Abstract
Objectives. To evaluate first-year doctor of pharmacy (PharmD) students' communication apprehension, outcome expectations, and self-efficacy for communication over the duration of a 15-week patient-counseling course.
Design. First-year PharmD students (n=94) were asked to complete a 47-item, self-administered questionnaire on 3 occasions over the duration of the Nonprescription Drugs/Patient-Counseling course during the fall 2009 and 2010 semesters.
Assessment. Eighty-seven of 94 students completed the survey instrument across data collection periods. There were significant reductions in total communication apprehension scores and in the communication apprehension subscores for meetings and public speaking, and significant increases in self-efficacy over time. No differences were found for outcome expectations of communication scores or the subscores for interpersonal conversations and group discussion.
Conclusions. Communication apprehension may be decreased and self-efficacy for communication increased in first-year PharmD students through a 15-week Nonprescription Drugs/Patient-Counseling course using small-group practice sessions, case studies, and role-play exercises in conjunction with classroom lectures.
Keywords: communication apprehension, self-efficacy, non-prescription medication, counseling
INTRODUCTION
The provision of optimal patient care requires pharmacists to communicate effectively with patients, physicians, and other members of the healthcare team to achieve effective medication consumption, improve health outcomes, and increase health-related quality of life.1-4 To do so, pharmacists must possess the knowledge, willingness, and opportunity to provide effective communication as well as the belief that communicating effectively is important.5,6
The importance of effective communication by pharmacists is emphasized by the Accreditation Council for Pharmacy Education as well as the American Association of Colleges of Pharmacy’s Center for the Advancement of Pharmaceutical Education Educational Outcomes.7,8 Patient counseling is also mandated by many state pharmacy practice acts and the Omnibus Budget Reconciliation Act of 1990.9 Pharmacists are obligated to devote more time to patient care, including providing comprehensive patient counseling and education to ensure that patients adequately comprehend how to take their medications and adhere to pharmacotherapy regimens. Pharmacists who lack effective communication skills are unlikely to provide or perhaps even offer such services to patient populations,6,10 placing patients at an increased risk for negative health outcomes and pharmacists at risk for legal consequences.
Three factors believed to potentially impede the development of effective communication skills of pharmacy students are their self-efficacy for communication, outcome expectations of communication, and communication apprehension. Self-efficacy for communication is an individual’s self-perception regarding the ability to engage in effective communication.11 Outcome expectation of communication is one’s belief that engaging in effective communication will lead to desired patient outcomes.11 Students who progress through the curriculum without developing an appreciation for the value of effective communication or confidence in their abilities to communicate effectively may become communication-apprehensive pharmacists. Communication apprehension, a term that refers to “an individual’s level of fear or anxiety associated with real or anticipated communication with others,”10 negatively affects students’ abilities to communicate effectively as well as their academic performance.12 Individuals possessing high communication apprehension may be viewed negatively within their environment.13 If pharmacists are perceived negatively within a pharmacy setting, patients may be much less likely to ask questions regarding their medication regimen, leading to missed opportunities for important patient counseling. This evidence suggests that communication apprehension could have a significant negative impact on pharmacists as well as patient care.14 The credibility of information provided by pharmacists who have high communication apprehension could be questioned by patients. Especially concerning is the strong possibility that pharmacy students possessing high communication apprehension will carry this trait into their careers as practicing pharmacists, impeding their ability to communicate effectively. Systematic desensitization training, a type of behavior therapy that helps individuals overcome various anxieties has been suggested as a method of decreasing communication apprehension in pharmacy students.5
Colleges and schools of pharmacy are responsible for ensuring that students graduating from their respective programs develop the knowledge and skills necessary to communicate effectively.15 The acquisition of such skills and knowledge must begin early in the PharmD students’ classroom curriculum. In order to assist students in attaining these traits, most PharmD programs have historically included some form of communications course in their curricula. The curricula in many programs have been modified to provide students greater opportunities to participate in group work, oral presentations, patient simulation laboratories, and additional writing assignments.15-19
An important area of focus for all colleges and schools of pharmacy is to help ensure that students mature into productive healthcare professionals by assisting in their development of effective communication skills. To address this need, we developed a 4-credit-hour required course (3 lecture hours and 1 laboratory hour). The goal of this course was to provide first-year PharmD students the opportunity to practice the elements of effective patient-pharmacist-communication, which are learned in classroom lectures, in a laboratory setting. The authors hypothesized that requiring students to actively practice effective communication would alleviate apprehension and facilitate the development of lifelong learning skills, such as effective communication. The purpose of this study was to evaluate the influence of this course on first-year PharmD students’ apprehension toward communication, outcome expectations of communication, and self-efficacy for communication.
DESIGN
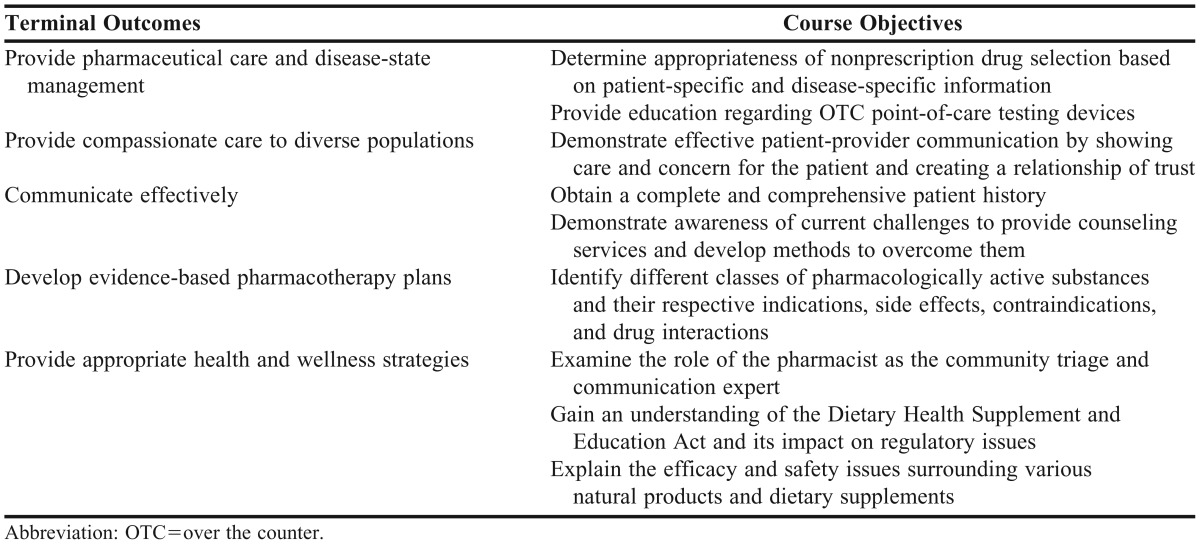
All students attending Union University School of Pharmacy are required to enroll in the Non-Prescription Drugs/Patient-Counseling course during the fall semester of their first year of the PharmD program. The terminal outcomes and course objectives are presented in Table 1. This 15-week course includes both classroom lecture and laboratory components. Pharmacy faculty members and guest speakers with knowledge or expertise in topics discussed during lectures or laboratory sessions were involved throughout the semester. The lecture component of the course was taught in 50-minute sessions, 3 days a week. This portion of the course was designed to acquaint students with indications, actions, possible adverse events, and contraindications of various nonprescription medications, with an emphasis on patient-provider communication. Readings were assigned with each lecture topic, and students were evaluated by means of 3 examinations given throughout the semester. The laboratory portion used a small-group environment to familiarize students with topics such as health literacy, appropriate nonverbal communication (eg, body language and eye contact), and optimization of patient counseling. This was accomplished through the use of patient cases that reinforced lecture material and allowed for the application of counseling and peer communication. Students were divided into groups of no more than 20 and assigned to 1 of 3 laboratory sections, which met once a week for 3 hours. Students were evaluated on their ability to obtain patient medical histories, perform finger-stick testing, and provide adequate counseling regarding appropriate use of various nonprescription products and devices.
Table 1.
Course Mapping to Terminal Outcomes of a Patient Counseling Course for First-Year Doctor of Pharmacy Students
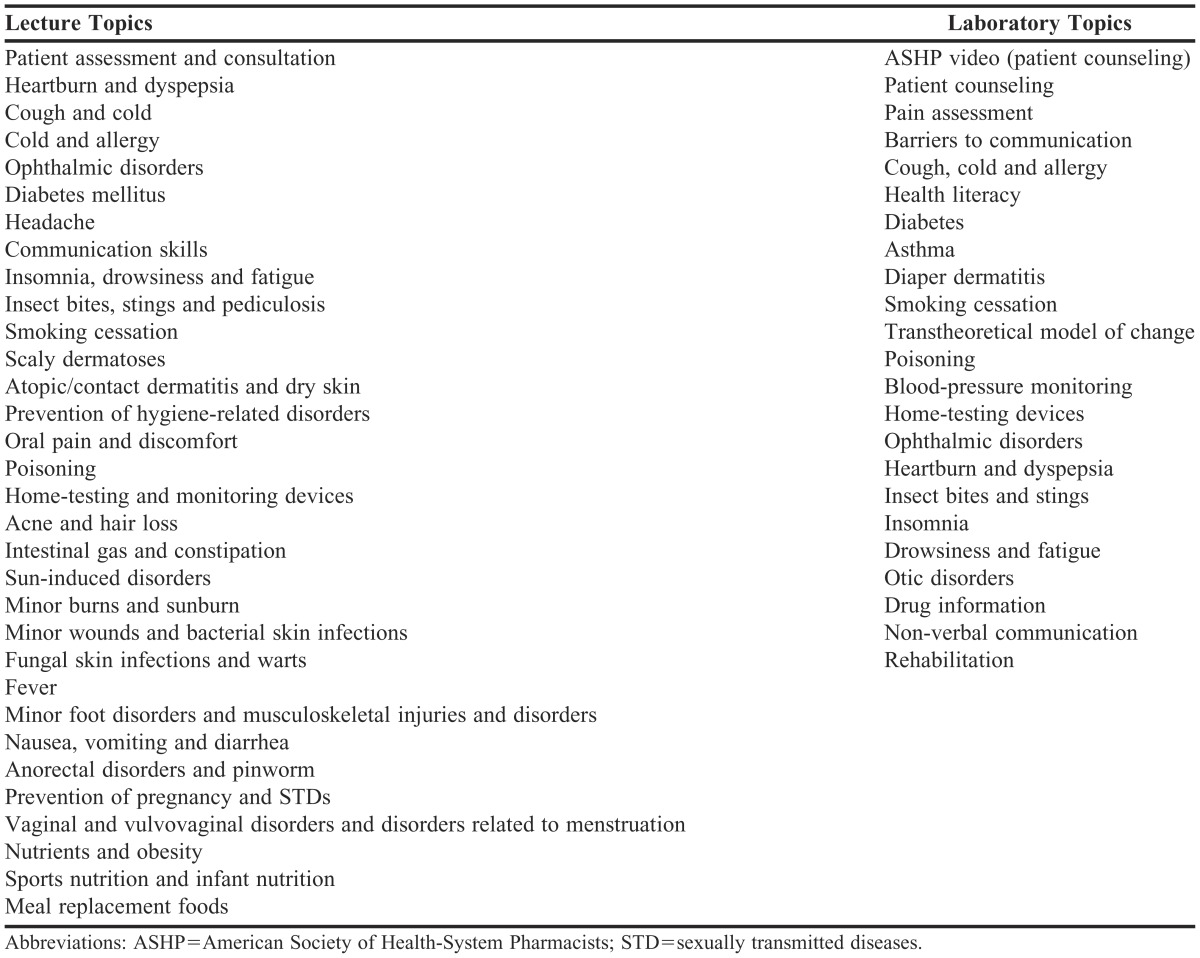
Role-play sessions using patient case scenarios were incorporated into laboratory sessions to provide students the opportunity to play various roles, including that of pharmacist, patient, and evaluator, for concepts addressed during prior lectures. Laboratory scenarios included patients with various disease states and the need for communicating specific information. Communication challenges, such as hearing and vision impairment, confusion regarding medications, and financial barriers, were incorporated into each scenario. More complex counseling situations involving patients exhibiting personality characteristics such as anxiety, belligerence, or apathy were also incorporated to challenge the students to convey pertinent information and ensure patient or caregiver understanding in a realistic situation. For an assignment, students were grouped into pairs and required to do research and develop a monograph for an herbal product. Each student pair delivered a 10-minute presentation on their monograph at the end of the semester. The final examination for the laboratory portion of the course consisted of successfully counseling a standardized patient with a particular disease state. Topics covered during lectures and laboratory sessions are provided in Table 2. The Union University Institutional Review Board approved this study.
Table 2.
Course Lecture and Laboratory Topics in a Patient Counseling Course for First-Year Doctor of Pharmacy Students
EVALUATION AND ASSESSMENT
Data were collected for this study over a 2-year period. All first-year PharmD students were asked to participate as part of their Non-Prescription Drugs/Patient Counseling Course in the fall semesters of the 2009 and 2010 school years. Students were provided an information letter explaining the purpose and procedures of the study, that participation was voluntary, and that they could decline to participate at any time without penalty.
All students were asked to complete a self-administered questionnaire on 3 occasions throughout the fall 2009 and fall 2010 semesters. Students completed the questionnaire during the first laboratory session (time 1), at midterm (time 2), and during the final laboratory session (time 3). The questionnaire consisted of 47 items and was divided into 4 sections. The first section measured students’ communication apprehension using the previously validated Personal Report of Communication Apprehension-24 (PRCA-24), which has consistently demonstrated high reliability, with alphas regularly exceeding 0.90.10,20 Measured on a 5-point Likert scale, this instrument was designed to assess respondents’ attitudes toward interpersonal communication. In addition to providing subscores on the contexts of group discussion, meeting, interpersonal conversation, and public speaking, the instrument generates an overall communication apprehension score for each student.
Overall PRCA-24 scores ranged from 24 to 120 with scores between 83 and 120, indicating high communication apprehension, 55 to 83 indicative of moderate levels, and scores between 24 and 55 indicating low levels. Scores on the 4 contexts of communication apprehension ranged from 6 to 30. A score greater than 18 indicates some degree of apprehension.14 Students possessing low self-efficacy for communication lack the confidence to engage in communication, and those with low outcome expectations believe that even if they were to engage in communication, the desired outcome would not be accomplished.21 Therefore, the second and third sections of the survey instrument contained 10 items, each assessing students’ outcome expectations and self-efficacy for communication. These statements were measured on a 5-point Likert scale and were based on course outcome objectives. Respondents’ ratings regarding statements within each scale were summed to obtain a total efficacy and outcome-expectation score. Higher scores on each scale indicated high self-efficacy or outcome expectations. As suggested by Roth and colleagues, the individual’s mean response to a particular scale was used to account for item-level missing data.22 In the final section, students were asked to provide demographic data, including age and gender.
All data were entered into a Microsoft Excel spreadsheet for management and accuracy verification. Once verified, data were exported to IBM SPSS, version 19 (IBM Corp, Armonk, NY) for analyses. Descriptive statistics were generated for all demographic measures. Repeated measures analysis of variance (ANOVA) was conducted at the a priori alpha level of 0.05 in order to examine the differences in total scores for students’ self-efficacy for communication, outcome expectations of communication, and communication apprehension over time. In addition to students’ PRCA-24 total scores, analyses also included a comparison of the PRCA-24 subscores among the 3 data collection times, including group discussion, meeting, interpersonal conversation, and public speaking.
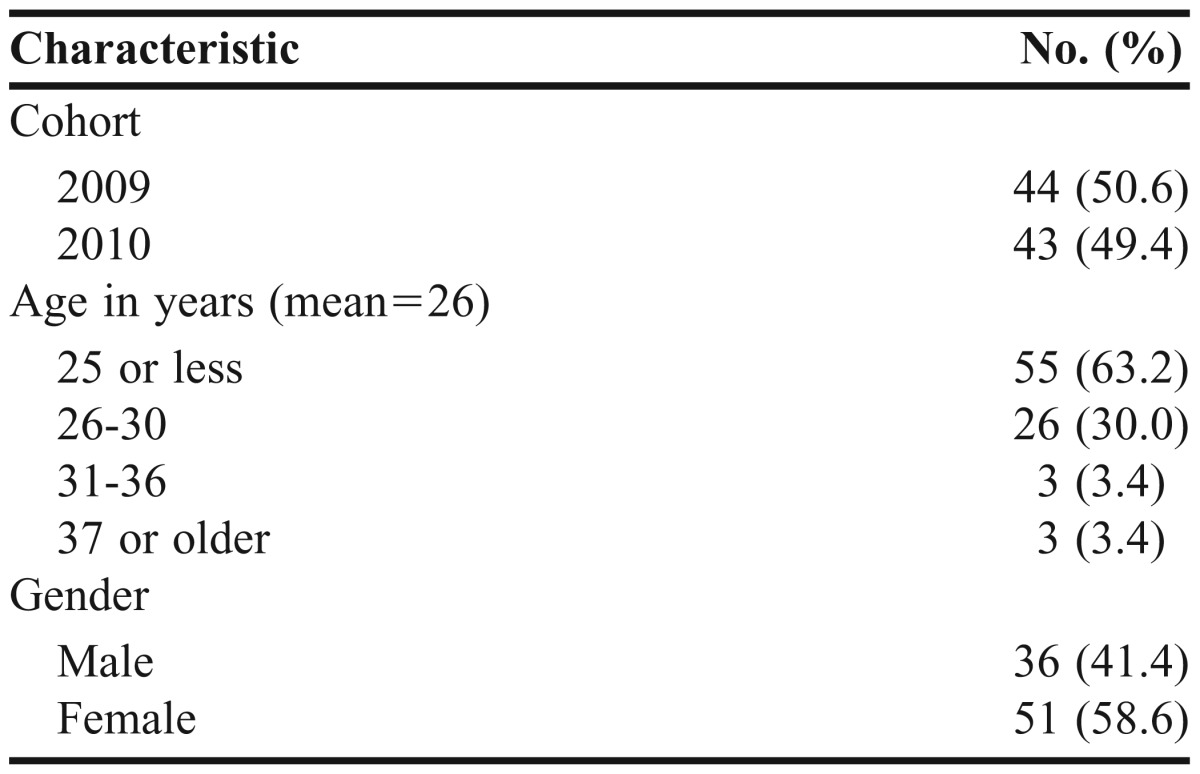
The demographic characteristics of participants are presented in Table 3. Eighty-seven of 94 students participated in the investigation, for a response rate of 92.6%. Forty-four were from the 2009 class and 43 were from the 2010 class. The majority of the students were female (58.6%) with an average age of 26 years. There were no significant gender differences related to any outcome variable. In an effort to minimize response burden, information concerning student age or pharmacy experience was not collected in the survey instrument used for this study. Because the average age of students in each class was obtained from the School of Pharmacy’s Office of Student Affairs, the effect of age and experience on the outcome variables could not be assessed. The criteria suggested by Nunnally were applied to determine the adequacy of the reliability coefficients obtained for the self-efficacy and outcome-expectation measures.23 After time 1, Cronbach’s alphas were found to be 0.86 and 0.90 for the outcome expectations and self-efficacy scales, respectively. In subsequent administrations of the instrument at times 2 and 3, the alphas for the outcome expectations and self-efficacy scales were 0.92 and 0.90 and 0.98 and 0.94, respectively.
Table 3.
Demographic Characteristics of First-Year Doctor of Pharmacy Students Participating in a Patient Counseling Course (N=87)
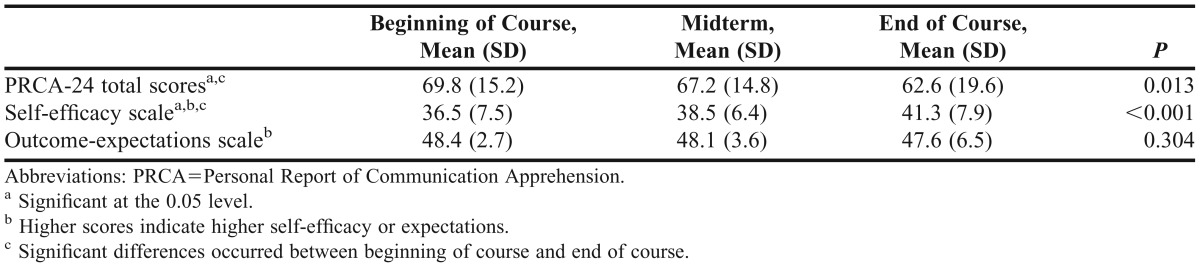
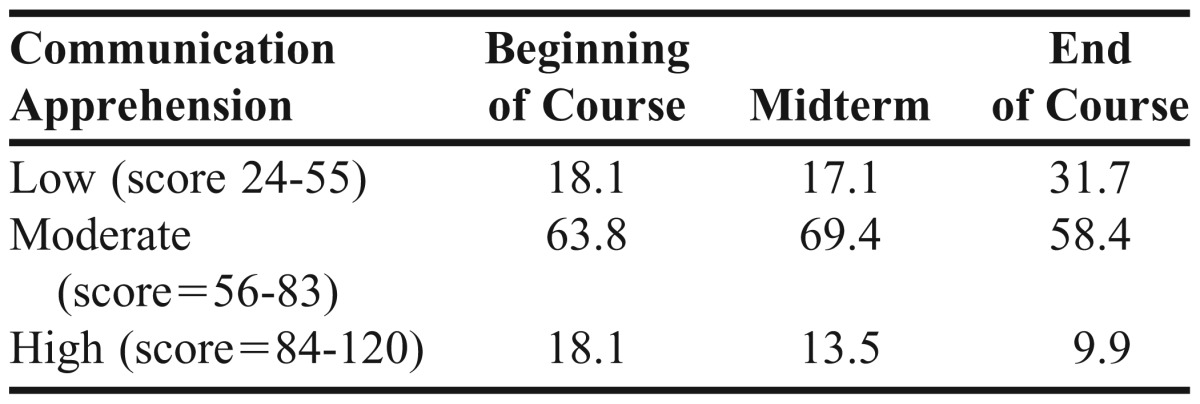
Comparisons of communication apprehension, outcome expectations of communication, and self-efficacy for communication over time are described in Table 4. Over the duration of a structured patient counseling course offered in the first semester of the PharmD curriculum, overall communication apprehension decreased significantly (p=0.013). Post-hoc tests using the Bonferroni correction revealed a significant reduction from the initial laboratory session mean of 68.8 to the final session mean of 62.6 (p=0.02). Differences observed between the initial laboratory session and midterm and between the midterm and the final laboratory session were not significant. The percentage of students reporting high levels of communication apprehension decreased greatly over the 3 data collection periods (Table 5).
Table 4.
Changes in First-year Doctor of Pharmacy Students’ Communication Apprehension, Self-Efficacy and Outcome-Expectation Scores During a Patient Counseling Course (N = 87)
Table 5.
Percent of Participating First-Year Doctor of Pharmacy Students Possessing Low, Moderate, and High Communication Apprehension Over Time, % (N = 87)
There were also significant improvements in the students’ self-efficacy for communication (p<0.001). Differences in self-efficacy were observed between the initial and final laboratory sessions (p<0.001) as well as between the midterm and final laboratory sessions (p=0.033) but not between the initial and midterm sessions (p=0.184). There was no significant difference for outcome expectations of communication at any point in time. Students’ expectations of communication appeared to remain high throughout the duration of the course.
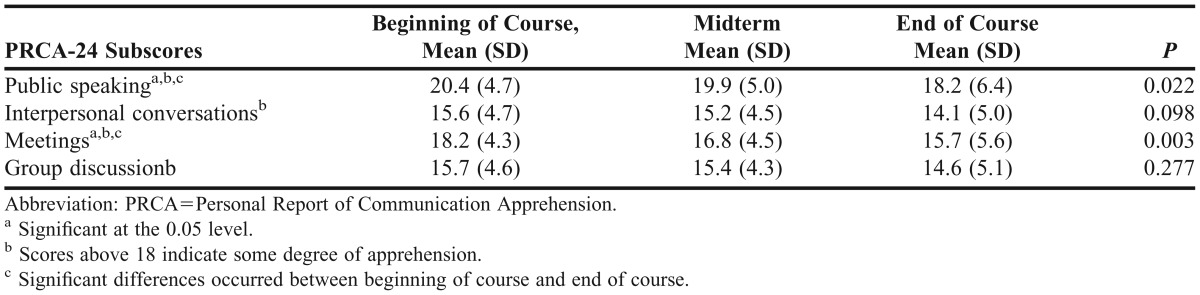
Results of the PRCA-24 subscores analyses are described in Table 6. The communication context subscores of public speaking and meetings decreased significantly over time ( p=0.022 and p=0.003, respectively). Post-hoc analyses revealed a slight reduction from the initial laboratory session to midterm for both public speaking and meetings (mean, 20.4 vs 19.9 and mean, 18.2 vs 16.8, respectively) (p>0.05). However, from the initial laboratory session to the final session, the mean scores regarding these 2 contexts decreased to 18.2 for public speaking and 15.7 for meetings (p=0.047 and p = 0.003, respectively). The differences for these 2 contexts from midterm to the final laboratory session were not significant (p=0.145 and p=0.093, respectively). The context scores of interpersonal conversations and group discussion did not decrease significantly over time.
Table 6.
Changes in Communication Apprehension Subscores of First-Year Doctor of Pharmacy Students During a Patient-Counseling Course (N = 87)
DISCUSSION
Almost 1 in 5 (18.1%) students in this study entered the program possessing high communication apprehension scores. The initial mean self-efficacy score was 36.5 out of a possible 50. By the end of the semester end, the percentage of students possessing high communication apprehension scores decreased by more than half (55%) and the mean self-efficacy score increased to 41.3. These findings are crucial, given the importance of patient counseling, the profession, and the plethora of complications resulting from inadequate health literacy of patients that are specific to pharmacy settings.24 These results suggest that a course that reinforces lectures with structured, small-group laboratory sessions emphasizing patient-pharmacist communication is an effective means of decreasing apprehension while increasing self-efficacy in first-year PharmD students. The participation of students in case studies and role-play scenarios during the same week that they attend a lecture on the topic was integral to these findings. Additionally, students also benefited from being involved in such a course early in their professional curriculum (ie, in the first semester of their first year). Although systematic desensitization was not truly used in this course, continuous practice in a laboratory setting with smaller groups using case studies and role-play helped students become less apprehensive and more confident about communicating medication information.
The finding of no significance over time on outcome expectations of communication may be a result of students believing, prior to the first class, that effective communication provided by pharmacists would result in improved patient outcomes. However, the mean outcome-expectation scores showing that students believe effective communication is crucial to patient care are not an indicator that students possess the traits necessary to communicate effectively. Focused training involving various techniques and practice are required to assist students in developing this skill. These findings are encouraging, though, given that the students in this study entered the PharmD program with high regard for the influence that effective communication from a pharmacist can have on patient outcomes. As the pharmacy profession becomes more patient-centered in its roles and responsibilities, the importance of pharmacists’ communication ability and their desire to engage in communication becomes more evident.
Students initially reported the greatest apprehension on the PRCA-24 context scores of public speaking (mean = 20.4) and meetings (mean = 18.2). However, significant decreases in apprehension were observed over time for these 2 context scores. According to PRCA-24 scoring guidelines, the reduction in each context was large enough to result in scores not indicative of apprehension. While slight mathematical differences over time were seen for the context scores of interpersonal conversations and group discussions, these decreases were not significant. This finding is believed to be a result of baseline or time 1 scores on these contexts being below that indicating apprehension, meaning that students in this study were apprehensive about communicating in a public setting and during meetings but not during group discussions or interpersonal conversations.
The generalizability of this study’s results should be further assessed in programs with larger class sizes, which may require additional resources, such as space, faculty, and time. Further studies could also evaluate whether interactions in other lecture courses, laboratories, or with faculty members may contribute to a decrease in students’ apprehension and/or an increase in their self-efficacy. This possibility was not addressed in the current study.
It would also be of interest to determine and demonstrate the effects of high communication apprehension and low self-efficacy for communication on patient counseling during laboratory exercises. This study sought only to examine if, over the duration of the course, these traits could be decreased and improved, respectively, in first-year PharmD students. Further exploration into the effect these traits have on the pharmacist-patient interaction is needed. Subsequent demonstration of these effects through patient cases and simulation may also serve as a valuable teaching tool for students. Additionally, in an effort to minimize response burden, information concerning students’ age or pharmacy experience was not collected for this investigation. This aspect of the study design made it impossible to assess the effect of age or experience on the outcome variables. It would be interesting to learn whether previous work experience or age has a positive effect on variables such as self-efficacy for communication. Future research into this area is needed.
Systematic desensitization is a commonly recognized method of mitigating communication apprehension.5 Earlier research also demonstrates its utility in reducing communication apprehension in pharmacy students.25 Although not formally used in this course because of resource constraints, methods of incorporating systematic desensitization into communication courses warrants further research. Integrating systematic desensitization may prove especially useful in laboratory sessions, which typically involve a smaller number of students and a more hands-on method of instruction.
SUMMARY
This study demonstrates that a 15-week course on nonprescription drugs and patient counseling that used small-group practice sessions, case studies, and role-play in conjunction with lectures can decrease communication apprehension and increase communication self-efficacy in first-year PharmD students. Requiring this type of course with both lecture and laboratory components early in the professional curriculum may facilitate the development of effective communication skills in pharmacy students. Pharmacy students who progress through the professional program without developing the abilities necessary to effectively convey medication information may become pharmacists who are hesitant to engage in such conversations with patients and other healthcare professionals. The onus of ensuring that graduates develop these abilities is on pharmacy educators in their respective programs.
REFERENCES
- 1.Hepler CD, Strand LM. Opportunities and responsibilities in pharmaceutical care. Am J Hosp. 1990(47):533–43. http://www.qu.edu.qa/pharmacy/professional_development/documents/Responsibilities_Hepler_Strand.pdf. Accessed September 19, 2012. [PubMed] [Google Scholar]
- 2.Yanchick JK. Implementation of a drug therapy monitoring clinic in a primary-care setting. Am J Health-Syst Pharm. 2000;57(Suppl 4):S30–S34. doi: 10.1093/ajhp/57.suppl_4.S30. [DOI] [PubMed] [Google Scholar]
- 3.Harrison DL, Bootman JL, Cox ER. Cost-effectiveness of consultant pharmacists in managing drug-related morbidity and mortality at nursing facilities. Am J Health-Syst Pharm. 1998;55(15):1588–1594. doi: 10.1093/ajhp/55.15.1588. [DOI] [PubMed] [Google Scholar]
- 4.Schumock GT, Meek PD, Ploetz PA, Vermeulen LC. Economic evaluations of clinical pharmacy services. Pharmacotherapy. 1996;16(6):1188–1208. [PubMed] [Google Scholar]
- 5.Berger BA, Richmond V, McCroskey JC. Baldwin. Reducing communication apprehension in pharmacy students: is there a better way? Am J Pharm Educ. 1982;46(2):132–136. [Google Scholar]
- 6.Anderson-Harper HM, Berger BA, Noel R. Pharmacists’ predisposition to communicate, desire to counsel and job satisfaction. Am J Pharm Educ. 1992;56(3):252–258. [Google Scholar]
- 7.Accreditation Council for Pharmacy Education. Accreditation Standards. https://www.acpe-accredit.org/pdf/FinalS2007Guidelines2.0.pdf. Accessed July 13, 2012.
- 8.American Association of Colleges of Pharmacy. Center for the Advancement of Pharmaceutical Education. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed July 13, 2012. [DOI] [PMC free article] [PubMed]
- 9.Omnibus Budget Reconciliation Act. Washington, DC: US Government Printing Office; 1990. p. 152. [Google Scholar]
- 10.McCroskey JC. Oral communication apprehension: a summary of recent theory and research. Hum Commun Res. 1977;4(1):78–96. [Google Scholar]
- 11.Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215. doi: 10.1037//0033-295x.84.2.191. [DOI] [PubMed] [Google Scholar]
- 12.Fremuth VS. The effects of communication apprehension on communication effectiveness. Hum Commun Res. 1976;2(3):389–295. [Google Scholar]
- 13.McCroskey JC, Anderson JF. The relationship between communication apprehension and academic achievement among college students. Hum Commun Res. 1976;3(1):73–81. [Google Scholar]
- 14.Sarriff A, Gillani WS. Communication apprehension among Malaysian pharmacy students: a pilot study. Indian J Pharm Educ Res. 2011;45(1):8–14. [Google Scholar]
- 15.Beardsley RS. Communication skills development in colleges of pharmacy. Am J Pharm Educ. 2001;65(4):307–314. [Google Scholar]
- 16.Mackellar A, Ashcroft DM, Bell D, James DH, Marriot J. Identifying criteria for the assessment of pharmacy students' communication skills with patients. Am J Pharm Educ. 2007;71(3):Article 50. doi: 10.5688/aj710350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Shah B, Chewning B. Conceptualizing and measuring pharmacist-patient communications: a review of publish studies. Res Social Adm Pharm. 2006;2(2):153–185. doi: 10.1016/j.sapharm.2006.05.001. [DOI] [PubMed] [Google Scholar]
- 18.Chereson RS, Bilger R, Mohr S, Wuller C. Design of a pharmaceutical laboratory: a survey of practitioners. Am J Pharm Educ. 2005;69(1):Article 3. [Google Scholar]
- 19.Gallimore S, George AK, Brown MC. Pharmacy students' preferences for various types of simulated patients. Am J Pharm Educ. 2008;72(1):Article 4. doi: 10.5688/aj720104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Baldwin JH, McCroskey JC, Knutson TJ. Communication apprehension in the pharmacy student. Am J Pharm Educ. 1979;43(2):91–93. [Google Scholar]
- 21.Strecher VJ, McEvoy B, Becker M, Rosestock I. The role of self-efficacy in achieving health behavior change. Health Educ Q. 1986;13(1):73–91. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- 22. Roth PL, Switzer III FS, Switzer D. Missing data in multi-item scales: A Monte Carlo Analysis of missing data techniques. Org Res Methods. 1999;2(3):211–232.
- 23.Nunnally JC. Psvchometric Theory. 2nd ed. New York: McGraw-Hill; 1978. [Google Scholar]
- 24.King SR, McCaffrey III DJ, Bouldin AS. Health literacy in the pharmacy setting: defining pharmacotherapy literacy. Pharm Pract. 2011;9(4):213–220. http://www.pharmacypractice.org/vol09/04/213-220.htm. Accessed July 13, 2012.
- 25.Berger BA, Baldwin HJ, Richmond VP, McCroskey JC. Implementation of a systematic desensitization program and classroom instruction to reduce communication apprehension in pharmacy students. Am J Pharm Educ. 1982;46(3):227–234. [Google Scholar]