Abstract
Objectives. To implement a pharmacokinetics curriculum that used small-team active learning and assess students’ perceptions.
Design. The course design and delivery were based on delivery of Student Team lecture followed by concept reinforcement through problem-based learning sessions. Course faculty members facilitated classroom and problem-based learning discussions to promote an active-learning environment.
Assessment. An anonymous survey instrument was administered to students prior to and following completion of the pharmacokinetics course. Students reported a significant decrease in anxiety from 67% to 44% related to working in small teams upon completion of the course. However, students maintained negative perceptions related to peer teaching, with 80% of students reporting anxiety related to receipt of course information from peers. The course had a positive impact on students’ ability to apply concepts to case-based scenarios, but little impact on their perceived ability to identify and critically evaluate new material and present that material to their peer team.
Conclusions. The team-based structure defined herein for delivery of a pharmacokinetics curriculum offers students a tangible method to increase their comfort and confidence in the application of pharmacokinetic concepts in therapy.
Keywords: team learning, active learning, pharmacokinetics, problem-based learning
INTRODUCTION
Historically, pharmacokinetics education in pharmacy programs has been delivered using traditional lecture-based pedagogy in which information is defined, controlled, and directed by the faculty member delivering the material. However, the authors believe this method limits higher levels of learning as the lecturer defines the “important” content using learning objectives, lecture materials, and required textbooks. Consequently, the breadth of the material covered is limited and assimilated based on topic content and associated cues from faculty members about which material is most important. By doing so, the practice of requiring students to independently assess data and information, as practitioners do daily, is deferred until later in the student’s education, generally until they begin advanced clinical practice experiences.
Some colleges and schools of pharmacy use problem-based learning (PBL) or case-based learning in their pharmacokinetics courses.1-3 Key attributes of these courses and the present course series structure include delivery of foundational information by student and/or faculty members with application of concepts through case-based problems, followed by a collective review of solutions.
Faculty members at South University developed an integrated delivery format for a pharmacokinetics course series centered on an active-learning process in which students are required to assess, assimilate, and deliver information to peers, as is required of pharmacists in clinical practice. In this system, the course series is facilitated jointly by faculty members in the Departments of Pharmacy Practice and Pharmaceutical Sciences with 3 to 4 faculty members serving as facilitators and 1 as the course coordinator. The course series is taught over two 10-week quarters and is integrated with fundamental pharmacokinetic principles presented and immediately followed by relevant clinical case applications. By teaching the course in this manner, pharmacokinetic theory is continuously overlaid upon timely clinical examples, reinforcing important pharmacokinetic principles. This collaboration of disciplines ensures students have a comprehensive understanding of the fundamental pharmacokinetic principles and proper clinical application. This method also requires students to become actively engaged in the learning process by performing searches for relevant scientific and clinical pharmacokinetic data. This paper describes implementation and assessment of the effectiveness of this team-based approach to learning.
DESIGN
Pharmacokinetics I is a 4-quarter-hour recitation course taught in three 2-hour blocks each week. Pharmacokinetics II is a 3-quarter hour course taught as a recitation course with three 1.5-hour blocks each week. Rather than using a traditional group learning approach, the design was modeled after the classic team/work group structure used in many companies. Students were divided into teams of 8 or 9 students based on their final grades in the Pharmaceutical Calculations course, thus balancing levels of academic performance among the teams. With this distribution technique, the grade point average among teams varied by only +/- 0.2 based on a 4.0 scale. Teams were assigned a color designation as the team name and asked to elect a team leader and an assistant team leader.
The team leader acted as a facilitator, directing team organization, time management, and interaction. Additionally, the team leader served as the liaison to the faculty coordinator (ie, faculty team leader) for course issues raised by an individual or the team via completion of a weekly written report. The weekly team report provided a summary of team activities, attendance at meetings and in class, suggestions for improvement, and concerns with class material or structure. These reports were reviewed by the faculty team leader and discussed at the 1-hour weekly faculty team meetings as needed. The assistant team leader served as team leader if the team leader was absent.
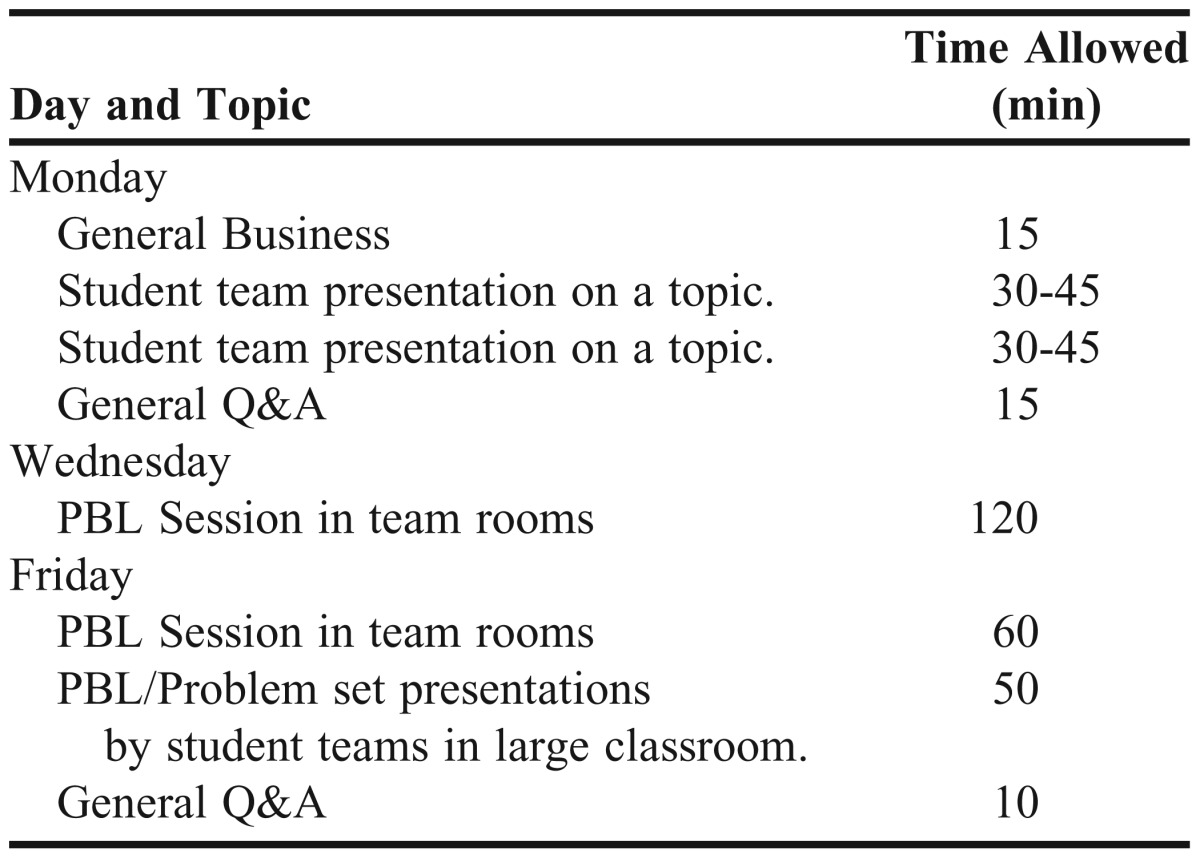
A typical week began with student-team presentations on 2 to 3 related topics, with question and answer time held after each presentation (Table 1). Student teams presented mini-lectures to the class on their assigned topic. Faculty members reviewed each presentation the week prior to delivery and provided feedback on the content to the team. On the day of the presentation, an online randomization tool (http://www.random.org) was used to determine which team member would present the topic for the group. At least 3 faculty members graded the presentation using a rubric, and the presentation grade, which comprised 10% of the final grade, was assigned to each team member. Following the presentations in the lecture hall, student teams convened for 1.5 class periods for further discussion and completion of associated problem sets/cases (ie, PBL). During this time, faculty members circulated among the teams and provided guidance. The class reassembled at the end of the week and randomly chosen teams presented solutions for the associated problem sets to the class. To foster an open-learning environment and discussion among teams of alternate solution methods, no grade was assigned to the team that initially presented the solutions to a problem set.
Table 1.
Class Schedule for a Typical Week
Assessment of individual student performance included a weekly, unannounced 10-minute quiz which collectively counted 5% of the final grade; three 25-question examinations per quarter, each of which counted 20% of the final grade; and a 50-question cumulative final examination, which counted 25% of the final grade. The Immediate Feedback Assessment Technique by Epstein Education Enterprise (http://www.if-at.com/home/) as described by Persky was used for administration of the examinations.4
ASSESSMENT
An IRB approved pre-exposure and post-exposure anonymous survey instrument was administered prior to and following completion of the 2-course series to determine students’ perception of the delivery method. Students were asked to rate on a 5-point Likert scale their response to questions related to the structure and delivery style of the courses as well as their ability to perform relative to the individual and team expectations within the courses. Students were asked to assess their feelings related to functioning within the small-team learning environment, the use of peer instruction coupled with independent study, and their ability to identify and evaluate key points applicable to specific case-based scenarios. Additionally, students evaluated their perceived ability to develop and present content to peers using a mini-lecture format. An open-ended response section was provided to collect perceptions of the greatest potential or realized benefits and the greatest obstacles related to the course delivery format. Data collection took place the first week of the course and again the week after final examinations without unique identifiers. As there was no mechanism to identify which students completed the pre- and post-exposure survey instrument, the data were analyzed as independent groups. Mann-Whitney U test was performed to identify significant differences in perceptions between groups using SPSS, version 17 software (IBM, New York, NY).
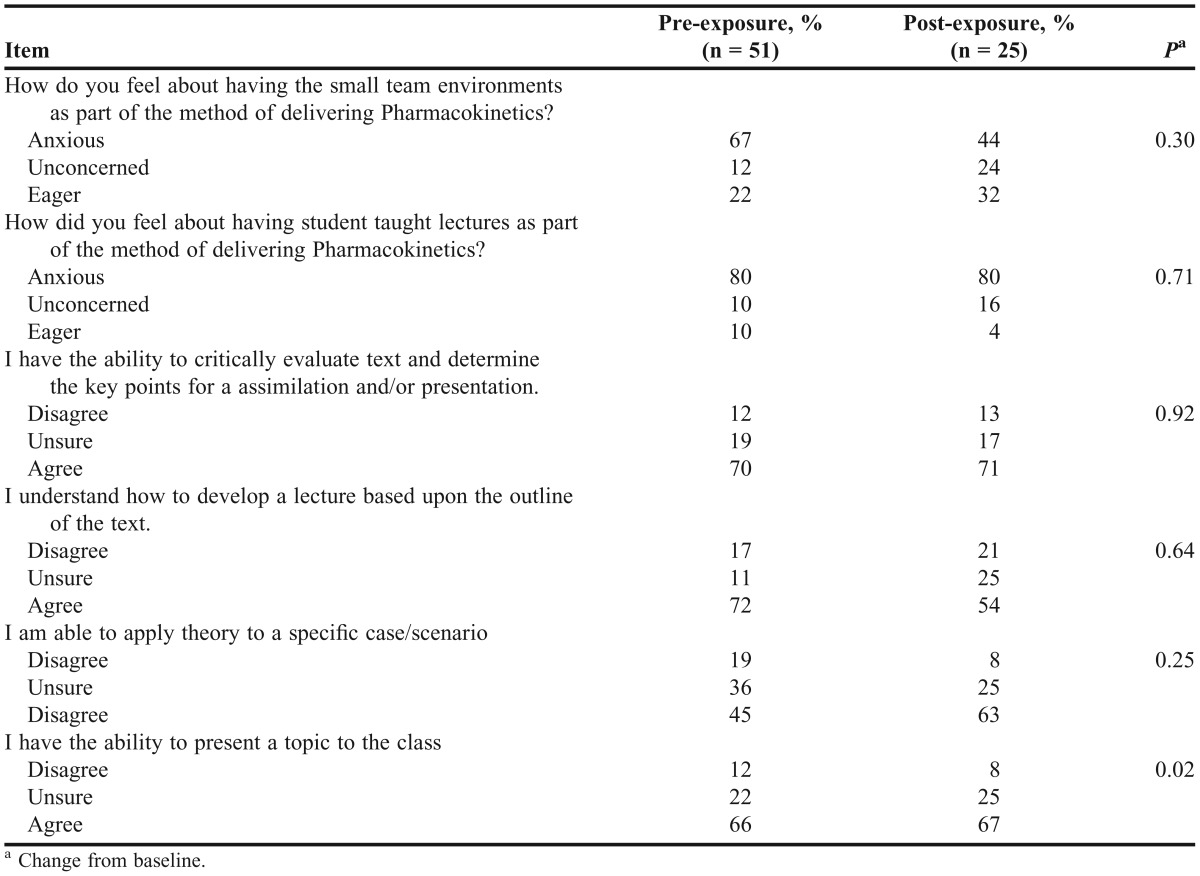
Enrollment in the Pharmacokinetics course series in 2009 was 89 students. Pre- and post-exposure survey response rates were 57% (n = 51) and 28% (n=25), respectively. Approximately 40% of the students reported participation in active-learning models (eg, small teams, peer lectures, etc) prior to taking the courses. Students reported a relative decrease in anxiousness related to working in small teams after completing the courses. Prior to the delivery of the courses, the majority of students reported being anxious (67%) about experiencing this learning method while others reported being unconcerned (12%) or eager (22%) (Table 2). Students’ anxiety level regarding peer instruction remained unchanged at 80% on the pre- and post-exposure survey instruments.
Table 2.
Survey Results of Unrelated Samples
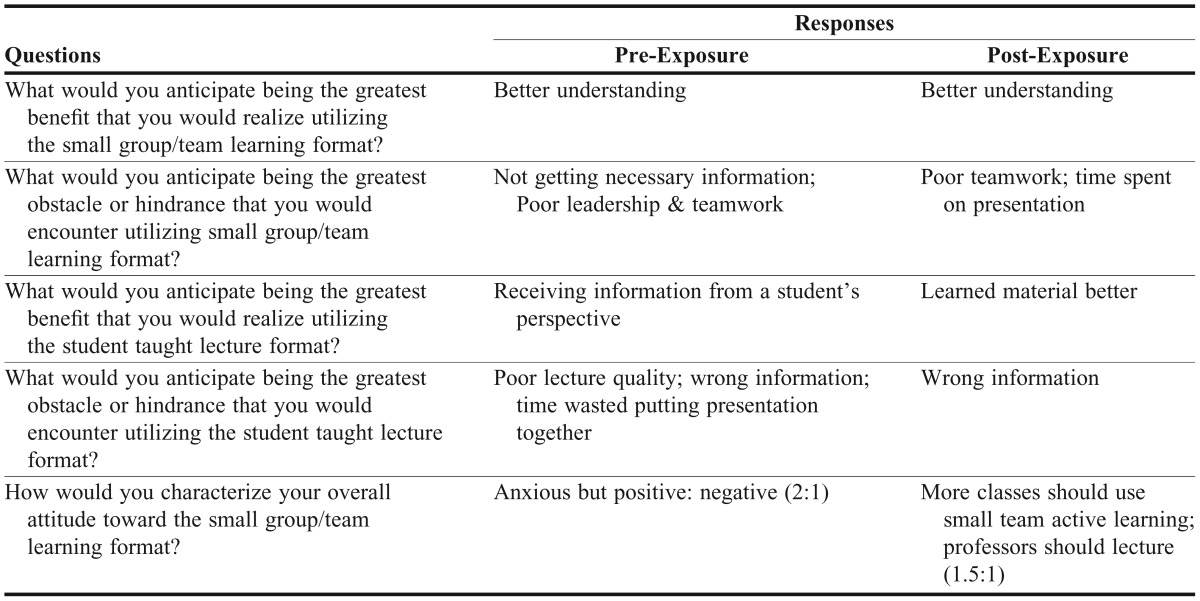
Based on written feedback from survey instruments, the students’ main concern regarding peer instruction was receiving “wrong” information during the team presentations on problem-set solutions (Table 3) despite that the discussions took place in class in the presence of faculty facilitators. On the pre-exposure survey, a majority of the students (70%) believed they would have the ability to critically evaluate and identify key points. This percentage remained essentially unchanged (71%) after completing the class (Table 2). Students’ agreement that they had the ability to develop a pharmacokinetic lecture decreased from 72% to 54% upon completion of the course. No significant change was noted in their perceived ability to present a topic to the class. There was a positive shift in students’ perceived ability to apply theory to case-based scenarios from 45% to 63%. The percentage of students who did not believe they were able to apply theory decreased from 19% to 8% and the percentage who were unsure of their ability decreased from 36% to 29%. The post-exposure survey was not powered to discern significant differences with respect to the previously reported data in the pre-exposure survey of student perceptions despite considerable trends in reported perceptions. However, there was a significant decrease (p=0.02) in post-exposure survey responses related to anxiety associated with group presentations occurring in front of the class.
Table 3.
Open-Ended Questions and Common Responses
In the open-ended section of the survey instrument, a high-frequency post-exposure response to the item regarding students’ overall attitude toward small-team learning was students’ preference for faculty members to deliver the course content using a traditional lecture format (Table 3). However, approximately 33% of responses also indicated that more classes should use an active-learning format.
DISCUSSION
While compilation and assessment of objective data is ongoing, anecdotal feedback from students and preceptors after completing intermediate practice experiences (immediately following Pharmacokinetics I) indicated that students were capable and comfortable performing pharmacokinetic calculations and possessed a functional foundation of pharmacokinetic principles. One of the most important responses in support of team-based learning coupled with problem-based activities was a positive shift in students’ perceived ability to apply theory to case-based scenarios.
While facilitation of pharmacokinetics using the team learning approach requires greater faculty commitment than that for a traditional lecture format, the authors believe the method offers superior preparation for modern, multidisciplinary practice by exposing students to pharmacokinetic concepts as well as how to work toward a common goal in a team setting. This change in learning format is understandably uncomfortable for most students who are accustomed to a traditional lecture setting where the information delivered is often limited and well defined by educational objectives. The necessity for identifying and prioritizing unfamiliar information and subsequently relaying that information to others is a new exercise for many students, but a vital skill they will need as practicing pharmacists. While student responses with respect to the ability to evaluate and identify key points remained unchanged, the perceived ability to convey that information decreased 18% over the progression of the course. The initial exposure to faculty clinicians with different backgrounds and training offers the first glimpse at the diversity of modern health care practice. The lack of traditional classroom structure and multiple “correct” approaches for any given situation were major contributing factors to the discomfort students reported. The authors believe the students’ apprehension is reflective of the curricular timing of the course combined with the course series’ departure from the predominant pedagogy in practice today, ie, lecture. The placement offers one of the first instances that students are consistently required to find and prioritize new information, as well as the realization, perhaps for the first time, that there are multiple “correct” answers in most clinical situations.
Interestingly, students were uncomfortable receiving information delivered by their peers because they felt it was suspect or incorrect. The authors also noted in multiple classroom interactions that the discussion of differing methods or points of view often exacerbated this phenomenon. Despite this inherent discomfort, the students ultimately reported perceived strengthening in their ability to apply knowledge and concepts to case-based scenarios similar to real practice situations.
SUMMARY
Implementing a small-team active-learning approach to teaching a pharmacokinetics course series continually reinforces pharmacokinetic principles by overlaying pharmacokinetic theory with clinical examples. In addition, this structure promotes personal and professional skills required to work in modern multidisciplinary teams and independent critical thinking, and develops a functional foundation of pharmacokinetics principles and confidence in individual clinical judgment. Although students’ are more critical of their pharmacokinetic ability upon completion of the course series, overall the experience will prepare them for careers within pharmacy.
ACKNOWLEDGEMENT
The authors wish to thank Lilia Z. Macías-Moriarity, PhD, MPH, for her invaluable assistance with the data analysis and its interpretation.
REFERENCES
- 1.Romero RM, Eriksen SP, Haworth IS. Quantitative assessment of assisted problem-based learning in a pharmaceutics course. Am J Pharm Educ. 2010;74(4):Article 66. doi: 10.5688/aj740466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dupuis RE, Persky AM. Use of case-based learning in a clinical pharmacokinetics course. Am J Pharm Educ. 2008;72(2):Article 29. doi: 10.5688/aj720229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomas SG, Hester EK, Duncan-Hewitt W, Villaume WA. A high-stakes assessment approach to applied pharmacokinetics instruction. Am J Pharm Educ. 2008;72(6):Article 146. doi: 10.5688/aj7206146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Persky AM. Multi-faceted approach to improve learning in pharmacokinetics. Am J Pharm Educ. 2008;72(2):Article 36. doi: 10.5688/aj720236. [DOI] [PMC free article] [PubMed] [Google Scholar]