ABSTRACT
BACKGROUND
Adverse drug events after hospital discharge are common and often serious. These events may result from provider errors or patient misunderstanding.
OBJECTIVE
To determine the prevalence of medication reconciliation errors and patient misunderstanding of discharge medications.
DESIGN
Prospective cohort study
SUBJECTS
Patients over 64 years of age admitted with heart failure, acute coronary syndrome or pneumonia and discharged to home.
MAIN MEASURES
We assessed medication reconciliation accuracy by comparing admission to discharge medication lists and reviewing charts to resolve discrepancies. Medication reconciliation changes that did not appear intentional were classified as suspected provider errors. We assessed patient understanding of intended medication changes through post-discharge interviews. Understanding was scored as full, partial or absent. We tested the association of relevance of the medication to the primary diagnosis with medication accuracy and with patient understanding, accounting for patient demographics, medical team and primary diagnosis.
KEY RESULTS
A total of 377 patients were enrolled in the study. A total of 565/2534 (22.3 %) of admission medications were redosed or stopped at discharge. Of these, 137 (24.2 %) were classified as suspected provider errors. Excluding suspected errors, patients had no understanding of 142/205 (69.3 %) of redosed medications, 182/223 (81.6 %) of stopped medications, and 493 (62.0 %) of new medications. Altogether, 307 patients (81.4 %) either experienced a provider error, or had no understanding of at least one intended medication change. Providers were significantly more likely to make an error on a medication unrelated to the primary diagnosis than on a medication related to the primary diagnosis (odds ratio (OR) 4.56, 95 % confidence interval (CI) 2.65, 7.85, p < 0.001). Patients were also significantly more likely to misunderstand medication changes unrelated to the primary diagnosis (OR 2.45, 95 % CI 1.68, 3.55), p < 0.001).
CONCLUSIONS
Medication reconciliation and patient understanding are inadequate in older patients post-discharge. Errors and misunderstandings are particularly common in medications unrelated to the primary diagnosis. Efforts to improve medication reconciliation and patient understanding should not be disease-specific, but should be focused on the whole patient.
KEY WORDS: quality of care, acute coronary syndrome, heart failure, pneumonia, discharge instructions, medication reconciliation, adverse drug events, adverse events, patient education
BACKGROUND
An appropriate medication regimen after hospital discharge is an essential component of safe and effective care following hospitalization. Yet, adverse drug events post-discharge are exceedingly common. One study estimated that 12.5 % of patients suffered adverse drug events within 30 days of discharge, of which 62 % were preventable or ameliorable.1 These preventable adverse events may be attributable to two primary factors: provider error and patient misunderstanding.
The primary means of avoiding provider errors in medication regimens is accurate medication reconciliation. Medication reconciliation accuracy has been studied at various transition points. On admission, medication reconciliation is prone to error with an estimated 67 % of medication histories being inaccurate, thereby contributing to 27 % of inpatient provider errors.2 Inpatient transfers between units are an additional source of risk for medication provider errors, with one study identifying 62 % of inpatient transfers as having at least one unintentional medication error; these errors were most often medication omissions.3 A further set of errors can be made at the time of hospital discharge.4–10 Errors include unintentional discontinuation of medication on discharge,4–7 inappropriate retention of inpatient medications on discharge,7,8 and inaccurate changes in dosing or frequency. Medication reconciliation inaccuracies accumulating at all these points of transition create substantial risk for medication errors on hospital discharge. For example, an observational study in Ireland found that 50 % of discharge medication reconciliations during 1,245 hospitalizations were inaccurate, involving 16 % of all medications prescribed.10
Equally important is patient understanding of the discharge medication regimen, particularly given that nearly half of all home medications regimens are modified via changes in dose, discontinuation, or new prescriptions after hospitalization.10,11 A 1999 study of 342 patients found that 54 % had inadequate knowledge of their medications 1 week after discharge;12 other smaller studies show similar results.13–17 Nonetheless, physicians grossly overestimate patient understanding.15
No study has simultaneously evaluated medication reconciliation accuracy and patient understanding to form a comprehensive view of medication problems associated with hospitalization. The goal of the DIagnosing Systemic failures, Complexities and HARm in GEriatric discharges study (DISCHARGE) was to comprehensively assess the discharge process for older patients discharged to the community. Here, we describe both discharge medication reconciliation accuracy and patient understanding of discharge lists for patients in the DISCHARGE study, in order to understand their collective impact on medication safety after hospital discharge.
METHODS
Patients
The DISCHARGE study was a prospective, observational cohort study of patients 65 years or older discharged to home from a medicine service at Yale-New Haven Hospital (a 966-bed urban facility), who were admitted with symptoms consistent with acute coronary syndrome, heart failure, or pneumonia. Physicians screened new admissions for eligibility within 24 h of admission. Reviewers confirmed diagnoses of acute coronary syndrome, heart failure, and pneumonia using specialty society guidelines.18–21 Additional inclusion criteria included speaking English or Spanish, not being enrolled in hospice care, and ability of the patient or caregiver to participate in a telephone interview. Patients were consented over the telephone within a week of hospital discharge. Patients were ineligible to participate if they failed the mini-COG mental status screen22 while in the hospital or appeared confused or delirious during the telephone interview. Caregivers of patients who did not manage their own medications could participate in lieu of patients if informed consent was granted by the patient.
The study was approved by the Yale Human Investigation Committee. Verbal informed consent was obtained from all patients or caregivers, including separate consent to access medical records. Patient medical records and databases for this study were guarded per Health Insurance Portability and Accountability Act (HIPAA) guidelines.
Medication Reconciliation Process
The hospital uses Sunrise Clinical Manager 5.8 (Eclipsys Corporation, Atlanta, GA) for its electronic medical records system. Discharge instructions and reconciliations are generated electronically for all patients; however, there is no active electronic medication reconciliation process. The admitting physician documents the admission medication list in a handwritten or electronic note. The discharging physician writes medications intended for discharge through a prescription writer module that is integrated into the discharge instructions template. Pharmacists do not systematically review discharge medication lists by prior to discharge. Nurses at our site are instructed to read the discharge instructions line by line together with patients at discharge. Nurses are encouraged to refer any issues with the discharge instructions to the discharging physician. There was no formal teach-back process in place at the time of this study.
Data Collection
Patients underwent a structured, standardized telephone interview by trained non-medical personnel within 1 week of discharge. Patients were asked if any modifications were made to their admission medication regimen, i.e., if doses or frequencies were changed or medications were stopped, or if any new medications were added. When relevant, patients were asked the name of and new regimen for changed medications, the name of stopped medications, and the name and frequency of new medications. Patients were free to consult their discharge instructions to answer interview questions. Interviewers did not have access to patients’ medical records during the telephone interviews.
Admission medication lists were abstracted by trained nurse abstractors from the emergency department record and admission history and physical. Discharge medication lists were abstracted from the discharge instruction sheets signed by the patient.
Outcome Measures
This analysis included two primary outcomes: medication reconciliation accuracy and patient understanding. Medication reconciliation accuracy was determined by comparing the discharge medication list to the admission medication list. The discharge medication list was identified from the patient’s copy of the discharge instructions, as well as the post-discharge patient interview. The admission medication list was defined as that indicated in the emergency room record or the admission history and physical. For each patient, all changes in dose or frequency (“redosed” medications), omissions (“stopped” medications) and additions (new medications) between admission and discharge were identified. A physician investigator (B.Z.) performed a chart review for every patient with any redosed or stopped medication (collectively referred to as a “medication modification”). Any medication modification that did not appear to be intended based on review of the medical record was classified as a suspected provider error. We did not assess new medications for accuracy or appropriateness. Examples of suspected provider errors include: switching a home medication to a drug of a similar class on discharge without clear indication (commonly for hospital formulary reasons), medication dosing that differed from intent noted in chart, discontinuation of a home medication without clinical indication or documented indication of intent to do so, and continuation of a medication on discharge that was noted in chart documentation and in patient interviews as intended to be stopped. Medication changes or discontinuations noted only by patients but not confirmed on chart review were categorized as patient misunderstanding rather than provider errors. These potential changes were not included in the analysis of patient understanding, which included only medication changes confirmed by the medical record.
Patient understanding of medication modifications was classified as full, partial or absent, based on concordance between the post-discharge interview and the hospital discharge medication list. Definitions of full, partial and absent understanding were developed for each type of medication modification (Table 1). One physician reviewer (B.Z.) who had full access to the medical charts scored patient understanding of each medication modification and each new medication. Patient understanding was not rated for medication modifications classified as suspected provider errors.
Table 1.
Definition of Patient Understanding of Medication Modifications
| Type of medication modification | Full understanding | Partial understanding | Absent understanding** |
|---|---|---|---|
| New medication | Name and frequency correct | Class of drug only or frequency of drug only | Medication not identified at all or criteria for partial understanding not met |
| Redosed medication | Name and change (dose or frequency) correct | Name only, change not named or incorrect* | Medication not identified at all or criteria for partial understanding not met |
| Stopped medication | Name correct | Class correct or different medication in same class named | Medication not identified at all or criteria for partial understanding not met |
*Credit for partial understanding was given for direction of change (higher or lower dose) for antihypertensives, diuretics or warfarin
**Patients naming medications that were not modified at all were classified as naming an unmodified medication
Main Explanatory Variable and Key Covariates
For the study’s main explanatory variable, we classified each medication as being relevant or non-relevant to acute coronary syndrome, heart failure or pneumonia. Medications relevant to the diagnosis of acute coronary syndrome included: antiaggregants, diuretics, lipid lowering agents, anti-hypertensives and antiarrhythmics. Medications relevant to heart failure included all ACS-relevant medications in addition to potassium supplements. Medications relevant to diagnosis of pneumonia were antibiotics. The following classes of medication were excluded from all analyses: vitamin supplements, as needed medications, ophthalmic medications, lozenges, allergy medications (including nasal sprays), all topical medications and non-opiate/non-benzodiazepine sleep aids.
Key clinical covariates included diagnosis, medical team (hospitalist, house staff or cardiology), comorbidity (defined as the van Walraven score of Elixhauser comorbidities23), length of stay, total number of medications, and being able to identify a usual source of care; sociodemographic covariates included age, gender, race, and education.
Statistical Analysis
Descriptive statistics are reported as counts and percentages for categorical variables and means and standard deviations for continuous variables. Suspected provider error and patient misunderstanding outcome scores were summed across all medications and percentages reported across total medications modified. Multivariable logistic regression models used robust variance estimators in a generalized estimating equations context to account for the clustering of medications within individuals. For the ordinal patient misunderstanding outcome, a proportional odds model was used. Proportional odds models are used in some cases where there are more than two levels to the categorical outcome measure. The reported odds ratio can be interpreted as the effect of the explanatory variable on the odds of having less rather than more understanding, for any dichotomization of the outcome. The extent and nature of missing data was assessed as part of the model fitting process; model fit was assessed with goodness-of-fit statistics, residual analysis and diagnostic statistics, as available. Abstracted data and compiled physician reviewer classifications were analyzed using SAS 9.2 (SAS Institute, Cary, NC). P-values less than 0.05 were interpreted as statistically significant for two-sided tests.
RESULTS
Enrollment and Study Sample
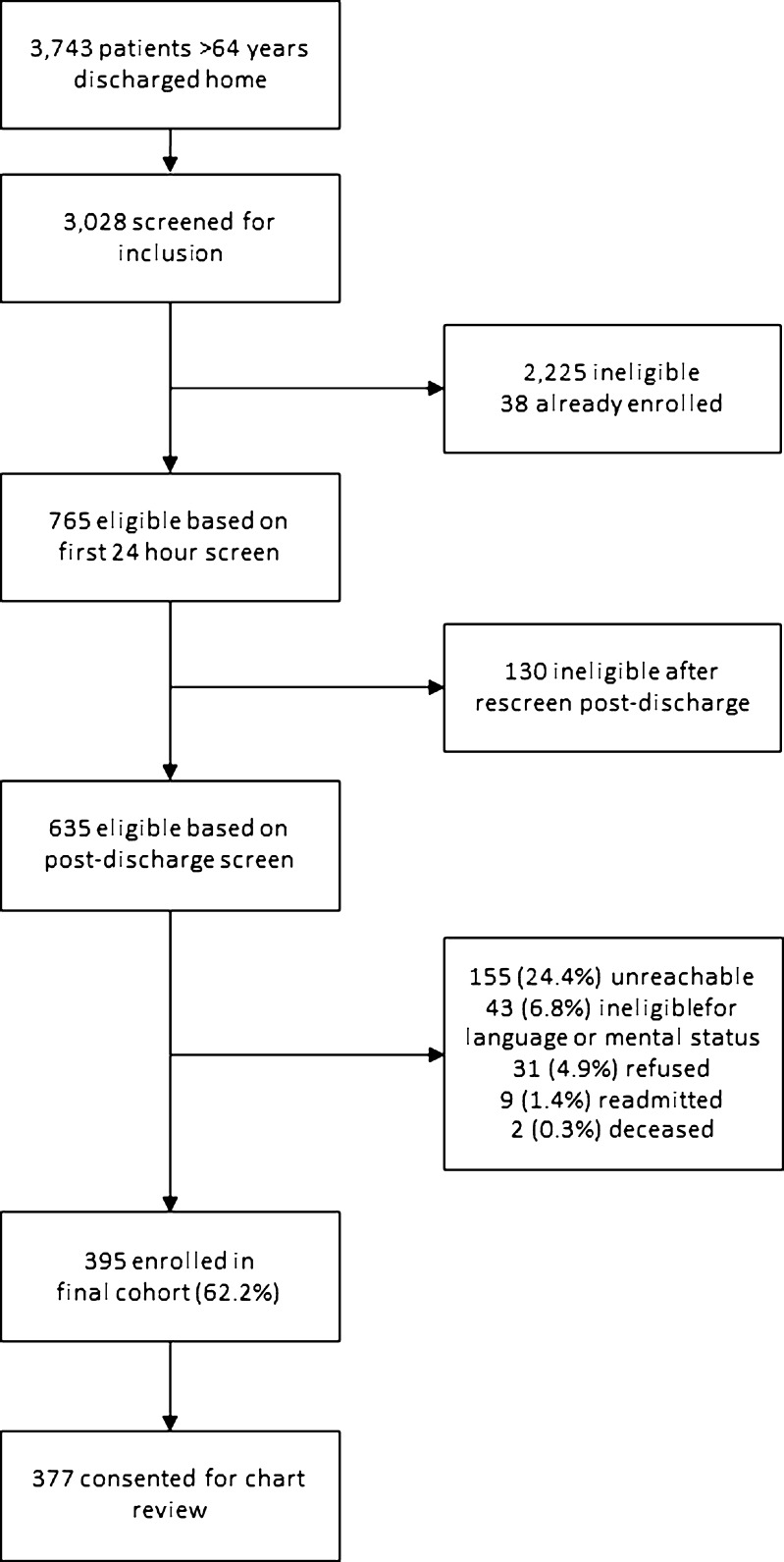
A total of 3,743 patients over 64 years of age were discharged home from the medical service at YNHH during the study period; 3,028 were screened for eligibility within 24 h of admission. Early screening identified 765 as eligible. However, rescreening after discharge revealed that 130 patients were no longer eligible. This left 635 eligible admissions, of which 395 (62.2 %) were enrolled in the study and completed the first post-discharge interview. Of these, 377 granted permission for chart review and were included in this analysis. See Figure 1.
Figure 1.
Flow diagram of enrolled participants.
The study sample had a mean age of 77.1 years (standard deviation 7.8); 205 (54.4 %) were male and 310 (82.4 %) were non-Hispanic white. 195 (51.7 %) had acute coronary syndrome, 146 (38.7 %) had heart failure, and 91 (24.1 %) had pneumonia. 54 (14.3 %) patients had more than one qualifying condition. 114 (30.2 %) were cared for by hospitalist teams, 123 (32.6 %) were cared for by service attending and house staff teams, and 140 (37.1 %) were cared for by physician assistants under the supervision of cardiologists. See Table 2.
Table 2.
Characteristics of Study Cohort, N = 377
| Characteristic | N (%) or mean (SD) |
|---|---|
| Condition | |
| Acute coronary syndrome | 195 (51.7) |
| Heart failure | 146 (38.7) |
| Community-acquired pneumonia | 91 (24.1) |
| Medical team | |
| Hospitalist team | 114 (30.2) |
| House staff | 123 (32.6) |
| Cardiology | 140 (37.1) |
| Length of stay, mean days | 3.5 (2.5) |
| Total number of medications, mean | 8.9 (3.3) |
| Total number of Elixhauser comorbidities, mean | 3.3 (1.8) |
| Identify a usual source of care | 360 (95.5) |
| Age, mean years | 77.1 (7.8) |
| Male | 205 (54.4) |
| English-speaking* | 366 (98.1) |
| Race/ethnicity† | |
| Non-Hispanic white | 310 (82.4) |
| Non-Hispanic black | 44 (11.7) |
| Hispanic | 15 (4.0) |
| Other | 7 (1.9) |
| High School Graduate or GED‡ | 268 (73.4) |
| Admission source† | |
| Emergency department | 248 (66.0) |
| Direct transfer from hospital or nursing facility | 94 (25.0) |
| Direct admission from office | 34 (9.0) |
N number of study participants; SD standard deviation
*Four missing values
†One missing value
‡Twelve missing values
Medication Changes
In total, the 377 patients in the study cohort were prescribed 2,534 medications on admission, of which 263 (10.4 %) were redosed and 302 (11.9 %) were stopped on discharge. Additionally, patients were prescribed 804 new medications at discharge. Of the 3,338 prescribed medications, 1,962 (58.8 %) were classified as relevant to the main diagnosis of heart failure, pneumonia or acute coronary syndrome. Of the 565 medications that were redosed or stopped, 380 (67.3 %) were relevant and 185 (32.7 %) were not relevant to the main diagnosis.
The mean number of prescriptions per patient on discharge was 8.0 (SD 3.1). A total of 329 (87.3 %) patients received at least one new prescription; of patients receiving new medications, the mean number of new prescriptions per patient was 2.4 (SD 1.6). A total of 263 (69.7 %) of patients had at least one medication modification: 182 (48.3 %) had a medication redosed and 171 (45.4 %) had a medication stopped. Of patients who had a medication redosed, the mean number of redosed medications per patient was 1.4 (0.8). Of patients who had a medication stopped, the mean number of stopped medications per patient was 1.8 (1.1).
Medication Reconciliation Accuracy
Of all 565 modified medications, 428 (75.8 %) appeared to be clinically appropriate or justified by documentation in the chart. The remaining 137 (24.2 %) modifications were classified as suspected provider errors (5.4 % of admission medications). New medications are not included in these analyses. A total of 103 of 377 patients (27.3 %) experienced at least one provider error; these 103 patients constituted 39.2 % of the 263 patients with redosed or stopped medications. Suspected errors were made in 61/380 (16.1 %) of medications relevant to the primary diagnosis and in 76/185 (41 %) of medications not relevant to the primary diagnosis. Suspected errors were made in 65/293 (22.2 %) of medications given to patients with acute coronary syndrome, 59/249 (23.7 %) of medications given to patients with heart failure, and 25/100 (25.0 %) of medications given to patients with pneumonia. Suspected errors were made in 42/148 (28.4 %) of medications given to patients on hospitalist teams, 48/225 (21.3 %) of medications given to patients on house staff teams, and 47/192 (24.5 %) of medications given to patients on cardiology teams.
In a multivariable logistic regression model, non-relevant medications were significantly associated with suspected provider errors (odds ratio (OR) 4.56, 95 % confidence interval (CI) 2.65, 7.85, p < 0.001). The amount of missing data was small and model fit was satisfactory; complete case, full model results are reported (Table 3).
Table 3.
Multivariable Logistic Regression Results of Suspected Provider Errors, N = 546
| Predictor | Odds ratio (95 % CI) | P value* |
|---|---|---|
| Non-relevant medication | 4.56 (2.65, 7.85) | <0.001 |
| Medical team | ||
| Hospitalist | 1.00 | 0.39 |
| House staff | 1.35 (0.74, 2.46) | |
| Cardiology | 0.91 (0.52, 1.58) | |
| Acute coronary syndrome | 0.76 (0.32, 1.81) | 0.54 |
| Heart failure | 0.73 (0.29, 1.79) | 0.47 |
| Pneumonia | 0.33 (0.12, 0.93) | 0.02 |
| Redosed medication | 0.92 (0.57, 1.48) | 0.74 |
| Total number of medications | 1.00 (0.92, 1.07) | 0.91 |
| Length of stay (in days) | 0.91 (0.84, 0.99) | 0.03 |
| Age (in years) | 1.01 (0.98, 1.04) | 0.71 |
| Male | 0.99 (0.62, 1.59) | 0.97 |
| Non-Hispanic white | 0.93 (0.52, 1.68) | 0.83 |
| High school education or higher | 1.14 (0.64, 2.04) | 0.66 |
| Comorbidity score | 1.00 (0.97–1.04) | 0.94 |
*From score statistics for type 3 GEE analysis
Patient Understanding
After excluding suspected provider errors, patients fully understood 33/205 (16.1 %) of the redosed medications, 35/223 (15.7 %) of the stopped medications, and 248/795 (31.2 %) of the new medications. Conversely, patients had no understanding of 142/205 (69.3 %) of redosed medications, 182/223 (81.6 %) of stopped medications, and 493 (62.0 %) of new medications.
From the patient perspective, 178/225 patients (79.1 %) who had an intended medication change (stopped or redosed medication) had no understanding of at least one change. A total of 142/225 (63.1 %) had no understanding of all intended medication changes. Of the 329 patients who received new medications, 232 (70.5 %) had no understanding of at least one new medication. A total of 154/329 (46.8 %) patients had no understanding of all new medications. The average patient had no understanding of 60.0 % of all stopped, redosed and new medications.
Patients fully understood 281/908 (30.9 %) of relevant new or modified medications and only 35/315 (11.1 %) of non-relevant new or modified medications. They had no understanding of 556/908 (61.2 %) of relevant new or modified medications and 261/315 (82.9 %) of non-relevant new or modified medications. Patients with acute coronary syndrome fully understood 241/677 (35.6 %) of new or modified medications, those with heart failure fully understood 88/488 (18.0 %), and those with pneumonia fully understood 29/274 (10.6 %).
In a multivariable proportional odds model, non-relevance of the medication to the primary diagnosis was the only variable significantly associated with patient misunderstanding. Patients were significantly more likely to misunderstand changes to non-relevant medications than to relevant medications (OR 2.45, 95 % CI 1.68, 3.55), p < 0.001). The amount of missing data was small and model fit was satisfactory; complete case, full model results are reported (Table 4).
Table 4.
Multivariable Proportional Odds Model Results of Patient Misunderstanding, N = 1,180
| Predictor | Odds ratio (95 % CI) | P value* |
|---|---|---|
| Non-relevant medication | 2.45 (1.68, 3.55) | <0.001 |
| Medical team | ||
| Hospitalist | 1.00 | 0.38 |
| House staff | 1.37 (0.81, 2.33) | |
| Cardiology | 1.02 (0.65, 1.60) | |
| Acute coronary syndrome | 0.73 (0.42, 1.28) | 0.27 |
| Heart failure | 1.47 (0.84, 2.58) | 0.17 |
| Pneumonia | 1.13 (0.60, 2.14) | 0.69 |
| Total number of medications | 1.02 (0.96, 1.09) | 0.47 |
| Length of stay (in days) | 1.06 (0.97, 1.15) | 0.18 |
| Age (in years) | 1.00 (0.97, 1.02) | 0.95 |
| Male | 1.27 (0.86, 1.87) | 0.23 |
| Non-Hispanic white | 0.72 (0.46, 1.12) | 0.15 |
| High school education or higher | 0.81 (0.52, 1.25) | 0.32 |
| Comorbidity score | 1.01 (0.98–1.04) | 0.67 |
*From score statistics for type 3 GEE analysis
In terms of the number of patients affected by both provider errors and poor understanding, 307 patients (81.4 %) had either a provider error or no understanding of at least one intended medication change. Furthermore, 84 patients (22.3 %) had both a provider error and no understanding of at least one intended medication change.
DISCUSSION
In the DISCHARGE study, we found that a quarter of all medication changes on hospital discharge were likely unintended errors, affecting more than a quarter of discharged patients. Furthermore, patients had no understanding of two thirds of intended medication changes or new medications. Together, these results indicate a very high potential for adverse medication events following hospital discharge, and suggest that efforts to reduce post-discharge medication adverse events must involve both providers and patients.
By far the most significant predictor of both discharge list accuracy and patient understanding was the relevance of the medication to the primary diagnosis. Relevant medications were more often accurate on the discharge medication list compared to non-relevant medications, and changes to relevant medications were more often understood by patients. This is clinically reasonable, as both clinicians and patients are likely to pay more attention to medications relating to the main reason for hospitalization than to other chronic conditions. From a patient safety perspective, however, inattention to secondary conditions can have important consequences. The majority of patients who are readmitted to the hospital post-discharge are readmitted for a different condition than the index diagnosis.24 Such readmissions are often thought to be non-preventable. Yet, our findings suggest that both errors and misunderstandings about chronic conditions may be generated during the index admission, potentially contributing to rehospitalizations for those conditions.
The rate of provider errors in this study is similar to other studies, although this study was more comprehensive than most in including errors in dosing and frequency, omissions, and inadvertent continuations.4–10 There was no difference in error rates between patients cared for by hospitalists or cardiology attendings and those cared for by house staff, suggesting that clinical experience and expertise are not adequate protections against medication errors at discharge. By contrast, a recent study of an electronic medication reconciliation intervention demonstrated a reduction in provider errors.25 Our hospital’s electronic records system for discharge instructions does not provide a formal reconciliation process for admission home medications, inpatient orders, and anticipated discharged medications. It is therefore possible that systems factors such as information technology play a larger role in transition-related medication errors than provider factors such as level of training or expertise. Efforts to improve medication reconciliation accuracy should take these findings into account.
Patient understanding of intended medication changes at discharge was very poor, and may be worse than in other studies. For example, other studies report at least some understanding of new medications among 64–68 % of patients;16,17,25 the corresponding rate in our study was 53.2 %. These low rates of understanding existed despite the fact that we allowed patients to consult discharge instructions or other documentation in answering the survey, excluded clearly cognitively impaired patients, and excluded medication changes that were potential provider errors. It is possible that our lower rates of comprehension result from restriction of the study to an older population taking a relatively large number of medications. It is also possible that time for patient education has diminished as length of stay has dropped.
Our study included several limitations. Our assessment of medication reconciliation accuracy was limited to chart review, and treated the admission medication list as the gold standard. Numerous studies have demonstrated high rates of errors in admission medication lists.2 Therefore, the true rate of medication errors at discharge compared to patients’ pre-admission medication regimen is likely higher. On the other hand, we were not able to communicate with hospital providers directly regarding suspected provider errors, and it is therefore possible that some changes we categorized as likely errors were actually intentional. We made no attempt to determine whether prescribed medications were appropriate, and we did not consider whether all appropriate medications were prescribed in this study; therefore, again this study likely underestimates medication errors. There were an insufficient number of readmitted patients in this study for us to determine whether patient misunderstanding or medication reconciliation errors contributed to readmissions. Finally, this study was restricted to older patients with three common diseases at one hospital, and may not be generalizable to the hospital population at large.
As hospital stays have been shortened and the involvement of outpatient providers in inpatient hospitalizations has dropped, accurate medication reconciliation and comprehensive patient education have become ever more important. Unfortunately, our study suggests that medication errors and misunderstandings at hospital discharge remain substantial, particularly for medications not relevant to the primary diagnosis. Together, these errors and misunderstandings place patients at increased risk of adverse medication events post-discharge. Efforts to improve patient education and medication reconciliation accuracy upon discharge should include a focus on the full medication list, not only medications relevant to the primary diagnosis.
Acknowledgments
Contributors
The authors would like to acknowledge Amy Browning and the staff of the Center for Outcomes Research and Evaluation Follow Up Center for conducting patient interviews, Mark Abroms and Katherine Herman for patient recruitment and screening, Peter Charpentier for website development, and the other members of the DISCHARGE study team: Ursula Brewster, MD, Christine Chen, MD, Grace Y. Jenq, MD, Sandhya Kanade, MD, Harlan M. Krumholz, MD, and John P. Moriarty, MD.
Funders
At the time this study was conducted, Dr. Horwitz was supported by the CTSA Grant UL1 RR024139 and KL2 RR024138 from the National Center for Advancing Translational Sciences (NCATS), a component of the National Institutes of Health (NIH), and NIH roadmap for Medical Research, and was a Centers of Excellence Scholar in Geriatric Medicine by The John A. Hartford Foundation and the American Federation for Aging Research. Dr. Horwitz is now supported by the National Institute on Aging (K08 AG038336) and by the American Federation for Aging Research through the Paul B. Beeson Career Development Award Program. This work was also supported by a grant from the Claude D. Pepper Older Americans Independence Center at Yale University School of Medicine (P30AG021342 NIH/NIA).
Prior Presentations
An earlier version of this work was presented as a poster at the American College of Cardiology 60th Annual Meeting in New Orleans, LA in April, 2011.
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Author Contributions
Dr. Horwitz had full access to all of the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Horwitz. Acquisition of data: Ziaeian. Analysis and interpretation of data: Ziaeian, Araujo, Van Ness, Horwitz. Drafting of the manuscript: Ziaeian and Horwitz. Critical revision of the manuscript for important intellectual content: Araujo and Van Ness. Approval of final manuscript for submission: Ziaeian, Araujo, Van Ness, Horwitz. Statistical analysis: Van Ness. Study supervision: Horwitz.
Financial Disclosure
None reported.
REFERENCES
- 1.Forster AJ, Murff HJ, Peterson JF, Gandhi TK, Bates DW. The incidence and severity of adverse events affecting patients after discharge from the hospital. Ann Intern Med. 2003;138(3):161–7. doi: 10.7326/0003-4819-138-3-200302040-00007. [DOI] [PubMed] [Google Scholar]
- 2.Tam VC, Knowles SR, Cornish PL, Fine N, Marchesano R, Etchells EE. Frequency, type and clinical importance of medication history errors at admission to hospital: a systematic review. Can Med Assoc J. 2005;173(5):510–5. doi: 10.1503/cmaj.045311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee JY, Leblanc K, Fernandes OA, et al. Medication reconciliation during internal hospital transfer and impact of computerized prescriber order entry. Ann Pharmacother. 2010;44(21098753):1887–95. doi: 10.1345/aph.1P314. [DOI] [PubMed] [Google Scholar]
- 4.Bell CM. Unintentional discontinuation of long-term medications for chronic diseases after hospitalization. Healthc Q. 2007;10(2):26–8. doi: 10.12927/hcq..18817. [DOI] [PubMed] [Google Scholar]
- 5.Bell CM, Brener SS, Gunraj N, et al. Association of ICU or hospital admission with unintentional discontinuation of medications for chronic diseases. JAMA. 2011;306(8):840–7. doi: 10.1001/jama.2011.1206. [DOI] [PubMed] [Google Scholar]
- 6.Bell CM, Rahimi-Darabad P, Orner AI. Discontinuity of chronic medications in patients discharged from the intensive care unit. J Gen Intern Med. 2006;21(9):937–41. doi: 10.1007/BF02743141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perren A, Previsdomini M, Cerutti B, Soldini D, Donghi D, Marone C. Omitted and unjustified medications in the discharge summary. Qual Saf Health Care. 2009;18(3):205–8. doi: 10.1136/qshc.2007.024588. [DOI] [PubMed] [Google Scholar]
- 8.Wohlt PD, Hansen LA, Fish JT. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmacother. 2007;41(10):1611–6. doi: 10.1345/aph.1K227. [DOI] [PubMed] [Google Scholar]
- 9.McMillan TE, Allan W, Black PN. Accuracy of information on medicines in hospital discharge summaries. Intern Med J. 2006;36(4):221–5. doi: 10.1111/j.1445-5994.2006.01028.x. [DOI] [PubMed] [Google Scholar]
- 10.Grimes TC, Duggan CA, Delaney TP, et al. Medication details documented on hospital discharge: cross-sectional observational study of factors associated with medication non-reconciliation. Br J Clin Pharmacol. 2011;71(21284705):449–57. doi: 10.1111/j.1365-2125.2010.03834.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Himmel W, Tabache M, Kochen MM. What happens to long-term medication when general practice patients are referred to hospital? Eur J Clin Pharmacol. 1996;50(8803514):253–7. doi: 10.1007/s002280050103. [DOI] [PubMed] [Google Scholar]
- 12.Stewart S, Pearson S. Uncovering a multitude of sins: medication management in the home post acute hospitalisation among the chronically ill. Aust N Z J Med. 1999;29(2):220–7. doi: 10.1111/j.1445-5994.1999.tb00687.x. [DOI] [PubMed] [Google Scholar]
- 13.Makaryus AN, Friedman EA. Patients’ understanding of their treatment plans and diagnosis at discharge. Mayo Clin Proc. 2005;80(16092576):991–4. doi: 10.4065/80.8.991. [DOI] [PubMed] [Google Scholar]
- 14.Holloway A. Patient knowledge and information concerning medication on discharge from hospital. J Adv Nurs. 1996;24(6):1169–74. doi: 10.1111/j.1365-2648.1996.tb01022.x. [DOI] [PubMed] [Google Scholar]
- 15.Calkins DR, Davis RB, Reiley P, et al. Patient–physician communication at hospital discharge and patients’ understanding of the postdischarge treatment plan. Arch Intern Med. 1997;157(9):1026–30. doi: 10.1001/archinte.1997.00440300148014. [DOI] [PubMed] [Google Scholar]
- 16.Kerzman H, Baron-Epel O, Toren O. What do discharged patients know about their medication? Patient Educ Couns. 2005;56(3):276–82. doi: 10.1016/j.pec.2004.02.019. [DOI] [PubMed] [Google Scholar]
- 17.Maniaci MJ, Heckman MG, Dawson NL. Functional health literacy and understanding of medications at discharge. Mayo Clin Proc. 2008;83(5):554–8. doi: 10.4065/83.5.554. [DOI] [PubMed] [Google Scholar]
- 18.Anderson JL, Adams CD, Antman EM, et al. ACC/AHA 2007 Guidelines for the Management of Patients with Unstable Angina/Non-ST-Elevation Myocardial Infarction: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non-ST-Elevation Myocardial Infarction) developed in collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine. J Am Coll Cardiol. 2007;50(7):e1–157. doi: 10.1016/j.jacc.2007.02.013. [DOI] [PubMed] [Google Scholar]
- 19.Thygesen K, Alpert JS, White HD, Joint ESCAAHAWHFTFftRoMI Universal definition of myocardial infarction. Eur Hear J. 2007;28(20):2525–38. doi: 10.1093/eurheartj/ehm355. [DOI] [PubMed] [Google Scholar]
- 20.Dickstein K, Cohen-Solal A, Filippatos G, et al. ESC guidelines for the diagnosis and treatment of acute and chronic heart failure 2008: the Task Force for the diagnosis and treatment of acute and chronic heart failure 2008 of the European Society of Cardiology. Developed in collaboration with the Heart Failure Association of the ESC (HFA) and endorsed by the European Society of Intensive Care Medicine (ESICM) Eur J Hear Fail. 2008;10(10):933–89. doi: 10.1016/j.ejheart.2008.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Mandell LA, Wunderink RG, Anzueto A, et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis. 2007;44(Suppl 2(17278083)):27–72. doi: 10.1086/511159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sunderland T, Hill JL, Mellow AM, et al. Clock drawing in Alzheimer’s disease. A novel measure of dementia severity. J Am Geriatr Soc. 1989;37(8):725–9. doi: 10.1111/j.1532-5415.1989.tb02233.x. [DOI] [PubMed] [Google Scholar]
- 23.Walraven C, Austin PC, Jennings A, Quan H, Forster AJ. A modification of the Elixhauser comorbidity measures into a point system for hospital death using administrative data. Med Care. 2009;47(6):626–33. doi: 10.1097/MLR.0b013e31819432e5. [DOI] [PubMed] [Google Scholar]
- 24.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360(14):1418–28. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 25.Schnipper JL, Hamann C, Ndumele CD, et al. Effect of an electronic medication reconciliation application and process redesign on potential adverse drug events: a cluster-randomized trial. Arch Intern Med. 2009;169(8):771–80. doi: 10.1001/archinternmed.2009.51. [DOI] [PubMed] [Google Scholar]