Abstract
Background:
Computed tomography (CT) requires highest radiation doses in radiology. The collective dose from the use of radiation in medicine is rising, partly due to increase in CT use as well as the growing popularity of multislice scanners. There is growing concern from multiple studies that radiation from repeated CT scans could induce malignancies later in life. Patients with hydrocephalus are unique in that they are often subjected to repeated CT imaging throughout their lives to monitor whether their hydrocephalus is under control. We designed a study to see whether a low dose radiation CT protocol could provide effective information for monitoring hydrocephalus.
Methods:
A pilot study was done with 10 patients with hydrocephalus who needed CT scanning to monitor their hydrocephalus. The CT protocol was altered for each patient to sequentially bring down the radiation dose to the minimum level, which would provide sufficient diagnostic information. Based on the pilot study, a new low dose CT scanning protocol was devised and tested on 25 shunted patients who needed monitoring of their hydrocephalus. All images were carefully scrutinized by a consultant neuroradiologist and consultant neurosurgeon to ensure that the following diagnostic information could be analyzed: 1. ventricular size, 2. cisterns, 3. sulcii, and 4. cathet er position
Results:
All low-dose CT images were diagnostically acceptable and provided sufficient information to the requesting clinician. None of the subjects required repeat imaging. The effective radiation dose was reduced from 2.2 mSv using a conventional CT protocol to 0.29 mSv with the new low dose CT protocol. The new CT protocol provides 87% less effective radiation dose compared with conventional scans.
Conclusions:
We propose a new low dose CT protocol which can be used for monitoring shunted hydrocephalus. The radiation to the patient with this protocol is comparable to that of a skull X-ray. However, this protocol should only be requested by a clinician who is aware of its limitations.
Keywords: As low as reasonably Achievable, computed tomography, hydrocephalus, malignancy
INTRODUCTION
There has been a steady increase in the application of computed tomography (CT) in recent years, but this has not been accompanied by a reduction in examination dose, so CT now makes up about 50% of the collective dose from medical radiology in European countries and 70% in the United States.[11]
CT utilization in the US has grown from 3 million scans in 1980 to 68 million procedures in 2007 (one scan for every five citizens). In England 2.8 million CT scans were performed in 2007(one scan for every 22 citizens). The average annual increase in the number of scans is about 10% in UK and 11.5% in the USA; this growth is faster than for other imaging modalities and shows no sign of slowing down.
The reductions in doses that have been achieved for radiography and fluoroscopy have not been replicated for CT, which is the highest dose technique.
The doses that some patients are receiving have now moved into the realm where definite risks to health are known from epidemiological studies rather than being predicted through extrapolation from higher dose levels.
ALARA is an acronym for an important principle in radiation protection and stands for “As Low As Reasonably Achievable”. The aim is to minimize the risk of radioactive exposure or amount of dose while keeping in mind that some exposure may be acceptable in order to further the task at hand.
All medical practitioners have a responsibility to keep their patients' exposure to diagnostic radiation to as minimum as possible.[8]
CT imaging for monitoring shunted hydrocephalus is unique. Patients need to be scanned at short, regular intervals; hence there is a risk of over-exposure due to increased cumulative radiation over a lifetime.
Cerebrospinal fluid (CSF) shunts fail at a rate of 30-40% in the first year after insertion and at roughly 5% per year subsequently.[5]
In keeping with the principles of ALARA, we decided to explore the possibility of trying to devise a new CT protocol with lesser radiation for monitoring shunted hydrocephalus. The aim of the study was to devise a low dose CT protocol which would provide sufficent diagnostic information for monitoring shunted hydrocephlaus with the lowest possible radiation. Informed consent was sought from all patients.
MATERIALS AND METHODS
All subjects were adult inpatients who were scheduled to have nonurgent CT scans to monitor their hydrocephalus.
Various technical modifications in CT scanners can result in substantial savings of radiation doses. Altering tube current is a commonly adopted strategy because ionizing radiation has a direct linear relationship with tube strength (mAs). However, alterations in tube potential (kV), collimation (determines the nominal or effective slice thickness), Pitch (it's a parameter used to characterize table movement relative to the collimated thickness of the fan beam), and section thickness can also contribute to dose savings. The radiation dose is proportional to the square of the tube potential, so any reduction there can substantially reduce the radiation dose.
The CT scanner in our institution is a Siemens (Siemens AG, D-91052 Erlangen, Germany) Somatom Sensation 16 slice multislice scanner.
The conventional CT head protocol in our institution was as follows:
kV:140,
mAs: 300,
Pitch: 1,
Collimation: 18 mm, and
Slice thickness: 3-6 mm (3 mm slices for the infra-tentorial compartment and 6 mm slices for the supra-tentorial compartment).
It was decided to leave unaltered the pitch, slice thickness, and collimation so as to enable comparison with previous scans using the conventional protocol.
Initially, a pilot study with ten patients was undertaken to sequentially reduce the mAs and then the kV.
All images were carefully scrutinized by a consultant neuroradiologist and consultant neurosurgeon to ensure that the following diagnostic information was available before proceeding to a further dose reduction:
ventricular size,
cisterns,
sulcii, and
catheter position.
Eventually we ascertained that the lowest radiation we could achieve with sufficient diagnostic information was 40 mAs and 120 kV. Below this radiation level, the sulcii were not clearly visible.
We then applied the new low dose CT protocol for a further 25 patients with hydrocephalus who were scheduled to have CT scanning to monitor their hydrocephalus.
Again all scans were carefully scrutinized by a consultant neuroradiologist and consultant neurosurgeon to ensure that the four diagnostic features were available for each scan.
All scans in this study were done for appropriate diagnostic need of the patient only and no additional scans were performed purely for this study. Crucially, no further scans had to be done due to lack of sufficient information on the low dose CT.
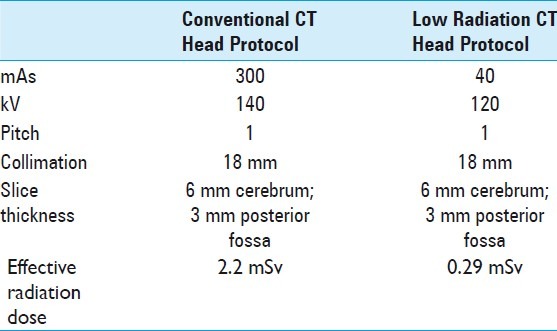
See Table 1 for comparison of the conventional and low radiation CT head protocols.
Table 1.
Comparing conventional and low dose computed tomography protocols
Calculation of radiation dose
Most studies in the literature use the effective dose to compare the risks from radiation of CT scanning. The effective dose is intended to provide a single-value estimate of the overall stochastic risk (i.e., the total risk of cancer and genetic defects) of a given irradiation, whether received by the whole body, part of the body, or 1 or more individual organs.
The Unit is milli Sievert (mSv).
Accurate measurement very difficult and even the best studies acknowledge up to 40% error. However, it is still useful as a guide.
Areas of error in effective dose calculation studies can be due to machine and operator, patient characteristic,s and calculation approximations.
The effective dose in our study was calculated with the help of our medical physics department using the ImPACT CTDosimetry dose calculator (a widely used software program for calculating the effective dose) and Siemens Specifications.[6]
RESULTS
The age group of the patients ranged from 19-67 years.
Average effective dose per CT using the conventional CT algorithm was calculated as 2.2 mSv.
Average effective dose per CT using the low radiation CT algorithm was calculated as 0.29 mSv. This amounts to a reduction of 87% in effective radiation dose compared with the conventional CT.
All the low-dose CT images were diagnostically acceptable to the requesting clinician as well as the consultant neurosurgeon and consultant neuroradiologist involved in the study.
None of the subjects required repeat imaging through failure of the low radiation CT to provide required information.
Using the low radiation CT, It was possible to visualize ventricular size, cisterns, sulcii, and catheter position.
Comparison of scans using conventional protocol and the new low radiation dose protocol: see Figures 1 and 2.
Figure 1.
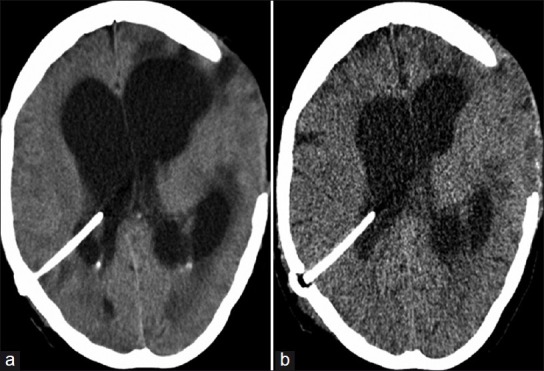
(a) CT head using conventional CT protocol of a patient who presented with a blocked ventriculoperitoneal shunt. (b) CT head using low dose CT protocol of same patient after shunt revision
Figure 2.
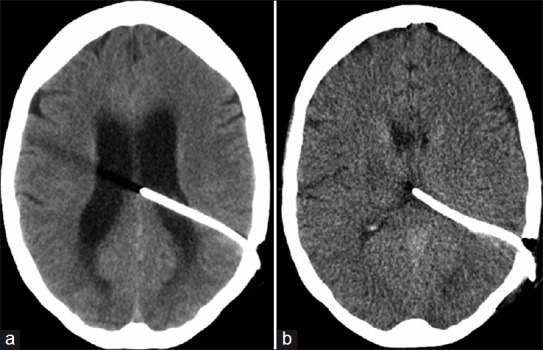
(a) CT head using conventional CT protocol of another patient who presented with a blocked ventriculoperitoneal shunt. (b) CT head using low dose CT protocol of same patient after shunt revision
DISCUSSION
Definite risks to health from current radiation doses have been identified from epidemiological studies.
Among approximately 30,000 individuals in the cancer incidence cohort of atomic bomb survivors who received doses between 5 and 100 mSv (mean dose, 29 mSv), there was a statistically significant increase in cancer risk (77 excess cancers, P = 0.05) compared with that in the control population.[9]
The International Commission on Radiological Protection (ICRP), used a linear no-threshold extrapolation of nuclear explosion data and estimated 50 additional fatal cancers induced per million people exposed to 1 mSv of medical radiation.[7]
In 2007, a 15-country study reported the cancer induction effect of low-level radiation exposure studied in 407,000 radiation workers followed for over 20 years providing 5.2 million person-years of follow-up.[3]
This study is unique as it reports on the largest cohort to date, has accurate dosimetry, and investigated multiethnic workers.
Ninety percent of the subjects received a dose less than 50 mSv and on average each worker received a dose of 19 mSv. Therefore this study is focused on low-level doses, close to that received during a single chest CT examination (6-11 mSv).
The authors reported an excess re lative risk (ERR) for all-cause mortality of 0.42 per Sievert (0.00042 per mSv), with a statistically significant increasing excess relative risk with increasing radiation dose (P < 0.02) indicating a dose-response effect.
The increased risk in all-cause mortality was mainly due to an increase in mortality from all cancers.
Risk of malignancy from diagnostic radiation.
The risk of fatal malignancy from a single CT examination in a young child has been estimated at about 1 in 1000. Though this might seem alarming, to put this in context, it must be borne in mind that the average expectation of dying from cancer (independent from any radiation exposure) is about 250 in 1000.[2]
In a more recent study, CT exposures were estimated to produce 0.7% of total expected baseline cancer incidence and 1% of total cancer mortality.[12]
The most widely accepted risk models do estimate that there is a lifetime attributable risk of radiation-induced cancer with a linear no-threshold dose-response curve.[4]
Hence CT scanning seems to cause a small but definite increase in the odds of one developing cancer.
CT scanning for shunted hydrocephalus seems to be on the increase despite more widespread availability of magnetic resonance imaging (MRI). This is partly due to the fact that many patients with hydrocephalus present as an emergency and it is easier to get CT scans as opposed to MRI scans. The time for image acquisition is also much quicker. The medical and legal consequences of missing a blocked shunt often mean that any admission of a patient with a shunt invariably will involve a CT scan at some stage of the admission process.
Reducing the dose of a CT can easily be achieved by altering the parameters of the scan such as the tube strength, then number of slices, the thickness of each slice, and the voltage strength. However, a reduction in dose invariably results in poor quality (noise) of the resultant image. Most modern CT scanners already have algorithms to try and reduce radiation doses to the minimum required for clear images. There have been previous attempts to produce low dose CT head protocols for monitoring hydrocephalus. Udaysankar et al. were able to achieve a 63% reduction in their radiation dose compared with conventional CT scans at their institution, by reducing the tube strength.[13] Rybka et al. were able to reduce radiation by up to 70% compared with their conventional CT scans.[10]
We have, however, been able to go the furthest so far, in reducing the radiation, by recognizing that the diagnostic information required from a scan of a shunted patient is unique in that it is usually limited to visualizing the size of the ventricles and CSF spaces and the ventricular catheter position. All these structures coincidently also have quite marked contrast to their surrounding structures. Therefore in theory, reducing the radiation dose though may result in a more poor quality image, it could still provide useful information of structures with significant differences in contrast from each other.
Using the new protocol we have shown that the radiation dose can be reduced by 87% while still providing enough diagnostic information to monitor hydrocephalus. The 0.29 mSv average effective dose from our low dose CT head protocol compares very favorably with diagnostic radiation reference levels for skull anteroposterior (0.54 mSv) and lateral (0.35 mSv) X-rays.[1]
One of the limitations of the low radiation protocol is that the resultant image has poorer quality compared with a normal CT and may not give information about subtle features like subarachnoid hemorrhage, cerebritis, early stages of infarction, etc. For this reason, we recommend that the low dose CT should be requested only by the treating doctor who is specifically looking only for certain features related to hydrocephalus and not for anything else. We also advise that the low dose CT protocol be used initially only for follow up CT scans.
As we were striving to reduce the radiation to the patient, we did not do concurrent conventional CT scans along with every low dose radiation CT.
There are other ways of reducing the radiation dose in CT such as increasing the thickness of each slice, reducing the number of slices, increasing the pitch of the gantry, etc. However, these measures would result in a CT scan which would be difficult to compare with a normal CT of the same patient, and hence our decision to achieve the reduction by only altering the voltage and tube current strength. Other parameters like the position of the head in the isocenter of the gantry were left unaltered.
Though it is possible to see transependymal migration of CSF in some of the scans in our study, it is possible that this may have been missed in some of the scans.
This is an ideal investigation when the information required is the size of the ventricles and position of the catheter, both of which can be very clearly seen in the low radiation CT. A substantial number of the scans done for hydrocephalus are for this reason. In our institution, it has been the practice to do a routine postoperative CT after a shunt revision to check the catheter position. We now use the low dose CT protocol for all such scans.
Even though one could argue that the best way to reduce radiation would be to avoid unnecessary scanning or use only MRI if imaging is necessary, it remains a fact that a substantial number of neurosurgeons order routine CT scans to monitor their patients with hydrocephalus. It is those neurosurgeons in particular, who we would encourage to use low dose CT protocols for their routine CTs.
It is worth mentioning that some of the patients in the pilot study had other pathologies in addition to hydrocephalus and with the low dose CT we were able to visualize clearly, certain pathologies like brain abscess, intracerebral hemorrhage, and intracranial air. It is possible that other low dose protocols could be devised to monitor such conditions.
CONCLUSION
Low dose CT protocol can be applied in the monitoring of shunted hydrocephalus to reduce unnecessary radiation.
To avoid unnecessary repeat scanning, such protocols should only be requested by the lead clinician with awareness of its limitations.
Further studies are needed into the role of low dose CT in other intracranial pathologies (e.g., abscesses/mass lesions).
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/103/100860
Contributor Information
Kuriakose J. George, Email: joshigeorge@doctors.org.uk.
Deb Roy, Email: drdebroy@doctors.org.uk.
REFERENCES
- 1.Aroua A, Besançon A, Buchillier-Decka I, Trueb P, Valley JF, Verdun FR, et al. Adult reference levels in diagnostic and interventional radiology for temporary use in Switzerland. Radiat Prot Dosimetry. 2004;111:289–95. doi: 10.1093/rpd/nch343. [DOI] [PubMed] [Google Scholar]
- 2.Brenner D, Elliston C, Hall E, Berdon W. Estimated risks of radiation-induced fatal cancer from pediatric CT. Am J Roentgenol. 2001;176:289–96. doi: 10.2214/ajr.176.2.1760289. [DOI] [PubMed] [Google Scholar]
- 3.Cardis E, Vrijheid M, Blettner M, Gilbert E, Hakama M, Hill C, et al. The 15 country collaborative study of cancer risk among radiation workers in the nuclear industry: Estimates of radiation related cancer risks. Radiat Res. 2007;167:396–416. doi: 10.1667/RR0553.1. [DOI] [PubMed] [Google Scholar]
- 4.Committee to Assess Health Risks from Exposure to Low Levels of Ionizing Radiation. BEIR VII, Phase 2. xvi. Washington DC: National Academies Press; 2006. National Research Council (U.S.) Health risks from exposure to low levels of ionizing radiation; pp. 264–92. [PubMed] [Google Scholar]
- 5.Farahmand D, Hilmarsson H, Högfeldt M, Tisell M. Perioperative risk factors for short term shunt revisions in adult hydrocephalus patients. J Neurol Neurosurg Psychiatry. 2009;80:1248–53. doi: 10.1136/jnnp.2007.141416. [DOI] [PubMed] [Google Scholar]
- 6.Huda W, Atherton JV, Ware DE, Cumming WA. An approach for the estimation of effective radiation dose at CT in pediatric patients. Radiology. 1997;203:417–22. doi: 10.1148/radiology.203.2.9114097. [DOI] [PubMed] [Google Scholar]
- 7.Oxford: Pergamon Press; 1991. ICRP-60 Recommendations of the International Commission on Radiological Protection; pp. 42–94. [Google Scholar]
- 8.The 2007 recommendations of the International Commission on Radiological Protection. ICRP Publication 103. [Last accessed on 2012 Apr 22]. Availble from: http://www.icrp. org/docs/ICRP_Publication_103-Annals_of_the_ICRP_37%282-4%29- Free_extract.pdf . [DOI] [PubMed]
- 9.Pierce DA, Preston DL. Radiation-related cancer risks at low doses among atomic bomb survivors. Radiat Res. 2000;154:178–86. doi: 10.1667/0033-7587(2000)154[0178:rrcral]2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 10.Rybka K, Staniszewska AM, Bieganski T. Low-dose protocol for head CT in monitoring hydrocephalus in children. Med Sci Monit. 2007;13(Suppl 1):147–5. [PubMed] [Google Scholar]
- 11.Shrimpton PC, Hillier MC, Lewis MA, Dunn M. National survey of doses from CT in the UK. Br J Radiol. 2006;79:968–80. doi: 10.1259/bjr/93277434. [DOI] [PubMed] [Google Scholar]
- 12.Sodickson A, Baeyens PF, Andriole KP, Prevedello LM, Nawfel RD, Hanson R, et al. Recurrent CT, cumulative radiation exposure, and associated radiation-induced cancer risks from CT of adults. Radiology. 2009;251:175–84. doi: 10.1148/radiol.2511081296. [DOI] [PubMed] [Google Scholar]
- 13.Udayasankar UK, Braithwaite K, Arvaniti M, Tudorascu D, Small WC, Little S, et al. Low-dose nonenhanced head CT protocol for follow-up evaluation of children with ventriculoperitoneal shunt: Reduction of radiation and effect on image quality. Am J Neuroradiol. 2008;29:802–6. doi: 10.3174/ajnr.A0923. [DOI] [PMC free article] [PubMed] [Google Scholar]


