Abstract
Background
The epidemiology of tuberculosis (TB) has been assessed based on the data of the analysis of TB patients notified to the surveillance system in Korea. However, the national status of TB is not validated through this surveillance system. The objective is to determine the epidemiology of TB and to understand the accurate status of TB patients treated in private institutions.
Methods
Medical records of 53,579 patients who had been diagnosed with TB in 2008 were analyzed.
Results
Among 53,579 patients, the number of sputum smear positive cases was 15,639(29.2%) and the number of new cases was 39,191 (73.1%). The drug resistance rate of new cases was 5.3%, while the rate stood at 13.3% for TB patients with treatment history. The number of multi-drug resistant TB (MDR-TB) patients was 2,472 (4.6%), which consists of 2.9% of new cases and 9.3% of TB patients with prior treatment history. The number of extensively drug-resistant TB patients was 749 (1.4%), consisting of 1.1% of new cases and 2.2% of TB patients with prior treatment history. In terms of treatment outcomes, 66.4% of all TB patients, 70.5% of new cases, 64.4% of relapse cases, and 46.8% of MDR-TB cases were cured or completed. It was inferred that in 2008, the total number of TB patients reached 70,767, 145.6 per 100,000 people (95% confidence interval, 145.5~145.7).
Conclusion
We conclude that the medical records review of the Health Insurance Review and Assessment Service (HIRA) data can be very effective in promoting the understanding of the current status of TB in private institutions.
Keywords: Tuberculosis; Disease Notification; Epidemiology; Tuberculosis, Multidrug-Resistant; Medical Records; Data Collection
Introduction
In Korea, the national tuberculosis (TB) prevalence survey had been conducted 7 times between 1965 and 1995, to investigate the TB infection rate, pulmonary TB prevalence and drug-resistant rate. However, as prevalence rate has shown a gradual decrease, the survey faced limits in securing sufficient number of samples and other problems such as high cost, low participation rate and difficulty in accurate prediction of incidence rate. To address these issues, the TB Surveillance System was introduced in June 2000 under the TB Prevention Act, which facilitated TB notification via internet. Through the analysis of notified TB patient's data, the trend of tuberculosis patients and the effect of the National TB Management System have been assessed. For the successful implementation of this surveillance system, cooperation with doctors is crucial to guarantee all patients are diagnosed by standardized measures and notified to the system.
On the other hand, all TB patients who are treated in public health centers are notified to the Korea TB Information Management System (TBnet). However, a 2006 survey of clinicians regarding patients treated in private institutions demonstrates only 67.6% of these patients were notified to Korea Centers for Disease Control and Prevention (KCDC)1. Moreover, according to TB patients data notified to the TBnet, the rate of TB patients treated in private institutions went up from 53% in 2001, to 85% in 20102. These figures well represent the limits of this surveillance system, in which TB patient's current status including the number and features of patients cannot be accurately monitored when private institutions neglect notification responsibility.
This study aims to define the epidemiology of TB and understand accurate status of the TB patients treated in private institutions, by analyzing investigation results of medical records which requested TB patient treatment expense to the The Health Insurance Review and Assessment Service (HIRA).
Materials and Methods
1. Subjects
This study comprehensively analyzes TB patient's medical records review jointly conducted by the KCDC and the Korean Medical Record Association from May to December 2010. Seventy-six thousand three hundred fifteen cases in 2008 from 4,049 private institutions were analyzed. To exclude non-TB patients, 3 criteria were applied: 1) notified with TB code (ICD-10: A15~19, U88.0~88.1); 2) treated with 2 or more anti-TB drugs; and 3) requested medical expenses more than 2 times to the HIRA. As several private institutions declined to participate in the survey, the response rate stood at 83.0%, making 63,359 patients treated in 3,461 private institutions subject to study. After excluding overlapping patients, who received treatments from two or more medical institutions, the actual number of patients in the study was 55,136. Among these patients, nontuberculous mycobacteria infected patients and non-TB patients were also excluded, and 53,579 TB patients were set as final analysis subjects.
2. Methods
To conduct a standardized survey on the medical records investigation, guidelines regarding the check list of the TB medical records and the implementation of investigation were developed, and medical records were reviewed by medical record administrators, who received education on the TB survey methods. Medical record administrators identified the administrative errors such as input and diagnosis errors and verified whether the subjects were TB patients or not, and recorded data on web-based data input program.
Ethical clearance was not required since this study is for the purpose of public health practice, to control communicable diseases by monitoring TB cases in Korea on a regular basis under TB prevention laws.
The study covers the following items: sex, age, classification of the medical institutions, TB treatment history, types of resistant drugs, primary test results (chest X-ray and other imaging studies such as computed tomography and magnetic resonance imaging scans, sputum smear and culture, biopsy and others), TB code, comorbid diseases (silicosis, peptic ulcer, cancer, chronic renal failure, diabetes, alcoholism, human immunodeficiency virus [HIV] infection), treatment outcomes, drug regimen, location of medical institutions. In terms of TB treatment history, the patients who had taken anti-TB drugs prior to their treatment at medical institutions were classified as 'patients with treatment history.' Comorbid diseases could be identified anytime during TB treatment, and the drug regimen refers to as an initially prescribed drug. However in case of drug-resistant TB, additional drugs prescribed after the detection of drug resistance are also included in drug regimen.
Classification of patients consists of the following categories: new, relapse, treatment after failure, treatment after default, transfer in, chronic and other. 'New' refers to patients who have never been treated before or are being treated for less than one month. 'Relapse' refers to patients who had completed their treatment but developed TB again. 'Treatment after failure' refers to patients whose treatment had failed in the past but resumed, while 'treatment after default' refers to patients with treatment history of one month or more, along with a cessation period of two months or more. 'Transfer in' refers to patients who transferred to other medical clinics within two months, with aggregate treatment period of one month or more. 'Chronic' refers to patients who failed to resume treatment but are in the state of smear-positive, and 'other' refers to patients not classified as any of the above categories3.
Treatment outcomes are classified as follows: cured, completed, failed, defaulted, transfer out, died from TB, died from other causes, diagnosis changed, and other. This classification follows the World Health Organization (WHO) guideline4, with the exception of 'diagnosis changed' and 'other.' 'Diagnosis changed' refers to patients who are diagnosed with other diseases during TB treatment. 'Other' refers to patients who do not fit into any of the above criteria, such as patients still receiving treatment or patients who were diagnosed with TB but unknown about their treatment status3.
Multi-drug resistant TB (MDR-TB) is defined as tuberculosis that is resistant to isoniazid and rifampicin. Extensively drug-resistant TB (XDR-TB) is defined as tuberculosis that is resistant to any fluoroquinolone, and resistant to at least one of the three injectable second-line drugs (amikacin, capreomycin, kanamycin), in addition to MDR-TB.
SAS version 9.2 (SAS institute Inc., Cary, NC, USA) was used to analyze data and Chi square test was conducted.
Results
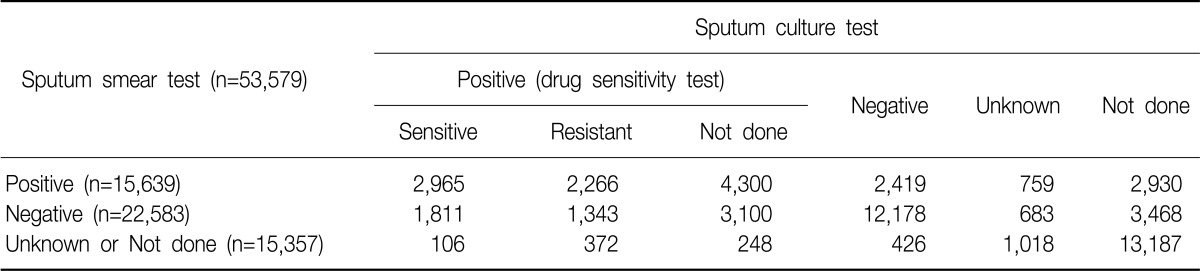
Among 53,579 TB patients, 22,619 (42.2%) were bacteriologically confirmed pulmonary TB patients, and 15,639 (29.2%) were sputum smear-positive pulmonary TB patients. 40,392 (75.4%) had sputum smear and culture examination (Table 1).
Table 1.
TB cases through medical records review by diagnosis test
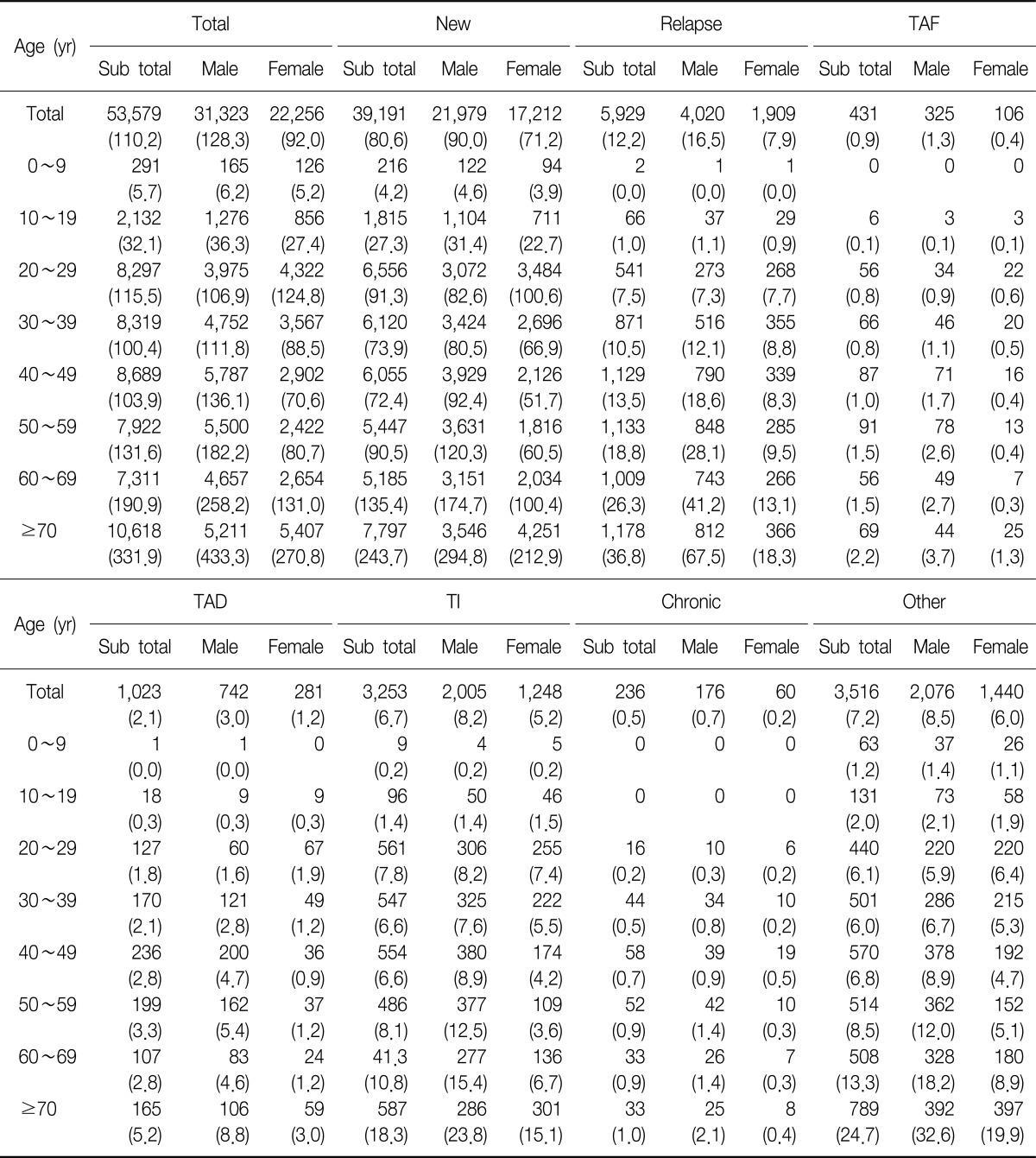
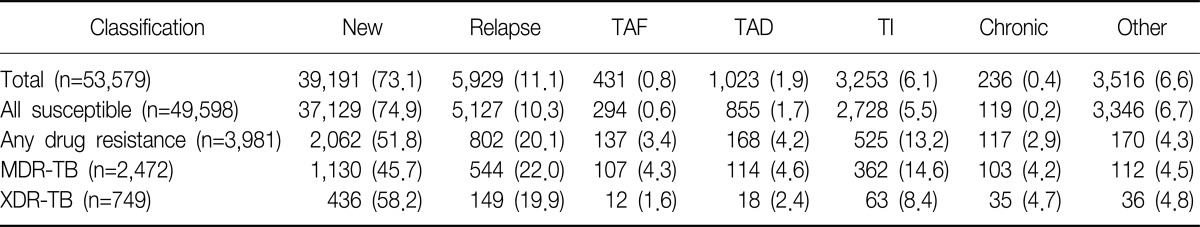
In terms of sex distribution, there were 1.4 times more male patients than female patients. However in twenties, there were more female patients than male patients. In terms of age distribution, the largest age group was seventies and over, while the smallest age group was under the age of ten. Classification of patients-wise, 39,191 (73.1%) were 'new,' accounting for the majority of all classifications, 5,929 (11.1%) were 'relapse,' 431 (0.8%) were 'treatment after failure,' 1,023 (1.9%) were 'treatment after default,' 3,253 (6.1%) were 'transfer in,' 236 (0.4%) were 'chronic,' and 3,516 (6.6%) were 'other.' In terms of age, the proportion of new cases is the highest in teens, but decreases to reach the lowest level in fifties (Table 2).
Table 2.
TB cases through medical records review by types of patient, sex and age group (n=53,579)
Values are presented as number of cases (case per 100,000 population).
TAF: treatment after failure; TAD: treatment after default; TI: transfer in.
According to classification of medical institutions, 37,951 (70.8%) were treated in general hospitals, 6,841 (12.8%) in hospitals, 8,742 (16.3%) in medical clinics and 45 (0.1%) in other facilities.
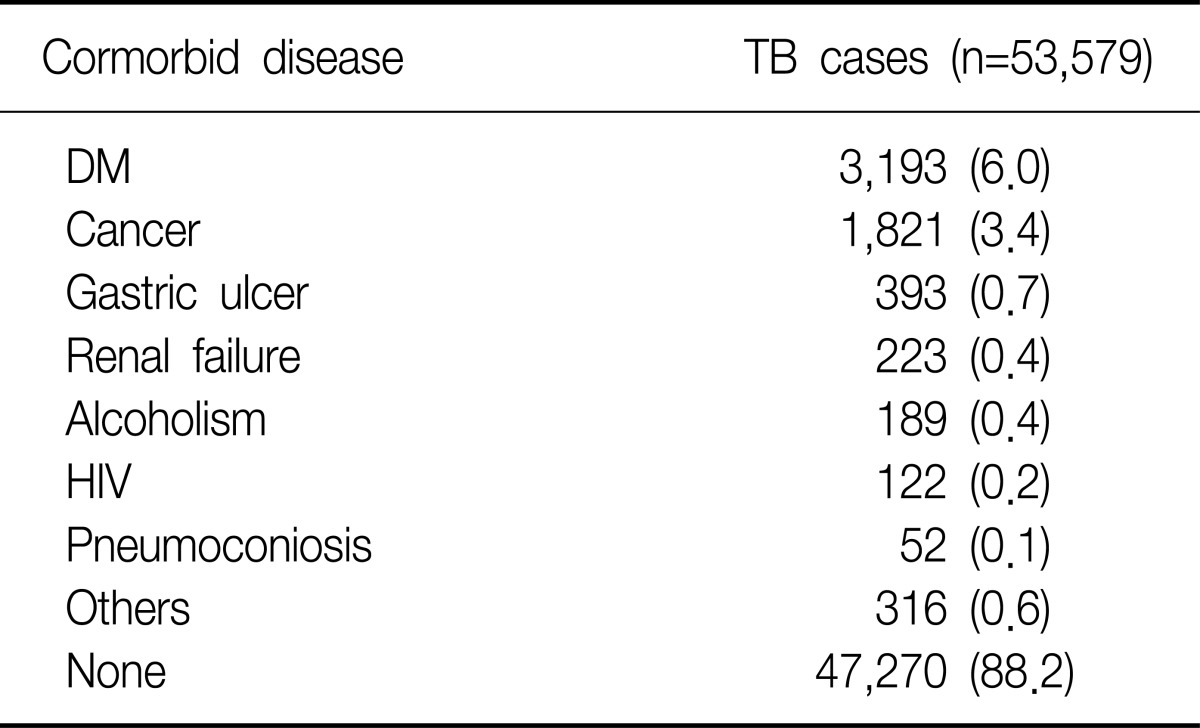
The study showed among all TB patients, 6,657 (12.4%) suffered from comorbid diseases, namely 3,193 (6.0%) from diabetes, 1,821 (3.4%) from cancer, 393 (0.7%) from peptic ulcer, 271 (0.5%) from cancer with diabetes, and 223 (0.4%) from renal failure (Table 3).
Table 3.
TB cases through medical records review by comorbid diseases
Values are presented as number (%).
TB: tuberculosis; DM: diabetes mellitus; HIV: human immunodeficiency virus.
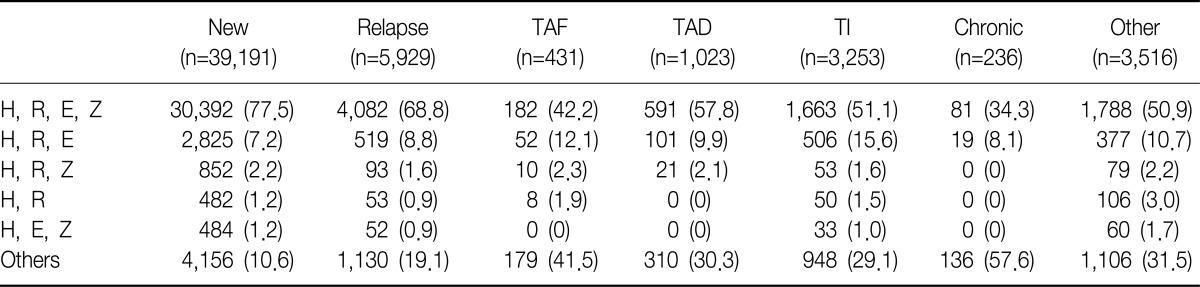
Among the 7 major primary drug regimens, 4-drug regimen (isoniazid, rifampicin, ethambutol, pyrazinamide) accounted for the majority of new cases, recording 77.5% (30,392 patients), followed by 3-drug regimen (isoniazid, rifampicin, ethambutol) which stood at 7.2% (2,825 patients) (Table 4).
Table 4.
Drug regimens through medical records review by classification types (n=53,579)
Values are presented as number (%).
TAF: treatment after failure; TAD: treatment after default; TI: transfer in; H: isoniazid; R: rifampicin; E: ethambutol; Z: pyrazinamide.
Three thousand nine hundred eighty one TB patients (7.4%) were resistant to one or more anti-TB drugs, while 2,062 patients (5.3%) of new cases (39,191 patients) and 1,919 patients (13.3%) of all TB patients with treatment history (14,388 patients) were resistant to one or more anti-TB drugs (Table 5).
Table 5.
TB cases through medical records review by classification of patients and drug resistant TB
Values are presented as number (%).
TB: tuberculosis; TAF: treatment after failure; TAD: treatment after default; TI: transfer in; MDR-TB: multi-drug resistant TB; XDR-TB: extensively drug-resistant TB.
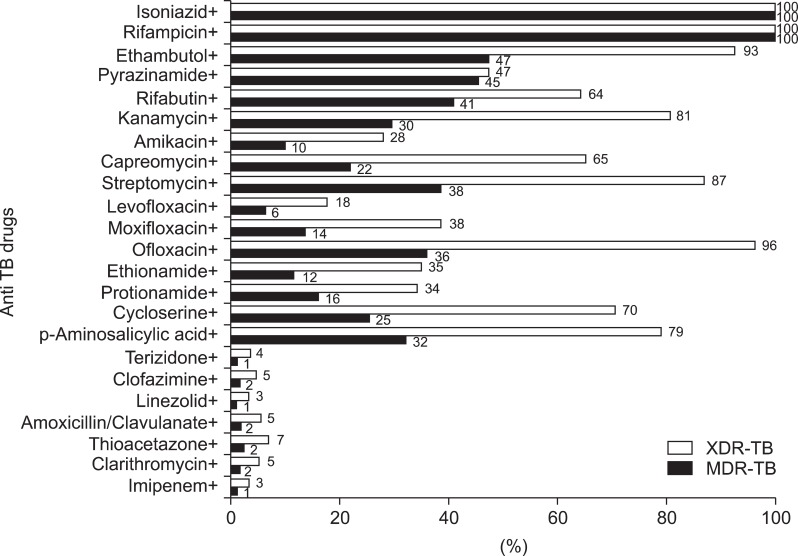
In terms of drug-resistant TB, the number of MDR-TB patients was 2,472 (4.6%), accounting for 62.1% of all drug-resistant TB patients. Among them, 1,130 patients (2.9%) were new cases (39,191 patients) and 1,342 patients (9.3%) were TB patients with prior treatment history (14,388 patients) (Table 5). In terms of distribution of resistance to first-line TB drugs, among 2,472 MDR-TB patients, 47% were resistant to ethambutol, 45% to pyrazinamide, 41% to rifabutin. In terms of distribution of resistance to second-line injectable drugs, 38% to streptomycin, 30% to kanamycin, 22% to capreomycin, 10% to amikacin. In terms of distribution of resistance to fluoroquinolones, 36% to ofloxacin, 14% to moxifloxacin, 6% to levofloxacin (Figure 1).
Figure 1.
Rate of resistance to anti TB drugs in MDR-TB and XDR-TB patient. TB: tuberculosis; MDR-TB: multi-drug resistant TB; XDR-TB: extensively drug-resistant TB.
The number of XDR-TB patients was 749 (1.4%), accounting for 18.8% of all drug-resistant TB patients. Among these patients, 436 were new cases of XDR-TB without prior treatment history, accounting for 1.1% of total new cases, and 313 patients with prior treatment history accounted for 2.2% of total patients (Table 5). In terms of distribution of resistance to first-line TB drugs, among 749 XDR-TB patients, 93% were resistant to ethambutol, 64% to rifabutin, 47% to pyrazinamide. In terms of distribution of resistance to second-line injectable drugs, 87% were resistant to streptomycin, 81% to kanamycin, 65% to capreomycin, and 28% to amikacin. In terms of distribution of resistance to fluoroquinolones, 96% were resistant to ofloxacin, 38% to moxifloxacin, 18% to levofloxacin (Figure 1).
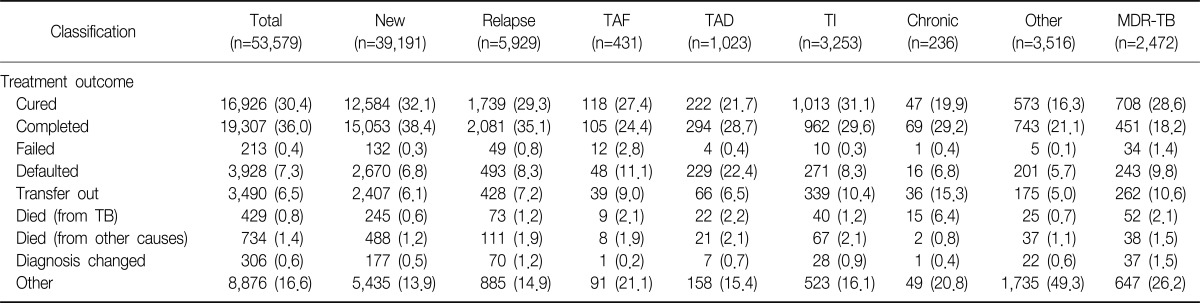
In terms of treatment outcomes, 66.4% of all TB patients, 70.5% of new cases, 64.4% of relapse cases, and 46.8% of MDR-TB cases were cured or completed. 'Other' 8,876 cases (16.6%) consist of patients still receiving treatment or patients who were diagnosed with TB but unknown about their treatment status (Table 6).
Table 6.
TB cases through medical records review by treatment outcome (n=53,579)
Values are presented as number (%).
TB: tuberculosis; TAF: treatment after failure; TAD: treatment after default; TI: transfer in; MDR-TB: multi-drug resistant TB.
Based on this study, we could derive TB prevalence rate in Korea. 9,791 TB patients were notified to public health centers and recorded on the Annual Report on the Notified Tuberculosis Patients in Korea. After excluding 1,463 overlapping patients who received treatments from both public health centers and private institutions, 52,116 patients were treated in private institutions in 2008. If we convert total coverage of this study into 100% (which in fact stands at 83%), total estimated number of patients subject to treatment will be 60,976. Accordingly, when we combine all patients treated in both public and private health centers, 70,767, or 145.6 in every 100,000 Koreans (95% confidence interval, 145.5~145.7) were treated for TB in 2008.
Discussion
According to the distribution of sex and age group, the age distribution of the TB patients treated in private institutions follows a bimodal distribution, which is similar to the TB patients' pattern in developing countries, with the first peak in twenties and the second peak in seventies. This distribution is typical in developing countries, so it can be concluded that Korea's tuberculosis control is remaining at developing country level. And there were more male patients than female patients in all age groups except for patients in their twenties. According to some clinicians, this could be explained by malnutrition among young female caused by extreme diet, but more research is needed in order to present a clear cause of this phenomenon.
Despite notification rate of MDR- and XDR-TB patients was low, and the final list of resistant drugs was yet to be obtained under the TBnet, the study provides an overview of current status of drug-resistant TB patients. According to the 7th National TB Prevalence Survey in 1995, the drug-resistant rate for new cases was 5.8%, and for TB patients with prior treatment history was 25.0%5. We can conclude that the rate of new cases without prior treatment history has not changed much since, while the rate of TB patients with prior treatment history has decreased. Comparing with the result of sample survey on drug-resistance for the new TB cases who received treatment from public health centers in 2004, 2.7% of new cases were MDR-TB patients treated in the public health centers6, which is similar to the rate of MDR-TB patients in private institutions in 2008.
In terms of treatment outcomes, 36.0% of total TB patients are categorized as 'completed' cases, which is more than 'cured' (30.4%) cases. There were no standardized TB treatment guidelines for private institutions back in 2008, thus not all patients who completed their treatment in the private institutions underwent sputum smear or culture test in the last month of their treatment. This is why there have been more completed cases than cured cases, but the proportion of cured cases is expected to increase in private institutions thanks to standardized guidelines for tuberculosis that has been provided since 2011.
National TB Prevalence Survey will provide the most accurate tool to understand current TB status in Korea, but it is difficult to conduct such survey considering vast amount of time and cost required and low level of expected private participation. Successfully managing surveillance system can be one of the most effective ways. As seen in the study, TB patient reporting rate to the TBnet increased from 67.6% in 20061 to 70%, but it is still low and measures should be taken to encourage private institutions to notify to the system.
Through this study, we could identify that among the patients who claimed for medical expenses to the HIRA, 97% of them were in fact TB patients, and we could conclude that HIRA data can be a very effective in promoting understanding on current status of TB in private institutions. In this regard, it is necessary to develop a model for sample abstraction and to establish guidelines for investigation to improve study accuracy.
References
- 1.Kim YS, Park KH, Yoo HS, Kwon JW, Shin E. Reporting of national notifiable infectious diseases (NNIDs) and related characteristics. Korean J Epidemiol. 2007;29:200–210. [Google Scholar]
- 2.Korea Centers for Disease Control and Prevention. Annual report on the notified tuberculosis patients in Korea 2010. Cheongwon: Korea Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 3.Korea Centers for Disease Control and Prevention. Guidelines for national tuberculosis control, 2011. Cheongwon: Korea Centers for Disease Control and Prevention; 2011. [Google Scholar]
- 4.World Health Organization. Treatment of tuberculosis guidelines. 4th ed. Geneva: World Health Organization; 2009. [PubMed] [Google Scholar]
- 5.Ministry of Health and Welfare, Korean Institute of Tuberculosis, Korean National Tuberculosis Association. Report on the 7th tuberculosis prevalence survey in Korea. Seoul: Korean Institute of Tuberculosis; 1996. [Google Scholar]
- 6.Bai GH, Park YK, Choi YW, Bai JI, Kim HJ, Chang CL, et al. Trend of anti-tuberculosis drug resistance in Korea, 1994-2004. Int J Tuberc Lung Dis. 2007;11:571–576. [PubMed] [Google Scholar]