Abstract
Objective. To measure changes in pharmacy and medical students’ physician-pharmacist collaboration scores resulting from a workshop designed to promote understanding of the others’ roles in health care.
Methods. More than 88% of first-year pharmacy (n = 215) and medical (n = 205) students completed the Scale of Attitudes Toward Physician-Pharmacist Collaboration on 3 occasions in order to establish a baseline of median scores and to determine whether the scores were influenced by an interprofessional workshop.
Results. Participation in the interprofessional workshop increased pharmacy students’ collaboration scores above baseline (p=0.02) and raised the scores of medical students on the education component of the collaboration survey instrument (p=0.015). The collaboration scores of pharmacy students greatly exceeded those of medical students (p<0.0001).
Conclusion. A workshop designed to foster interprofessional understanding between pharmacy and medical students raised the physician-pharmacist collaboration scores of both. Crucial practical goals for the future include raising the collaboration scores of medical students to those of pharmacy students.
Keywords: interprofessional education, interdisciplinary education, health profession students, pharmacy students, medical students, attitudes
INTRODUCTION
Important attributes of healthcare professionals include but are not limited to cognitive empathy,1 interprofessional collaboration,2 and patient-centered orientations.3 Survey instruments to measure each of these attributes have been designed and validated to varying degrees.1-5 Scores of healthcare professions students on the empathy and patient-centered orientation survey instruments have declined or remain unchanged instead of increasing during training.1,3,6,7 The latter findings are disturbing because good relationships with patients and colleagues, which are likely fostered by these attributes, increase patient satisfaction, promote adherence with treatment plans, and minimize malpractice claims.1 For example, patients with type 2 diabetes mellitus have an 80% greater chance of achieving good control of their blood hemoglobin A1c and low-density lipoprotein cholesterol levels if their primary care physician has a high rather than low empathy score.8 The Jefferson Scale of Physician Empathy, which was used in the latter study, is a content-specific and context-relevant instrument to measure cognitive empathy in healthcare professions students and practitioners.9 We modified this instrument to measure empathy in other health professions students and validated its use in pharmacy students.4
By using regular assignments to elicit and perform critical reflection on difficult issues in the healthcare professions, professional education, and life, we have succeeded at modestly increasing cognitive empathy and patient-centered orientation scores in healthcare professions students.3,5,10,11 The efforts also included a number of workshops3,5,11 involving activities such as watching and discussing a performance about the challenges of aging.10 While such interventions helped to improve students’ empathy and patient-centered orientation scores, changes in their interprofessional collaboration scores had not been measured using a validated instrument. In this study, we determined whether students’ collaboration scores changed over the course of their first 5 or 6 months of professional education. Additionally, we hypothesized that a workshop designed to promote understanding between heathcare professions students would increase their interprofessional collaboration scores. We also began to test whether all of these important attributes of healthcare professionals may be interdependent rather than independent by determining whether students’ collaboration scores correlated with their empathy scores.
METHODS
Two hundred fifteen first-year pharmacy students, 205 first-year osteopathic medical students, and 82 first-year biomedical sciences students at Midwestern University (Downers Grove, IL, campus) were invited to complete the physician-pharmacist collaboration survey instrument (Scale of Attitudes Toward Physician-Pharmacist Collaboration2) on 3 separate occasions. Most biomedical sciences students pursue masters of sciences degrees while attempting to improve their applications to medical, dental, or other health professions schools.
To establish a baseline and to determine whether the student survey scores changed over time, students completed the survey instrument during the first week of biochemistry classes (August 2011 for medical students and September 2011 for pharmacy and biomedical sciences students) and again immediately prior to the workshop that was designed to foster understanding among healthcare professions students (January 2012). To determine whether the workshop influenced their collaboration scores, students were asked to complete the survey instrument following the workshop.
Students also completed the Jefferson Scale of Empathy (HPS-Version, which was validated in pharmacy students for use in this study by Dr. Mohammadreza Hojat, Jefferson Medical College, Thomas Jefferson University, and the authors) for pharmacy and biomedical sciences students4 and JSE, S-Version for medical students8,9) during the first week of classes. They were asked to mark their survey forms with a unique 4-digit or letter identification code of their choice so that their scores on the empathy survey instrument could be matched with their scores on the collaboration instrument for correlation analysis. Students used a second unique identification code for their pre- and post-workshop collaboration instrument forms so their scores could be paired for more powerful statistical analysis of changes occurring in association with the interprofessional workshop. Students selected a second identification code because we found in prior studies10 that students do not always recall their codes over several weeks or months.
Pharmacy and biomedical sciences students were introduced to the interprofessional workshop on January 5, 2012, and medical students were introduced on January 10, 2012. This workshop consisted of two 50-minute sessions and was included in the biochemistry courses without decreasing either the total biochemistry course content or the requirements for satisfactory completion. At the beginning of the first session, students completed the physician-pharmacist collaboration survey instrument (preworkshop survey instrument). They were then asked to think about the details of the professional role they aspired to play in the care and management of 2 patients and their families.
The first patient was Henrietta Lacks, a 31-year-old woman who was near death from cancer as described in the book The Immortal Life of Henrietta Lacks.14(p63-66) Students were required to read this entire book, an account of the lives of Mrs. Lacks and her descendants, for their biochemistry courses prior to (for pharmacy and biomedical sciences students) or shortly after (for medical students) matriculating at the university in August 2011. Thus, students knew a great deal about Mrs. Lacks and her family before the interprofessional workshop in January 2012.
The second patient was Cameron Lord, a child born with Tay Sachs disease and the subject of the documentary, “Cameron’s Arc.”15 This 21-minute DVD describes the patient and her family as they learned the diagnosis and decided how to proceed as a family who wanted Cameron to remain at home and out of the hospital and emergency department as much as possible. Care in the latter case covered more than 18 months prior to and immediately after the death of the patient at 2 years of age.
For the second session of the workshop, students were asked to reflect individually on the roles they believed the other healthcare professional group represented at the workshop (future pharmacists or physicians) would have in the care and management of each patient. They were instructed to bring their theories about the other professional’s role to the second session of the workshop occurring on January 12, 2012 (2 or 7 days later, depending on the group). During this second session, students were randomly assigned to an interprofessional team. Most teams consisted of 6 members: 1 biomedical sciences student, 2 to 3 pharmacy students, and 2 to 3 medical students. During this workshop session, team members exchanged contact information, began a team assignment concerning the purpose and value of critical reflection,11 and planned future meetings or other means of communicating in order to complete all assignments.
After team discussions of individual theories about their respective roles in the care and management of the 2 patients, students were instructed to complete and submit a final individual critical reflection concerning how their understanding of the role of the other professional prior to the workshop may not have been completely correct and consistent with their humanistic and professional values. All team meetings were to be held by January 19, 2012, at which time students completed the physician-pharmacist collaboration survey form (post-workshop survey instrument) a final time during class.
Pearson’s correlation coefficients (r) and other statistical analyses were performed using GraphPad Prism 5 Software, Inc. (GraphPad, La Jolla, CA). Students’ collaboration scores deviated significantly from a Gaussian distribution and were skewed dramatically toward the highest possible values every time the survey instrument was administered (D’Agostino-Pearson normality test, p<0.0001 7 of 9 administrations, p=0.001 and p=0.05, 1 administration each). Consequently, analysis of variance and t tests could not be used to compare mean values of the survey scores obtained at different times or for different groups. Instead, median survey scores were compared using the Kruskal-Wallis test with Dunn’s comparison for individual groups, the Mann-Whitney U test, or the Wilcoxon matched-pairs signed rank test (when pre- and post-workshop survey results could be paired for the same individuals using their unique ID codes). Chi square and effect size values also were calculated using the modified treatments of the data indicated in the results and discussion sections, given that median values cannot be used to calculate effect size values.12,13 This study was reviewed and found to fulfill the criteria for exemption by the Midwestern University Institutional Review Board.
RESULTS
Of the 215 first-year pharmacy students in the 2015 class, 99%, 97%, and 93% completed the physician-pharmacist collaboration survey instrument the first, second, and third time it was administered, respectively. These rates were 97%, 94%, and 88%, respectively, for the 205 first-year medical students, and 98%, 95%, and 90%, respectively, for the 82 first-year biomedical sciences students. Of the collaboration survey instruments completed the first day of classes, 83%, 88%, and 83% of survey instruments from pharmacy, medical, and biomedical sciences students, respectively, could be matched for correlation analysis with their Jefferson empathy survey instruments. Similarly, the collaboration scores of 82% of medical students completing the post-workshop survey instrument could be matched with their preworkshop collaboration survey scores for a more powerful paired statistical analysis. The vast majority of our biomedical sciences students eventually want to enter other professional programs (primarily dental, allopathic or osteopathic medicine). For this reason and because the results for biomedical sciences students mirrored those observed for medical students, we report only medical and pharmacy student data in this study.
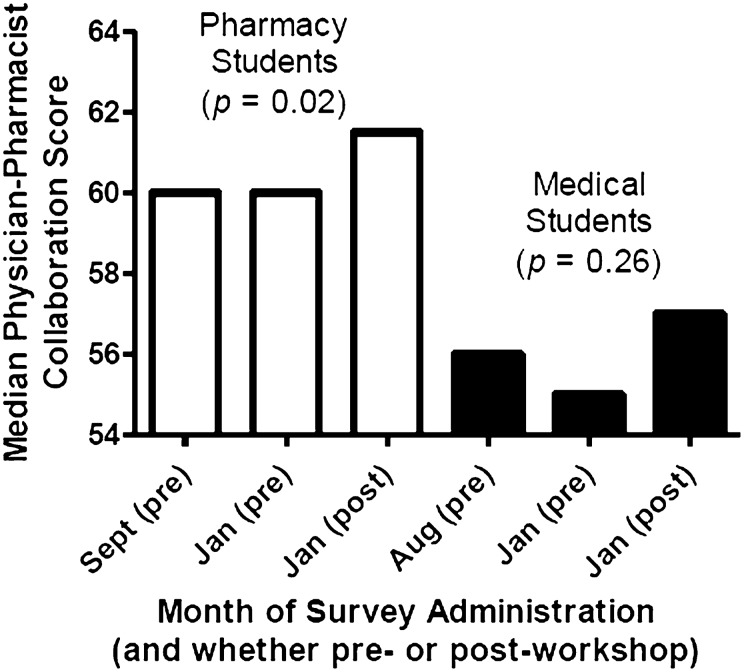
At the beginning of their academic programs (August/September), pharmacy students scored significantly higher on the physician-pharmacist collaboration survey instrument than did medical students (p<0.0001). Of a maximum possible score of 64, the median scores for pharmacy and medical students were 60 and 56, respectively (Figure 1), indicating a high level of commitment to interprofessional collaboration by both groups of students at the time of matriculation into their respective programs. This difference between pharmacy and medical students persisted on both the pre- and post-workshop survey instruments. Results of the Kruskal-Wallis test comparing the 2 groups of students at all 3 administrations of the survey instrument are shown in Figure 1.
Figure 1.
Differences between collaboration scores of first-year pharmacy students’ and first-year medical students’ and changes in these scores over time and in relation to students’ participation in an interprofessional collaboration workshop.
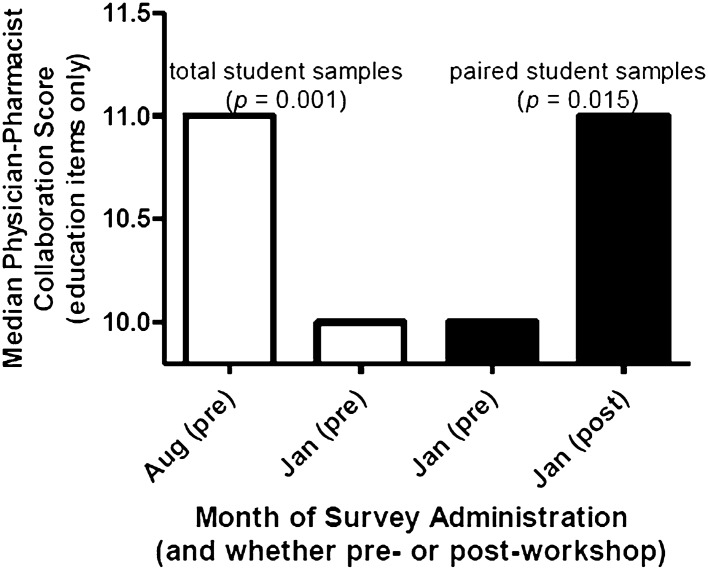
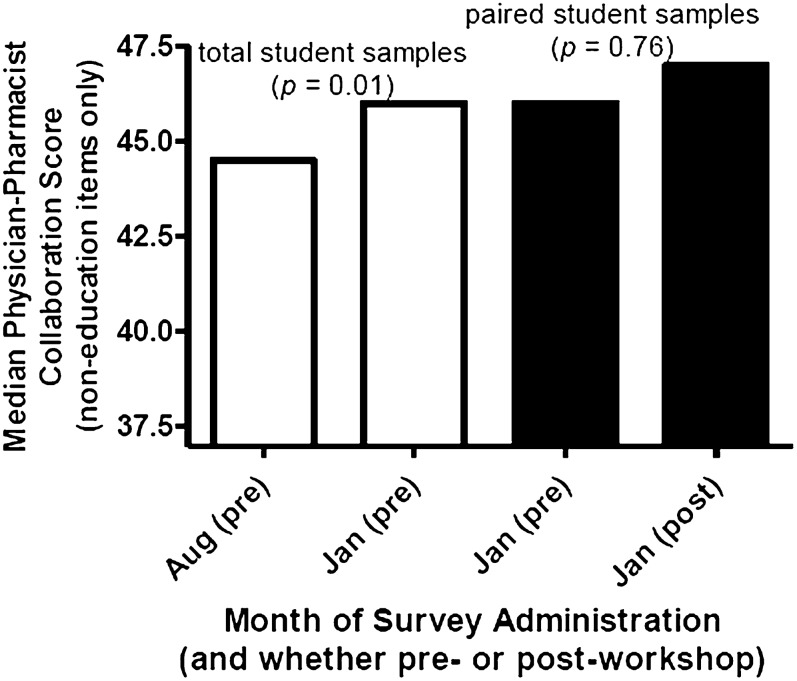
The physician-pharmacist collaboration scores did not change significantly for pharmacy or medical students during the 4 or 5 months preceding the interprofessional workshop (Figure 1). The underlying 3-factor structure of the survey instrument2 was examined for possible changes in each of 3 factors: responsibility and accountability, shared authority, and interprofessional education. No changes in the factors were observed in pharmacy students prior to the interprofessional workshop; however, when the 3 items explicitly mentioning education were assessed together and separately from the other 13 items on the collaboration survey instrument, a significant decrease in these interprofessional education scores (p=0.001) was observed in medical students during the 5 months preceding the interdisciplinary workshop (Figure 2). In contrast, scores on the other 2 factors (13 items) increased significantly (p=0.01) among medical students prior to the workshop (Figure 3). The decrease in the education component was offset by the increase in the other 2 factors during the months preceding the workshop (Figures 1-3).
Figure 2.
Changes in medical students’ scores on the combined 3 items of the physician-pharmacist collaboration survey instrument explicitly mentioning education over time (months [open bars]) and in association with the workshop intervention (pre- vs post-workshop [filled bars]).
Figure 3.
Changes in medical students’ scores on the 13 non-education items of the physician-pharmacist collaboration survey instrument over time (months [open bars]) and in association with the workshop intervention (pre- vs post-workshop [filled bars]).
The median physician-pharmacist collaboration score increased significantly for pharmacy students by 38% of the maximum increase that was possible in association with the interprofessional workshop (p=0.02) (Figure 1). The proportion of pharmacy students who achieved the maximum possible score of 64 more than doubled in association with the workshop from 16% to 35% of students completing the pre- and post-workshop survey instruments, respectively (p<0.0001).
In the 82% of medical students whose scores could be paired for more powerful statistical analysis, the median score of the education component of the collaboration survey instrument increased significantly (p=0.015) in association with the interprofessional workshop (Figure 2). The increase in scores for the other 2 factors (13 items) was not significant (p=0.76) for medical students completing the workshop (Figure 3). Physician-pharmacist collaboration scores correlated positively with those on the Jefferson Scale of Empathy for both pharmacy and medical students. The Pearson correlation coefficient (r) values were 0.42 (p<0.0001) for pharmacy students and 0.38 (p<0.0001) for medical students.
DISCUSSION
We examined whether students’ physician-pharmacist collaboration scores would change in association with a workshop designed to increase understanding of the role of the other professional in health care. Based on students’ scores on the physician-pharmacist collaboration scale, our results for 3 distinct groups of students support the conclusion that such a workshop fosters interprofessional collaboration.
The workshop was associated with an increase in first-year pharmacy students’ total median physician-pharmacist collaboration scores and an increase in the proportion of pharmacy students achieving the maximum collaboration score on the survey instrument. From these results, the interprofessional empathy workshop is estimated to have had an effect size on pharmacy students that is equivalent to increasing the success rate of a treatment from 39.5 to 60.5% (r2 = X2/N = 0.044, r = 0.21).12,13 As pharmacy students’ physician-pharmacist collaboration scores did not change during the 4 months preceding the workshop, the increased collaboration scores occurring in association with the workshop likely can be attributed directly to an effect of the workshop.
Changes in first-year medical and biomedical sciences students’ physician-pharmacist collaboration scores were more complex and subtle, requiring consideration of the 3-factor structure underlying this collaboration scale.2 These factors include responsibility and accountability, shared authority, and interprofessional education. Analysis of the results of the physician-pharmacist collaboration survey instruments using only the 3 items specifically addressing education2 showed an increase in the median score of 50% of the maximum possible interprofessional education scores in medical and biomedical sciences students in association with the workshop (Figure 2). As these median education scores had decreased by about the same amount during the 4 or 5 months preceding the interprofessional workshop (Figure 2), the workshop likely led to the increased education scores. Regardless, the effects of the workshop on medical students’ collaboration scores were relatively small in relation to increases that could have been achieved (Figure 1).
In this regard, the relatively large difference between pharmacy students’ and medical students’ collaboration scores remained about the same throughout the study (Figure 1). While the median values we report cannot be used to estimate effect size, we can use the 3 median values reported for pharmacy students and the 3 median values for medical students (Figure 1) to calculate mean and standard deviation values (n = 3) for each group of students (p=0.004 for a significant difference between the groups, t test). These mean and standard deviation values also can be used12,13 to calculate an effect size r value of 0.95 (GraphPad Prism 5, Graph Pad Software, Inc, La Jolla, CA). Because this effect size is of crucial practical importance,12,13 it would be desirable to design a series of workshops in which teamwork with pharmacy students could more dramatically and favorably influence the attitudes of medical students toward interprofessional collaboration. In our view,3,5,10,11 such a permanent and progressive increase in collaboration scores would require repeated interventions and emphasis on the practical importance of interprofessional collaboration to patient care. Future studies should include such a curricular design and goal for increasing and maintaining higher collaboration scores.
The present study is, to our knowledge, also the first to show a significant correlation between interprofessional collaboration scores and empathy scores in both pharmacy and medical students. These correlations (Pearson’s coefficients of about 0.4 in both cases) are of moderate to crucial practical importance.12,13 Hence, these measures of 2 important healthcare professional attributes are, in part, interdependent rather than entirely independent. Educational efforts to foster 1 attribute may also promote the other.
While this study benefits from results for 3 distinct groups of healthcare professions students, the single-institution nature of the observations limits their generalizability. Similarly, the studies did not include randomly assigned control groups, but we did establish baselines of survey results over the 4 or 5 months preceding the workshop on interprofessional empathy. Changes in survey scores in association with the workshop increased above this baseline for pharmacy students’ total scores and for medical and biomedical sciences students’ education component scores.
Additionally, there were 14 days between pharmacy students’ completion of the pre- and post-workshop survey instruments of attitudes toward physician-pharmacist collaboration, while there were only 9 days between medical students’ completion of the survey instruments. Furthermore, medical students matriculated 1 month earlier than did pharmacy students. However, the different results for pharmacy and medical students are unlikely to be attributable to the difference in time between administrations of the survey instrument or the different times of matriculation. The results for biomedical sciences students mirrored those of medical students, while the times of matriculation and between survey instrument administrations were the same for biomedical sciences students and pharmacy students. Finally, other courses in the curriculum of each program could have had an impact on collaboration scores, although the net effect of these other courses appears to have been neutral, according to our baseline data for students’ total collaboration scores (Figure 1).
CONCLUSIONS
A workshop to foster understanding of other professionals’ roles in health care improved students’ attitudes toward interprofessional collaboration. While these attitudes were generally favorable, medical students’ collaboration scores remained significantly lower than those of pharmacy students across the course of this study. Sustained efforts to promote and maintain appreciation for other professionals’ work in health care could improve medical students’ collaboration scores in a way that might increase the likelihood of successful interprofessional collaborations in their future practices.
ACKNOWLEDGMENT
We thank Dr. Mohammadreza Hojat for stimulating discussions of possible research efforts and for critiquing earlier versions of the manuscript.
REFERENCES
- 1.Hojat M. Empathy in Patient Care: Antecedents, Development, Measurement, and Outcomes. New York: Springer; 2007. [Google Scholar]
- 2.Van Winkle LJ, Fjortoft N, Hojat M. Validation of an instrument to measure pharmacy and medical students’ attitudes toward physician-pharmacist collaboration. Am J Pharm Ed. 2011;75(9):Article 178. doi: 10.5688/ajpe759178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Van Winkle LJ, Chandar N, Green JM, et al. Does critical reflection by biochemistry learning teams foster patient-centered beliefs among medical students? Med Sci Educator. 2011;21(2):158–168. [Google Scholar]
- 4.Fjortoft N, Van Winkle LJ, Hojat M. Measuring empathy in pharmacy students. Am J Pharm Educ. 2011;75(6):Article 109. doi: 10.5688/ajpe756109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Van Winkle LJ, Dobie S, Ross VR, et al. Acute intervention to foster reflection on reciprocity in relationships increased participants’ patient- or student-centered orientation scores in association with a medical biochemistry course. Internet J Med Educ. 2011;1(2) [Google Scholar]
- 6.Neumann M, Edelhäuser F, Tauschel D, et al. Empathy decline and its reasons: a systematic review of studies with medical students and residents. Acad Med. 2011;86(8):996–1009. doi: 10.1097/ACM.0b013e318221e615. [DOI] [PubMed] [Google Scholar]
- 7.Nunes P, Williams S, Sa B, Stevenson K. A study of empathy decline in students from five health disciplines during their first year of training. Intl J Med Educ. 2011;2:12–17. [Google Scholar]
- 8.Hojat M, Louis DZ, Markham FW, Wender R, Rabinowitz C, Gonnella JS. Physician empathy and clinical outcomes for diabetic patients. Acad Med. 2011;86(3):359–364. doi: 10.1097/ACM.0b013e3182086fe1. [DOI] [PubMed] [Google Scholar]
- 9.Hojat M, Mangione S, Nasca TJ, et al. The Jefferson scale of physician empathy: development and preliminary psychometric data. Educ Psychol Meas. 2001;61(2):349–365. [Google Scholar]
- 10.Van Winkle LJ, Fjortoft N, Hojat M. Impact of a workshop about aging on the empathy scores of pharmacy and medical students. Am J Pharm Educ. 2012;76(1):Article 9. doi: 10.5688/ajpe7619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Van Winkle LJ, Robson C, Chandar N, et al. Use of poems written by physicians to elicit critical reflection by students in a medical biochemistry course. J Learn Arts. 2011 7(1) [Google Scholar]
- 12.Hojat M, Xu G. A visitor’s guide to effect size: statistical versus practical significance of research findings. Adv Health Sci Educ. 2004;9(3):241–249. doi: 10.1023/B:AHSE.0000038173.00909.f6. [DOI] [PubMed] [Google Scholar]
- 13.Rosenthal R, Rubin DB. A simple, general purpose display of magnitude of experimental effect. J Educ Psych. 1982;74(2):166–169. [Google Scholar]
- 14.Skloot R. The Immortal Life of Henrietta Lacks. New York: Random House; 2010. [Google Scholar]
- 15.American Academy of Pediatrics. Cameron’s Arc: Creating a Full Life [DVD]. Boston, MA: Care Points; 2007. [Google Scholar]