Abstract
United States health expenditures continue to escalate at unsustainable rates. A recent movement around increasing price transparency has been suggested as a way of reducing the rate of increase in expenditures, with legislative efforts taking place at both the state and federal level. While this seems on the surface like a good idea, simply providing information on prices to physicians, particularly trainees, may not achieve the type of large changes in practice patterns that proponents expect. The manner in which price transparency is implemented will likely play a significant role in its effectiveness as an intervention. In this article, the authors review efforts of transparency and default options from other contexts and leverage insights from behavioral economics to provide recommendations for increasing the likelihood that price transparency will lead to physicians weighing the relative value of interventions.
KEY WORDS: health-care costs, health-care value, restaurant food labeling, asymmetric paternalism, nudges
INTRODUCTION
United States health expenditures continue to escalate and are expected to exceed $2.8 trillion by 2012.1 One suggestion for improvement centers largely on increasing price transparency in health care, with legislative actions taking place at both the state and federal level.2 These efforts are in hopes of improving health-care value, or the benefits attained for a given amount of health expenditures, by reducing unnecessary spending through changes in physician behavior. While simply providing the price of tests and treatments may have some impact in encouraging physicians to weigh the relative value of different diagnostic or treatment options, providing this information alone will likely have a limited impact. The precise manner and context in which price transparency is implemented will likely play a large role in the effectiveness of this initiative to increase the likelihood that physicians will weigh the relative value of treatments in their decision making.
The pricing of tests and treatments is based on a variety of market forces and other factors that are largely invisible to providers that are ordering these interventions3,4 and most physicians practice medicine with limited knowledge of the price of the services they provide.4,5 Several studies have demonstrated that providing pricing information on diagnostic tests can change physician behavior by reducing the number of tests that are ordered.6–9 Efforts to increase price transparency for physicians are intended to increase cost consciousness.2 For example, if a physician wants to prescribe a medication, he or she might select among one of several brand name formulations with available generic alternatives. While brand and generic formulations are equally effective, the associated costs can vary considerably. In fact, in 2009, Medicaid spent an excess of $329 million on brand name medications that had existing generic alternatives.10 However, simply displaying the price in isolation of a therapy when it is ordered will not ensure that physicians will choose equally effective, lower cost alternatives since the relative prices of alternatives may not be salient to physicians. The question of how to provide such information is particularly relevant in the setting of teaching hospitals, in which trainees do much of the ordering and where habitual patterns may affect not only current but also future medical decision making. There is evidence that internal medicine residents in academic settings have poor knowledge of the associated charges related to commonly ordered tests, but are eager to learn this information for weighing medical decisions.11
Medical decision making is influenced by several contextual factors including issues related to the salience of information on benefits, risks, and costs; relevant alternatives; financial incentives; and social dynamics. Price transparency is intended to encourage physicians to weigh the value of diagnostic tests and treatments. For insights into how this could be done more versus less effectively, we describe findings related to two different literatures: (1) the provision of information of calories in restaurant chains, a major initiative that has expanded nationally as part of the Affordable Care Act; (2) the provision of information relating to retirement savings, which has been a highly successful application of insights from behavioral economics.
LESSONS FROM FOOD LABELING AND RETIREMENT SAVINGS
The intent behind displaying calorie information on menus has been to reduce obesity by making consumers more conscious of calories, particularly in fast food restaurants. While this may seem to be far afield from the impact of price transparency on physician behavior, there are a number of lessons that are informative for health policy initiatives. Despite the intuitive appeal of providing consumers with information at fast food chain restaurants as a way of making them more aware of the caloric content of different food items, studies to date have generally failed to show significant reductions in calorie consumption from these initiatives.12–14 There are several potential reasons why these efforts had little impact. First, consumers may not understand what the numbers of calories mean. Second, they may not know what an appropriate daily calorie target is. Third, low income people, in whom rates of obesity are higher, may deliberately choose higher calorie items because it provides them with more energy per dollar spent.15
Asymmetric or libertarian paternalism is an approach to public policy that applies principles of behavioral economics to help individuals achieve their goals.16 Interventions that apply these efforts have been described as “nudges,” for they can help people who are making suboptimal decisions behave more optimally without affecting those who are already behaving optimally.17 Suggestions for improvements in designing food labeling in restaurants have included making caloric information more understandable, framing information in a more meaningful way to consumers, and setting defaults to favor healthy food choices.15 Changing the defaults (specifically ordering of menu items based on caloric content) has been tested and found to be more effective in reducing caloric consumption than simply displaying caloric information.18,19 “Opt in” vs. “opt out” defaults have also been found in other contexts, such as organ donation, to be associated with dramatic differences in the uptake of the desired behavior.20
Retirement savings programs nationally have been transformed through changes in defaults. In 2001 a seminal study was published that showed that when the default employee contribution to 401(k) plans was 0 %, the majority of employees did not contribute to their retirement savings, despite its importance. In contrast, when the default was changed an automatic enrollment with a 3 % contribution, almost all employees chose to save at least 3 % for retirement.21 Subsequent work has shown that providing employees with information or training about retirement savings has little impact on savings behavior.22 The most powerful manipulation has been switching the automatic enrollment for retirement savings from an opt in to an opt out process, which elevated participation rates from 9.9 % to 86.1 %.23 A new approach in which people are compelled to make a decision between alternatives (‘active choice’) to try to reduce objections that people sometimes may have with 'opt out' of ‘being manipulated’ or being pushed too strongly into a particular alternative often achieves rates close to that of an ‘opt out.’ Active choice makes the choice between alternatives salient at the time a decision is potentially being made to both reduce the cost of decision making and to try to minimize procrastination, positioning an individual to make a choice between alternatives that can be enhanced to highlight the relevant advantages and disadvantages of the two options.24
CHANGING DEFAULTS TO INFLUENCE PHYSICIAN DECISION MAKING
The proliferation of computerized physician order entry (CPOE) systems creates new possibilities for putting pricing information in the hands of providers at the time they make a decision. Typically, many CPOE systems use a process in which the name of the test or therapy is entered manually. This is analogous to an ‘opt in’ system when it comes to choosing lower priced treatment alternatives. While adding prices of tests might have some impact, it is likely that this will, similar to the experience described above with calorie labeling and retirement savings, not be transformative.
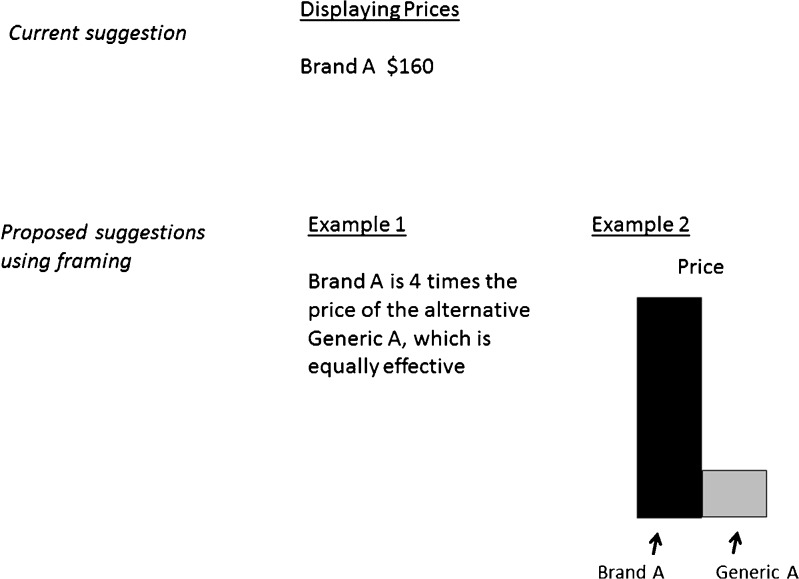
Influencing physicians to consider the value of diagnostic or treatment alternatives could be done more effectively than by simply displaying prices of each test or treatment in isolation. First, prices should be framed in ways that are easily comprehensible and where reasonable alternatives are highlighted. Instead of simply displaying the price of an intervention, the price could be graphically depicted as a multiple of the price of another less expensive, yet equally effective intervention (Fig. 1). This displays the information in relative terms in a context that provides a direct and readily apparent comparison with reasonable alternatives.
Figure 1.
Proposed examples for framing prices by leveraging insights from behavioral economics.
Second, information about the relative price of interventions could be enhanced by providing relative information on more than just price. Simply providing information about the price of a particular diagnostic test in isolation or stating that it is less expensive than another diagnostic test doesn’t help physicians (particularly trainees) to understand which one is the best to order, especially if the sensitivity and specificity of the tests vary widely. The US Preventable Services Task Force has created a grading system that helps physicians to better understand when it is recommended to conduct screening tests. Displaying similar grading systems and providing both the relative prices and ratings of different tests could help physicians to rapidly interpret this information at the time they are making ordering decisions. For many diagnostic tests, such grading systems do not yet exist. In these cases, as we work toward developing these guidelines, health systems can provide meaningful information that in the proper context can empower physicians to make better decisions. For example, when choosing among tests to diagnose a pulmonary embolism, a physician that is ordering a ventilation-perfusion could be shown the difference in sensitivity and specificity as well as cost compared to a CT scan in graphical format, along with the major contraindications for each test. The overall goal, whether a grading system or comparison of tests, is to provide the physician with evidence-based information in a manner that is meaningful and relevant to the decision at hand.
Third, using enhanced active choice to make physicians choose between higher and lower cost alternatives of similar effectiveness when ordering will likely lead to more physicians choosing the lower cost alternatives. In isolation, it is easy to order a more expensive test of similar effectiveness. However, these decisions can be structured in a way that makes more visible the cost and quality tradeoffs, e.g. “You can order test x for $1,000. Or, you can order test y for $4,000. These tests have similar sensitivity and sensitivity and risks. Click here to order the test that is more cost effective or click here to order the test that costs 4x as much but has similar benefits.”
Finally, while enhanced active choice would likely be quite effective in improving the weighing of costs and benefits in physician decision making, in cases in which there is a clearly a dominant alternative from a value standpoint, consideration should be given to moving beyond active choice to modifying electronic order entry sets such that the higher value options are set as defaults where an ‘opt out’ is possible. This will achieve the greatest likelihood of the highest value alternatives being chosen. In situations in which it is not clear what is the highest value alternative, enhanced active choice is likely the best alternative. It is also important to have a mechanism for easily opting out so that if there are special circumstances for a given patient, an alternative can easily be chosen.
An example of how CPOE systems can be helpful is in the context of a patient with their first episode of clostridium difficile, where in an ‘opt in’ system a physician would have to enter an order for either metronidazole or the more expensive vancomycin. The active choice alternative would present these two options after asking the physician the indication for therapy (e.g. clostridium difficile), highlighting that vancomycin has a success rate that is only slightly higher but much more expensive than metronidazole. The opt out alternative would present metronidazole as the default option with vancomycin as an alternative only if the physician opted out. While this approach might have some initial incremental costs for health information technology modifications, such costs would be trivial compared to the potential savings from using lower cost (and similarly effective) interventions at higher rates.
CONCLUSIONS
Providing price information at the point of ordering services is unlikely in isolation to transform physician decision making to consistently weigh the value of health-care services. Provision of relative information on the price of alternatives as well as context that helps physicians to understand an intervention’s value will be important. The proliferation of electronic order entry systems creates a opportunity nationally to use ‘active choice’ and systematic modification of defaults in computer order entry templates to have a large impact on provider decision making. Leveraging insights from other public policy initiatives around the relative effectiveness of information provision vs. defaults can help us more quickly get to a point where physicians choose higher value treatments at higher rates.
Acknowledgements
The authors have no funding sources to report.
Conflict of Interest
Dr. Mitesh Patel declares he has no conflicts of interest. He discloses being the co-founder of Docphin Inc.
Dr. Kevin Volpp declares he has no conflicts of interest.
References
- 1.National Health Expenditure Projections 2010-2020. Centers for Medicare and Medicaid. Available online at: https://www.cms.gov/NationalHealthExpendData/downloads/proj2010.pdf. Accessed February 19, 2012.
- 2.Sinaiko AD, Rosenthal MB. Increased price transparency in health care—Challenges and potential effects. N Engl J Med. 2011;364(10):891–3. doi: 10.1056/NEJMp1100041. [DOI] [PubMed] [Google Scholar]
- 3.Blumenthal D. Controlling health care expenditures. N Engl J Med. 2001;344(10):766–9. doi: 10.1056/NEJM200103083441012. [DOI] [PubMed] [Google Scholar]
- 4.Reinhardt UE. The pricing of US hospital services: chaos behind the veil of secrecy. Health Aff. 2006;25(1):57–69. doi: 10.1377/hlthaff.25.1.57. [DOI] [PubMed] [Google Scholar]
- 5.Allan GM, Lexchin J, Wiebe N. Physician awareness of drug cost: a systematic review. PLoS Med. 2007;4(9):e283. doi: 10.1371/journal.pmed.0040283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tierney WM, Miller ME, McDonald CJ. The effect of test ordering of informing physicians of the charges for outpatient diagnostic tests. N Engl J Med. 1990;322(21):1499–1504. doi: 10.1056/NEJM199005243222105. [DOI] [PubMed] [Google Scholar]
- 7.Sachdera RC, Jefferson LS, Coss-Bu J, et al. Effects of availability of patient-related charges on practice patterns and cost containment in the pediatric intensive care unit. Crit Care Med. 1996;24:501–6. doi: 10.1097/00003246-199603000-00022. [DOI] [PubMed] [Google Scholar]
- 8.Hampers LC, Cha S, Gutglass DJ, Krug SE, Binns HJ. The effect of price information on test-ordering behavior and patient outcomes in a pediatric emergency department. Pediatrics. 1997;100:128–134. doi: 10.1542/peds.100.1.128. [DOI] [PubMed] [Google Scholar]
- 9.Powell EC, Hampers LC. Physician variation in test ordering in the management of gastroenteritis in children. Arch Pediatr Adolesc Med. 2003;157:978–83. doi: 10.1001/archpedi.157.10.978. [DOI] [PubMed] [Google Scholar]
- 10.Brill A. Overspending on multisource drugs in Medicaid. American Enterprise Institute for Public Policy Research. March 28, 2011. Available online at: http://www.aei.org/papers/health/entitlements/overspending-on-multi-source-drugs-in-medicaid/. Accessed February 19, 2012.
- 11.Sehgal RT, Gorman P. Internal medicine physicians’ knowledge of health care changes. J Grad Med Educ. 2011;3(2):182–7. doi: 10.4300/JGME-D-10-00186.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bollinger B, Leslie P, Sorensen A. Calorie posting at chain restaurants. Am Econ J Econ Policy. 2011;3:91–128. doi: 10.1257/pol.3.1.91. [DOI] [Google Scholar]
- 13.Elbel B, Kersh R, Brescoll VL, Dixon LB. Calorie labeling and food choices: A first look at the effects on low-income people in New York City. Health Aff. 2009;28:w1110–w1121. doi: 10.1377/hlthaff.28.6.w1110. [DOI] [PubMed] [Google Scholar]
- 14.Harnack LJ, French SA. Effect of point-of-purchase calorie labeling on restaurant and cafeteria food choices: a review of the literature. Int J Behav Nutr Phys Act. 2008;5:51. doi: 10.1186/1479-5868-5-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Blumenthal K, Volpp KG. Enhancing the effectiveness of food labeling in restaurants. J Am Med Assoc. 2010;303(6):553–4. doi: 10.1001/jama.2010.85. [DOI] [PubMed] [Google Scholar]
- 16.Loewenstein G, Brennan T, Volpp KG. Asymmetric paternalism to improve health behaviors. J Am Med Assoc. 2007;298(20):2415–7. doi: 10.1001/jama.298.20.2415. [DOI] [PubMed] [Google Scholar]
- 17.Thaler RH, Sunstein CR. Nudge: Improving decisions about health, wealth, and happiness. New Haven, CT: Yale University Press; 2008. [Google Scholar]
- 18.Downs J, Loewenstein G, Wisdom J. Strategies for promoting healthier food choices. Am Econ Rev. 2009;2:159–64. doi: 10.1257/aer.99.2.159. [DOI] [PubMed] [Google Scholar]
- 19.Wisdom J, Downs JS, Loewenstein G. Promoting healthy choices: Information versus convenience. Am Econ J Appl Econ. 2010;2(2):164–78. doi: 10.1257/app.2.2.164. [DOI] [Google Scholar]
- 20.Johnson EJ, Goldstein DG. Do defaults save lives? Science. 2003;302:1338–9. doi: 10.1126/science.1091721. [DOI] [PubMed] [Google Scholar]
- 21.Madrian BC, Shea DF. The power of suggestion: Inertia in 401(k) participation and savings behavior. Q J Econ. 2001;4:1149–87. doi: 10.1162/003355301753265543. [DOI] [Google Scholar]
- 22.Beshears J, Choi JJ, Laibson D, Madrian BC, Weller B. “Public policy and saving for retirement: The autosave features of the pension protection act of 2006” in Better Living through Economics. Harvard University Press. 2010
- 23.Beshears J, Choi JJ, Laibson D, Madrian BC. “The importance of default options for retirement savings outcomes: Evidence from the United States” in Social Security Policy in a Changing Environment. University of Chicago Press. 2009.
- 24.Keller AP, Harlam B, Loewenstein G, Volpp KG. Enhanced active choice: A new method to motivate behavior change. J Consum Psychol. 2011;21:376–383. doi: 10.1016/j.jcps.2011.06.003. [DOI] [Google Scholar]