Abstract
Aims and objectives: Heatwaves can pose a severe threat to health, especially to older people. However, warnings do not necessarily lead to preventive action. This study aims at exploring individual risk perception and adaptive measures of older people and their carers. Their views are explored, taking into account personal backgrounds.
Methods: Questionnaire-based interviews were administered to 20 men and women (64–94 years, living in their own homes or nursing homes) and 13 carers. A qualitative analysis following a framework approach was performed.
Results: The majority of respondents stated that older people might be compromised by heatwaves; however, a large proportion of respondents saw themselves as less affected than the average population. Most respondents adopted preventive measures during heatwaves and a majority received warnings or pieces of information. The role of general practitioners in direct warning situations was judged controversial. Survey respondents displayed resistance to the use of technical devices to monitor potentially dangerous situations.
In addition, the results support many previous findings. In particular, the relative concepts of ageing, variety of information channels used, and control orientations could be confirmed.
Conclusions: General practitioners hold a position of trust and play a central role in the promotion of preventive action, but there are also limitations to their outreach. Many respondents could be classified as socially active, which has implications for preventive information campaigns. Information campaigns using different channels and targeting a larger audience should be considered. The degree of information of carers can partly be improved.
Keywords: older people, carers, preventive care, behavioural change, heatwaves, risk perception
Abstract
Zielsetzung: Hitzewellen können insbesondere für ältere Menschen eine ernstzunehmende gesundheitliche Bedrohung darstellen. Allerdings führen Warnungen nicht notwendigerweise zum Ergreifen von Schutzmaßnahmen. Diese Studie zielt auf die Exploration der individuellen Risikowahrnehmung sowie Anpassungsmaßnahmen älterer Menschen und ihrer Pflegepersonen. Ihre Ansichten werden unter Berücksichtigung persönlicher Hintergründe exploriert.
Methodik: Fragebogenbasierte Interviews wurden mit 20 älteren Menschen (64–94 Jahre, in Pflegeheimen oder zuhause lebend) und 13 Pflegepersonen durchgeführt. Eine qualitative Analyse im Sinne eines Framework Approach wurde durchgeführt.
Ergebnisse: Die Mehrzahl der Probanden äußerte, dass ältere Menschen durch Hitzewellen beeinträchtigt sein könnten; dennoch schätzte sich eine große Zahl von Befragten als unterdurchschnittlich gefährdet ein. Die meisten Probanden ergriffen während Hitzewellen Schutzmaßnahmen und eine Mehrheit erhielt Warnungen oder Informationen. Die Rolle des Hausarztes wurde in diesem Zusammenhang kontrovers beurteilt. Die Probanden stellten sich gegen die Nutzung technischer Hilfsmittel zur Überwachung potentiell gefährlicher Situationen. Im Übrigen unterstützen die Ergebnisse der Studie einige frühere Erkenntnisse. Insbesondere relative Alternskonzepte, die Vielzahl der genutzten Informationswege und Kontrolleinstellungen konnten bestätigt werden.
Fazit: Hausärzte besitzen eine besondere Vertrauensposition und spielen eine zentrale Rolle in der Förderung von Anpassungsmaßnahmen, allerdings ist der Radius ihres Einflusses begrenzt. Viele der Probanden konnten als sozial aktiv eingestuft werden, was für zukünftige Informationskampagnen von Bedeutung ist. Hierbei sollte die Nutzung diverser Informationswege und ein breiterer Adressatenkreis erwogen werden. Der Informationsgrad von Pflegepersonen kann teilweise verbessert werden.
Introduction
Heatwaves can pose a severe threat to the health of older people. Numerous studies have shown high excess mortalities, for example in 2003 [1], [2]. Projections indicate that this threat will increase in the course of the next century [3]. Longer and more intense heatwaves are expected to coincide with larger numbers of older people [4].
Heat can directly affect people’s health, increasing amongst others cardiovascular and respiratory mortality and deteriorating pre-existing chronic diseases [5].
Especially vulnerable groups of people include older people, chronically ill people and those living alone [1], [6]. But also being bound to bed and psychiatric disorders can aggravate the potential danger [7].
In Germany, few studies have yet analysed the effects of heatwaves on mortality; results from Essen [8] and Frankfurt [9] for the 2003 heatwave showed excess mortalities of 27% or 47% to 97%, respectively. Currently, only very limited data are available for small or medium sized cities. However, the authors of this article performed a study in Freiburg, aiming at closing this gap, and found excess mortalities of 26% to 33% in 2003 [10]. For the province of Baden-Wuerttemberg (general population: 10 million), excess mortality has been estimated to be 20%, which amounts to 900 to 1,300 excess deaths during the heatwaves in 2003 [11]. It has to be underlined, that the effects of heatwaves are more pronounced in cities, thus causing higher excess mortalities [12].
To deal with this situation, public health actions are being designed by government and health agencies to protect the population. A special focus is put on older people and other vulnerable subgroups identified so far [13]. Warning systems and information about possible preventive actions are used and made available. Pilot studies in Germany [14] try to raise awareness and build up networks for common action, including risk assessments, other projects in Italy [15] register those at high risk and use volunteers to make control visits at older people’s homes during heatwaves. So far, there are no standardized warning protocols in Germany; the heat information service (located at the German Weather Service) issues warnings which are transmitted to nursing homes. Other actions have to be organised by the communities and cities themselves. The media coverage of warnings has not been sufficiently studied yet. However, there is evidence that many people do not sufficiently react to warnings, even if they reach them [16]. The self-perceptions of vulnerable individuals have been identified as a key aspect of resistance to preventive action [17]; this construct closely interacts with the individual’s subjective judgement of risk’s properties and implications [18]. The evaluation of efficiency and efficacy of public health interventions is currently under scientific investigation; first results tend to the conclusion that systems implementing more measures than just warnings seem to be more effective [13].
Telephone surveys and interview studies revealed several important aspects about perceptions of older people. Self-concepts of aging, and regarding oneself as less vulnerable than others were identified as important aspects [16], [19]. There are different approaches to explain the low degrees of perceived threat. These include the concept of unrealistic optimism, stating that it is natural for people to believe that they are less in danger than others and that their preventive measures are more effective than those of others [20], [21]. This belief can inhibit proactive behaviour and prevent individuals from addressing their weaknesses.
Other studies focused on the reasons why older people do not perceive themselves as vulnerable. Though asking for proactive behaviour in regard to potential future care requirements, the results of Pinquart’s study [22] are nevertheless valuable for the discussion in the field of heatwave research. By denying their vulnerability, people were protecting their current (psychological) well-being. Worrying about future health problems was reported to deteriorate their current well-being. This could mean that low degrees of perceived risk might not only result from a lack of information or self-consciousness, but might rather represent a coping strategy.
This hypothesis has not yet been further examined.
In the US, it has been shown that many older people received warnings or information, but fewer reacted to this information [17]. However, these findings changed when a special population was examined: a group of chronically ill people directly recruited from university hospitals. Many of these people perceived themselves as vulnerable and used appropriate preventive strategies [23]. These results may indicate that people who are aware of their constraints are more likely to react to warnings. If preventive measures are taken, people seem to concentrate on few strategies [16]. This could mean that only a few strategies are being transported by the information channels or that only a few strategies are remembered and put in effect, e.g. because of overwhelming information or because of the easy recollection of some of the measures. The answer to this question has consequences for the design of information campaigns, leaflets, etc.
The degree of information regarding heatwave-associated aspects of warning and care demonstrated by carers has not been thoroughly analysed yet. First results find either ill- [24] or well-informed personnel [25]. This matter is of special importance because ignorant or uninformed carers can pose a real threat to those for whom they are responsible [26]. This is due to the fact that the carers can act as important sources of information, being responsible for transmitting warnings to the older people and also for taking appropriate preventive measures (especially for impaired people).
A model study in the UK used semi-structured interviews in a sample of older people [19]. Their findings are that older people do not perceive themselves as particularly vulnerable; however, risks were recognized in others. Most respondents changed their daily routine during hot weather. Advice and information was judged positive, whereas more intense state interventions were seen as unnecessary. In regard of health and social care workers, deficits concerning knowledge about the national heatwave plans, a low perceived hazard to older people and difficulties in implementing as well as suggestions to use a multi-faceted approach were stated [24].
Methods
This study analysed perceptions and reported preventive actions by interviewing a sample of older people and their carers in Freiburg, southwest Germany. The aim was to reveal new information and to confirm existing knowledge in this emerging field of research. Taking into account the results other studies revealed so far, we aimed at further elucidating the following key questions: What advice is received? Do older people change their behaviour? If yes, how? If no, why not? The answers to these questions can add new insights into the perceptions of one particularly vulnerable subgroup. In addition to making direct comparisons to two studies which have been conducted in London and Norwich, UK [19], [24], it is also an aim of this study to contribute to possible following steps of quantitative research [27].
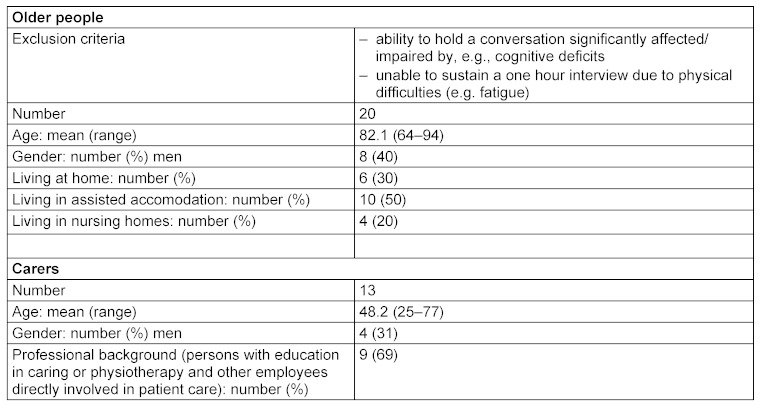
Individuals were selected from different urban quarters, representing differently deprived areas (according to the statistical bureau of the city of Freiburg), and from a broad age-range from 64 years upwards. In addition, the individuals partly lived in their own homes and partly in nursing homes. The aim was to diversify the interview sample, thus increasing the chances of getting to know different approaches and attitudes. Detailed information about the study population can be found in Table 1 (Tab. 1).
Table 1. Characteristics of the study population.
For recruitment purposes, three different channels were used. First, the nursing homes were contacted directly and asked to provide one or two interviewees (a random selection from amongst the different providers was made). Second, institutions of ambulatory care and centers for older people were used to contact individuals living at home. Third, one interviewee was recruited directly.
The institutions contacted had been asked to provide one or two interviewees of different age and gender if possible. So the staff independently chose individuals deemed intellectually able and willing to participate in a one-hour interview. There were few explicit inclusion and exclusion criteria. The potential interviewees had to be over 64 years of age and physically as well as mentally able to conduct a one-hour interview. Severe dementia and similar factors were used as exclusion criteria. Apart from this, the willingness of nursing home residents to participate determined the inclusion.
Information about participants’ medical history was received by the nursing homes, if applicable, otherwise by the individuals directly.
The interview guide was adopted from Abrahamson, who conducted a semi-structured interview study with 73 individuals in London and Norwich, UK in 2007 [19]. The topic guide contained 43 questions. The topics covered included the perception of the last heat episode and actions taken then, impairments due to hot weather, general measures taken under these circumstances, advice and information received, general living conditions, household characteristics and outdoor and leisure activities. The interviews were located in the interviewees’ homes – for their convenience and to make sure that adaptation strategies could be more easily remembered. The 20 interviews with older people were tape-recorded in full length and the answers given were also written down in short notes during the interview. The carers’ interviews were shorter (25 questions) and the answers were written down only: no tape-records were requried because of the short duration of these interviews, making comprehensive note-taking possible. The interviews were conducted by the first-author in September 2009.
The analysis of the interviews was carried out in close accordance to Abrahamson [19], who used a framework approach with its theme-based structure [28]. The framework approach consists of five consecutive steps, namely familiarization, identification of a thematic framework, indexing, charting and mapping and interpretation [29].
Therefore, following the process outlined above, having submerged into the data corresponding themes which were either given through the structure of the interview guide or which emerged in different interviews were identified through close study of the written protocols and accordingly grouped in a chart. This chart evolved with the progression through the interviews, including steps of re-grouping and merging themes and including new themes [30]. Hypotheses formed during the process were tested for consistency and applicability incorporating all available data and hence either approved or dropped [31].
After completion, this process yielded a scheme with five major themes or categories which were used as a guide for interpretation. Hence, direct comparison between the interviews, quantification of certain statements and linking of corresponding attitudes were rendered possible. However, it has to be noted that due to the small sample size and the assumed selection of relatively hale interviewees only very limited statements concerning frequencies of views and opinions in the general population can be made. Therefore, the reported incidences are mainly given to illustrate the relative prevalence of statements in the study sample.
Quality assurance aspects were also addressed [32]: Besides the aforementioned diversification of the sample, deviant cases were also being discussed. In addition, the interviews with the carers allowed to cross-check their experiences with those from the older people. This process of triangulation also improved the comprehensiveness of the data. All interviews were conducted by the same person to ensure comparability of data acquisition. In terms of reflexivity, the authors report of no prior assumptions in addition to those set by the research questions. Distance between the researcher and the interviewees remained at a professional, yet friendly and open level. The protocols were checked for completeness using the tape-records.
Results
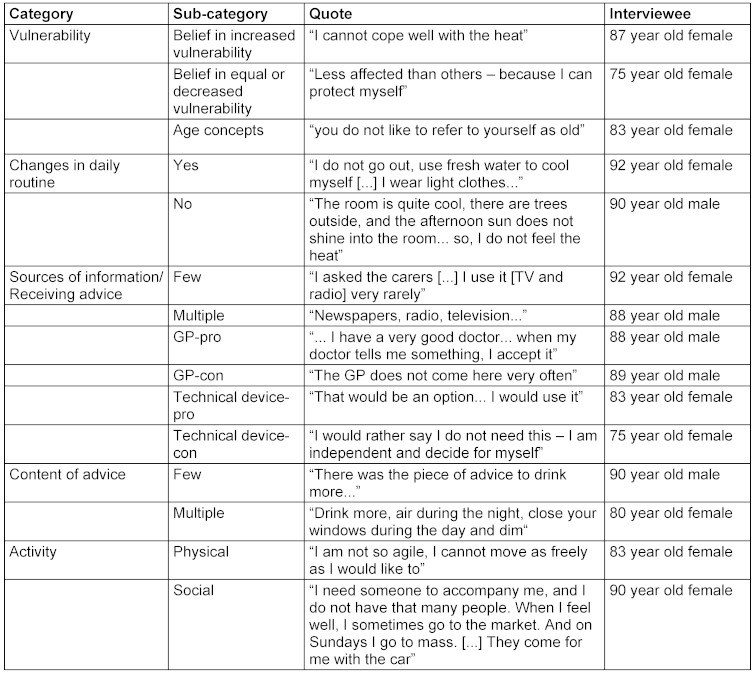
In the interpretation process outlined above, five major themes could be identified. These can be subsumed under the headwords vulnerability, changes in daily routine, sources of information, content of advice received and activity level and health status. Exemplary quotes are given in Table 2 (Tab. 2).
Table 2. Exemplary prototypical quotes for the categories and sub-categories of the interviews with 20 older people.
Most of the respondents (16 out of 20) claimed that older people might be a vulnerable group. However, some of these respondents went on to say that health status rather than age was a decisive factor in determining vulnerability. A minority of respondents (4) regarded themselves as higher-than-average endangered by heat waves compared to the rest of the population. In contrast, a larger group (8) regarded themselves below average endangered. Others mentioned that ill people (14), small children (4) and overweight people (3) should be regarded as vulnerable groups. When differentiating between different diseases connected with increased risks, cardiovascular problems (6) and being bed-ridden (3) were stated.
Except for one individual, all respondents stated that they changed their daily routine during heat. The preventive strategies mentioned included darkening the home (19), wearing light clothes (19), staying indoors (15) and drinking more fluids (14). Two respondents said they used a fan; two cooled themselves by using cool water. There were two individuals claiming that they were not allowed to drink more because their general practitioner (GP) told them how much to drink.
Two thirds of the respondents received warnings or other information. Nursing services (4), television (8), newspapers and magazines (5), and the radio (3) were the most common sources mentioned. When asked for the best way to be informed, respondents stated the same sources they had already named. On further inquiry, for some respondents the GP was also deemed to be a good source of information.
To reflect latest developments in engineering, the respondents were asked about the possible usage of a technical device – such as a personal sensor system – to monitor ambient temperature in order to detect potentially dangerous situations. A large majority rejected the idea (17), mostly because of trusting one’s own senses was deemed sufficient (7).
The six respondents who did not receive any information wished to be informed by their GP (4), by radio (2), nursing services or television (2). In total, five respondents made their GP the first source of information, whereas four others did not think so at all. Reasons stated included the scarcity of visits (2) and difficulty in contacting their GP (1). However, the GP was regarded as trusted person.
Drinking more fluids was the most prominent piece of advice (12), followed by staying inside (4). It remains unclear whether only these pieces of advice have been communicated or whether only these have been perceived by the respondents.
Most respondents appeared (physically) very active or active, going along with a relatively high amount of social contacts and interaction. The health status revealed ten respondents with relevant underlying diseases and six respondents with strongly reduced mobility.
The thirteen carers interviewed were reponsible for eighteen of the older people interviewed. Nine of the carers had a professional (health service) background and were responsible for fourteen of the interviewees. In most cases they were (head) nurses or other personnel (e.g. social service of a center for older people) from nursing homes. All of them stated that they used preventive strategies during heatwaves for themselves. They displayed a high degree of awareness to the dangers of heat and a high degree of willingness to consult a doctor when the individual’s health status deteriorates.
However, some of the carers would like to do more for the older people, but this was being prevented by budget constraints. For example, the idea of administering more visits per day was appreciated; however, the time allotted for services of this kind was judged to be too scarce. In addition, many of the older people interviewed could only afford basic nursing services, for example a bath once a day. Thus, it was their budget preventing them from receiving more throrough assistance. There was some disagreement concerning the receipt of warnings and specific information during heatwaves. Some carers were not informed about heat warnings in their institutions, whereas others were well informed about the warnings by the German Weather Service, which are sent to nursing homes and similar institutions before and during heat waves. In general, head nurses showed a higher degree of information compared to other staff.
Discussion
Main findings of this study
The interviews allow insights into perceptions and views of older people and their carers.
One of the first findings is the relative concept of age presented by several respondents. Despite older people often being stated as a vulnerable group, in many cases the individual health status is perceived as a more important indicator. In addition, the control beliefs (“others are more vulnerable than me”) shown by many respondents are to be highlighted. These concepts and perceptions are similar to those found by other studies [16], [19].
A vast majority of the older people interviewed implemented preventative strategies and tried to protect themselves from the heat. However, most used a selection of a few wide-spread strategies, i.e. darkening the home, wearing light clothes, staying indoors and drinking more fluids. In general, the strategies used were similar to or exceeded the pieces of advice perceived from the media. As notable outlier, the interviewee stating not to change his daily routine claimed that his room was cool enough and he therefore did not feel the heat. In quantitative studies, the percentage of people implementing preventive strategies varied. However, in general, a majority of people seemed to change their daily routine during heatwaves [19], [33]. The most wide-spread strategies used by the interviewees were also very similar to those found before [17].
When comparing the degree of information and the measures reported with the recommendations for preventive actions, given e.g. by the World Health Organization [34], it can be stated that there is a potential for improvement. More strategies and personal measures are feasible and easy to implement, but they do not seem to be known or taken. Therefore, the dissemination of information on this topic is clearly an important point to consider, implicating the need for coordinated and sustained public health efforts.
Another finding is the controversial role of the GP. Some respondents regarded the GP as best source of information, with an important position of trust, while others were more critical. Previous studies partly found an even more critical attitude towards GPs [19]. However, the GP is generally seen as one of the key figures in promoting preventive behaviour [35], [36].
The carers in general were aware of the threat which heat can pose to older people. They use effective strategies themselves and stated that they would not hesitate to call a doctor if required. This underlines the general competencies of (professional) carers and partly contradicts previous results, which showed a lower risk awareness amongst carers [24]. On the other hand, the degree of information in regard to the receipt of heat warnings is partly insufficient (except for the head nurses). This ignorance can be dangerous for those dependent on professional carers.
Limitations of this study
Our study findings are limited due to the sampling method. The opportunistic sampling resulting from the small sample size and the selection of interviewees widely performed by nursing homes and other institutions was seen as the only way to get access to older people living in these homes.
Other limitations evolve from the execution of the study. A diversified sample of older people has been interviewed; however, general assumptions about the basic population can only very carefully be made. In addition, the nursing homes and other agencies involved in interviewee selection might not have chosen the most fragile people, for whom an interview could have been too stressful. However, people with dementia or older people living alone in badly ventilated homes seem to be at most high risk in heat waves. Therefore, particularly vulnerable sub-groups might be under-represented in this study.
Another limitation is due to courtesy bias when judging the respondents’ answers. It could not be controlled whether respondents would have answered differently if they had been interviewed in continuously hot weather.
Conclusions
Despite working with a relatively small study population, severall important aspects could be identified.
This study was able to confirm results in the field of interview-based explorations: relative self-concepts of ageing, seeing vulnerability preferably in others, concentration on a small selection of preventive measures, and the variety in channels used for receiving information.
In addition, deficits in knowledge among the professional carers could also be observed. Therefore, the degree of information of health-care personnel might have to be assessed; there may be room for improvement.
Besides these results confirming previous findings, there are some new findings.
First, most of the interviewees were socially relatively active. This might be due to the selection bias, but could also have important implications for designing and targeting information campaigns, which might be more effective when focused more broadly. When taking into account the relative self-concepts of age, there is also another point to consider: when information campaigns manage to successfully target younger people, these may also be more easily convinced to implement preventive measures when they grow old themselves.
Second, the two different aspects of the role of the GP were highlighted. On the one hand, the GP as an important partner and person of trust, and on the other hand, the GP as rarely valuable for short-term advice. This underlines the central role of GPs in the promotion of preventive actions and increasing risk perceptions, but also shows where the limits of a sole concentration on GPs might be.
With regards to the question of whether low degrees of perceived vulnerability represent a coping strategy, this study was not able to provide definite answers. However, there are indicators that will hopefully stimulate further research in this field.
It might be reasonable to consider quantitative data acquisition approaches using insights provided by this study to find out more about the amount of people sharing the views and perceptions captured in this study. In any case, the fostering of knowledge about heatwaves and the threats they pose can be seen as valuable step towards empowering this vulnerable subgroup. Older people do have to be seen as reasonable and autonomous individuals. Therefore, explaining the importance and implementation of preventive strategies, thus fostering understanding and compliance, has to be seen as an essential task.
Notes
Competing interests
The authors declare that they have no competing interests.
Acknowledgements
The authors would like to thank Vanessa Abrahamson, Canterbury Christchurch University, UK, for providing in-depth information about her interview studies in Norwich and London.
Special thanks go to the nursing homes and other institutions contacted, and above all, the respondents and their carers for their time and willingness which made this study possible.
Funding
This project was funded by means of the institute in charge.
References
- 1.Kosatsky T. The 2003 European heat waves. Euro Surveill. 2005;10(7):148–149. [PubMed] [Google Scholar]
- 2.Robine JM, Cheung SL, Le Roy S, Van Oyen H, Griffiths C, Michel JP, Herrmann FR. Death toll exceeded 70,000 in Europe during the summer of 2003. C R Biol. 2008;331(2):171–178. doi: 10.1016/j.crvi.2007.12.001. Available from: http://dx.doi.org/10.1016/j.crvi.2007.12.001. [DOI] [PubMed] [Google Scholar]
- 3.Beniston M. The 2003 heat wave in Europe: A shape of things to come? An analysis based on Swiss climatological data and model simulations. Geophys Res Lett. 2004;31:2022–2026. doi: 10.1029/2003GL018857. Available from: http://dx.doi.org/10.1029/2003GL018857. [DOI] [Google Scholar]
- 4.Luber G, McGeehin M. Climate change and extreme heat events. Am J Prev Med. 2008;35:429–435. doi: 10.1016/j.amepre.2008.08.021. Available from: http://dx.doi.org/10.1016/j.amepre.2008.08.021. [DOI] [PubMed] [Google Scholar]
- 5.Kjellström T, Butler AJ, Lucas RM, Bonita R. Public health impact of global heating due to climate change: potential effects on chronic noncommunicable diseases. Int J Public Health. 2010;55(2):97–103. doi: 10.1007/s00038-009-0090-2. Available from: http://dx.doi.org/10.1007/s00038-009-0090-2. [DOI] [PubMed] [Google Scholar]
- 6.O’Neill MS, Carter R, Kish JK, Gronlund CJ, White-Newsome JL, Manarolla X, Zanobetti A, Schwartz JD. Preventing heat-related morbidity and mortality: new approaches in a changing climate. Maturitas. 2009;64(2):98–103. doi: 10.1016/j.maturitas.2009.08.005. Available from: http://dx.doi.org/10.1016/j.maturitas.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bouchama A, Dehbi M, Mohamed G, Matthies F, Shoukri M, Menne B. Prognostic factors in heat wave related deaths: a meta-analysis. Arch Intern Med. 2007;167(20):2170–2176. doi: 10.1001/archinte.167.20.ira70009. Available from: http://dx.doi.org/10.1001/archinte.167.20.ira70009. [DOI] [PubMed] [Google Scholar]
- 8.Hoffmann B, Hertel S, Boes T, Weiland D, Jöckel KH. Increased causespecific mortality associated with 2003 heat wave in Essen, Germany. J Toxicol Environ Health A. 2008;71(11-12):759–765. doi: 10.1080/15287390801985539. Available from: http://dx.doi.org/10.1080/15287390801985539. [DOI] [PubMed] [Google Scholar]
- 9.Heudorf U, Meyer C. Gesundheitliche Auswirkungen extremer Hitze – am Beispiel der Hitzewelle und der Mortalität in Frankfurt am Main August 2003. Gesundheitswesen. 2005;67(5):369–374. doi: 10.1055/s-2004-813924. Available from: http://dx.doi.org/10.1055/s-2004-813924. [DOI] [PubMed] [Google Scholar]
- 10.Bittner MI, Stößel U. Heatwave-associated excess mortality in Freiburg and Rostock in 2003 and 2005 – methods and results. Gesundheitswesen. 2012 doi: 10.1055/s-0032-1331243. [DOI] [PubMed] [Google Scholar]
- 11.Jendritzky G, Koppe C. Die Auswirkungen der Hitzewellen 2003 auf die Mortalität in Baden-Württemberg (Zwischenbericht I des Projekts „Klimawandel – Auswirkungen, Risiken, Anpassung – KLARA“) In: Sozialministerium Baden-Württemberg., editor. Gesundheitliche Auswirkungen der Hitzewelle im August 2003. Stuttgart: 2004. pp. 5–18. [Google Scholar]
- 12.Grize L, Huss A, Thommen O, Schindler C, Braun-Fahrländer C. Heat wave 2003 and mortality in Switzerland. Swiss Med Wkly. 2005;135(13-14):200–205. doi: 10.4414/smw.2005.11009. [DOI] [PubMed] [Google Scholar]
- 13.Kalkstein LS, Sheridan SC, Kalkstein AJ. Heat/Health warning systems: Development, implementation, and intervention activities. In: Ebi KL, Burton I, McGregor GR, editors. Biometeorology for adaptation to climate variability and change. AK Houten, NL: Springer; 2009. pp. 33–48. Available from: http://dx.doi.org/10.1007/978-1-4020-8921-3_3. [DOI] [Google Scholar]
- 14.Heckenhahn M, Müller K. Kommunale Strategien der primären Prävention hitzebedingter Gesundheitsschäden. Präv Gesundheitsf. 2011;6(3):185–191. doi: 10.1007/s11553-010-0283-9. Available from: http://dx.doi.org/10.1007/s11553-010-0283-9. [DOI] [Google Scholar]
- 15.Michelozzi P, de Donato FK, Bargagli AM, D'Ippoliti D, De Sario M, Marino C, Schifano P, Cappai G, Leone M, Kirchmayer U, Ventura M, di Gennaro M, Leonardi M, Oleari F, De Martino A, Perucci CA. Surveillance of summer mortality and preparedness to reduce the health impact of heat waves in Italy. Int J Environ Res Public Health. 2010;7(5):2256–2273. doi: 10.3390/ijerph7052256. Available from: http://dx.doi.org/10.3390/ijerph7052256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sheridan SC. A survey of public perception and response to heat warnings across four North American cities: an evaluation of municipal effectiveness. Int J Biometeorol. 2007;52:3–15. doi: 10.1007/s00484-006-0052-9. Available from: http://dx.doi.org/10.1007/s00484-006-0052-9. [DOI] [PubMed] [Google Scholar]
- 17.Kalkstein AJ, Sheridan SC. The social impacts of the heat-health watch/warning system in Phoenix, Arizona: assessing the perceived risk and response of the public. Int J Biometeorol. 2007;52:43–55. doi: 10.1007/s00484-006-0073-4. Available from: http://dx.doi.org/10.1007/s00484-006-0073-4. [DOI] [PubMed] [Google Scholar]
- 18.Slovic P, Fischhoff B, Lichtenstein S. Facts and fears: understanding perceived risk. In: Schwing RC, Albers WA, editors. Societal risk assessment: how safe is safe enough? New York: Springer; 1980. pp. 181–214. [Google Scholar]
- 19.Abrahamson V, Wolf J, Lorenzoni I, Fenn B, Kovats S, Wilkinson P, Adger WN, Raine R. Perceptions of heatwave risks to health: interview-based study of older people in London and Norwich, UK. J Public Health (Oxf) 2009;31(1):119–126. doi: 10.1093/pubmed/fdn102. Available from: http://dx.doi.org/10.1093/pubmed/fdn102. [DOI] [PubMed] [Google Scholar]
- 20.Weinstein ND. Unrealistic optimism about susceptibility to health problems: conclusions from a community-wide sample. J Behav Med. 1987;10(5):481–500. doi: 10.1007/BF00846146. Available from: http://dx.doi.org/10.1007/BF00846146. [DOI] [PubMed] [Google Scholar]
- 21.Weinstein ND. Optimistic biases about personal risks. Science. 1989;246:1232–1233. doi: 10.1126/science.2686031. Available from: http://dx.doi.org/10.1126/science.2686031. [DOI] [PubMed] [Google Scholar]
- 22.Pinquart M, Sörensen S. Factors that promote and prevent preparation for future care needs: perceptions of older Canadian, German, and US women. Health Care Women Int. 2002;23(6-7):729–741. doi: 10.1080/07399330290107467. Available from: http://dx.doi.org/10.1080/07399330290107467. [DOI] [PubMed] [Google Scholar]
- 23.Kosatsky T, Dufresne J, Richard L, Renouf A, Giannetti N, Bourbeau J, Julien M, Braidy J, Sauve C. Heat awareness and response among Montreal residents with chronic cardiac and pulmonary disease. Can J Public Health. 2009;100(3):237–240. doi: 10.1007/BF03405548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Abrahamson V, Raine R. Health and social care responses to the Department of Health Heatwave Plan. J Public Health (Oxf) 2009;31(4):478–489. doi: 10.1093/pubmed/fdp059. Available from: http://dx.doi.org/10.1093/pubmed/fdp059. [DOI] [PubMed] [Google Scholar]
- 25.Augustin J, Paesel HK, Mücke HG, Grams H. Anpassung an die gesundheitlichen Folgen des Klimawandels – Untersuchung eines Hitzewarnsystems am Beispiel Niedersachsen. Präv Gesundheitsf. 2011;6(3):179–184. doi: 10.1007/s11553-011-0294-1. Available from: http://dx.doi.org/10.1007/s11553-011-0294-1. [DOI] [Google Scholar]
- 26.Wolf J, Adger WN, Lorenzoni I. Talk: Barriers to adaptation: Vulnerability of the elderly to the impacts of heat waves. IHDP Open meeting 2009, 7th International Conference on the Human Dimensions of Global Environmental Change; 2009 Apr 26-30; Bonn, Germany. 2009. [Google Scholar]
- 27.Pope C, Mays N. Reaching the parts other methods cannot reach: an introduction to qualitative methods in health and health services research. BMJ. 1995;311(6996):42–45. doi: 10.1136/bmj.311.6996.42. Available from: http://dx.doi.org/10.1136/bmj.311.6996.42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ritchie J, Lewis J, editors. Qualitative Research Practice. London: Sage Publications; 2003. [Google Scholar]
- 29.Ritchie J, Spencer L. Qualitative data analysis for applied policy research. In: Bryman A, Burgess RG, editors. Analyzing qualitative data. London, UK: Routledge; 1994. pp. 173–194. [Google Scholar]
- 30.Srivastava A, Thomson SB. Framework Analysis: A Qualitative Methodology for Applied Policy Research. Research Note. JOAAG. 2009;4(2) [Google Scholar]
- 31.Pope C, Ziebland S, Mays N. Qualitative research in health care. Analysing qualitative data. BMJ. 2000;320(7227):114–116. doi: 10.1136/bmj.320.7227.114. Available from: http://dx.doi.org/10.1136/bmj.320.7227.114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mays N, Pope C. Qualitative research in health care. Assessing quality in qualitative research. BMJ. 2000;320(7226):50–52. doi: 10.1136/bmj.320.7226.50. Available from: http://dx.doi.org/10.1136/bmj.320.7226.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Semenza JC, Wilson DJ, Parra J, Bontempo BD, Hart M, Sailor DJ, George LA. Public perception and behavior change in relationship to hot weather and air pollution. Environ Res. 2008;107(3):401–411. doi: 10.1016/j.envres.2008.03.005. Available from: http://dx.doi.org/10.1016/j.envres.2008.03.005. [DOI] [PubMed] [Google Scholar]
- 34.Matthies F, Nurse J, Menne B, editors. World Health Organization: Public health advice on preventing health effects of heat. Copenhagen, Denmark: WHO Regional Office for Europe; 2011. [accessed on 10 September 2012]. Available from: http://www.euro.who.int/__data/assets/pdf_file/0007/147265/Heat_information_sheet.pdf. [Google Scholar]
- 35.Brauerhoch FO, Ewen C, Sinemus K. Risikokommunikation – eine Herausforderung für öffentliche Institutionen. Umweltmedizinischer Informationsdienst (UMID) 2008;1:16–20. Available from: http://www.umweltbundesamt.de/umid/archiv/umid0108.pdf. [Google Scholar]
- 36.Forastiere F. Climate change and health: a challenge for epidemiology and public health. Int J Public Health. 2010;55:83–84. doi: 10.1007/s00038-009-0096-9. Available from: http://dx.doi.org/10.1007/s00038-009-0096-9. [DOI] [PubMed] [Google Scholar]