Abstract
Anxiety disorders are characterized by persistent, excessive fear. Therapeutic interventions that reverse deficits in fear extinction represent a tractable approach to treating these disorders. We previously reported that 129S1/SvImJ (S1) mice show no extinction learning following normal fear conditioning. We now demonstrate that weak fear conditioning does permit fear reduction during massed extinction training in S1 mice, but reveals specific deficiency in extinction memory consolidation/retrieval. Rescue of this impaired extinction consolidation/retrieval was achieved with d-cycloserine (N-methly-d-aspartate partial agonist) or MS-275 (histone deacetylase (HDAC) inhibitor), applied after extinction training. We next examined the ability of different drugs and non-pharmacological manipulations to rescue the extreme fear extinction deficit in S1 following normal fear conditioning with the ultimate aim to produce low fear levels in extinction retrieval tests. Results showed that deep brain stimulation (DBS) by applying high frequency stimulation to the nucleus accumbens (ventral striatum) during extinction training, indeed significantly reduced fear during extinction retrieval compared to sham stimulation controls. Rescue of both impaired extinction acquisition and deficient extinction consolidation/retrieval was achieved with prior extinction training administration of valproic acid (a GABAergic enhancer and HDAC inhibitor) or AMN082 [metabotropic glutamate receptor 7 (mGlu7) agonist], while MS-275 or PEPA (AMPA receptor potentiator) failed to affect extinction acquisition in S1 mice. Collectively, these data identify potential beneficial effects of DBS and various drug treatments, including those with HDAC inhibiting or mGlu7 agonism properties, as adjuncts to overcome treatment resistance in exposure-based therapies.
This article is part of a Special Issue entitled ‘Cognitive Enhancers’.
Keywords: Fear extinction, Metabotropic glutamate receptor, Epigenetics, HDAC inhibitor, Ventral striatum deep brain stimulation, NMDA receptor
Highlights
► Nucleus accumbens stimulation during training rescues deficient extinction in S1. ► mGluR7 agonism or duel HDAC inhibition/GABA enhancement rescues S1 extinction. ► Weak fear conditioning permit extinction learning, not retrieval, in S1 mice. ► HDAC inhibitor, MS-275, rescues S1 extinction after weak, not strong, conditioning. ► d-cycloserine, NMDAR partial agonist, rescues S1 extinction after weak conditioning.
1. Introduction
Anxiety disorders, such as post-traumatic stress disorder, social phobia, specific phobias, panic and obsessive-compulsive disorders, are among the most common mental disorders in humans (Olesen et al., 2012). These disorders are associated with problems to extinguish learned fear responses and also to consolidate extinction memories (Myers and Davis, 2007; Milad et al., 2009). To date, the most effective strategies in the treatment of anxiety disorders include use of pharmacological and cognitive strategies (Nutt, 2005). However, significant drawbacks to current therapy exist including lack of treatment response and also a lack of long-term beneficial effect of combining available drugs with exposure-based therapy (Barlow et al., 2000; Davidson et al., 2004; Foa et al., 2005; Yehuda and LeDoux, 2007; Norberg et al., 2008).
Clinical interventions which rescue deficits in fear extinction acquisition and consolidation would constitute important treatment options in these disorders. Along these lines, pharmacological and genetic silencing studies, predominantly in normally behaving rodents and using massed extinction training paradigms, have identified a number of neurobiological mechanisms that govern acquisition of fear extinction learning and extinction consolidation. Acquisition of extinction learning requires N-methyl-d-aspartate (NMDA) receptor 2B (Sotres-Bayon et al., 2007), α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) (Zushida et al., 2007; Yamada et al., 2009) and metabotropic glutamate 7 (mGlu7) (Fendt et al., 2008) receptor activities in addition to GABAergic signalling [for example, see (Harris and Westbrook, 1998; Chhatwal et al., 2005; Akirav et al., 2006; Lin et al., 2009; Dalton et al., 2012)], amongst others. Following acquisition of extinction, there is a consolidation phase which lasts up to several hours which serves to stabilize plastic events into long-term memory (McGaugh, 2000). Activation of NMDA receptors (Davis, 2011), brain-derived neurotrophic factor (BDNF) signalling (Chhatwal et al., 2006; Soliman et al., 2010) and inhibition of histone deacetylases (HDAC) (Guan et al., 2009; McQuown et al., 2011), amongst others, are important for consolidation of extinction [for detailed reviews, see (Myers and Davis, 2007; Quirk and Mueller, 2008; Herry et al., 2010; Pape and Pare, 2010; Steckler and Risbrough, 2011; Orsini and Maren, 2012; Tronson et al., 2012)].
The present study used isogenic 129S1/SvImJ (S1) mice which display deficient extinction acquisition, poor recovery of fear-induced suppression of heart-rate variability, enlarged dendritic arbours in basolateral amygdala neurons and functional abnormalities in cortico-amygdala circuitry mediating fear extinction (Hefner et al., 2008; Camp et al., 2009, 2012; Whittle et al., 2010). In the current study we reduced the intensity of fear conditioning and observed that “weak” fear conditioning allowed for extinction acquisition in S1 mice but revealed deficient extinction retrieval. Recent findings show that impaired extinction acquisition and dysfunctional cortico-amygdala circuitry can be rescued by a novel zinc restricted diet (Whittle et al., 2010), which interestingly did not affect either fear learning or fear expression. Also, recent findings reveal that the S1 fear extinction phenotype can be rescued by fluoxetine (a serotonin-selective reuptake inhibitor) (Camp et al., 2012) which is of clinical relevance as serotonin-selective reuptake inhibitors are first-line treatment for anxiety disorders (Nutt, 2005). Considering the well-known disadvantages of long-term SSRI treatments, we screened for novel treatments which rescue both deficient extinction acquisition and extinction consolidation/retrieval in S1 mice.
Evidence suggests that deep brain stimulation (DBS) of the nucleus accumbens (AcbC) can enhance extinction-like behaviour in intractable obsessive-compulsive disorder patients, which is characterised by avoidance behaviours that fail to extinguish (Lipsman et al., 2007; Burdick et al., 2009; Goodman et al., 2010; Greenberg et al., 2010; Grant et al., 2011). Furthermore, a small clinical study involving patients suffering from treatment-resistant depression has shown that DBS of the AcbC can enhance various measures of cognition independent of mood status (Bewernick et al., 2012). However, there are also reports of no effect of AcbC-DBS in mood disorder patients (Grubert et al., 2011). Very recently, DBS of the AcbC during extinction training reduced fear expression and strengthened extinction memory in normally behaving rats (Rodriguez-Romaguera et al., 2012) potentially showing the utility of DBS of the AcbC as a novel fear reducing adjunct during exposure-based therapy. Here, we went beyond using normally behaving rodents and assessed whether DBS of the AcbC during extinction training can rescue deficient extinction acquisition and extinction consolidation/retrieval in S1 mice.
Pharmacological compounds which enhance glutamatergic signalling, including DCS (NMDA receptor partial agonist), PEPA (AMPA receptor potentiator) or AMN082 (mGlu7 receptor agonist), can facilitate fear extinction in normally extinguishing animal models and in clinical studies (Myers et al., 2011). We have previously shown that prior extinction training administration of DCS is ineffective in rescuing deficient extinction learning in S1 mice (Hefner et al., 2008). However, it remains unknown whether DCS can rescue deficient extinction consolidation/retrieval once at least some extinction learning is induced, which we revealed in “weak” fear conditioned S1 mice. Furthermore, it is not known whether PEPA or AMN082 can reduce fear in an animal model of impaired extinction.
Drugs inhibiting HDAC proteins to prevent the removal of acetyl groups on histone tails is a promising approach in central nervous system disorders associated with disturbed learning and memory (Kazantsev and Thompson, 2008). Interestingly, inhibiting HDACs has been shown to enhance fear learning (Guan et al., 2009) and rescue deficits in fear learning in mouse models of anxiety or neurodegeneration (Li et al., 2006; Dash et al., 2009; Kilgore et al., 2010). Facilitation of fear extinction by HDAC inhibition has been reported in normally extinguishing mice (Bredy et al., 2007; Lattal et al., 2007; Bredy and Barad, 2008; Guan et al., 2009; Monsey et al., 2011). However, it is not known whether inhibiting HDACs can improve extinction learning in animal models of impaired extinction. Thus, we tested whether valproic acid (VPA), a dual HDAC inhibitor and enhancer of GABAergic signalling or MS-275, a more specific HDAC inhibitor (Khan et al., 2008; Bantscheff et al., 2011), can rescue deficient extinction in S1 mice.
2. Materials and methods
2.1. Subjects
Subjects were male 3–5 month old 129S1/SvImJ (S1) mice. For experiments performed at the University of Innsbruck, mice (obtained from Charles River, Germany) were housed (4–5 per cage) in a temperature- (22 ± 2 °C) and humidity- (50–60%) controlled vivarium under a 12 h light/dark cycle (lights on at 7:00 A.M.). For experiments conducted at the National Institutes of Health, mice (obtained from The Jackson Laboratory, USA) were housed (2 per cage) in a temperature (22 ± 1 °C)- and humidity (45 ± 15%)-controlled vivarium under a 12 h light/dark cycle (lights on, 6:00 A.M.). All experimental procedures were approved by the Austrian Animal Experimentation Ethics Board and by the National Institute on Alcohol Abuse and Alcoholism Animal Care and Use and Austrian Ethical Committees on Animal Care and Use (Bundesministerium für Wissenschaft und Verkehr, Kommission für Tierversuchsangelegenheiten) and followed the National Institutes of Health guidelines outlined in Using Animals in Intramural Research and the local animal care and use committees.
2.2. General procedures for fear conditioning and extinction
For experiments performed at the University of Innsbruck, mice were conditioned in a 25 × 25 × 35 cm chamber with transparent walls and a metal rod floor, cleaned with water and illuminated to 300 lux (‘context A’). After a 120 s acclimation period, there were 3× pairings of a 120 s, 80 dB white noise conditioned stimulus (CS) and a 2 s scrambled foot shock unconditioned stimulus (US) (0.6 mA unless stated otherwise), with a 120 s inter-pairing interval. There was a 120 s no-stimulus consolidation period after the final pairing before mice were returned to the home cage. Extinction training was performed the next day in a 25 × 25 × 35 cm cage with a solid grey floor and black walls, cleaned with a 100% ethanol and illuminated to 10 lux (‘context B’). After a 120 s acclimation period, there were CS-alone trials (16 unless stated otherwise), with a 5-sec inter-CS interval. Stimulus presentation was controlled by a TSE operant system (TSE, Bad Homburg, Germany). Extinction retrieval was conducted the following day by repeating the extinction training procedure but with 2× CS trials. Freezing was measured as an index of fear (Blanchard and Blanchard, 1969), manually scored based on DVD recordings of the duration of the CS, defined as no visible movement except that required for respiration, and converted to a percentage [(duration of freezing within the CS/total time of the CS) × 100] by a trained observer blind to the animals' group.
For experiments performed at NIAAA, mice were conditioned in a 27 × 27 × 11 cm chamber with a metal-rod floor, cleaned with a 79.5% water/19.5% ethanol/1% vanilla-extract solution (‘context A’). After a 180 s acclimation period, there were 3× pairings (60–120 s inter-pairing interval) of the conditioned stimulus (CS; 30 s 80 dB, 3 kHz tone) and the unconditioned stimulus (US; 2 s, 0.6 mA scrambled foot shock), in which the US was presented during the last 2 s of the CS. The session ended 120 s after the final CS–US pairing. Stimulus presentation was controlled by the Med Associates VideoFreeze system (Med Associates, Burlington, VT, USA). 24 h after conditioning, extinction training was conducted in a novel context (‘context B’) (cylinders with black/white-chequered walls and a solid Plexiglas opaque floor cleaned with a 1% acetic acid/99% water solution) housed in a different room from conditioning. After a 180 s acclimation period, there were 16× CS presentations (5-sec inter-CS interval). Extinction retrieval was tested in context B 48 h after extinction training. After a 180 s acclimation period, there were 3× CS presentations (5-sec inter-CS interval). Freezing (no visible movement except respiration) was scored every 5 s by an observer blind to condition/treatment and converted to a percentage [(freezing observations/total observations) × 100].
2.3. Extinction in S1 mice after weak versus normal fear conditioning
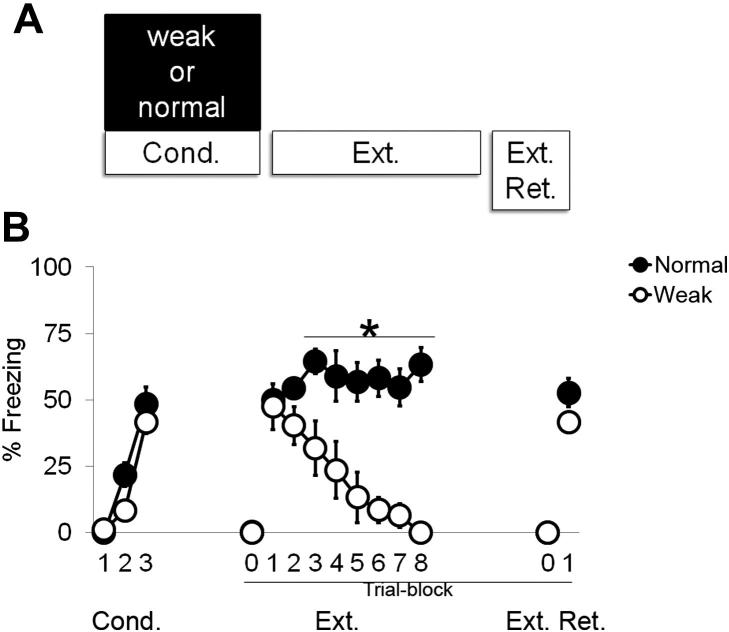
Procedures and apparatuses for normal fear conditioning were as described above and involved 3× pairings of the CS with a 0.6 mA US. The weak fear conditioning procedure was the same with the exception that the US was 0.3 mA. Mice were randomly assigned to either weak or normal fear conditioning and tested for extinction training and retrieval as above (Fig. 1A).
Fig. 1.
Comparison of “normal” and “weak” fear conditioning paradigms during fear conditioning (Cond.), extinction training (Ext.) and extinction retrieval (Ext. Ret.). A) Schematic of experimental design. B) No differences in freezing were observed during fear conditioning or fear expression between “normal” and “weak” fear conditioned groups. During extinction training, “weak” fear conditioned mice displayed reduced freezing compared to “normal” fear conditioned mice. No differences in freezing behaviour were observed between “normal” and “weak” fear conditioned mice during extinction retrieval. 0 = baseline/pre-tone freezing levels. *p < 0.05 “normal” vs. “weak” fear conditioned groups.
2.4. Effects of deep brain stimulation of the nucleus accumbens
Mice were anaesthetized with a mixture of ketamine/xylazine (80/5 mg/kg) injected intraperitoneally (i.p.). Using a stereotaxic frame, electrodes (MS303-3-B-SPC, bipolar, twisted, 8 mm, Plastics ONE, USA) were implanted unilaterally, targeting the core of the nucleus accumbens. The coordinates were +1.10 mm anterior to Bregma, +1.45 mm lateral from midline, −4.65 mm ventral according to the atlas of (Franklin and Paxinos, 2008). Electrodes were fixed to the skull with 2 stainless steel screws and dental cement (Havard Cement, Richter & Hoffmann Harvard Dental GmbH, Germany). After surgery animals were individually caged and received buprenorphin (0.1 mg/kg injected intraperitoneally) every 8 h for 3 days to minimise pain.
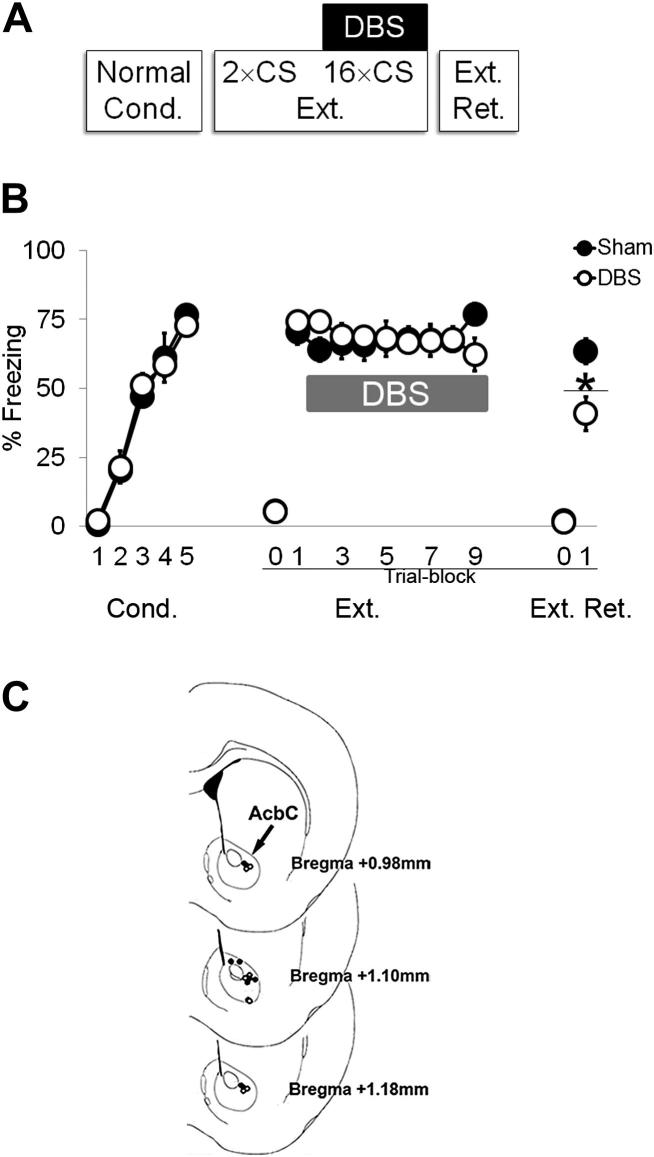
After 4–5 days of recovery, mice were conditioned via 5× pairings of the CS with a 0.7 mA US. Extinction training began with 2× CS-alone trials without DBS to measure fear expression in the absence of any influence of DBS before presenting 16× CS-alone extinction trials. DBS (130 Hz, 100 μA, 60 μs pulse width) was applied via an A310 Accupulser and A365 Stimulus Isolator (World Precision Instruments, Sarasota, USA) throughout the CS period during each 16× CS extinction trials (Fig. 2A). Sham controls were connected to the stimulator but received no current. At the completion of testing, the localization of electrodes was confirmed from inspection of cresyl violet stained coronal sections (Fig. 2C), and mice with misplaced electrodes were excluded.
Fig. 2.
DBS of the AcbC during extinction training reduces fear in S1 mice. A) Schematic of experimental design. B) Sham and DBS groups did not differ in freezing during “stronger” fear conditioning (Cond.). DBS did not alter fear expression as no differences were observed in the DBS group during the first CS-block in which the stimulator was off and the first CS-block (CS-block 2) when the stimulator was on. Freezing did not differ between Sham and DBS groups during the remainder of extinction training (Ext.). Lower freezing was observed in DBS mice during an extinction retrieval session (Ext. Ret.). C) Schematic diagram showing electrode placement in the AcbC. Diagram adapted from Franklin and Paxinos (2008). Sham stimulated mice are shown as filled circles and DBS stimulated mice are shown as white filled circles. Level indicated is mm from Bregma. 0 = baseline/pre-tone freezing levels. *p < 0.001 Sham vs. DBS.
2.5. Effects of VPA administration
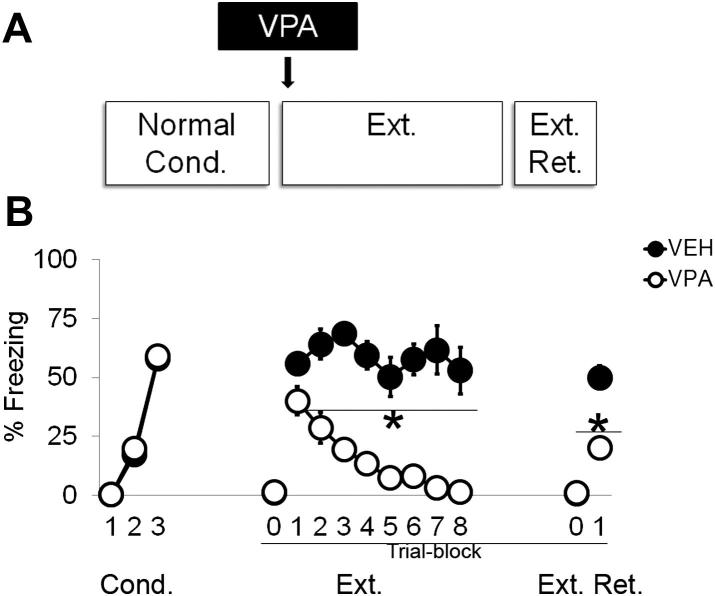
Mice were conditioned via 3× pairings of the CS with a 0.6 mA US. 100 mg/kg VPA (Sigma, St. Louis, USA) or saline vehicle was injected i.p. in a volume of 10 ml/kg body weight 2 h prior to extinction training (Fig. 3A). The dose, route and timing of administration was based on previous studies showing extinction facilitating effects of VPA in mice (Bredy et al., 2007; Bredy and Barad, 2008) and that 2 h is required before maximal histone acetylation is observed (Tremolizzo et al., 2005).
Fig. 3.
VPA, administered prior to extinction training, rescues impaired extinction acquisition and deficient extinction consolidation/expression in S1 mice. A) Schematic of experimental design. B) During extinction training (Ext.), freezing was lower in VPA treated S1 mice than VEH S1 mice on CS presentation blocks 2–8. Lower freezing was observed in VPA treated S1 mice during extinction retrieval (Ext. Ret.). No differences in freezing was observed between VEH and VPA groups during “normal” fear conditioning (Cond.). 0 = baseline/pre-tone freezing levels. *p < 0.05 VEH vs. VPA.
2.6. Effects of AMN082 administration
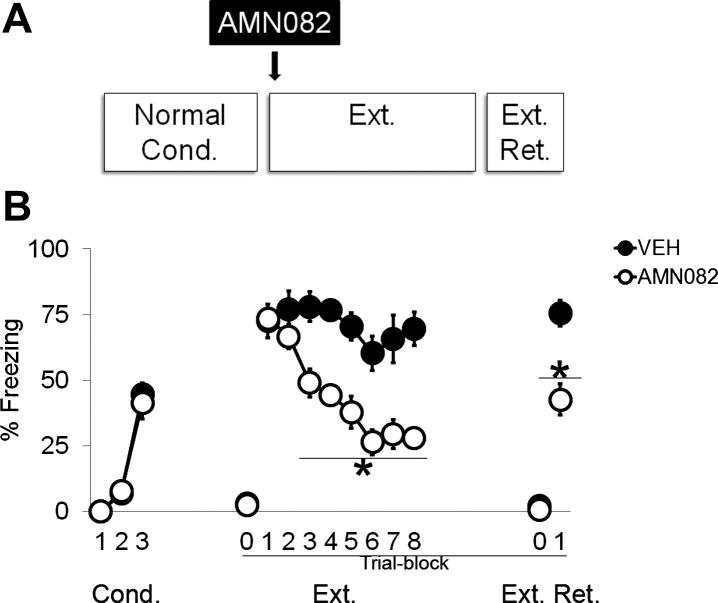
Mice were conditioned via 3× pairings of the CS with a 0.6 mA US. 6 mg/kg AMN082 (Tocris Bioscience, Bristol, United Kingdom) or saline + 0.5% methylcellulose vehicle was administered per oral (p.o.) via gavage in a volume of 10 ml/kg body weight 2 h prior to extinction training (Fig. 4A). The dose, route and timing of administration was based on previous studies showing extinction facilitating effects of AMN082 in mice (Fendt et al., 2008).
Fig. 4.
AMN082, administered prior to extinction training, rescues impaired extinction learning and deficient extinction consolidation/retrieval in S1 mice. A) Schematic of experimental design. B) During extinction training (Ext.), freezing was lower in AMN082 treated S1 mice than VEH S1 mice on CS presentation blocks 3–8. Lower freezing was observed in AMN082 treated S1 mice during extinction retrieval (Ext. Ret.). No differences in freezing were observed between VEH and AMN082 groups during “normal” fear conditioning (Cond.). 0 = baseline/pre-tone freezing levels. *p < 0.05 VEH vs. AMN082.
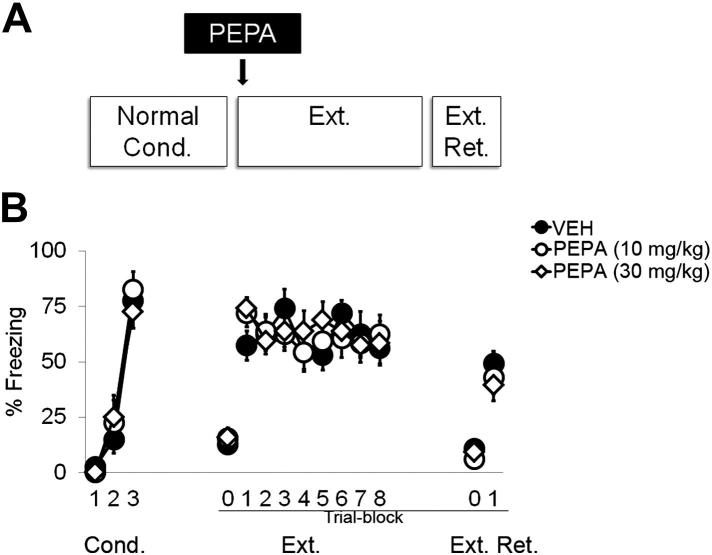
2.7. Effects of PEPA administration
Mice were conditioned via 3× pairings of the CS with a 0.6 mA US. 10 or 30 mg/kg PEPA (Sigma, St. Louis, USA) or saline + 0.45% NaCl + 33% (2-hydroxypropyl)-β-cyclodextrin vehicle was injected i.p. in a volume of 10 ml/kg body weight 15 min prior to extinction training (Fig. 5A). The doses, route and timing of administration was based on previous studies showing extinction facilitating effects of PEPA in mice (Zushida et al., 2007; Yamada et al., 2009).
Fig. 5.
PEPA, administered prior to extinction training, does not rescue deficient extinction acquisition or deficit extinction consolidation/retrieval in S1 mice. A) Schematic of experimental design. B) Freezing responses did not differ between VEH or 10 or 30 mg/kg MS-275 groups during “normal” fear conditioning (Cond.), extinction training (Ext.) or an extinction retrieval session (Ext. Ret.). 0 = baseline/pre-tone freezing levels.
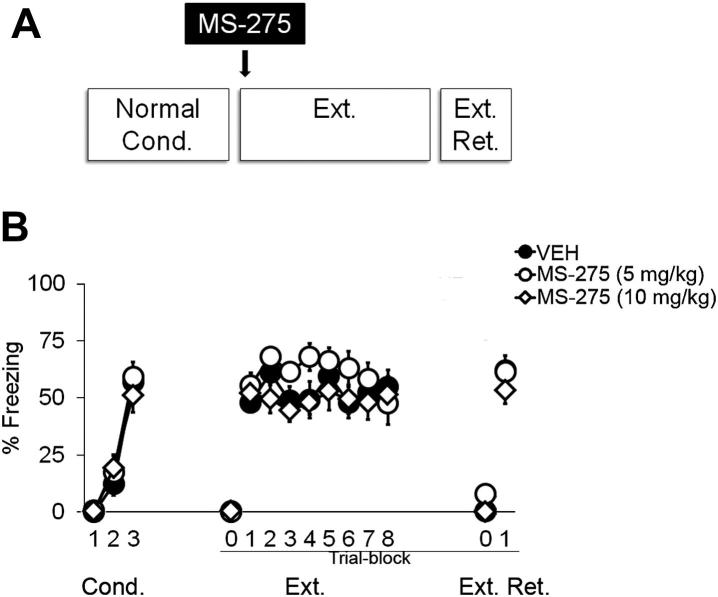
2.8. Effects of MS-275 administration
Mice were conditioned via 3× pairings of the CS with a 0.6 mA US. 5 or 10 mg/kg MS-275 (Sigma, St. Louis, USA) or saline + 25% DMSO vehicle was injected i.p. in a volume of 10 ml/kg body weight 2 h prior to extinction training (Fig. 6A). The doses, route and timing of administration was based on a previous study showing that maximal increases in histone acetylation occurs 2 h following s.c. injection of MS-275 (Simonini et al., 2006).
Fig. 6.
MS-275, administered prior to extinction training (arrow), does not rescue deficient extinction acquisition or deficit extinction consolidation/retrieval in S1 mice. A) Schematic of experimental design. B) Freezing responses did not differ between VEH or 5 or 10 mg/kg MS-275 groups during “normal” fear conditioning (Cond.), extinction training (Ext.) or an extinction retrieval session (Ext. Ret.). 0 = baseline/pre-tone freezing levels.
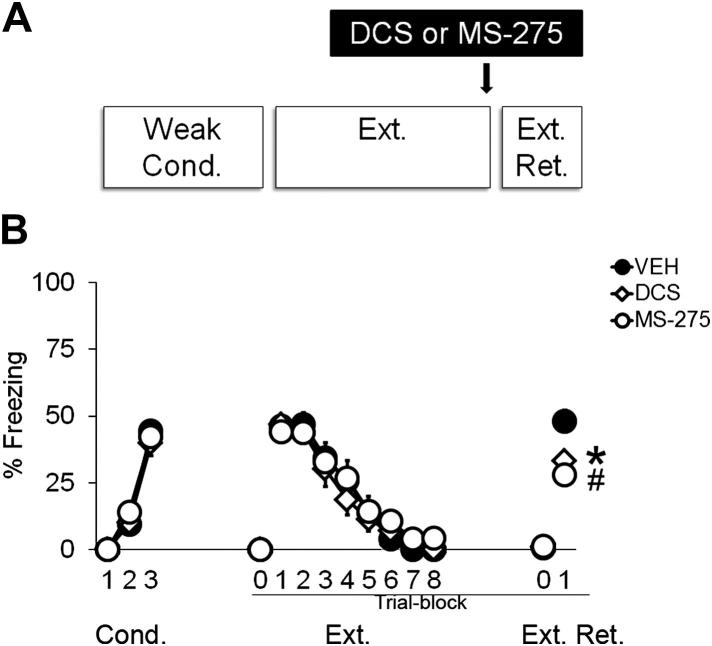
2.9. Effects of MS-275 and DCS administration after weak conditioning
Mice were conditioned via 3× pairings of the CS with a 0.3 mA US. 10 mg/kg MS-275 (Eubio, Vienna, Austria), 15 mg/kg DCS (Sigma, St. Louis, USA) or saline + 25% DMSO vehicle was injected i.p. in a volume of 10 ml/kg body weight immediately (<2 min) after extinction training (Fig. 7A). The doses, route and timing of administration of MS-275 was based on our earlier experiment and the doses, route and timing of administration of DCS was based on previous studies showing extinction facilitating effects in rats and humans (Walker and Davis, 2002; Ressler et al., 2004; Richardson et al., 2004).
Fig. 7.
Post extinction administration of DCS or MS-275 rescues impaired extinction consolidation/retrieval in S1 mice. A) Schematic of experimental design. B) Lower freezing was observed during a retrieval test (Ext. Ret.) when DCS or MS-275 was administered immediately following successful extinction (arrow). Groups did not differ in freezing responses either during “weak” fear conditioning (Cond.) or during extinction training (Ext.). 0 = baseline/pre-tone freezing levels. *p < 0.05 VEH vs. DCS; #p < 0.01 VEH vs. MS-275.
2.10. Statistical analysis
All data were examined for equal variances using Levene's test before performing parametric tests. Data were analyzed using analysis of variance (ANOVA), with repeated measures for trial/trial-block, or by Student's t-test. Significant ANOVA results were followed by Fisher's LSD post hoc tests.
3. Results
3.1. Weak fear conditioning in S1 mice permits fear reduction during extinction training, but not retrieval
We have previously found that the level of fear expression in S1 mice can be modulated by the intensity (shock amplitude, shock-tone trial number) of fear conditioning (Camp et al., 2009). Therefore, we asked whether extinction in S1 was graded by the intensity of conditioning. There was a significant and similar increase in freezing across 3 conditioning trials in mice given 0.3 mA and 0.6 mA shocks [ANOVA effect of trial: F(2, 20) = 80. 15, p < 0.001; effect of group: p > 0.05, interaction: p > 0.05, n = 6/group] (Fig. 1B). During extinction training, there was a significant group × trial–block interaction for freezing (F(7, 70) = 8.71, p < 0.001). Post hoc tests revealed that the weak shock group displayed lower freezing than the 0.6 mA group on blocks 3–8, but not blocks 1 or 2 (Fig. 1B). However, during extinction retrieval, freezing was not different between groups (t-test: p > 0.05) (Fig. 1B). These results show that while this weak conditioning procedure did not reduce fear learning or expression compared to normal conditioning, it did allow for significant fear reduction during the extinction learning trial in S1 mice. However, extinction memory was not successfully consolidated/retrieved on the next day.
3.2. Deep brain stimulation of the nucleus accumbens rescues impaired extinction retrieval
We first examined the effects of DBS of the AcbC, applied during extinction training, on impaired extinction in S1 mice. During conditioning, freezing increased across trials and did not differ between groups [ANOVA effect of trial: F(4, 64) = 109.80, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 9/group] (Fig. 2B). DBS during extinction training did not affect freezing, as compared to sham-stimulated controls, as both groups showed no change in freezing across trial-blocks [ANOVA effect of group: p > 0.05, effect of trial-block: p > 0.05, group × trial-block interaction: p > 0.05] (Fig. 2B). During extinction retrieval, freezing was significantly lower in DBS than sham controls during extinction retrieval (t16 = 2.96, p < 0.01) (Fig. 2B). These results show that DBS of the nucleus accumbens rescued extinction retrieval, but not extinction acquisition, in S1 mice.
3.3. VPA rescues impaired extinction learning and retrieval
We next examined the effects of 3 diverse pharmacological compounds, applied acutely prior to extinction training, on impaired S1 extinction. Our first experiment tested the effects of VPA. During conditioning, freezing increased across trials and did not differ between groups [ANOVA effect of trial: F(2, 32) = 347.05, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 8–9/group] (Fig. 3B). There was a significant group × trial block interaction for freezing during training (F(7, 98) = 3.24, p < 0.01). Post hoc tests showed freezing was significantly lower in the VPA group relative to vehicle, on trial-blocks 2–8 (Fig. 3B). During extinction retrieval, freezing was again significantly lower in the VPA than the vehicle group (t15 = 4.75, p < 0.001) (Fig. 3B). These data show that VPA rescues impaired extinction learning and retrieval in S1 mice.
3.4. AMN082 rescues impaired extinction learning and retrieval
Our next experiment examined the effects of pre-extinction-administered AMN082. During conditioning, freezing increased across trials and did not differ between groups [ANOVA effect of trial: F(2, 28) = 90.25, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 8/group] (Fig. 4B). There was a significant treatment × trial-block interaction for freezing during extinction training (F(7, 98) = 4.82, p < 0.001). Post hoc tests showed significantly lower freezing in the AMN082 treated group as compared to vehicle on trial-blocks 3–8 (Fig. 4B). Freezing was also significantly lower in the AMN082 group than the vehicle group during extinction retrieval (t14 = 4.24, p < 0.001) (Fig. 4B). The results of this experiment indicate rescue of impaired S1 extinction learning and retrieval by AMN082.
3.5. PEPA does not rescue either impaired extinction learning or retrieval
We next studied the effects PEPA applied before extinction. During conditioning, freezing increased across trials and did not differ between groups [ANOVA effect of trial: F(2, 42) = 140.25, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 8/group] (Fig. 5B). There was no effect of treatment on freezing during extinction training and neither group showed a reduction in freezing across trial-blocks (Fig. 5B). Freezing was also no different between groups on extinction retrieval (Fig. 5B). These data show that, unlike VPA and AMN082, PEPA failed to rescue impaired S1 extinction.
3.6. MS-275 does not rescue either impaired extinction learning or retrieval
In our next experiment, we examined the ability of MS-275, administered prior to extinction training, to rescue impaired S1 extinction retrieval. Freezing increased across conditioning trials, and treatment groups did not differ from one another [ANOVA effect of trial: F(2, 42) = 90.82, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 7–10/group] (Fig. 6B). There was no effect of treatment on freezing during extinction training and neither group showed a reduction in freezing across trial-blocks (Fig. 6B). Freezing was also no different between groups on extinction retrieval (Fig. 6B). This experiment shows that, like PEPA, application of MS-275 prior to extinction training failed to rescue impaired S1 extinction.
3.7. After weak conditioning, MS-275 and DCS rescues impaired extinction retrieval
Our observation that S1 mice can exhibit extinction learning after weak conditioning, but still have a deficit in extinction retrieval, led us to test whether two drug treatments shown here (MCS-275) and previously (DCS) (Hefner et al., 2008) to be ineffective in rescuing extinction after normal conditioning would be effective after weaker conditioning. Freezing increased across conditioning trials, and treatment groups did not differ from one another [ANOVA effect of trial: F(2, 50) = 163.80, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05, n = 9–10/group] (Fig. 7B). During extinction training, there was a significant reduction in freezing across trials that was similar between groups [ANOVA effect of trial: F(7, 175) = 88.18, p < 0.001, effect of group: p > 0.05, interaction: p > 0.05] (Fig. 7B). Mice were treated immediately after training. There was a significant effect of treatment on freezing during extinction retrieval (F(2, 25) = 7.21, p < 0.01). Post hoc tests showed that freezing was significantly lower in the DCS (p < 0.05) and MS-275 (p < 0.01) treated groups as compared to vehicle (Fig. 7B). The results of this experiment show that MS-275 and DCS can rescue impaired extinction retrieval in S1 mice given weak conditioning.
4. Discussion
The present study revealed a number of novel findings. Behaviourally, we show that using a “weak” fear conditioning paradigm S1 mice were able to reduce fear during extinction training, but were unable to consolidate/retrieve this memory during an extinction retrieval test. This result, in addition to the well described profound extinction acquisition deficit observed following “normal” conditioning (Hefner et al., 2008; Camp et al., 2009; Whittle et al., 2010), reveal that S1 mice, by using graded conditioning paradigms, can serve as an ideal model to dissociate whether extinction-promoting interventions act via inducing extinction acquisition and/or by enhancing extinction consolidation/retrieval. We next assessed a variety of treatments in their ability to rescue the profound extinction acquisition deficit seen after normal fear conditioning in S1 mice. Here we show that DBS of the AcbC during extinction training lowers fear in extinction retrieval and that pharmacological compounds which enhance GABAergic signalling in tandem with HDAC inhibition, or drugs that activate mGlu7 receptors, rescue extinction acquisition deficits and lower fear during extinction retrieval in S1 mice. AMPA receptor potentiation on the other hand was ineffective. Lastly, we revealed that compounds which enhance NMDA receptor activity or inhibit HDACs rescue the impaired extinction consolidation/retrieval deficit in S1 mice.
4.1. Weak fear conditioning in S1 mice permits fear reduction during extinction training, revealing specific deficiency in extinction consolidation/retrieval
Present data reveal a novel behavioural finding that “weak” fear conditioned S1 mice display impaired extinction consolidation/retrieval despite successful reduction of fear during extinction training. No significant alterations in either fear learning or fear expression were observed between “weak” and “normal” fear conditioned S1 mice demonstrating the selectivity of the extinction consolidation/retrieval deficit. Importantly, it is unlikely that sensitisation to the CS contributed to the observed extinction retrieval deficit as we have previously shown that S1 mice do not sensitise to the CS (Camp et al., 2009). Collectively, our current data and that of previously published behavioural findings showing S1 mice display deficient extinction acquisition following “normal” fear conditioning (Hefner et al., 2008; Camp et al., 2009; Whittle et al., 2010), reveal that S1 mice represent a unique model to determine whether extinction promoting treatments act via inducing extinction acquisition and/or enhancing extinction consolidation by using “normal” and “weak” fear conditioning paradigms.
4.2. DBS of the AcbC during extinction training reduces fear in a retrieval test session
DBS of the AcbC during extinction training reduced freezing in the extinction retrieval test indicating a novel treatment to overcome impaired extinction and thus to reduce learned fear. The AcbC was chosen based on evidence that stimulation of the AcbC enhances extinction-like cognitive performance in intractable obsessive-compulsive disorder patients (Lipsman et al., 2007; Burdick et al., 2009; Goodman et al., 2010; Greenberg et al., 2010; Grant et al., 2011) and is associated with long-term enhancement in cognitive performance on tests including attention, learning and memory in remitted depressed patients (Bewernick et al., 2012). Interestingly, the extinction promoting effect of AcbC stimulation was independent of any observable reduction of fear during extinction training. Reasons for this may be inferred from clinical studies showing that DBS of the AcbC can induce/enhance symptoms of fear and panic (palpitations and increased heart rate, flushing, fearful and panicky feelings) in patients (Shapira et al., 2006; Okun et al., 2007). Thus, assessment of potential reductions in freezing behaviour during the extinction session may be overlaid by enhancing fearful responses by DBS of the AcbC per se.
The exact mechanisms via which DBS of the AcbC promotes extinction are not fully understood and different hypotheses exist. DBS has been proposed to cause a functional lesion by suppressing neural activity at the stimulated brain area, or that DBS elicits stimulation-induced activation of axons resulting in a wide range of effects on local cells and at a circuit level (McIntyre et al., 2004). However, existing data indicate that suppression of AcbC activity may not mediate fear reductions directly since lesions of the AcbC (Riedel et al., 1997; Levita et al., 2002; Josselyn et al., 2005), or temporary inactivation (Haralambous and Westbrook, 1999; Rodriguez-Romaguera et al., 2012) do not disrupt fear responses regardless of how fear is measured (fear-potentiated startle or conditioned freezing). In addition, DBS of the AcbC does not evoke any change in local neurotransmitter release within this brain region (van Dijk et al., 2011) further negating a direct role of the AcbC mediating fear reduction. It is possible that DBS of the AcbC exerts its fear reducing effect at a circuit level to modulate pathological network activity, as our experiment used 130 Hz, 100 μA and 60 μs pulse width, conditions which can influence fibres of passage (Nowak and Bullier, 1998a,b) and induce changes in excitability and plasticity in brain regions critically involved in fear extinction. Specifically, DBS of the AcbC selectively increases slow oscillatory activity (McCracken and Grace, 2009) and supresses pyramidal cell firing (McCracken and Grace, 2007) in the orbitofrontal cortex, and increases spontaneous and stimulus-induced coherent activity between regions in the thalamocortical system, which are implicated in extinction circuitry [e.g. medial prefrontal cortex and mediodorsal thalamus (Pape and Pare, 2010; Lee et al., 2011)]. Furthermore, increased expression of phosphorylated extra cellular-regulated kinase (pERK), a marker of cell plasticity (Sweatt, 2004), is observed in brain regions critical for extinction learning including the medial prefrontal cortex, orbitofrontal cortex, and a small subregion of the lateral part of the central amygdala following DBS in the AcbC (Rodriguez-Romaguera et al., 2012), indicating that many of exactly those areas are targeted by AcbC DBS that have been shown to be aberrantly activated in extinction-impaired S1 mice (Whittle et al., 2010). Collectively, our results reveal for the first time that DBS of the AcbC rescued deficient extinction retrieval in an animal model of impaired extinction, most likely by positively interfering with the documented cortico-limbic extinction circuitry failure accompanying the impaired extinction.
4.3. Enhancing mGlu7 receptor activity during extinction training reduces fear in S1 mice
We have previously revealed that enhancing the activity of ionotropic NMDA receptors, via administration of DCS, is ineffective in inducing extinction acquisition in S1 mice (Hefner et al., 2008). Here, we investigated whether enhancing the activity of ionotropic AMPA receptors by administration of PEPA, or metabotropic mGlu7 receptors, by administration of AMN082, could rescue the extinction acquisition deficit in S1. Administration of AMN082, but not PEPA, prior to an extinction training session induced fear extinction and also reduced fear during a retrieval test in S1 mice. The lack of extinction promoting effect of PEPA is in contrast with published studies in normally behaving mice (Zushida et al., 2007). It is likely that PEPA, like DCS, facilitates the consolidation of extinction learning rather than inducing extinction learning per se (Davis et al., 2006). Evidence supporting this hypothesis is that long-term potentiation elicited by the AMPA receptor glutamate receptor 1 is necessary for the formation of emotional memories (Humeau et al., 2007).
The present finding that AMN082 rescued deficient extinction acquisition in S1 mice extends recent studies showing that AMN082, a specific allosteric modulator of mGlu7 receptors (Mitsukawa et al., 2005), impairs the acquisition of conditioned fear as well as facilitates between-session extinction in normally behaving rodents (Fendt et al., 2008; Siegl et al., 2008). Thus, AMN082, in addition to dietary zinc-restriction (see ‘Introduction’), constitute rare examples of treatments which enhance extinction learning, but not fear learning. Moreover, these results show that AMN082 can rescue extinction deficits in a psychopathological animal model, suggesting that AMN082 be used during extinction-based therapy to induce extinction learning in individuals with pathological fear.
At present, it is difficult to understand the extinction promoting effect of AMN082 (O'Connor et al., 2010). mGlu7 receptors, located entirely pre-synaptically, are widely distributed throughout the central nervous system (Ohishi et al., 1995). Activation of this receptor generally inhibits glutamatergic and GABAergic synaptic transmission (Schoepp, 2001), although facilitation of glutamatergic transmission has also been reported in specific brain regions (Millan et al., 2002; Li et al., 2008; Martin et al., 2010). Given the wide-spread distribution of mGlu7 receptors and their location on both glutamatergic and GABAergic axon terminals, the cumulative excitatory and inhibitory effects of systemic application of AMN082 is difficult to predict at present as precise knowledge of the location of the receptor in the microcircuits underlying fear extinction acquisition is lacking. Further studies on localised effects of AMN082 are warranted. Furthermore, recent findings reveal that a major metabolite of AMN082 inhibits serotonin-, dopamine- and noradrenaline-transporters (Sukoff Rizzo et al., 2011). As chronic treatment with the selective serotonin re-uptake inhibitor fluoxetine reduces fear in S1 mice (Camp et al., 2012) and protects against the return of fear in normally extinguishing mice (Karpova et al., 2011), we cannot exclude the contribution of enhanced monoaminergic neurotransmission in AMN082-induced reduction of fear.
4.4. Enhancing NMDA receptor activity after successful extinction learning reduces fear in S1 mice
A meta-analysis of published data shows that DCS is effective in reducing fear when combined with fear extinction or exposure therapy (Norberg et al., 2008). Results from normally extinguishing rodents show that DCS, administered immediately post extinction training, can lower fear by enhancing extinction memory consolidation (Ledgerwood et al., 2003). Clinically, DCS, combined with exposure-based therapy, is effective in reducing fear in patients with so-called simple fears including acrophobia, social anxiety, obsessive compulsive and panic disorders (Graham et al., 2010). However, in most cases beneficial effects of DCS were only apparent after a few exposure sessions further suggesting that the primary mechanism of DCS is to consolidate fear extinction memories. Along these lines, we have previously published that prior extinction training administration of DCS is ineffective in rescuing deficient extinction learning in S1 mice (Hefner et al., 2008). Here, using a novel behavioural finding that S1 mice display impaired extinction consolidation/retrieval we tested whether DCS is effective in lowering fear when administered following successful fear reduction in extinction learning. Results revealed that DCS rescued deficient extinction consolidation/retrieval in S1 mice. Thus, present data and that of Hefner et al. (2008) conclusively demonstrate that DCS can rescue deficient extinction learning only when administered during the extinction consolidation phase and that the efficacy of DCS is gated by the ability of S1 mice to acquire (at least to some extent) extinction acquisition. These results using a psychopathological animal model have clinical implications as they strengthen the suggestion that DCS be used as an add-on drug to facilitate reductions in fear by exposure therapy in specific anxiety disorders (Norberg et al., 2008; Davis, 2011).
4.5. HDAC inhibition rescues deficient extinction consolidation/retrieval
Recent studies have demonstrated that histone acetylation is dynamically regulated following successful extinction learning (Levenson et al., 2004; Fontan-Lozano et al., 2008; Bousiges et al., 2010; Peleg et al., 2010; Monsey et al., 2011; Stafford et al., 2012), and furthermore, that pharmacological or genetic silencing of HDAC enzyme isoforms can enhance fear extinction (Bredy et al., 2007; Lattal et al., 2007; Bredy and Barad, 2008; Guan et al., 2009; Monsey et al., 2011). Here, we first assessed whether MS-275, which is, using a chemoproteomic approach a HDAC1- 2- and 3-isoform inhibitor (Bantscheff et al., 2011), or using purified rhHDACs primarily a HDAC1- and 9-isoform inhibitor (Khan et al., 2008), could rescue deficient extinction consolidation/retrieval in “weak” fear conditioned S1 mice. We revealed that post extinction training administration of MS-275, at a dose with demonstrated HDAC inhibitory properties (Simonini et al., 2006), rescued deficient extinction consolidation/retrieval in S1 mice. It is likely that combined inhibition of HDAC1-, HADAC2- and HDAC3-isoforms contributes to the observed rescue of deficient extinction consolidation/retrieval in S1 mice. Pharmacological and/or genetic silencing of HDAC1- or HDAC2-isoforms have been shown to enhance the consolidation of fear and/or extinction memories (Guan et al., 2009; Bahari-Javan et al., 2012) and that genetic silencing of the HDAC3-isoform enhances long term memory in the object recognition test (McQuown et al., 2011). Notwithstanding, our data show for the first time that preferentially selective HDAC inhibitors such as MS-275 can rescue profound extinction consolidation/retrieval deficits in a psychopathological animal model and thus suggest that such compounds be used as an add-on drugs to facilitate reductions in fear in exposure-based therapy.
The extinction consolidation/retrieval-promoting effect of MS-275 was specific as results revealed that following “normal” fear conditioning, in which S1 mice display deficient extinction acquisition, prior extinction training administration of MS-275 did not induce extinction acquisition or reduce fear during a retrieval test. This indicates that rescue of deficient extinction acquisition requires mechanisms beyond HDAC inhibition. As enhancing GABAergic activity has been shown to significantly contribute to the molecular mechanisms underlying fear extinction [for example, see (Harris and Westbrook, 1998; Chhatwal et al., 2005; Akirav et al., 2006; Lin et al., 2009; Dalton et al., 2012)], we tested whether VPA, a pharmacological compound which enhances GABAergic signalling (Mimaki et al., 1984; Miller et al., 1988; Ko et al., 1997; Simonini et al., 2006) in addition to exhibiting robust HDAC inhibition (Kramer et al., 2003; Khan et al., 2008), can rescue impaired extinction acquisition and deficient extinction consolidation/retrieval. Indeed, our results revealed that prior extinction training administration of VPA rescued both deficient extinction acquisition and deficient extinction consolidation/retrieval in S1 mice. This result in a psychopathological animal model further extends findings showing prior extinction training administration of VPA potentiates reductions in fear extinction in normally extinguishing B6 mice (Bredy et al., 2007; Bredy and Barad, 2008) and, when administered prior to cognitive behavioural therapy, facilitates extinction in healthy humans (Kuriyama et al., 2011).
Our current result using a psychopathological animal model reveals that prior exposure-based extinction training administration of VPA, acutely applied, can rescue impaired extinction acquisition and deficient extinction consolidation/retrieval. This result has clear clinical applications. Specifically, to date, in preclinical animal models of impaired fear learning and neurodegeneration, cognitive enhancing effects of VPA have been shown only with chronic prior fear conditioning administration (Li et al., 2006; Dash et al., 2009; Kilgore et al., 2010). Our present result in a psychopathological animal model demonstrates the utility of a single VPA treatment in combination with exposure-based therapy to rescue impaired extinction acquisition and deficient extinction consolidation/retrieval. Furthermore, a number of small clinical studies demonstrate that chronic VPA monotherapy, for a minimum of eight weeks, reduces fear in social anxiety- (Kinrys et al., 2003), panic- (Primeau et al., 1990; Keck et al., 1993; Woodman and Noyes, 1994; Baetz and Bowen, 1998) and obsessive-compulsive- (Cora-Locatelli et al., 1998) disorder patients. Beneficial effects of chronic VPA monotherapy have also been reported in combat veterans with PTSD (Fesler, 1991; Otte et al., 2004), however, lacking effects are also reported (Davis et al., 2008; Hamner et al., 2009). A major drawback to chronic VPA monotherapy is that up to 25% of patients within the afore-mentioned studies are reported to stop medication due to adverse effects (including nausea, dizziness, fatigue, sedation and gastrointestinal complaints). Our current data suggests that acute VPA treatment, combined with exposure-based therapy may be an effective and novel clinical strategy to reduce fear in anxiety patients with minimal adverse effects.
5. Conclusions
In summary, we show that S1 mice are a unique psychopathological animal model as they display deficient extinction acquisition and deficient extinction retrieval, which can be experimentally dissociated by choosing different experimental conditioning setups. Using this mouse model the present data identify novel therapeutic targets that induce fear reductions when combined with extinction, resembling exposure-based therapy. Different pharmacological and non-pharmacological treatments that target cellular and molecular mechanisms with a documented or putative role in extinction memory formation within relevant brain areas and circuitries were chosen. This study reveals that DBS of the AcbC during exposure-based therapy may be a novel non-pharmacological treatment strategy to overcome impairments in reducing learned fear. Furthermore, that pharmacological enhancement of NMDA receptor activity or inhibition of HDAC1-, HDAC2- and HDAC3-isoforms, may rescue deficient extinction retrieval only following successful reductions in fear during extinction training, which can have important implications for the use of such agents in human exposure therapy. On the other hand, enhancing mGlu7 activity or enhancement in GABAergic activity in tandem with broad inhibition of HDAC isoforms could be a novel pharmacological treatment strategy to rescue both, impairments in extinction acquisition and extinction retrieval.
Acknowledgements
The authors would like to acknowledge that funding for this study was provided by the Austrian Science Funds FWF SFB F4410 (NS) and P22969-B11 (FF), and the NIAAA Intramural Research Program and Department of Defense in the Center for Neuroscience and Regenerative Medicine (AH). Neither the Austrian Science Fund nor NIH had a role in the study design; in the collection, analysis and interpretation of data; in the writing of the manuscript; or in the decision to submit the paper for publication.
References
- Akirav I., Raizel H., Maroun M. Enhancement of conditioned fear extinction by infusion of the GABA agonist muscimol into the rat prefrontal cortex and amygdala. Eur. J. Neurosci. 2006;23:758–764. doi: 10.1111/j.1460-9568.2006.04603.x. [DOI] [PubMed] [Google Scholar]
- Baetz M., Bowen R.C. Efficacy of divalproex sodium in patients with panic disorder and mood instability who have not responded to conventional therapy. Can. J. Psychiatry Revue canadienne de psychiatrie. 1998;43:73–77. doi: 10.1177/070674379804300109. [DOI] [PubMed] [Google Scholar]
- Bahari-Javan S., Maddalena A., Kerimoglu C., Wittnam J., Held T., Bahr M., Burkhardt S., Delalle I., Kugler S., Fischer A., Sananbenesi F. HDAC1 regulates fear extinction in mice. J. Neurosci. 2012;32:5062–5073. doi: 10.1523/JNEUROSCI.0079-12.2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bantscheff M., Hopf C., Savitski M.M., Dittmann A., Grandi P., Michon A.M., Schlegl J., Abraham Y., Becher I., Bergamini G., Boesche M., Delling M., Dumpelfeld B., Eberhard D., Huthmacher C., Mathieson T., Poeckel D., Reader V., Strunk K., Sweetman G., Kruse U., Neubauer G., Ramsden N.G., Drewes G. Chemoproteomics profiling of HDAC inhibitors reveals selective targeting of HDAC complexes. Nat. Biotechnol. 2011;29:255–265. doi: 10.1038/nbt.1759. [DOI] [PubMed] [Google Scholar]
- Barlow D.H., Gorman J.M., Shear M.K., Woods S.W. Cognitive-behavioral therapy, imipramine, or their combination for panic disorder: a randomized controlled trial. JAMA. 2000;283:2529–2536. doi: 10.1001/jama.283.19.2529. [DOI] [PubMed] [Google Scholar]
- Bewernick B.H., Kayser S., Sturm V., Schlaepfer T.E. Long-term effects of nucleus accumbens deep brain stimulation in treatment-resistant depression: evidence for sustained efficacy. Neuropsychopharmacology. 2012;37:1975–1985. doi: 10.1038/npp.2012.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blanchard R.J., Blanchard D.C. Crouching as an index of fear. J. Comp. Physiol. Psychol. 1969;67:370–375. doi: 10.1037/h0026779. [DOI] [PubMed] [Google Scholar]
- Bousiges O., Vasconcelos A.P., Neidl R., Cosquer B., Herbeaux K., Panteleeva I., Loeffler J.P., Cassel J.C., Boutillier A.L. Spatial memory consolidation is associated with induction of several lysine-acetyltransferase (histone acetyltransferase) expression levels and H2B/H4 acetylation-dependent transcriptional events in the rat hippocampus. Neuropsychopharmacology. 2010;35:2521–2537. doi: 10.1038/npp.2010.117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredy T.W., Barad M. The histone deacetylase inhibitor valproic acid enhances acquisition, extinction, and reconsolidation of conditioned fear. Learn. Mem. 2008;15:39–45. doi: 10.1101/lm.801108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bredy T.W., Wu H., Crego C., Zellhoefer J., Sun Y.E., Barad M. Histone modifications around individual BDNF gene promoters in prefrontal cortex are associated with extinction of conditioned fear. Learn. Mem. 2007;14:268–276. doi: 10.1101/lm.500907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick A., Goodman W.K., Foote K.D. Deep brain stimulation for refractory obsessive-compulsive disorder. Front. Biosci.: a Journal and Virtual Library. 2009;14:1880–1890. doi: 10.2741/3348. [DOI] [PubMed] [Google Scholar]
- Camp M., Norcross M., Whittle N., Feyder M., D'Hanis W., Yilmazer-Hanke D., Singewald N., Holmes A. Impaired Pavlovian fear extinction is a common phenotype across genetic lineages of the 129 inbred mouse strain. Genes Brain Behav. 2009;8:744–752. doi: 10.1111/j.1601-183X.2009.00519.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Camp M., MacPherson K.P., Lederle L., Graybeal C., Gaburro S., Debrouse L.M., Ihne J.L., Bravo J.A., O'Connor R.M., Ciocchi S., Wellman C.L., Luthi A., Cryan J.F., Singewald N., Holmes A. Genetic strain differences in learned fear inhibition associated with variation in neuroendocrine, autonomic, and amygdala dendritic phenotypes. Neuropsychopharmacology. 2012 doi: 10.1038/npp.2011.340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chhatwal J.P., Davis M., Maguschak K.A., Ressler K.J. Enhancing cannabinoid neurotransmission augments the extinction of conditioned fear. Neuropsychopharmacology. 2005;30:516–524. doi: 10.1038/sj.npp.1300655. [DOI] [PubMed] [Google Scholar]
- Chhatwal J.P., Stanek-Rattiner L., Davis M., Ressler K.J. Amygdala BDNF signaling is required for consolidation but not encoding of extinction. Nat. Neurosci. 2006;9:870–872. doi: 10.1038/nn1718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cora-Locatelli G., Greenberg B.D., Martin J.D., Murphy D.L. Valproate monotherapy in an SRI-intolerant OCD patient. J. Clin. Psychiatry. 1998;59:82. doi: 10.4088/jcp.v59n0207b. [DOI] [PubMed] [Google Scholar]
- Dalton G.L., Wu D.C., Wang Y.T., Floresco S.B., Phillips A.G. NMDA GluN2A and GluN2B receptors play separate roles in the induction of LTP and LTD in the amygdala and in the acquisition and extinction of conditioned fear. Neuropharmacology. 2012;62:797–806. doi: 10.1016/j.neuropharm.2011.09.001. [DOI] [PubMed] [Google Scholar]
- Dash P.K., Orsi S.A., Moore A.N. Histone deactylase inhibition combined with behavioral therapy enhances learning and memory following traumatic brain injury. Neuroscience. 2009;163:1–8. doi: 10.1016/j.neuroscience.2009.06.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson J.R., Foa E.B., Huppert J.D., Keefe F.J., Franklin M.E., Compton J.S., Zhao N., Connor K.M., Lynch T.R., Gadde K.M. Fluoxetine, comprehensive cognitive behavioral therapy, and placebo in generalized social phobia. Arch. Gen. Psychiatry. 2004;61:1005–1013. doi: 10.1001/archpsyc.61.10.1005. [DOI] [PubMed] [Google Scholar]
- Davis M., Ressler K., Rothbaum B.O., Richardson R. Effects of D-cycloserine on extinction: translation from preclinical to clinical work. Biol. Psychiatry. 2006;60:369–375. doi: 10.1016/j.biopsych.2006.03.084. [DOI] [PubMed] [Google Scholar]
- Davis L.L., Davidson J.R., Ward L.C., Bartolucci A., Bowden C.L., Petty F. Divalproex in the treatment of posttraumatic stress disorder: a randomized, double-blind, placebo-controlled trial in a veteran population. J. Clin. Psychopharmacol. 2008;28:84–88. doi: 10.1097/JCP.0b013e318160f83b. [DOI] [PubMed] [Google Scholar]
- Davis M. NMDA receptors and fear extinction: implications for cognitive behavioral therapy. Dialogues Clin. Neurosci. 2011;13:463–474. doi: 10.31887/DCNS.2011.13.4/mdavis. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fendt M., Schmid S., Thakker D.R., Jacobson L.H., Yamamoto R., Mitsukawa K., Maier R., Natt F., Husken D., Kelly P.H., McAllister K.H., Hoyer D., van der Putten H., Cryan J.F., Flor P.J. mGluR7 facilitates extinction of aversive memories and controls amygdala plasticity. Mol. Psychiatry. 2008;13:970–979. doi: 10.1038/sj.mp.4002073. [DOI] [PubMed] [Google Scholar]
- Fesler F.A. Valproate in combat-related posttraumatic stress disorder. J. Clin. Psychiatry. 1991;52:361–364. [PubMed] [Google Scholar]
- Foa E.B., Liebowitz M.R., Kozak M.J., Davies S., Campeas R., Franklin M.E., Huppert J.D., Kjernisted K., Rowan V., Schmidt A.B., Simpson H.B., Tu X. Randomized, placebo-controlled trial of exposure and ritual prevention, clomipramine, and their combination in the treatment of obsessive-compulsive disorder. Am. J. Psychiatry. 2005;162:151–161. doi: 10.1176/appi.ajp.162.1.151. [DOI] [PubMed] [Google Scholar]
- Fontan-Lozano A., Romero-Granados R., Troncoso J., Munera A., Delgado-Garcia J.M., Carrion A.M. Histone deacetylase inhibitors improve learning consolidation in young and in KA-induced-neurodegeneration and SAMP-8-mutant mice. Mol. Cell Neurosci. 2008;39:193–201. doi: 10.1016/j.mcn.2008.06.009. [DOI] [PubMed] [Google Scholar]
- Franklin G., Paxinos K. Academic Press; London: 2008. The Mouse Brain in Stereotaxic Coordinates. [Google Scholar]
- Goodman W.K., Foote K.D., Greenberg B.D., Ricciuti N., Bauer R., Ward H., Shapira N.A., Wu S.S., Hill C.L., Rasmussen S.A., Okun M.S. Deep brain stimulation for intractable obsessive compulsive disorder: pilot study using a blinded, staggered-onset design. Biol. Psychiatry. 2010;67:535–542. doi: 10.1016/j.biopsych.2009.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graham B.M., Langton J.M., Richardson R. Pharmacological enhancement of fear reduction: preclinical models. Br. J. Pharmacol. 2010 doi: 10.1111/j.1476-5381.2010.01175.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant J.E., Odlaug B.L., Chamberlain S.R. Neurocognitive response to deep brain stimulation for obsessive-compulsive disorder: a case report. Am. J. Psychiatry. 2011;168:1338–1339. doi: 10.1176/appi.ajp.2011.11071108. [DOI] [PubMed] [Google Scholar]
- Greenberg B.D., Gabriels L.A., Malone D.A., Jr., Rezai A.R., Friehs G.M., Okun M.S., Shapira N.A., Foote K.D., Cosyns P.R., Kubu C.S., Malloy P.F., Salloway S.P., Giftakis J.E., Rise M.T., Machado A.G., Baker K.B., Stypulkowski P.H., Goodman W.K., Rasmussen S.A., Nuttin B.J. Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: worldwide experience. Mol. Psychiatry. 2010;15:64–79. doi: 10.1038/mp.2008.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grubert C., Hurlemann R., Bewernick B.H., Kayser S., Hadrysiewicz B., Axmacher N., Sturm V., Schlaepfer T.E. Neuropsychological safety of nucleus accumbens deep brain stimulation for major depression: effects of 12-month stimulation. World J. Biol. Psychiatry: the Official Journal of the World Federation of Societies of Biological Psychiatry. 2011;12:516–527. doi: 10.3109/15622975.2011.583940. [DOI] [PubMed] [Google Scholar]
- Guan J.S., Haggarty S.J., Giacometti E., Dannenberg J.H., Joseph N., Gao J., Nieland T.J., Zhou Y., Wang X., Mazitschek R., Bradner J.E., DePinho R.A., Jaenisch R., Tsai L.H. HDAC2 negatively regulates memory formation and synaptic plasticity. Nature. 2009;459:55–60. doi: 10.1038/nature07925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamner M.B., Faldowski R.A., Robert S., Ulmer H.G., Horner M.D., Lorberbaum J.P. A preliminary controlled trial of divalproex in posttraumatic stress disorder. Ann. Clin. Psychiatry. 2009;21:89–94. [PubMed] [Google Scholar]
- Haralambous T., Westbrook R.F. An infusion of bupivacaine into the nucleus accumbens disrupts the acquisition but not the expression of contextual fear conditioning. Behav. Neurosci. 1999;113:925–940. doi: 10.1037//0735-7044.113.5.925. [DOI] [PubMed] [Google Scholar]
- Harris J.A., Westbrook R.F. Evidence that GABA transmission mediates context-specific extinction of learned fear. Psychopharmacology (Berl) 1998;140:105–115. doi: 10.1007/s002130050745. [DOI] [PubMed] [Google Scholar]
- Hefner K., Whittle N., Juhasz J., Norcross M., Karlsson R.M., Saksida L.M., Bussey T.J., Singewald N., Holmes A. Impaired fear extinction learning and cortico-amygdala circuit abnormalities in a common genetic mouse strain. J. Neurosci. 2008;28:8074–8085. doi: 10.1523/JNEUROSCI.4904-07.2008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herry C., Ferraguti F., Singewald N., Letzkus J.J., Ehrlich I., Luthi A. Neuronal circuits of fear extinction. Eur. J. Neurosci. 2010;31:599–612. doi: 10.1111/j.1460-9568.2010.07101.x. [DOI] [PubMed] [Google Scholar]
- Humeau Y., Reisel D., Johnson A.W., Borchardt T., Jensen V., Gebhardt C., Bosch V., Gass P., Bannerman D.M., Good M.A., Hvalby O., Sprengel R., Luthi A. A pathway-specific function for different AMPA receptor subunits in amygdala long-term potentiation and fear conditioning. J. Neurosci. 2007;27:10947–10956. doi: 10.1523/JNEUROSCI.2603-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Josselyn S.A., Falls W.A., Gewirtz J.C., Pistell P., Davis M. The nucleus accumbens is not critically involved in mediating the effects of a safety signal on behavior. Neuropsychopharmacology. 2005;30:17–26. doi: 10.1038/sj.npp.1300530. [DOI] [PubMed] [Google Scholar]
- Karpova N.N., Pickenhagen A., Lindholm J., Tiraboschi E., Kulesskaya N., Agustsdottir A., Antila H., Popova D., Akamine Y., Sullivan R., Hen R., Drew L.J., Castren E. Fear erasure in mice requires synergy between antidepressant drugs and extinction training. Science. 2011;334:1731–1734. doi: 10.1126/science.1214592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazantsev A.G., Thompson L.M. Therapeutic application of histone deacetylase inhibitors for central nervous system disorders. Nat. Rev. Drug Discov. 2008;7:854–868. doi: 10.1038/nrd2681. [DOI] [PubMed] [Google Scholar]
- Keck P.E., Jr., Taylor V.E., Tugrul K.C., McElroy S.L., Bennett J.A. Valproate treatment of panic disorder and lactate-induced panic attacks. Biol. Psychiatry. 1993;33:542–546. doi: 10.1016/0006-3223(93)90010-b. [DOI] [PubMed] [Google Scholar]
- Khan N., Jeffers M., Kumar S., Hackett C., Boldog F., Khramtsov N., Qian X., Mills E., Berghs S.C., Carey N., Finn P.W., Collins L.S., Tumber A., Ritchie J.W., Jensen P.B., Lichenstein H.S., Sehested M. Determination of the class and isoform selectivity of small-molecule histone deacetylase inhibitors. Biochem. J. 2008;409:581–589. doi: 10.1042/BJ20070779. [DOI] [PubMed] [Google Scholar]
- Kilgore M., Miller C.A., Fass D.M., Hennig K.M., Haggarty S.J., Sweatt J.D., Rumbaugh G. Inhibitors of class 1 histone deacetylases reverse contextual memory deficits in a mouse model of Alzheimer's disease. Neuropsychopharmacology. 2010;35:870–880. doi: 10.1038/npp.2009.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinrys G., Pollack M.H., Simon N.M., Worthington J.J., Nardi A.E., Versiani M. Valproic acid for the treatment of social anxiety disorder. Int. Clin. Psychopharmacol. 2003;18:169–172. doi: 10.1097/01.yic.0000064261.66765.9f. [DOI] [PubMed] [Google Scholar]
- Ko G.Y., Brown-Croyts L.M., Teyler T.J. The effects of anticonvulsant drugs on NMDA-EPSP, AMPA-EPSP, and GABA-IPSP in the rat hippocampus. Brain Res. Bull. 1997;42:297–302. doi: 10.1016/s0361-9230(96)00268-7. [DOI] [PubMed] [Google Scholar]
- Kramer O.H., Zhu P., Ostendorff H.P., Golebiewski M., Tiefenbach J., Peters M.A., Brill B., Groner B., Bach I., Heinzel T., Gottlicher M. The histone deacetylase inhibitor valproic acid selectively induces proteasomal degradation of HDAC2. EMBO J. 2003;22:3411–3420. doi: 10.1093/emboj/cdg315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuriyama K., Honma M., Soshi T., Fujii T., Kim Y. Effect of D-cycloserine and valproic acid on the extinction of reinstated fear-conditioned responses and habituation of fear conditioning in healthy humans: a randomized controlled trial. Psychopharmacology (Berl) 2011;218:589–597. doi: 10.1007/s00213-011-2353-x. [DOI] [PubMed] [Google Scholar]
- Lattal K.M., Barrett R.M., Wood M.A. Systemic or intrahippocampal delivery of histone deacetylase inhibitors facilitates fear extinction. Behav. Neurosci. 2007;121:1125–1131. doi: 10.1037/0735-7044.121.5.1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ledgerwood L., Richardson R., Cranney J. Effects of D-cycloserine on extinction of conditioned freezing. Behav. Neurosci. 2003;117:341–349. doi: 10.1037/0735-7044.117.2.341. [DOI] [PubMed] [Google Scholar]
- Lee S., Ahmed T., Kim H., Choi S., Kim D.S., Kim S.J., Cho J., Shin H.S. Bidirectional modulation of fear extinction by mediodorsal thalamic firing in mice. Nat. Neurosci. 2011;15:308–314. doi: 10.1038/nn.2999. [DOI] [PubMed] [Google Scholar]
- Levenson J.M., O'Riordan K.J., Brown K.D., Trinh M.A., Molfese D.L., Sweatt J.D. Regulation of histone acetylation during memory formation in the hippocampus. J. Biol. Chem. 2004;279:40545–40559. doi: 10.1074/jbc.M402229200. [DOI] [PubMed] [Google Scholar]
- Levita L., Dalley J.W., Robbins T.W. Nucleus accumbens dopamine and learned fear revisited: a review and some new findings. Behav. Brain Res. 2002;137:115–127. doi: 10.1016/s0166-4328(02)00287-5. [DOI] [PubMed] [Google Scholar]
- Li S., Murakami Y., Wang M., Maeda K., Matsumoto K. The effects of chronic valproate and diazepam in a mouse model of posttraumatic stress disorder. Pharmacol. Biochem. Behav. 2006;85:324–331. doi: 10.1016/j.pbb.2006.08.015. [DOI] [PubMed] [Google Scholar]
- Li X., Gardner E.L., Xi Z.X. The metabotropic glutamate receptor 7 (mGluR7) allosteric agonist AMN082 modulates nucleus accumbens GABA and glutamate, but not dopamine, in rats. Neuropharmacology. 2008;54:542–551. doi: 10.1016/j.neuropharm.2007.11.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin H.C., Mao S.C., Gean P.W. Block of gamma-aminobutyric acid-a receptor insertion in the amygdala impairs extinction of conditioned fear. Biol. Psychiatry. 2009;66:665–673. doi: 10.1016/j.biopsych.2009.04.003. [DOI] [PubMed] [Google Scholar]
- Lipsman N., Neimat J.S., Lozano A.M. Deep brain stimulation for treatment-refractory obsessive-compulsive disorder: the search for a valid target. Neurosurgery. 2007;61:1–11. doi: 10.1227/01.neu.0000279719.75403.f7. discussion 11–13. [DOI] [PubMed] [Google Scholar]
- Martin R., Durroux T., Ciruela F., Torres M., Pin J.P., Sanchez-Prieto J. The metabotropic glutamate receptor mGlu7 activates phospholipase C, translocates munc-13-1 protein, and potentiates glutamate release at cerebrocortical nerve terminals. J. Biol. Chem. 2010;285:17907–17917. doi: 10.1074/jbc.M109.080838. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken C.B., Grace A.A. High-frequency deep brain stimulation of the nucleus accumbens region suppresses neuronal activity and selectively modulates afferent drive in rat orbitofrontal cortex in vivo. J. Neurosci. 2007;27:12601–12610. doi: 10.1523/JNEUROSCI.3750-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken C.B., Grace A.A. Nucleus accumbens deep brain stimulation produces region-specific alterations in local field potential oscillations and evoked responses in vivo. J. Neurosci. 2009;29:5354–5363. doi: 10.1523/JNEUROSCI.0131-09.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGaugh J.L. Memory–a century of consolidation. Science. 2000;287:248–251. doi: 10.1126/science.287.5451.248. [DOI] [PubMed] [Google Scholar]
- McIntyre C.C., Savasta M., Walter B.L., Vitek J.L. How does deep brain stimulation work? Present understanding and future questions. J. Clin. Neurophysiol.: Official Publication of the American Electroencephalographic Society. 2004;21:40–50. doi: 10.1097/00004691-200401000-00006. [DOI] [PubMed] [Google Scholar]
- McQuown S.C., Barrett R.M., Matheos D.P., Post R.J., Rogge G.A., Alenghat T., Mullican S.E., Jones S., Rusche J.R., Lazar M.A., Wood M.A. HDAC3 is a critical negative regulator of long-term memory formation. J. Neurosci. 2011;31:764–774. doi: 10.1523/JNEUROSCI.5052-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Milad M.R., Pitman R.K., Ellis C.B., Gold A.L., Shin L.M., Lasko N.B., Zeidan M.A., Handwerger K., Orr S.P., Rauch S.L. Neurobiological basis of failure to recall extinction memory in posttraumatic stress disorder. Biol. Psychiatry. 2009;66:1075–1082. doi: 10.1016/j.biopsych.2009.06.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millan C., Lujan R., Shigemoto R., Sanchez-Prieto J. The inhibition of glutamate release by metabotropic glutamate receptor 7 affects both [Ca2+]c and cAMP: evidence for a strong reduction of Ca2+ entry in single nerve terminals. J. Biol. Chem. 2002;277:14092–14101. doi: 10.1074/jbc.M109044200. [DOI] [PubMed] [Google Scholar]
- Miller L.G., Greenblatt D.J., Barnhill J.G., Summer W.R., Shader R.I. 'GABA shift' in vivo: enhancement of benzodiazepine binding in vivo by modulation of endogenous GABA. Eur. J. Pharmacol. 1988;148:123–130. doi: 10.1016/0014-2999(88)90461-x. [DOI] [PubMed] [Google Scholar]
- Mimaki T., Yabuuchi H., Laird H., Yamamura H.I. Effects of seizures and antiepileptic drugs on benzodiazepine receptors in rat brain. Pediatr. Pharmacol. (New York) 1984;4:205–211. [PubMed] [Google Scholar]
- Mitsukawa K., Yamamoto R., Ofner S., Nozulak J., Pescott O., Lukic S., Stoehr N., Mombereau C., Kuhn R., McAllister K.H., van der Putten H., Cryan J.F., Flor P.J. A selective metabotropic glutamate receptor 7 agonist: activation of receptor signaling via an allosteric site modulates stress parameters in vivo. Proc. Natl. Acad. Sci. U S A. 2005;102:18712–18717. doi: 10.1073/pnas.0508063102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Monsey M.S., Ota K.T., Akingbade I.F., Hong E.S., Schafe G.E. Epigenetic alterations are critical for fear memory consolidation and synaptic plasticity in the lateral amygdala. PLoS One. 2011;6:e19958. doi: 10.1371/journal.pone.0019958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers K.M., Davis M. Mechanisms of fear extinction. Mol. Psychiatry. 2007;12:120–150. doi: 10.1038/sj.mp.4001939. [DOI] [PubMed] [Google Scholar]
- Myers K.M., Carlezon W.A., Jr., Davis M. Glutamate receptors in extinction and extinction-based therapies for psychiatric illness. Neuropsychopharmacology. 2011;36:274–293. doi: 10.1038/npp.2010.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norberg M.M., Krystal J.H., Tolin D.F. A meta-analysis of D-cycloserine and the facilitation of fear extinction and exposure therapy. Biol. Psychiatry. 2008;63:1118–1126. doi: 10.1016/j.biopsych.2008.01.012. [DOI] [PubMed] [Google Scholar]
- Nowak L.G., Bullier J. Axons, but not cell bodies, are activated by electrical stimulation in cortical gray matter. I. Evidence from chronaxie measurements. Exp. Brain Res. 1998;118:477–488. doi: 10.1007/s002210050304. [DOI] [PubMed] [Google Scholar]
- Nowak L.G., Bullier J. Axons, but not cell bodies, are activated by electrical stimulation in cortical gray matter. II. Evidence from selective inactivation of cell bodies and axon initial segments. Exp. Brain Res. 1998;118:489–500. doi: 10.1007/s002210050305. [DOI] [PubMed] [Google Scholar]
- Nutt D.J. Overview of diagnosis and drug treatments of anxiety disorders. CNS Spectr. 2005;10:49–56. doi: 10.1017/s1092852900009901. [DOI] [PubMed] [Google Scholar]
- O'Connor R.M., Finger B.C., Flor P.J., Cryan J.F. Metabotropic glutamate receptor 7: at the interface of cognition and emotion. Eur. J. Pharmacol. 2010;639:123–131. doi: 10.1016/j.ejphar.2010.02.059. [DOI] [PubMed] [Google Scholar]
- Ohishi H., Nomura S., Ding Y.Q., Shigemoto R., Wada E., Kinoshita A., Li J.L., Neki A., Nakanishi S., Mizuno N. Presynaptic localization of a metabotropic glutamate receptor, mGluR7, in the primary afferent neurons: an immunohistochemical study in the rat. Neurosci. Lett. 1995;202:85–88. doi: 10.1016/0304-3940(95)12207-9. [DOI] [PubMed] [Google Scholar]
- Okun M.S., Mann G., Foote K.D., Shapira N.A., Bowers D., Springer U., Knight W., Martin P., Goodman W.K. Deep brain stimulation in the internal capsule and nucleus accumbens region: responses observed during active and sham programming. J. Neurol. Neurosurg. Psychiatry. 2007;78:310–314. doi: 10.1136/jnnp.2006.095315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Olesen J., Gustavsson A., Svensson M., Wittchen H.U., Jonsson B. The economic cost of brain disorders in Europe. Eur. J. Neurol.: the Official Journal of the European Federation of Neurological Societies. 2012;19:155–162. doi: 10.1111/j.1468-1331.2011.03590.x. [DOI] [PubMed] [Google Scholar]
- Orsini C.A., Maren S. Neural and cellular mechanisms of fear and extinction memory formation. Neurosci. Biobehav. Rev. 2012 doi: 10.1016/j.neubiorev.2011.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Otte C., Wiedemann K., Yassouridis A., Kellner M. Valproate monotherapy in the treatment of civilian patients with non-combat-related posttraumatic stress disorder: an open-label study. J. Clin. Psychopharmacol. 2004;24:106–108. doi: 10.1097/01.jcp.0000106234.36344.a4. [DOI] [PubMed] [Google Scholar]
- Pape H.C., Pare D. Plastic synaptic networks of the amygdala for the acquisition, expression, and extinction of conditioned fear. Physiol. Rev. 2010;90:419–463. doi: 10.1152/physrev.00037.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peleg S., Sananbenesi F., Zovoilis A., Burkhardt S., Bahari-Javan S., Agis-Balboa R.C., Cota P., Wittnam J.L., Gogol-Doering A., Opitz L., Salinas-Riester G., Dettenhofer M., Kang H., Farinelli L., Chen W., Fischer A. Altered histone acetylation is associated with age-dependent memory impairment in mice. Science. 2010;328:753–756. doi: 10.1126/science.1186088. [DOI] [PubMed] [Google Scholar]
- Primeau F., Fontaine R., Beauclair L. Valproic acid and panic disorder. Can. journal Psychiatry Revue Canadienne De Psychiatrie. 1990;35:248–250. doi: 10.1177/070674379003500309. [DOI] [PubMed] [Google Scholar]
- Quirk G.J., Mueller D. Neural mechanisms of extinction learning and retrieval. Neuropsychopharmacology. 2008;33:56–72. doi: 10.1038/sj.npp.1301555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ressler K.J., Rothbaum B.O., Tannenbaum L., Anderson P., Graap K., Zimand E., Hodges L., Davis M. Cognitive enhancers as adjuncts to psychotherapy: use of D-cycloserine in phobic individuals to facilitate extinction of fear. Arch. Gen. Psychiatry. 2004;61:1136–1144. doi: 10.1001/archpsyc.61.11.1136. [DOI] [PubMed] [Google Scholar]
- Richardson R., Ledgerwood L., Cranney J. Facilitation of fear extinction by D-cycloserine: theoretical and clinical implications. Learn. Mem. 2004;11:510–516. doi: 10.1101/lm.78204. [DOI] [PubMed] [Google Scholar]
- Riedel G., Harrington N.R., Hall G., Macphail E.M. Nucleus accumbens lesions impair context, but not cue, conditioning in rats. Neuroreport. 1997;8:2477–2481. doi: 10.1097/00001756-199707280-00013. [DOI] [PubMed] [Google Scholar]
- Rodriguez-Romaguera J., Do Monte F.H., Quirk G.J. Deep brain stimulation of the ventral striatum enhances extinction of conditioned fear. Proc. Natl. Acad. Sci. U S A. 2012 doi: 10.1073/pnas.1200782109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoepp D.D. Unveiling the functions of presynaptic metabotropic glutamate receptors in the central nervous system. J. Pharmacol. Exp. Ther. 2001;299:12–20. [PubMed] [Google Scholar]
- Shapira N.A., Okun M.S., Wint D., Foote K.D., Byars J.A., Bowers D., Springer U.S., Lang P.J., Greenberg B.D., Haber S.N., Goodman W.K. Panic and fear induced by deep brain stimulation. J. Neurol. Neurosurg. Psychiatry. 2006;77:410–412. doi: 10.1136/jnnp.2005.069906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegl S., Flor P.J., Fendt M. Amygdaloid metabotropic glutamate receptor subtype 7 is involved in the acquisition of conditioned fear. Neuroreport. 2008;19:1147–1150. doi: 10.1097/WNR.0b013e328307f295. [DOI] [PubMed] [Google Scholar]
- Simonini M.V., Camargo L.M., Dong E., Maloku E., Veldic M., Costa E., Guidotti A. The benzamide MS-275 is a potent, long-lasting brain region-selective inhibitor of histone deacetylases. Proc. Natl. Acad. Sci. U S A. 2006;103:1587–1592. doi: 10.1073/pnas.0510341103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soliman F., Glatt C.E., Bath K.G., Levita L., Jones R.M., Pattwell S.S., Jing D., Tottenham N., Amso D., Somerville L.H., Voss H.U., Glover G., Ballon D.J., Liston C., Teslovich T., Van Kempen T., Lee F.S., Casey B.J. A genetic variant BDNF polymorphism alters extinction learning in both mouse and human. Science. 2010;327:863–866. doi: 10.1126/science.1181886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sotres-Bayon F., Bush D.E., LeDoux J.E. Acquisition of fear extinction requires activation of NR2B-containing NMDA receptors in the lateral amygdala. Neuropsychopharmacology. 2007;32:1929–1940. doi: 10.1038/sj.npp.1301316. [DOI] [PubMed] [Google Scholar]
- Stafford J.M., Raybuck J.D., Ryabinin A.E., Lattal, K.M. Increasing histone acetylation in the hippocampus-infralimbic network enhances fear extinction. Biol. Psychiatry. 2012;72(1):25–33. doi: 10.1016/j.biopsych.2011.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steckler T., Risbrough V. Pharmacological treatment of PTSD – established and new approaches. Neuropharmacology. 2011 doi: 10.1016/j.neuropharm.2011.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sukoff Rizzo S.J., Leonard S.K., Gilbert A., Dollings P., Smith D.L., Zhang M.Y., Di L., Platt B.J., Neal S., Dwyer J.M., Bender C.N., Zhang J., Lock T., Kowal D., Kramer A., Randall A., Huselton C., Vishwanathan K., Tse S.Y., Butera J., Ring R.H., Rosenzweig-Lipson S., Hughes Z.A., Dunlop J. The metabotropic glutamate receptor 7 allosteric modulator AMN082: a monoaminergic agent in disguise? J. Pharmacol. Exp. Ther. 2011;338:345–352. doi: 10.1124/jpet.110.177378. [DOI] [PubMed] [Google Scholar]
- Sweatt J.D. Mitogen-activated protein kinases in synaptic plasticity and memory. Curr. Opin. Neurobiol. 2004;14:311–317. doi: 10.1016/j.conb.2004.04.001. [DOI] [PubMed] [Google Scholar]
- Tremolizzo L., Doueiri M.S., Dong E., Grayson D.R., Davis J., Pinna G., Tueting P., Rodriguez-Menendez V., Costa E., Guidotti A. Valproate corrects the schizophrenia-like epigenetic behavioral modifications induced by methionine in mice. Biol. Psychiatry. 2005;57:500–509. doi: 10.1016/j.biopsych.2004.11.046. [DOI] [PubMed] [Google Scholar]
- Tronson N.C., Corcoran K.A., Jovasevic V., Radulovic J. Fear conditioning and extinction: emotional states encoded by distinct signaling pathways. Trends Neurosci. 2012;35:145–155. doi: 10.1016/j.tins.2011.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Dijk A., Mason O., Klompmakers A.A., Feenstra M.G., Denys D. Unilateral deep brain stimulation in the nucleus accumbens core does not affect local monoamine release. J. Neurosci. Methods. 2011;202:113–118. doi: 10.1016/j.jneumeth.2011.04.034. [DOI] [PubMed] [Google Scholar]
- Walker D.L., Davis M. The role of amygdala glutamate receptors in fear learning, fear-potentiated startle, and extinction. Pharmacol. Biochem. Behav. 2002;71:379–392. doi: 10.1016/s0091-3057(01)00698-0. [DOI] [PubMed] [Google Scholar]
- Whittle N., Hauschild M., Lubec G., Holmes A., Singewald N. Rescue of impaired fear extinction and normalization of cortico-amygdala circuit dysfunction in a genetic mouse model by dietary zinc restriction. J. Neurosci. 2010;30:13586–13596. doi: 10.1523/JNEUROSCI.0849-10.2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Woodman C.L., Noyes R., Jr. Panic disorder: treatment with valproate. J. Clin. Psychiatry. 1994;55:134–136. [PubMed] [Google Scholar]
- Yamada D., Zushida K., Wada K., Sekiguchi M. Pharmacological discrimination of extinction and reconsolidation of contextual fear memory by a potentiator of AMPA receptors. Neuropsychopharmacology. 2009;34:2574–2584. doi: 10.1038/npp.2009.86. [DOI] [PubMed] [Google Scholar]
- Yehuda R., LeDoux J. Response variation following trauma: a translational neuroscience approach to understanding PTSD. Neuron. 2007;56:19–32. doi: 10.1016/j.neuron.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Zushida K., Sakurai M., Wada K., Sekiguchi M. Facilitation of extinction learning for contextual fear memory by PEPA: a potentiator of AMPA receptors. J. Neurosci. 2007;27:158–166. doi: 10.1523/JNEUROSCI.3842-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]