Abstract
The influence of ethnicity on vaccination uptake in urban slums in Kenya is largely unknown. We examined the disparities in timeliness and coverage of measles vaccination associated with ethnicity in the Korogocho slum of Nairobi. The study used data from the Maternal and Child Health component of the Urbanization, Poverty and Health Dynamics Research Programme undertaken in the Korogocho and Viwandani slums by the African Population and Health Research Center from 2006 to 2010. Vaccination information was collected from children recruited into the study during the first year after birth, and a sub-sample of 2,317 who had been followed throughout the period and had the required information on measles vaccination was included in the analysis. Cox regression analysis was used to determine the association of ethnicity with delayed measles in the slum. We found significant disparities in the coverage and timeliness of measles vaccination between the ethnic groups in Korogocho. The Luhya and minor ethnic groups in the slum were more likely than the Kikuyu to have delayed measles vaccination. Ethnic groups with a high proportion of children with delayed measles vaccination need to be targeted to address cultural barriers to vaccination as part of efforts to improve coverage in urban slums.
Keywords: Ethnicity, vaccination delay, measles, slum, Kenya
Introduction
The low coverage of measles vaccination among urban poor is evident in the literature and continues to be a major public health concern in many countries [1–2]. Addressing this problem requires a better understanding of the determinants of vaccination uptake in slums and other informal settlements where the urban poor reside. High vaccination coverage may mask the prevalence of late or delayed vaccination which is a risk factor for childhood illness and has been associated with non-specific adverse effects and reduced survival [3–5].
Studies on the timeliness of vaccinations among urban poor are scarce, and the complexity of these informal settlements heightens the challenge of addressing missed or late vaccinations. National studies have revealed significant differences in health-seeking behaviour among the ethnic groups in Kenya [6], and the presence of these diverse ethnic populations in slums suggests the possibility of similar variations in utilization of health services. A previous study on vaccination in Korogocho showed that coverage for measles was below the national average and highlights the ethnic differences in the likelihood of up-to-date vaccination [2]. In this study, we examine the relationship between ethnicity and the timeliness of measles vaccination uptake in a Nairobi slum.
Methods
Study area and population
The study was conducted in the Korogocho slum of Nairobi, which is part of a surveillance system known as the Nairobi Urban Health and Demographic Surveillance System (NUHDSS) run by the African Population and Health Research Centre (APHRC). Korogocho slum, which is made up of seven villages, is densely populated and suffers from high levels of unemployment, poverty, poor sanitation and morbidity especially among children under five years of age [7]. Due to the informal nature of the settlement, Korogocho has no formal public health facility to serve the population. Residents rely on private-for-profit and private-not-for-profit health facilities, but the quality of services offered at these facilities varies considerably.
Study Sample and Design
Data was obtained as part of the Maternal and Child Health project within the Urbanization, Poverty and Health Dynamics research programme undertaken in the Korogocho and Viwandani slums from 2006 to 2010. All women from the NUHDSS area who gave birth from September 2006 to December 2010 were enrolled in the project and administered a questionnaire which asked about the vaccination history of their children. For the purpose of this study, we used data on 2,317 children aged 9–59 months who had been followed throughout the period and had the required information on measles vaccination. The date of measles vaccination, which is scheduled for administration nine months after birth, was obtained from vaccination cards. Data on the socio-demographic characteristics of the mother and household were also collected as part of the routine NUHDSS census rounds.
Statistical Analysis
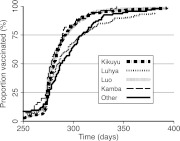
The two outcomes assessed in the descriptive analysis included measles vaccination coverage and delayed measles vaccination, which was defined as a measles vaccination conducted later than 10 months after birth. Analysis was conducted only for children aged 9–59 months using data on their measles vaccination status. The wealth status was computed by dividing the monthly household expenditure by the equivalent household size, taking a child to be equivalent to half an adult. Five covariates were included in the analysis: sex of child, maternal education (none, primary, and secondary or higher), household wealth status based on expenditure (poorest, poor, not poor), ethnicity (Kikuyu, Luhya, Luo, Kamba and Other), and village of residence (Grogan A, Grogan B, Gitathuru, Nyayo/Kisumu Ndogo, Korogocho A, Korogocho B and Highridge). Descriptive analysis was used to show the characteristics of the participants in the study in relation to measles vaccination uptake and delay. A Cox regression model was fitted with all covariates and used to identify the risk factors associated with on-time measles vaccination in the slum. The differences in timeliness of measles vaccination across the different ethnic groups are shown using Kaplan-Meier curves. The Kaplan-Meier method, which describes time-to-event data, is increasingly applied to assessments of age-appropriate vaccinations [8].
Ethical considerations
The Urbanization, Poverty and Health Dynamics research programme was approved by the Ethical Review Board of the Kenya Medical Research Institute (KEMRI). Informed consent was obtained from all respondents in the Maternal and Child Health project prior to data collection.
Results
The results of the descriptive and Cox regression analysis are shown in Table 1. A total of 2,317 children (51% male and 49% female) were included in the analysis. Coverage of measles vaccine was less than 40% among males and females. The proportion of children with delayed measles vaccination ranged from 20% in females to 24% in males, although this difference was not statistically significant. The measles vaccine coverage was slightly higher among children of mothers with secondary or more education, but there was no difference in the proportion that had delayed vaccination. The wealth status of the household was not a significant determinant of delayed measles vaccination in children. However, significant differences were evident in the proportion of children with delayed vaccination among the difference ethnic groups. Children of the Kikuyu ethnic group had the highest measles coverage and the lowest level of delayed measles vaccination. Children from the Luhya and minor ethnic minorities meanwhile had the highest levels of delayed measles vaccination and lower likelihood of on-time vaccination compared to the Kikuyu ethnic group. Table 2 shows the differences among the ethnic groups in mean age and median delay at the time of measles vaccination. The results reveal a median delay of more than two weeks in the Luhya and smaller ethnic groups. The Kaplan-Meier curves show that beyond the 50th percentile, measles vaccination occurred increasingly later in these ethnic groups compared to the other ethnic groups (Fig. 1). There was no significant relationship between delayed measles vaccination and village of residence within the slum.
Table 1.
Factors associated with delay in measles vaccination in Korogocho
| Coverage |
Delay |
RRR | (95% CI) | P value | |||
|---|---|---|---|---|---|---|---|
| (%) | (n/N) | (%) | (n/N) | ||||
| Sex of Child | |||||||
| Male | 38.0 | (447/1176) | 24.2 | (108/447) | 1.00 | ||
| Female | 36.5 | (417/1141) | 20.1 | (84/417) | 1.04 | (0.91, 1.20) | 0.55 |
| Maternal Education | |||||||
| No education | 36.3 | (306/842) | 22.2 | (68/306) | 1.00 | ||
| Primary | 40.0 | (392/979) | 21.2 | (83/392) | 0.96 | (0.82, 1.12) | 0.61 |
| Secondary or higher | 47.0 | (140/298) | 22.9 | (32/140) | 0.98 | (0.81, 1.19) | 0.84 |
| Household Wealth Status | |||||||
| Poorest | 40.7 | (384/943) | 23.7 | (91/384) | 1.00 | ||
| Poor | 39.5 | (269/681) | 21.9 | (59/269) | 0.98 | (0.84, 1.13) | 0.77 |
| Not poor | 36.4 | (153/420) | 19.6 | (30/153) | 0.92 | (0.75, 1.13) | 0.42 |
| Ethnicity | |||||||
| Kikuyu | 47.9 | (302/631) | 16.2 | (49/302) | 1.00 | ||
| Luhya | 39.2 | (173/441) | 31.8 | (55/173) | 0.65 | (0.53, 0.80) | 0.00 |
| Luo | 34.7 | (215/620) | 17.7 | (38/215) | 0.97 | (0.78, 1.19) | 0.76 |
| Kamba | 41.0 | (55/134) | 16.4 | (9/55) | 1.12 | (0.85, 1.49) | 0.42 |
| Other | 31.7 | (93/293) | 34.4 | (32/93) | 0.73 | (0.58, 0.91) | 0.01 |
| Village | |||||||
| Grogan A | 39.8 | (66/166) | 28.8 | (19/66) | 1.00 | ||
| Grogan B | 44.2 | (61/138) | 16.4 | (10/61) | 1.18 | (0.83, 1.69) | 0.35 |
| Gitathuru C | 33.0 | (97/294) | 20.6 | (20/97) | 1.20 | (0.87, 1.65) | 0.27 |
| Nyayo/Kisumu Ndogo | 41.9 | (224/535) | 18.3 | (41/224) | 1.34 | (1.01, 1.79) | 0.04 |
| Korogocho A | 40.1 | (109/272) | 20.2 | (22/109) | 1.23 | (0.90, 1.69) | 0.20 |
| Korogocho B | 38.1 | (120/315) | 23.3 | (28/120) | 1.21 | (0.89, 1.63) | 0.22 |
| Highridge | 31.3 | (187/597) | 27.8 | (52/187) | 1.09 | (0.82, 1.45) | 0.54 |
RRR: Relative risk ratio refers to the likelihood of on-time vaccination for measles
Table 2.
Mean age and median delay at time of measles vaccination among ethnic groups in Korogocho
| n | Mean age (Days) | SEM | Median delay (Days) | (95% CI) | |
|---|---|---|---|---|---|
| Kikuyu | 302 | 286 | 1.8 | 10 | 9, 13 |
| Luhya | 173 | 301 | 4.7 | 15 | 11, 19 |
| Luo | 215 | 280 | 3.2 | 9 | 7, 11 |
| Kamba | 55 | 279 | 3.9 | 8 | 4, 14 |
| Other | 93 | 293 | 4.5 | 17 | 13, 26 |
SEM: Standard error of mean
Fig. 1.
Timing of measles vaccination uptake among the ethnic groups in Korogocho.
Discussion
This study reports the relationship between ethnic origin and timeliness of measles vaccination in the Korogocho slum of Nairobi. Measles vaccine coverage was about 40% in the slum, highlighting the risk of measles infection faced by infants in a slum with a population of about 200,000. In addition to the challenge of increasing coverage in the informal settlements of Nairobi, there is need to reduce the proportion that receive measles vaccine many weeks after the recommended age for vaccination. In this study a little less than a fourth of all measles vaccinations were received later than 10 months after birth.
Delays in receipt of vaccinations are usually associated with service-related factors such as health worker perceptions and attitudes, vaccine stock-outs and policies regarding opened multi-dose vials [9–10]. However, client-associated factors are also commonly linked to late vaccinations, and these may be associated with the individual or community [9]. In this study, we found that the main factor associated with delayed measles vaccination among children in the slum was their ethnic origin. No association was observed between late vaccination and maternal education, household wealth or village of residence. This suggests that unknown cultural factors and practices may directly influence health-seeking behaviour related to measles vaccination. Our previous study on vaccination in Nairobi slums indicated that children of the Kikuyu ethnic group were more likely than the Luhya and minor ethnic groups to be fully vaccinated [2]. This pattern is observed in the present study as delayed measles vaccination and suggests a higher risk for mortality due to measles among these two groups compared to the Kikuyu. The influence of ethnicity on immunization has been attributed to the difficulty of reaching and engaging with ethnically distinct communities for immunization uptake, and may be related to high levels of mistrust and suspicion between ethnic groups resulting in lower uptake by some groups [11].
The absence of a clear definition of what constitutes a delayed or late measles vaccination posed an operational challenge. We used an adapted definition of four weeks after the 9th month from birth based on a previous study [12], which allows an extension of the vaccination period and compensates for short delays due to supply factors. Despite the extension of the period of on-time vaccination to four weeks, the proportion of children that were classified as having delayed vaccination was about 20%. Another limitation of the study is the reliance on data only from the children for whom information on the date of measles vaccination was available. A significant proportion of children in these slum do not have vaccination cards [2], and excluding these children therefore reduces the statistical power of the study. However, the precise date of vaccination is essential for timeliness analysis, and this is not available or reliable when based on maternal recall.
In conclusion, ethnicity in the Korogocho slum of Nairobi is significantly related to the likelihood of delayed measles vaccination. Further research is required to understand the socio-cultural and contextual factors that account for these disparities in vaccination uptake. Ethnic groups with a high proportion of children with delayed measles vaccination need to be targeted with initiatives to address barriers to vaccination as part of efforts to improve coverage in urban slums.
Acknowledgement
This study is part of the Urbanization, Poverty and Health Dynamics research programme which was funded by the Wellcome Trust (GR 07830 M).
References
- 1.Bhagyalaxmi A, Kedia G, Rawal VS. Study of incidence of measles and vaccination coverage in Ahmedabad urban slums. Indian J Public Health 2007; 51: 52–53 [PubMed] [Google Scholar]
- 2.Mutua MK, Kimani-Murage E, Ettarh RR. Childhood vaccination in informal urban settlements in Nairobi, Kenya: who gets vaccinated? BMC Public Health 2011; 11: 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mhatre SL, Schryer-Roy AM. The fallacy of coverage: uncovering disparities to improve immunization rates through evidence. Results from the Canadian International Immunization Initiative Phase 2—Operational Research Grants. BMC Int Health Hum Rights 2009; 9 Suppl 1: S1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Aaby P, Bhuiya A, Nahar L, Knudsen K, de Francisco A, Strang M. The survival benefit of measles immunization may not be explained entirely by the prevention of measles disease: a community study from rural Bangladesh. Int J Epidemiol 2003; 32: 106–116 [DOI] [PubMed] [Google Scholar]
- 5.Clark A, Sanderson C. Timing of children’s vaccinations in 45 low-income and middle-income countries: an analysis of survey data. Lancet 2009; 373: 1543–1549 [DOI] [PubMed] [Google Scholar]
- 6.Kenya National Bureau of Statistics (KNBS), ICF Macro. Kenya Demographic and Health Survey 2008-09: Calverton, Maryland: KNBS and ICF Macro; 2009.
- 7.Emina J, Beguy D, Zulu E, Ezeh AC, Muindi K, Elungáta P, Otsola JK, Yé Y. Monitoring of Health and Demographic Outcomes in Poor Urban Settlements: Evidence from the Nairobi Urban Health and Demographic Surveillance System. J Urban Health 2011; 88 Suppl 2: 200–218 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Dayan GH, Shaw KM, Baughman AL, Orellana LC, Forlenza R, Ellis A, Chaui J, Kaplan S, Strebel P. Assessment of delay in age-appropriate vaccination using survival analysis. Am J Epidemiol 2006; 163: 561–570 [DOI] [PubMed] [Google Scholar]
- 9.IMMUNIZATION basics. Epidemiology of the Unimmunized Child: Arlington, VA: IMMUNIZATION basics; 2009.
- 10.Borus PK. Missed opportunities and inappropriately given vaccines reduce immunisation coverage in facilities that serve slum areas of Nairobi. East Afr Med J 2004; 81: 124–129 [DOI] [PubMed] [Google Scholar]
- 11.Platas MR. Africa’s Health Tragedy? Ethnic Diversity and Health Outcomes. Winter Working Group on African Political Economy. Stanford University; 2010.
- 12.Yadav K, Srivastava R, Kumar R, Chinnakal P, Rai SK, Krishnan A. Significant Vaccination Delay can Occur Even in a Community with Very High Vaccination Coverage: Evidence from Ballabgarh, India. J Trop Pediatr 2012; 58(2): 133–138 [DOI] [PubMed] [Google Scholar]