Abstract
Background:
Although persistent trigeminal artery (PTA) is uncommonly identified, knowledge of this structure is essential for clinicians who interpret cranial imaging, perform invasive studies of the cerebral vasculature, and operate this region.
Methods:
A review of the medical literature using standard search engines was performed to locate articles regarding the PTA, with special attention with anatomical descriptions.
Results:
Although anatomical reports of PTA anatomy are very scarce, those were analyzed to describe in detail the current knowledge about its anatomical relationships and variants. Additionally, the embryology, classification, clinical implications, and imaging modalities of this vessel are extensively discussed.
Conclusions:
Through a comprehensive review of isolated reports of the PTA, the clinician can better understand and treat patients with such an anatomical derailment.
Keywords: Carotid-basilar anastomosis, fetal intracranial artery, persistence, trigeminal artery, vascular anatomy
INTRODUCTION
The persistent trigeminal artery (PTA) was first reported at autopsy by Richard Quain in 1844 and via angiography by Sutton in 1950.[34] This artery is a rare remnant of the embryonic circulatory system that unites the proximal intracavernous segment of internal carotid artery (ICA) with the middle or distal portion of the basilar artery (BA) [Figure 1]. Sometimes, its origin could be more proximal and be misinterpreted as the otic artery, another remnant of the embryonic arterial system.[40]
Figure 1.
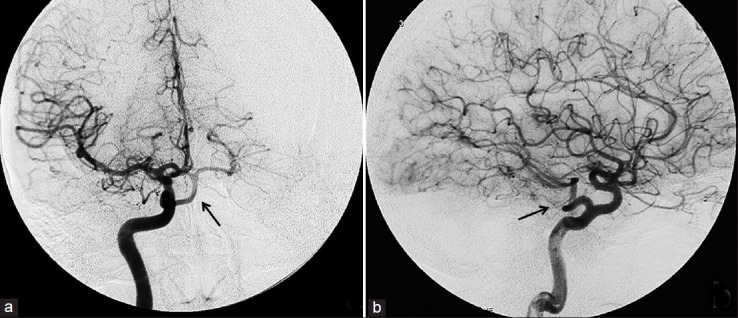
Selective right internal carotid angiography showing persistent trigeminal artery (black arrows) on anteroposterior view (a) and lateral view (b)
EMBRYOLOGICAL ASPECTS
At 28-29 days of embryonic development, the ICA can be seen supplying the forebrain, midbrain, and hindbrain.[14,40] The hypoglossal artery along the hypoglossal nerve and the proatlantal artery (first intersegmental cervical C1 artery) along the first cervical nerve are also seen.[40] By this time, the otic artery at the level of the otic vesicle and the trigeminal artery at the level of the trigeminal ganglion are observed.[14,40,47] These anastomotic arteries supply the most proximal segment of the hindbrain through paired ventral bilateral longitudinal neural arteries.[40] The ventral bilateral longitudinal neural arteries are interconnected through multiple channels, which generally regress but may persist in adults. The anastomoses between the ICA and the longitudinal neural arteries exist for a very short time of 4 and at most 8 days (for the trigeminal and proatlantal arteries) before disappearing as the BA ends its formation at an embryonic length of 14 mm.[40] Persistence of these primitive intracranial embryonic anastomoses occurs in 0.1-1.25% of the population and PTA is the most common.[14] Such persistence has an unknown etiology.[47]
ANATOMY AND CLASSIFICATION
The detailed anatomy of PTA is lacking in the literature and is composed primarily of scattered cadaveric case reports.[35,43,47,52,57] The origin of the PTA is usually in the posterior or lateral surface of the intracavernous ICA just proximal to the origin of the meningohypophyseal trunk. Less commonly, the PTA arises more proximally from the ICA, before the proximal dural ring and there are also reports of it branching from the petrous ICA.[53,56] Suttner et al. made a detailed microscopic description of a PTA found in a cadaveric specimen. This artery arose from the superomedial portion of the distal horizontal segment of the intracavernous carotid artery and coursed medially and immediately posteroinferiorly, passing between the posterior bend of the ICA laterally and the pituitary gland medially. Crossing the cavernous sinus, the PTA has been observed to cross superior as well as inferior to the oculomotor, trochlear, and abducent nerves and is usually medial to the ophthalmic division of the trigeminal nerve [Figure 2]. Conversely, when the PTA arises from the posteromedial aspect of the intracavernous segment of the ICA, it becomes extradural at the dorsum sellae, being medial to the abducent nerve in the majority of cases.[53] Along its intracavernous course, the PTA may give rise to the inferior hypophyseal and dorsal meningeal arteries and branches to the trigeminal nerve.[47] Ohshiro et al. also described the origin of arteries from the PTA including a well developed meningohypophyseal trunk.[35] The PTA may also send branches to the pons.[30,35,43,47] Salas et al. and Khodadad described pontine perforating branches of the PTA.[26,27,43]
Figure 2.
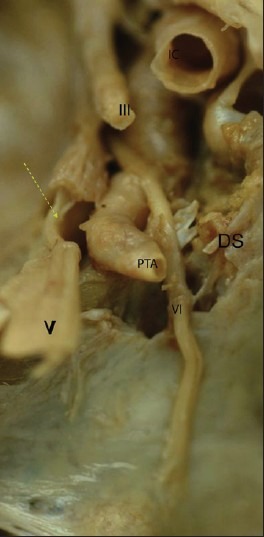
Origin of the artery is identifiable at posterolateral wall of intracavernous segment of internal carotid (IC). It courses adjacent to lateral wall of cavernous sinus, closely related with abducens nerve (VI), which passes over the artery in an oblique direction toward the superior orbital fissure. The ophthalmic branch of trigeminal nerve (V) faces medially with its lateral side. In this specimen, it became extradurally through a channel delimited superiorly by the posterior petroclinoid ligament and inferiorly by a groove of the lateral side of dorsum sellae (DS). Oculomotor nerve (III)
On the basis of its anatomical relationships, Salas et al. purposed to classify PTA into a medial sphenoid variation where it travels into the sella turcica and perforates the dura mater in a groove lateral to the clivus, or sometimes through the dorsum sellae and a lateral petrosal variation where the vessel runs together with the sensory roots of the trigeminal nerve and exits Meckel's cave below the petroclinoid ligament [Figures 2 and 3].[43,53] The former appears to be the most frequent variation occurring up to 11 times more often than the medial variation.[34,35,55]
Figure 3.
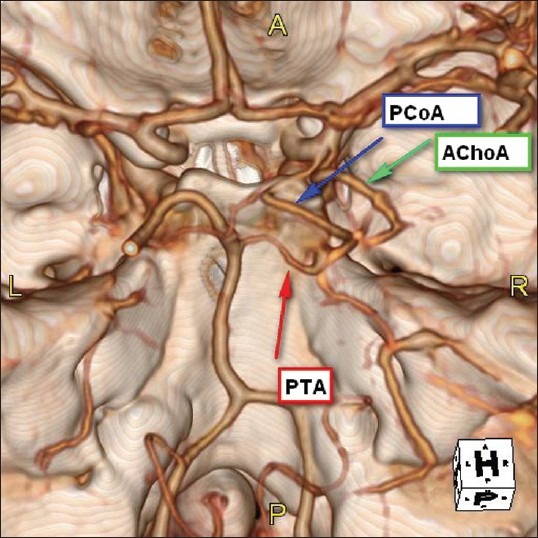
Three-dimensional computed tomographic (CT) angiography showing a lateral petrosal variant of persistent trigeminal artery (PTA) as it exits immediately superior to the cranial end of petroclival fissure; just medial to Meckel's cave and closely related with the ophthalmic branch of trigeminal nerve. It courses posterior and medially to reach the basilar artery before its bifurcation. It relationships with posterior communicating artery (PcomA) and anterior choroidal artery (AchoA) are also showed
Additionally, Saltzman using angiography analyzed eight cases and developed a classification system according to the relationship with the PcomA and the territory that a PTA supplies.[44] Type I was defined when the PTA supplies the upper BA with the superior cerebellar and posterior cerebral arteries and where the proximal BA is typically hypoplastic and the ipsilateral PcomA is absent. Saltzman type II is when the PTA provides the anterior superior cerebellar arteries only and the posterior cerebral arteries arise from the posterior communicating arteries. In this configuration, the first segment (BA) of the posterior cerebral artery is missing. Saltzman type III demonstrates a PTA that unites with a remnant of the primitive paired longitudinal neural artery and supplies one ipsilateral cerebellar artery, which is usually the anterior inferior cerebellar artery, and does not join the BA.[40]
Although the Saltzman classification is commonly used for such variations of the PTA, some authors disagree with its use, due to the embryologic derivation of the PcomA.[34] However, the cases of type I PTA, which makes up 24% of all cases, supplying both posterior cerebral and superior cerebellar arteries associated with hypoplasia or absence of PcomA indicates a relationship between the development of PTA and PcomA.[10]
PTA is frequently associated with other anatomical variations such as absence of the ipsilateral posterior communicating, vertebral or BA.[16,18] In a large case series, approximately 75% of cases demonstrated different grades of BA hypoplasia.[34]In these circumstances, the BA received its flow almost exclusively from the ICA with supply to the upper brain stem, cerebellum and ipsilateral cerebral hemisphere arising from the ICA [Figure 1].[16]
FREQUENCY
The incidence of PTA is variable among different studies, in part, due to differences in the imaging modalities employed. Allen et al., using conventional angiography in 481 patients, identified a prevalence of 0.1%.[2] Chen et al. in their observational study using 3-dimensional time-of-flight magnetic resonance angiography (MRA) at 3.0 Tesla found 25 cases (0.54%) among 4650 patients imaged for various circumstances, which is similar to the findings of Uchino et al. who used similar methodology (0.51%).[10,55] O'uchi and O'uchi also performed MRA using 1.5 and 1.0 Tesla systems in 16,415 patients. In this large series, 48 cases of PTA (0.29%) and 50 cases of PTA variant (0.34%) were identified. Assuming that this PTA variant corresponds to the Saltzman type III PTA, the addition of these cases increases this incidence to 0.68%.[34] Similarly, Rhee et al. reviewed 1250 conventional cerebral angiograms and found a PTA variant in 0.32% and of 2947 cranial MRA, found this entity in 0.1%.[41] Therefore, according to the Saltzman classification system, the frequency of a type I PTA is 24%, type II, 16%, and type III 60%.[10]
CLINICAL IMPLICATIONS
Most cases of PTA had been described when found incidentally on imaging performed for unrelated reasons. However, there are several case reports of pathological processes associated with a PTA. The association between concomitant intracranial aneurysms and PTA is controversial. However, anatomical variations of intracranial arteries, particularly of the anterior communicating artery, have been found to be related to the development of intracranial aneurysms. According to Karazincir et al., nearly half of patients harboring an intracranial aneurysm will be found to have a variation or anomaly of their intracranial arterial vessels.[24] Referring to patients with PTA, older articles have shown a prevalence of associated intracranial saccular aneurysms as high as 14-32%.[8,17] However, this range was estimated on the basis of case reports and literature reviews that included patients whose symptoms were compatible with neurovascular pathology.
More recently, Chen et al. found, in patients with PTA, a prevalence of intracranial aneurysms in 16% using MRA.[10] On the contrary, Cloft et al. and O'uchi and O'uchi, in their respective studies have established a prevalence of aneurysms in this group between 3% and 4.2%, which is very similar to the general population.[8,34]
Saccular and fusiform aneurysms arising from the ICA segment where the PTA arises have also been described and successfully treated by endovascular coiling or microsurgical clipping.[1,22,48,58,61] Ruptures of such aneurysms have presented as spontaneous PTA to cavernous sinus fistula and have been treated with an endovascular approach.[3,9,19,20,50,59,62] Therapeutically, the PTA could provide an alternative endovascular approach to the posterior circulation, especially in some cases where the vertebral or basilar arteries are hypoplastic or compressed and do not permit catheter advancement. For example, Schlamann for treating an acutely ruptured, wide-necked aneurysm of the posterior cerebral artery in a patient with a hypoplastic vertebral artery on one side and tumor compression of the contralateral vertebral artery.[45] Arteriovenous malformations in the septum pellucidum and corpus callosum have been reported in conjunction with a PTA.[33,49]
Along its extradural or intradural course, PTA is intimately related with the medial surface of branches of the trigeminal nerve or with its ganglion, which provides a situation for potential neurovascular conflict.[11,60] Using MRA, de Bondt et al. evaluated 136 patients diagnosed trigeminal neuralgia and found a PTA on the same side of the neuropathic pain in three, which corresponds to a prevalence of 2.2% and this is higher than in the general population.[12]Similarly, the close anatomical relationships of the PTA with the oculomotor, abducens, and trochlear nerves may explain cases of ophthalmoparesis in the presence of a PTA.[7,38] Such deficits may be persistent or intermittent and the abducens nerve is the most commonly affected, probably due to the higher relative frequency of a lateral variant of the PTA, which pierces the dura mater below the petroclinoid ligament, just superior to the entry of the abducens nerve into Dorello's canal Figure 3].[23] Parkinson and Shields identified a PTA at autopsy where the cavernous segment of the abducens nerve coursed below the abducens nerve, which it slightly elevated along its course.[39] However, no abducens nerve palsy was recognized premortem. The oculomotor nerve enters the cavernous sinus via the posterior portion of its roof and could be compressed especially bymedial variants of a PTA. Bosco et al. reported a patient with complete oculomotor nerve palsy with PTA dolichoectasia.[6] Likewise, Lee et al. reported a case of PTA with transient pupil sparing oculomotor nerve palsy associated with hypertensive crisis that resolved following hypertension control.[31] Merry and Jamieson reported a patient with facial pain and diplopia who was found to have an ipsilateral PTA. The trigeminal and abducens nerves were found to be compressed and following decompression, her facial pain more or less resolved. Over 4 months, her diplopia improved.[32] Tschabitscher and Perneczky have stated that the PTA is located superior to the oculomotor, trochlear, and abducens nerves, and is medial to the ophthalmic part of the trigeminal nerve.[51] Silver and Wilkins have depicted the oculomotor, trochlear, and abducens nerves as coursing inferior to the PTA.[46] The third, fourth and sixth cranial nerves have been compressed with resultant paresis in some patients with a PTA. After branching from the posteromedial aspect of the intracavernous ICA, the medial type PTA closely surrounds the pituitary gland and could exert compression on its stalk resulting in hormonal disturbances that may produce hyperprolactinemia due to stalk effect, to complete hypopituitarism.[15,54] Moreover, during the planning of surgical approaches to the skull base, it is important to evaluate the vascular anatomy of the sellar and parasellar regions, searching for PTA. The unnoticed presence of a PTA may result in disastrous outcomes following approaches to the sellar or parasellar regions, the cavernous sinus or Gasserian ganglion.[4,13,47,53]
As mentioned earlier, PTA is frequently associated with BA hypoplasia and in this condition, the majority of blood flow to the upper pons, mesencephalon, cerebellum, and basal surfaces of the temporal and occipital lobes is provided from the ICA via the PTA.[16] In these cases, dissections, atherosclerotic lesions or cardiac emboli of the ICA may result in ischemic events of the posterior circulation.[5,21,30] It is also important to take in account that during examination with Doppler ultrasonography in presence of PTA, the peak systolic velocity in carotid could be abnormally high as in other diseases as carotid stenosis.[28,42]
Occlusion of branches that arise directly from the PTA or in the segment of the ICA where it emerges also could be clinically evident as brainstem infarctions, as was informed by Kwon et al. and Okada et al.[30,36] Symptoms related with this event are variable in severity since dizziness, vertigo or paresthesias to more devastating clinical events as locked-in syndrome.[25,47] Such patients refer complaints as recurrent episodes of vertigo, dizziness, headache, nausea, vomiting, blurred vision, numbness, tinnitus, paresthesias, transient hypoesthesia, which suggest the presentation of a vertebrobasilar insufficiency.
The pathophysiology of this clinical picture remains poorly understood. In patients with risk factors for cerebrovascular disease a rational explanation is transient ischemic attacks due to ICA microembolism as hypothesized by Eluvathingal et al. and Battista et al.[5,16] Nevertheless, these complaints have been also informed in several young patients without risk factors for stroke. In contrast, PTA conforms an alternate passage through which the ICA territory could be supplied from BA; generating a “carotid steal” and triggering the symptoms despite normal diameter of basilar, posterior cerebral, or posterior communicating arteries. Interestingly, Okanishi et al. described a 6-month-old boy presenting with lower brainstem dysfunction and demonstrated on imaging a PTA, with flow from a dilated BA to the right ICA and additional lower brainstem compression by the dilated BA. Clinical evidence of a compressive effect of the BA has been confirmed by evoked potentials.[37] Therefore, mass effect might be considered in this group of patients presenting with symptoms of brainstem dysfunction in the absence of demonstrable ischemia. Persistent embryonic intracranial arteries may be more common in patients with moyamoya disease.[29]
CONCLUSIONS
PTA is a rare remnant of the embryonic circulatory system that unites the internal carotid and vertebrobasilar systems. Its significance in association with other vascular pathologies, especially with intracranial aneurysms, remains unclear. During neuroimaging, the presence of a PTA should be assessed due to potentially dangerous complications that may occur with surgical procedures of the skull base. Moreover, evidence derived from cases series of suggests that compressive effects of a PTA may result in ophthalmoparesis or trigeminal neuralgia. For these reasons and others, anatomical knowledge of the PTA may decrease patient morbidity.
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/111/101798
Contributor Information
Gabriel Alcalá-Cerra, Email: alcalagabriel@gmail.com.
R S Tubbs, Email: shane.tubbs@chsys.org.
Lucía M Niño-Hernández, Email: lu_dharma@hotmail.com.
REFERENCES
- 1.Agrawal D, Mahapatra AK, Mishra NK. Fusiform aneurysm of a persistent trigeminal artery. J Clin Neurosci. 2005;12:500–3. doi: 10.1016/j.jocn.2004.06.018. [DOI] [PubMed] [Google Scholar]
- 2.Allen JW, Alastra AJ, Nelson PK. Proximal intracranial internal carotid artery branches: Prevalence and importance for balloon occlusion test. J Neurosurg. 2005;102:45–52. doi: 10.3171/jns.2005.102.1.0045. [DOI] [PubMed] [Google Scholar]
- 3.Asai K, Hasuo K, Hara T, Miyagishima T, Terano N. Traumatic persistent trigeminal artery-cavernous sinus fistula treated by transcatheter arterial embolization.A case report. Interv Neuroradiol. 2010;16:93–6. doi: 10.1177/159101991001600113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Baltsavias G, Valavanis A. Endovascular occlusion of a lacerated primitive trigeminal artery during surgical resection of clival chordoma.A case report . Interv Neuroradiol. 2010;16:204–7. doi: 10.1177/159101991001600214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Battista RA, Kwartler JA, Martinez DM. Persistent trigeminal artery as a cause of dizziness. Ear Nose Throat J. 1997;76:43–5. [PubMed] [Google Scholar]
- 6.Bosco D, Consoli D, Lanza PL, Plastino M, Nicoletti F, Ceccotti C. Complete oculomotor palsy caused by persistent trigeminal artery. Neurol Sci. 2010;31:657–9. doi: 10.1007/s10072-010-0342-1. [DOI] [PubMed] [Google Scholar]
- 7.Clerici AM, Merlo P, Rognone F, Noce M, Rognone E, Bono G. Persistent trigeminal artery causing “double” neurovascular conflict. Headache. 2009;49:472–6. doi: 10.1111/j.1526-4610.2008.01258.x. [DOI] [PubMed] [Google Scholar]
- 8.Cloft HJ, Razack N, Kallmes DF. Prevalence of cerebral aneurysms in patients with persistent primitive trigeminal artery. J Neurosurg. 1999;90:865–7. doi: 10.3171/jns.1999.90.5.0865. [DOI] [PubMed] [Google Scholar]
- 9.Chan YL, Shing KK, Wong KC, Poon WS. Transvenous embolisation of a carotid-trigeminal cavernous fistula. Hong Kong Med J. 2006;12:310–2. [PubMed] [Google Scholar]
- 10.Chen YC, Li MH, Chen SW, Hu DJ, Qiao RH. Incidental findings of persistent primitive trigeminal artery on 3-dimensional time-of-flight magnetic resonance angiography at 3.0 T: An analysis of 25 cases. J Neuroimaging. 2011;21:152–8. doi: 10.1111/j.1552-6569.2010.00472.x. [DOI] [PubMed] [Google Scholar]
- 11.Chidambaranathan N, Sayeed ZA, Sunder K, Meera K. Persistent trigeminal artery: A rare cause of trigeminal neuralgia - MR imaging. Neurol India. 2006;54:226–7. [PubMed] [Google Scholar]
- 12.de Bondt BJ, Stokroos R, Casselman J. Persistent trigeminal artery associated with trigeminal neuralgia: Hypothesis of neurovascular compression. Neuroradiology. 2007;49:23–6. doi: 10.1007/s00234-006-0150-8. [DOI] [PubMed] [Google Scholar]
- 13.Dimmick SJ, Faulder KC. Normal variants of the cerebral circulation at multidetector CT angiography. Radiographics. 2009;29:1027–43. doi: 10.1148/rg.294085730. [DOI] [PubMed] [Google Scholar]
- 14.Donkelaar M, van der Vliet T. Overview of human brain development. In: Donkelaar M, Lammens M, Hori A, editors. Clinical Neuroembryology Development and developmental disorders of the human central nervous system. 2nd ed. Springer: Würzburg; 2006. pp. 31–5. [Google Scholar]
- 15.Ekinci G, Baltacioglu F, Kilic T, Cimsit C, Akpinar I, Pamir N, et al. A rare cause of hyperprolactinemia: Persistent trigeminal artery with stalk-section effect. Eur Radiol. 2001;11:648–50. doi: 10.1007/s003300000573. [DOI] [PubMed] [Google Scholar]
- 16.Eluvathingal Muttikkal TJ, Varghese SP, Chavan VN. Persistent trigeminal artery and associated vascular variations. Australas Radiol. 2007;51:31–3. doi: 10.1111/j.1440-1673.2007.01828.x. [DOI] [PubMed] [Google Scholar]
- 17.George AE, Lin JP, Morantz RA. Intracranial aneurysm on a persistent primitive trigeminal artery.Case report. J Neurosurg. 1971;35:601–4. doi: 10.3171/jns.1971.35.5.0601. [DOI] [PubMed] [Google Scholar]
- 18.Goyal M. The tau sign. Radiology. 2001;220:618–9. doi: 10.1148/radiol.2202991498. [DOI] [PubMed] [Google Scholar]
- 19.Guglielmi G, Vinuela F, Dion J, Duckwiler G, Cantore G, Delfini R. Persistent primitive trigeminal artery-cavernous sinus fistulas: Report of two cases. Neurosurgery. 1990;27:805. doi: 10.1097/00006123-199011000-00021. discussion 808-9. [DOI] [PubMed] [Google Scholar]
- 20.Hurst RW, Howard RS, Zager E. Carotid cavernous fistula associated with persistent trigeminal artery: Endovascular treatment using coil embolization. Skull Base Surg. 1998;8:225–8. doi: 10.1055/s-2008-1058188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Iancu D, Anxionnat R, Bracard S. Brainstem infarction in a patient with internal carotid dissection and persistent trigeminal artery:A case report. BMC Med Imaging. 2010;10:14. doi: 10.1186/1471-2342-10-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kai Y, Ohmori Y, Watanabe M, Morioka M, Hirano T, Kawano T, et al. Coil embolization of an aneurysm located at the trunk of the persistent primitive trigeminal artery. Neurol Med Chir (Tokyo) 2011;51:361–4. doi: 10.2176/nmc.51.361. [DOI] [PubMed] [Google Scholar]
- 23.Kalidindi RS, Balen F, Hassan A, Al-Din A. Persistent trigeminal artery presenting as intermittent isolated sixth nerve palsy. Clin Radiol. 2005;60:515–9. doi: 10.1016/j.crad.2004.09.004. [DOI] [PubMed] [Google Scholar]
- 24.Karazincir S, Ada E, Sarsilmaz A, Yalcin O, Vidinli B, Sahin E. [Frequency of vascular variations and anomalies accompanying intracranial aneurysms] Tani Girisim Radyol. 2004;10:103–9. [PubMed] [Google Scholar]
- 25.Kato Y, Nagoya H, Furuya D, Deguchi I. [Locked-in syndrome due to bilateral cerebral peduncular infarctions with occlusion of persistent primitive trigeminal artery] Rinsho Shinkeigaku. 2007;47:601–4. [PubMed] [Google Scholar]
- 26.Khodadad G. Persistent hypoglossal artery in the fetus. Acta Anat (Basel) 1977;99:477–81. doi: 10.1159/000144873. [DOI] [PubMed] [Google Scholar]
- 27.Khodadad G. Trigeminal artery and occlusive cerebrovascular disease. Stroke. 1977;8:177–81. doi: 10.1161/01.str.8.2.177. [DOI] [PubMed] [Google Scholar]
- 28.Koch S, Romano JG, Forteza A. Subclavian steal and a persistent trigeminal artery. J Neuroimaging. 2002;12:190–2. doi: 10.1111/j.1552-6569.2002.tb00120.x. [DOI] [PubMed] [Google Scholar]
- 29.Komiyama M, Nakajima H, Nishikawa M, Yasui T, Kitano S, Sakamoto H, et al. High incidence of persistent primitive arteries in moyamoya and quasi-moyamoya diseases. Neurol Med Chir (Tokyo) 1999;39:416–20. doi: 10.2176/nmc.39.416. discussion 420-2. [DOI] [PubMed] [Google Scholar]
- 30.Kwon JY, Lee EJ, Kim JS. Brainstem infarction secondary to persistent trigeminal artery occlusion: Successful treatment with intravenous rt-PA. Eur Neurol. 2010;64:311. doi: 10.1159/000321417. [DOI] [PubMed] [Google Scholar]
- 31.Lee MR, Chuang YM, Chen WJ, Lin CP. Meticulous blood pressure control is mandatory for symptomatic primitive trigeminal artery. Am J Emerg Med. 2009;27:634.e5–7. doi: 10.1016/j.ajem.2008.09.034. [DOI] [PubMed] [Google Scholar]
- 32.Merry GS, Jamieson KG. Operative approach to persistent trigeminal artery producing facial pain and diplopia.Case report. J Neurosurg. 1977;47:613–8. doi: 10.3171/jns.1977.47.4.0613. [DOI] [PubMed] [Google Scholar]
- 33.Mohanty CB, Devi BI, Somanna S, Bhat DI, Dawn R. Corpus callosum arteriovenous malformation with persistent trigeminal artery. Br J Neurosurg. 2011;25:736–40. doi: 10.3109/02688697.2011.554583. [DOI] [PubMed] [Google Scholar]
- 34.O'Uchi E, O'Uchi T. Persistent primitive trigeminal arteries (PTA) and its variant (PTAV): Analysis of 103 cases detected in 16,415 cases of MRA over 3 years. Neuroradiology. 2010;52:1111–9. doi: 10.1007/s00234-010-0669-6. [DOI] [PubMed] [Google Scholar]
- 35.Ohshiro S, Inoue T, Hamada Y, Matsuno H. Branches of the persistent primitive trigeminal artery-an autopsy case. Neurosurgery. 1993;32:144–8. doi: 10.1227/00006123-199301000-00025. [DOI] [PubMed] [Google Scholar]
- 36.Okada Y, Shima T, Nishida M, Yamada T, Yamane K, Okita S, et al. Bilateral persistent trigeminal arteries presenting with brain-stem infarction. Neuroradiology. 1992;34:283–6. doi: 10.1007/BF00588182. [DOI] [PubMed] [Google Scholar]
- 37.Okanishi T, Saito Y, Miki S, Nagaishi J, Hanaki K, Tomita Y, et al. Lower brainstem dysfunction in an infant with persistent primitive trigeminal artery. Brain Dev. 2007;29:189–92. doi: 10.1016/j.braindev.2006.08.008. [DOI] [PubMed] [Google Scholar]
- 38.Olivares J, Alonso-Verdegay G. Persistent trigeminal artery and isolated sixth cranial nerve. Rev Neurol. 2007;44:685–6. [PubMed] [Google Scholar]
- 39.Parkinson D, Shields CB. Persistent trigeminal artery: Its relationship to the normal branches of the cavernous carotid. J Neurosurg. 1974;40:244–8. doi: 10.3171/jns.1974.40.2.0244. [DOI] [PubMed] [Google Scholar]
- 40.Raybaud C. Normal and abnormal embryology and development of the intracranial vascular system. Neurosurg Clin N Am. 2010;21:399–426. doi: 10.1016/j.nec.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 41.Rhee SJ, Kim MS, Lee CH, Lee GJ. Persistent trigeminal artery variant detected by conventional angiography and magnetic resonance angiography-incidence and clinical significance. J Korean Neurosurg Soc. 2007;42:446–9. doi: 10.3340/jkns.2007.42.6.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Romero JM, Lev MH, Chan ST, Connelly MM, Curiel RC, Jackson AE, et al. US of neurovascular occlusive disease: Interpretive pearls and pitfalls. Radiographics. 2002;22:1165–76. doi: 10.1148/radiographics.22.5.g02se141165. [DOI] [PubMed] [Google Scholar]
- 43.Salas E, Ziyal IM, Sekhar LN, Wright DC. Persistent trigeminal artery: An anatomic study. Neurosurgery. 1998;43:557–61. doi: 10.1097/00006123-199809000-00082. discussion 561-2. [DOI] [PubMed] [Google Scholar]
- 44.Saltzman GF. Patent primitive trigeminal artery studied by cerebral angiography. Acta Radiol. 1959;51:329–36. doi: 10.3109/00016925909171103. [DOI] [PubMed] [Google Scholar]
- 45.Schlamann M, Doerfler A, Schoch B, Forsting M, Wanke I. Balloon-assisted coil embolization of a posterior cerebral artery aneurysm via a persistent primitive trigeminal artery: Technical note. Neuroradiology. 2006;48:931–4. doi: 10.1007/s00234-006-0149-1. [DOI] [PubMed] [Google Scholar]
- 46.Silver J, Wilkins R. Persistent embryonic intracranial and extracranial vessels. In: Wilkins R, Rengachary S, editors. Neurosurgery Update II Vascular, Spinal, Pediatric, and Functional Neurosurgery. 2nd ed. McGraw-Hill, Inc: New York; 1991. pp. 50–9. [Google Scholar]
- 47.Suttner N, Mura J, Tedeschi H, Ferreira MA, Wen HT, de Oliveira E, et al. Persistent trigeminal artery: A unique anatomic specimen analysis and therapeutic implications. Neurosurgery. 2000;47:428–33. doi: 10.1097/00006123-200008000-00030. [DOI] [PubMed] [Google Scholar]
- 48.Takase T, Tanabe H, Kondo A, Nonoguchi N, Tane K. Surgically treated aneurysm of the trunk of the persistent primitive trigeminal artery-case report. Neurol Med Chir (Tokyo) 2004;44:420–3. doi: 10.2176/nmc.44.420. [DOI] [PubMed] [Google Scholar]
- 49.Talanov AB, Filatov Iu M, Eliava S, Novikov AE, Kulishova Ia G. [Arteriovenous malformation of septum pellucidum in combination with persistent trigeminal neuralgia] Zh Vopr Neirokhir Im N N Burdenko. 2009:50–3. discusion 53-4. [PubMed] [Google Scholar]
- 50.Tokunaga K, Sugiu K, Kameda M, Sakai K, Terasaka K, Higashi T, et al. Persistent primitive trigeminal artery-cavernous sinus fistula with intracerebral hemorrhage: Endovascular treatment using detachable coils in a transarterial double-catheter technique.Case report and review of the literature. J Neurosurg. 2004;101:697–9. doi: 10.3171/jns.2004.101.4.0697. [DOI] [PubMed] [Google Scholar]
- 51.Tschabitscher M, Perneczky A. [Relation of the cerebellar arteries to the meatus acusticus internus] Acta Anat (Basel) 1974;88:231–44. [PubMed] [Google Scholar]
- 52.Tubbs RS, Shoja MM, Salter EG, Oakes WJ. Cadaveric findings of persistent fetal trigeminal arteries. Clin Anat. 2007;20:367–70. doi: 10.1002/ca.20386. [DOI] [PubMed] [Google Scholar]
- 53.Tubbs RS, Verma K, Riech S, Mortazavi MM, Shoja MM, Loukas M, et al. Persistent fetal intracranial arteries: A comprehensive review of anatomical and clinical significance. J Neurosurg. 2011;114:1127–34. doi: 10.3171/2010.11.JNS101527. [DOI] [PubMed] [Google Scholar]
- 54.Tungaria A, Kumar V, Garg P, Jaiswal AK, Behari S. Giant, thrombosed, sellar-suprasellar internal carotid artery aneurysm with persistent, primitive trigeminal artery causing hypopituitarism. Acta Neurochir (Wien) 2011;153:1129–33. doi: 10.1007/s00701-010-0931-z. [DOI] [PubMed] [Google Scholar]
- 55.Uchino A, Saito N, Okada Y, Kozawa E, Mizukoshi W, Inoue K, et al. Persistent trigeminal artery and its variants on MR angiography. Surg Radiol Anat. 2012;34:271–6. doi: 10.1007/s00276-011-0848-0. [DOI] [PubMed] [Google Scholar]
- 56.Uchino A, Sawada A, Takase Y, Kudo S. MR angiography of anomalous branches of the internal carotid artery. AJR Am J Roentgenol. 2003;181:1409–14. doi: 10.2214/ajr.181.5.1811409. [DOI] [PubMed] [Google Scholar]
- 57.Warnke JP, Tschabitscher M, Thalwitzer J, Galzio R. Endoscopic anatomy for transnasal transsphenoidal pituitary surgery in the presence of a persistent trigeminal artery. Cen Eur Neurosurg. 2009;70:207–10. doi: 10.1055/s-0028-1093354. [DOI] [PubMed] [Google Scholar]
- 58.Watanabe T, Aoki A, Chan SC. [Two cases of persistent trigeminal artery variant] No Shinkei Geka. 1988;16:95–100. [PubMed] [Google Scholar]
- 59.Xin-Ya Qian C, Ares C, Codere F, Tampieri D. Rupture of an aneurysm of the persistent trigeminal artery presenting as a carotid-cavernous sinus fistula. Orbit. 2009;28:275–80. doi: 10.3109/01676830903190222. [DOI] [PubMed] [Google Scholar]
- 60.Yamada Y, Kondo A, Tanabe H. Trigeminal neuralgia associated with an anomalous artery originating from the persistent primitive trigeminal artery. Neurol Med Chir (Tokyo) 2006;46:194–7. doi: 10.2176/nmc.46.194. [DOI] [PubMed] [Google Scholar]
- 61.Yang Z, Liu J, Zhao W, Xu Y, Hong B, Huang Q, et al. A fusiform aneurysm of a persistent trigeminal artery variant: Case report and literature review. Surg Radiol Anat. 2010;32:401–3. doi: 10.1007/s00276-009-0537-4. [DOI] [PubMed] [Google Scholar]
- 62.Yoshida M, Ezura M, Mino M. Carotid-cavernous fistula caused by rupture of persistent primitive trigeminal artery trunk aneurysm. Neurol Med Chir (Tokyo) 2011;51:507–11. doi: 10.2176/nmc.51.507. [DOI] [PubMed] [Google Scholar]


