japan. J Hum Ergol (Tokyo) 1999;28:39–47. [PubMed] [Google Scholar]
- 8.Sarrafzadegan N, Toghianifar N, Roohafza H, Siadat Z, Mohammadifard N, O’Loughlin J. Lifestyle-related determinants of hookah and cigarette smoking in Iranian adults. J Community Health. 2010;35:36–42. doi: 10.1007/s10900-009-9186-0. [DOI] [PubMed] [Google Scholar]
- 9.Palmer CD, Harrison GA, Hiorns RW. Association between smoking and drinking and sleep duration. Ann Hum Biol. 1980;7:103–7. doi: 10.1080/03014468000004111. [DOI] [PubMed] [Google Scholar]
- 10.Grandner MA, Kripke DF, Naidoo N, Langer RD. Relationships among dietary nutrients and subjective sleep, objective sleep, and napping in women. Sleep Med. 2010;11:180–4. doi: 10.1016/j.sleep.2009.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Shi Z, McEvoy M, Luu J, Attia J. Dietary fat and sleep duration in Chinese men and women. Int J Obes (Lond) 2008;32:1835–40. doi: 10.1038/ijo.2008.191. [DOI] [PubMed] [Google Scholar]
- 12.Rontoyanni VG, Baic S, Cooper AR. Association between nocturnal sleep duration, body fatness, and dietary intake in Greek women. Nutrition. 2007;23:773–7. doi: 10.1016/j.nut.2007.07.005. [DOI] [PubMed] [Google Scholar]
- 13.Theorell-Haglow J, Berne C, Janson C, Sahlin C, Lindberg E. Associations between short sleep duration and central obesity in women. Sleep. 2010;33:593–8. [PMC free article] [PubMed] [Google Scholar]
- 14.St-Onge M-P, Perumean-Chaney S, Desmond R, Lewis CE, Yan LL, Person SD, et al. Gender Differences in the Association between Sleep Duration and Body Composition: The Cardia Study. Int J Endocrinol. 2010;2010:1–8. doi: 10.1155/2010/726071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Park SE, Kim HM, Kim DH, Kim J, Cha BS, Kim DJ. The association between sleep duration and general and abdominal obesity in Koreans: data from the Korean National Health and Nutrition Examination Survey, 2001 and 2005. Obesity (Silver Spring) 2009;17:767–71. doi: 10.1038/oby.2008.586. [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Garcia E, Faubel R, Leon-Munoz L, Zuluaga MC, Banegas JR, Rodriguez-Artalejo F. Sleep duration, general and abdominal obesity, and weight change among the older adult population of Spain. Am J Clin Nutr. 2008;87:310–6. doi: 10.1093/ajcn/87.2.310. [DOI] [PubMed] [Google Scholar]
- 17.Kripke DF, Garfinkel L, Wingard DL, Klauber MR, Marler MR. Mortality associated with sleep duration and insomnia. Arch Gen Psychiatry. 2002;59:131–6. doi: 10.1001/archpsyc.59.2.131. [DOI] [PubMed] [Google Scholar]
- 18.Wu AH, Wang R, Koh WP, Stanczyk FZ, Lee HP, Yu MC. Sleep duration, melatonin and breast cancer among Chinese women in Singapore. Carcinogenesis. 2008;29:1244–8. doi: 10.1093/carcin/bgn100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.McElroy JA, Newcomb PA, Titus-Ernstoff L, Trentham-Dietz A, Hampton JM, Egan KM. Duration of sleep and breast cancer risk in a large population-based case-control study. J Sleep Res. 2006;15:241–9. doi: 10.1111/j.1365-2869.2006.00523.x. [DOI] [PubMed] [Google Scholar]
- 20.Ikehara S, Iso H, Date C, Kikuchi S, Watanabe Y, Wada Y, et al. Association of sleep duration with mortality from cardiovascular disease and other causes for Japanese men and women: the JACC study. Sleep. 2009;32:295–301. doi: 10.1093/sleep/32.3.295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tuomilehto H, Peltonen M, Partinen M, Seppa J, Saaristo T, Korpi-Hyovalti E, et al. Sleep duration is associated with an increased risk for the prevalence of type 2 diabetes in middle-aged women - The FIN-D2D survey. Sleep Med. 2008;9:221–7. doi: 10.1016/j.sleep.2007.04.015. [DOI] [PubMed] [Google Scholar]
- 22.Zheng W, Chow WH, Yang G, Jin F, Rothman N, Blair A, et al. The Shanghai Women’s Health Study: rationale, study design, and baseline characteristics. Am J Epidemiol. 2005;162:1123–31. doi: 10.1093/aje/kwi322. [DOI] [PubMed] [Google Scholar]
- 23.Krueger PM, Friedman EM. Sleep duration in the United States: a cross-sectional population-based study. Am J Epidemiol. 2009;9(169):1052–63. doi: 10.1093/aje/kwp023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Espiritu JR. Aging-related sleep changes. Clin Geriatr Med. 2008;24:1–14. doi: 10.1016/j.cger.2007.08.007. [DOI] [PubMed] [Google Scholar]
- 25.Ohayon MM, Carskadon MA, Guilleminault C, Vitiello MV. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep. 2004;27:1255–73. doi: 10.1093/sleep/27.7.1255. [DOI] [PubMed] [Google Scholar]
- 26.Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 27.Fang J, Wheaton AG, Keenan NL, Greenlund KJ, Perry GS, Croft JB. Association of sleep duration and hypertension among US adults varies by age and sex. Am J Hypertens. 2012;25:335–41. doi: 10.1038/ajh.2011.201. [DOI] [PubMed] [Google Scholar]
- 28.Magee CA, Caputi P, Iverson DC. Relationships between self-rated health, quality of life and sleep duration in middle aged and elderly Australians. Sleep Med. 2011;12:346–50. doi: 10.1016/j.sleep.2010.09.013. [DOI] [PubMed] [Google Scholar]
- 29.Ferrie JE, Shipley MJ, Akbaraly TN, Marmot MG, Kivimäki M, Singh-Manoux A. Change in sleep duration and cognitive function: findings from the Whitehall II Study. Sleep. 2011;34:565–73. doi: 10.1093/sleep/34.5.565. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patel SR, Malhotra A, Gottlieb DJ, White DP, Hu FB. Correlates of long sleep duration. Sleep. 2006;29:881–9. doi: 10.1093/sleep/29.7.881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Sanchez-Ortuno M, Moore N, Taillard J, Valtat C, Leger D, Bioulac B, et al. Sleep duration and caffeine consumption in a French middle-aged working population. Sleep Med. 2005;6:247–51. doi: 10.1016/j.sleep.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 32.Zwyghuizen-Doorenbos A, Roehrs TA, Lipschutz L, Timms V, Roth T. Effects of caffeine on alertness. Psychopharmacology. 1990;100:36–9. doi: 10.1007/BF02245786. [DOI] [PubMed] [Google Scholar]
- 33.Chen H, Schernhammer E, Schwarzschild MA, Ascherio A. A prospective study of night shift work, sleep duration, and risk of Parkinson’s disease. Am J Epidemiol. 2006;163:726–30. doi: 10.1093/aje/kwj096. [DOI] [PubMed] [Google Scholar]
- 34.Ohayon MM, Smolensky MH, Roth T. Consequences of shiftworking on sleep duration, sleepiness, and sleep attacks. Chronobiol Int. 2010;27:575–89. doi: 10.3109/07420521003749956. [DOI] [PubMed] [Google Scholar]
- 35.Knutsson A. Health disorders of shift workers. Occup Med (Lond) 2003;53:103–8. doi: 10.1093/occmed/kqg048. [DOI] [PubMed] [Google Scholar]
- 36.Li F, Fisher KJ, Harmer P, Irbe D, Tearse RG, Weimer C. Tai chi and self-rated quality of sleep and daytime sleepiness in older adults: a randomized controlled trial. J Am Geriatr Soc. 2004;52:892–900. doi: 10.1111/j.1532-5415.2004.52255.x. [DOI] [PubMed] [Google Scholar]
- 37.de Castro Toledo Guimaraes LH, de Carvalho LB, Yanaguibashi G, do Prado GF. Physically active elderly women sleep more and better than sedentary women. Sleep Med. 2008;9:488–93. doi: 10.1016/j.sleep.2007.06.009. [DOI] [PubMed] [Google Scholar]
- 38.Lichstein KL, Payne KL, Soeffing JP, Heith Durrence H, Taylor DJ, Riedel BW, et al. Vitamins and sleep: an exploratory study. Sleep Med. 2007;9:27–32. doi: 10.1016/j.sleep.2006.12.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Tamakoshi A, Ohno Y. Self-reported sleep duration as a predictor of all-cause mortality: results from the JACC study, Japan. Sleep. 2004;27:51–55. [PubMed] [Google Scholar]
- 40.Heslop P, Smith GD, Metcalfe C, Macleod J, Hart C. Sleep duration and mortality: The effect of short or long sleep duration on cardiovascular and all-cause mortality in working men and women. Sleep Med. 2002;3:305–14. doi: 10.1016/s1389-9457(02)00016-3. [DOI] [PubMed] [Google Scholar]
- 41.Lauderdale DS, Knutson KL, Yan LL, Rathouz PJ, Hulley SB, Sidney S, et al. Objectively measured sleep characteristics among early-middle-aged adults: the CARDIA study. Am J Epidemiol. 2006;164:5–16. doi: 10.1093/aje/kwj199. [DOI] [PubMed] [Google Scholar]
- 42.Chaput JP, Despres JP, Bouchard C, Tremblay A. Short sleep duration is associated with reduced leptin levels and increased adiposity: results from the Quebec Family Study. Obesity. 2007;15:253–61. doi: 10.1038/oby.2007.512. [DOI] [PubMed] [Google Scholar]
- 43.Ko GT, Chan JC, Chan AW, Wong PT, Hui SS, Tong SD, et al. Association between sleeping hours, working hours and obesity in Hong Kong Chinese: the ‘better health for better Hong Kong’ health promotion campaign. Int J Obes (Lond) 2007;312:254–60. doi: 10.1038/sj.ijo.0803389. [DOI] [PubMed] [Google Scholar]
- 44.Moreno CR, Louzada FM, Teixeira LR, Borges F, Lorenzi-Filho G. Short Sleep Is Associated with Obesity among Truck Drivers. Chronobiol Int. 2006;23:1295–303. doi: 10.1080/07420520601089521. [DOI] [PubMed] [Google Scholar]
- 45.Ievers-Landis CE, Storfer-Isser A, Rosen C, Johnson NL, Redline S. Relationship of sleep parameters, child psychological functioning, and parenting stress to obesity status among preadolescent children. J Dev Behav Pediatr. 2008;29:243–52. doi: 10.1097/DBP.0b013e31816d923d. [DOI] [PubMed] [Google Scholar]
- 46.Lumeng JC, Somashekar D, Appugliese D, Kaciroti N, Corwyn RF, Bradley RH. Shorter sleep duration is associated with increased risk for being overweight at ages 9 to 12 years. Pediatrics. 2007;120:1020–9. doi: 10.1542/peds.2006-3295. [DOI] [PubMed] [Google Scholar]
- 47.Watson NF, Buchwald D, Vitiello MV, Noonan C, Goldberg J. A twin study of sleep duration and body mass index. J Clin Sleep Med. 2010;6:11–7. [PMC free article] [PubMed] [Google Scholar]
- 48.Buxton OM, Marcelli E. Short and long sleep are positively associated with obesity, diabetes, hypertension, and cardiovascular disease among adults in the United States. Soc Sci Med. 2010;71:1027–36. doi: 10.1016/j.socscimed.2010.05.041. [DOI] [PubMed] [Google Scholar]
- 49.Reid KJ, Martinovich Z, Finkel S, Statsinger J, Golden R, Harter K, et al. Sleep: a marker of physical and mental health in the elderly. Am J Geriatr Psychiatry. 2006;1410:860–6. doi: 10.1097/01.JGP.0000206164.56404.ba. [DOI] [PubMed] [Google Scholar]
- 50.Shankar A, Koh WP, Yuan JM, Lee HP, Yu MC. Sleep duration and coronary heart disease mortality among Chinese adults in Singapore: a population-based cohort study. Am J Epidemiol. 2008;168:1367–73. doi: 10.1093/aje/kwn281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lauderdale DS, Knutson KL, Yan LL, Liu K, Rathouz PJ. Self-reported and measured sleep duration: how similar are they? Epidemiology. 2008;196:838–45. doi: 10.1097/EDE.0b013e318187a7b0. [DOI] [PMC free article] [PubMed] [Google Scholar]