Abstract
Background:
An avalanche of literature exists on almost every aspect of lumbar disc pathology but very limited studies have quantified the diagnostic performance of elements of clinical examination in predicting disc level, meticulously collated the reflex changes in lumbar disc herniation (LDH) as well as assessed the diagnostic performance of the medial hamstring reflex (MHR). Our study underscores the diagnostic performance of the MHR in L5 radiculopathy comparing its diagnostic power to that of the knee and ankle reflexes.
Methods:
One hundred consecutive patients operated for de novo LDH in our department between January and December 2011 were prospectively followed-up. A nested case control study was designed from our cohort to assess the performance of the MHR in L5 sciatica. All patients were examined by two independent examiners pre-operatively for the MHR and the results collated and correlated to MRI and intra-operative findings.
Results:
The MHR has a diagnostic performance intermediate to that of knee and ankle reflexes. The percentages correctly classified were respectively: 86%, 79% and 67% for the knee, MHR and ankle reflexes. The MHR is highly precise with an intra-rater reliability of 100% and inter-rater repeatability of above 90% and test-retest reproducibility of 100%.
Conclusion:
The MHR hitherto described as elusive has a high diagnostic performance and is a valid neurologic test that should be included in the routine neurologic examination of patients with suspected L5 radiculopathy.
Keywords: Diagnostic performance, lumbar disc herniation, medial hamstring reflex
INTRODUCTION
Lumbar disc herniation (LDH) is one of the most common pathology encountered in routine neurosurgical practice. With a prevalence of 1-3%, LDH or its sequelae account for an important proportion of discomfort, debility and destitution.[10] The outlook of management of patients with LDH is heavily weighted on the right decision: “selecting the right patient, making the right diagnosis and giving the right treatment”.
The very impressive development of imaging techniques during recent decades has led to the increased prevalence of abnormal findings on imaging among asymptomatic subjects.[7] The implications of the latter are that a good clinical and radiological correlation and collation should be the lynchpin in patient selection.[8] A patient with LDH usually presents with a characteristic clinical picture of low back pain and/or radicular pain, sensory and/or motor deficit, reflex changes and presence of nerve root stretch signs. Occasionally they present with a cauda equina syndrome a veritable neurosurgical emergency.[10] The diagnostic accuracy of clinical findings individually or in combinations have been extensively investigated and confirmed.[3,5–7,9] Back pain while probably the most common symptom of herniated lumbar disc is perhaps the least useful symptom in making diagnosis because of its non-specificity and ubiquitousness in a wide array of spine pathologies. The sclerotomal distribution of radicular pain is generally the most informative individual neurological test though can be simulated or exaggerated by patients with pending litigation benefits.[3]
The dermatomal sensory deficits being dependent on the patient's interpretation is the most subjective portion of the neurologic examination with the results depending on the degree of patient's cooperation. The myotomal strength examination while less subjective, relies on the consistency of the patient's effort which can be limited by pain.[10]
The reflex examination is the least subjective portion of the neurologic examination. The diagnostic performance of the knee reflex for L3 and L4 femoralgia and ankle reflex for S1 sciatica are known accepted and routinely checked for during neurologic examination[4,9] but till date there is no consensus on an explorable reflex for L5 radiculopathy. Hence, the raison d'être of our study to collate and confirm the diagnostic value of the medial hamstring reflex in predicting L5 radiculopathy.
MATERIALS AND METHODS
Subjects: One hundred consecutive patients with an MRI diagnosed de novo herniated lumbar disc were examined pre-operatively for the reflex changes by two independent evaluators (EI and AM) without prior knowledge of the involved disc level. All patients underwent conventional open discectomy in our department of neurosurgery between January 2011 to December 2011 for a period of 12 months. Intra-operative findings of disc level were carefully recorded, considered as definite diagnoses-“gold standard” and collated with the preoperative clinical findings. Diagnostic test parameters were calculated using the conventional contingency tables.
Excluded from our study were patients with recurrent LDH or LDH with other associated spinal pathologies.
Technique of medial hamstring reflex Examination
The reflexes explored were: knee reflex for L3 and L4 femoralgia, ankle (Achilles ) reflex for S1 sciatica and the medial hamstring reflex for L5 radiculopathy.
The knee and ankle reflexes were tested for in the usually way[5] while the medial hamstring reflex (MHR) was tested for as follows:
With the patient in the Supine position, hip slightly flexed, externally rotated and abducted, the ipsilateral knee is semi flexed and supported by one of the examiner's hands. The reflex muscle contraction was elicited by striking the index finger of the supporting hand placed on the medial hamstring tendon (tendons of semitendinosus, semimembranosus) just above the knee join (postero-medially) with a reflex hammer. The normal response is contraction of the medial mass of hamstring muscles [Video 1]. Knee flexion is hardly observed because of friction between heel and couch. The action of the semimembranosus and semitendinosus muscles is to extend the hip joint, flex and internally rotate the knee. The MHR is mediated by the tibial portion of the sciatic nerve, primarily by the L5 nerve root and is the only deep tendon reflex useful in the evaluation of suspected L5 radiculopathy. It is shown that in the presence of symmetrically active gastrocsoleus reflexes, asymmetry of the hamstring reflexes indicates an L5 root lesion.[2] The tibialis posterior reflex another explorable reflex for L5 radiculopathy is limited by its occurrence only in 70% of Caucasians.[5] The adductor reflex-a pathologic reflex can be easily distinguished from the MHR.
Data was analyzed using STATA version 10.1.
This study was approved by Ethics Committee of our department of neurosurgery thus university.
RESULTS
One hundred patients were included in our study. Mean Age was 39.9 ± 9.7 Years [Min = 16 Years Max = 65 Years]. Male to female sex ratio was 3:2.
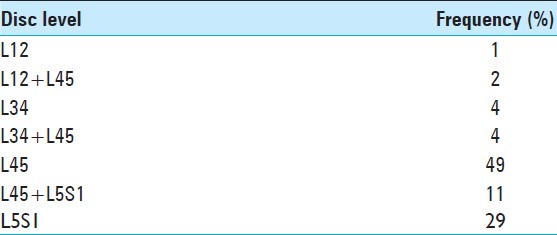
L45 herniated disc was the most common (66%) and L12 the least (3%)[Table 1].
Table 1.
Frequency of lumbar disc herniation by level
Reliability and validity
Reproducibility: The patients were examined by two independent examiners EI and AM and the degree of consistency in the measurement of the MHR between the two expressed using Kappa statistics. Intra-rater reliability was evaluated at 100% while the chance-adjusted measure of agreement-the inter-rater reliability was 93.9% (fixed-marginal Kappa statistics).
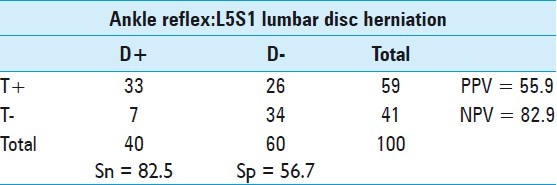
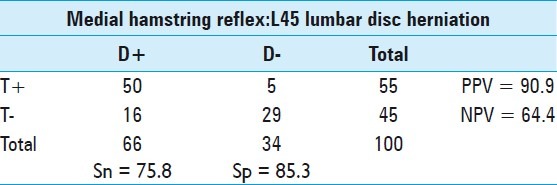
Validity: From the contingency table, [Tables 2–4] the sensitivity (Sn), Specificity (Sp), Positive Predictive Values (PPV) and Negative Predictive Values (NPV) were calculated to evaluate the accuracy of the MHR.
Table 2.
Decision matrix for knee reflex
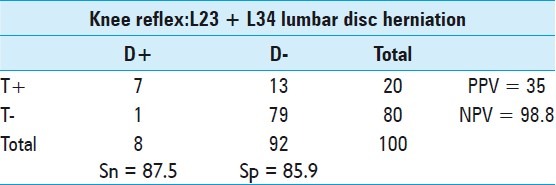
Table 4.
Decision matrix for ankle reflex
Decision matrix and diagnostic parameters
The prevalence of an L23 and L34 LDH was 8.0% (95% CI: 3.53% to 15.16%). Of the 8 patients (D+) with either an L23 or L34 LDH, the knee reflex had a sensitivity of 87.5% (95% CI: 47.4% to 97.9%) and specificity of 85.9% (95% CI:77.0% to 92.3%) in predicting the disc level. False negative prediction of level was observed in 12.5% and false positives in 14.1%. Of the 20 cases with a positive knee reflex (T+), disc herniation was confirmed at the corresponding level in only 35% (95% CI: 15.5% to 59.2%) (PPV) and in the 80 patients with a normal knee reflex (T-), 98.8% (95% CI: 93.2% to 99.8%) (NPV) had no corresponding disc pathology[Table 2].
From the 100 subjects, LDH at L45 level was present (D+) in 66 and absent (D-) in 34 cases. The MHR was positive (T + = Absent) in 55 and negative (T- = Normal reflex) in 45 cases. The prevalence of an L45 herniated disc was 66.0% (95% CI: 55.85% to 75.18%)
The respective Sn and Sp were 75.8% (95% CI: 63.6% to 85.4%) and 85.3% (95% CI: 68.93% to 94.99%). The PPV and NPV were 90.9% (95% CI: 80.03% to 96.95%) and 64.4% (95% CI: 48.78% to 78.12%) respectively [Table 3].
Table 3.
Decision matrix for medial hamstring reflex
L5S1 LDH compromises the traversing S1 nerve root and causes changes in Achilles' reflex. L5S1 was the second most affected disc level with a prevalence of 40% (95% CI: 30.33% to 50.28 %). The ankle reflex was positive in 33 of the 40 cases [Sn = 82.5% (95% CI: 67.21% to 92.63%)] and negative in 34 of 60 cases [Sp = 56.7% (95% CI: 43.24% to 69.41%)].
Of the 59 patients with a positive ankle reflex (reflex absent) 33 had an L5S1 herniated disc [PPV = 55.9% (95% CI: 42.40% to 68.84%)] and of the 41 patients without a positive ankle reflex (those with normal reflex) 34 didn't have a herniated disc [NPV = 82.9% (95% CI: 67.93% to 92.82%)].
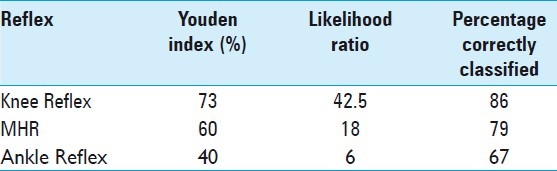
Because the concepts of sensitivity, specificity and predictive values are not easily conceived by non-statisticians we went an extra mile to produce summary statistics for diagnostic tests parameters to ease comprehensibility by computing the Youden Index (YI), Likelihood Ratios (LR), and Percentage Correctly Classified (PCC) [Tables 5–7].
Table 5.
Summary statistics: youden index
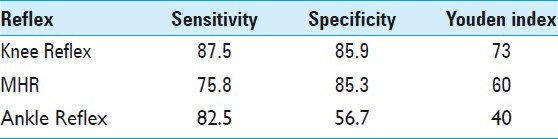
Table 7.
Summary of diagnostic parameters for knee, medial hamstring and ankle reflexes
Youden index[11]
The Youden Index (YI) is defined as:
YI = Sensitivity + Specificity -1. The higher the YI the better the diagnostic test. YI for the knee reflex was 73%, MHR was 60% and ankle reflex 40%[Table 5].
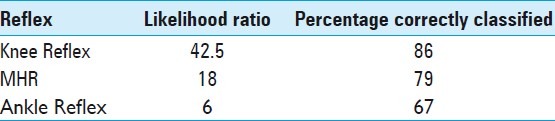
Likelihood Ratio: The Likelihood Ratio(LR) also calculated on the basis of sensitivity and specificity expresses how many times more or less likely the presence of an abnormal reflex (positive test = T+) occurs in patients with a herniated disc (D+) compared to patients with no disc herniation (D-).
The LR was 42.5 for the knee reflex, 18 for the MHR and 6 for the ankle reflex[Table 6].
Table 6.
Likelihood ratio and percentage correctly classified
Percentage correctly classified (Accuracy)
The reflex changes were present in the presence of a herniated disc and absent in its absence or in other words the percentage of patient of patients correctly classified was 86% for the knee reflex, 79% for the MHR and 67 for the ankle reflex [Table 7].
Summary statistics of parameters of diagnostic performance viz.: YI, LR and PCC rank the knee reflex to be the most predictive of the level of herniated disc followed by the medial hamstring reflex and lastly the Achilles' reflex.
DISCUSSION
History and physical examination, in tandem with radiological findings, provide the basis for the diagnosis of a herniated lumbar disc.[6] The diagnostic accuracy of clinical findings in herniated lumbar disc individually or in combinations have been extensively investigated, confirmed and reaffirmed in many studies but none has meticulously collated and quantified the diagnostic power of reflex changes.[9] While the knee and ankle reflexes are widely accepted explorable reflexes for the prediction of L3 - L4 and S1 radiculopathies, the reliability and validity of the medial hamstring reflex reported by Jensen [5] is still to be widely accepted by physicians. To elucidate on this time long ambiguity we scrupulously examined the knee, medial hamstring and ankle reflexes in patients with herniated lumbar disc and collated our findings to the gold standard which was intra-operative identification of the herniated disc. Lumbar disc herniation was chosen because it is the most homogenous of disc pathologies.
A common inherent characteristic of studies on diagnostic performance is “experimenter’s or examiner’s bias” resulting in inter-rater disagreement.[9] This was controlled and checked for in our study by restricting the examination to two independent investigators. The degree of precision or concordance was evaluated by calculating the inter-rater reliability which was at 94% - excellent enough for our results to be considered as reproducible. Cases of disagreement were re-examined by both investigators and the second inter-rater reliability was 100%. The intra-rater reliability was 100%. Test-retest reproducibility was 100% for the EI.
The validity of our findings was evaluated by computing for the sensitivity, specificity, predictive values and summary statistics presented as Youden Index, Likelihood Ratio and Percentage Correctly classified.
The Sensitivity and Specificity of the knee reflex was greatest at 87.5% and 85.9% respectively. This implies 87.5% of patients with herniated disc at L23 and L34 will have an abnormal knee reflex with only 12.5% of false negative results. Similarly, 85.9% of patients without a herniated disc at the above level will have a normal knee reflex, but 14% will have an abnormal reflex when there is no radiculopathy.
The Sensitivity of MHR (75.8%) is lower than that of ankle reflex (82.5%) but the specificity of MHR is higher (85.3%) than that of ankle reflex (56.7%). To determine which has a better performance we computed the Youden Index which is 60% for MHR and 40% for ankle reflex-thus the MHR has a higher performance than the ankle reflex. The corresponding YI for the knee reflex is 73%.
Also the Likelihood Ratio which expresses how many times more or less likely the presence of an abnormal reflex (positive test = T+) occurs in patients with a herniated disc (D+) compared to patients with no disc herniation (D-) was 42.5 for the knee reflex, 18 for the MHR and 6 for the ankle reflex [Figure 1].
Figure 1.
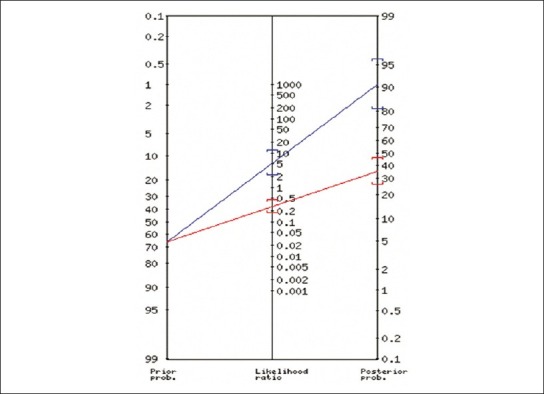
Likelihood Ratio Nomogram for the MHR [LR = LR+/ LR- (=5.15/0.28 = 18)
As regards the predictive values , amongst patients with abnormal reflexes, only 35% had a corresponding herniated disc for knee reflex, 90.9% had an L45 LDH for MHR and 55.9% an L5S1 for ankle reflex. The highest Positive Predictive Value of the MHR for L5 radiculopathycould be explained by the high prevalence of L45 herniated disc. The predictive value is affected by the prevalence of the disease unlike sensitivity and specificity which are intrinsic characteristics of a diagnostic test and are unaffected by the disease prevalence. Contrariwise, the negative predictive values (NPV) were 98.8% for the knee reflex, 64.4% for the MHR and 82.9% for the ankle reflex. This means that amongst patients with a normal reflex, 98.8% with a normal knee reflex will not harbor an L3 or L4 radiculopathy, 82.9% with a normal ankle reflex will not have S1 sciatica but only 64.4% with a normal MHR wouldn't be having an L5 radiculopathy. Jensen found PPV of an abnormal MHR as a sign of herniation from the fourth lumbar disc to be 85-89% and the NPV to be 51-61%. The corresponding values for an abnormal Achilles tendon reflex as a sign of herniation from the fifth lumbar disc were 67-84% and 79-84%, respectively.[5] Our results corroborate his findings but differ from those of Vroomen et al. whom in their review expressed the non-sensitivity of depressed reflexes in patients with herniated disc especially the knee reflex. Their review also outlined the disagreement regarding the high specificity of the knee and ankle reflexes but made no mention of the MHR.[9] Interpreting the Sn, Sp, YI, LR, PPV and NPV of a diagnostic test can be confusing but when we assess the percentage of patients correctly classified by our diagnostic tests parameters, viz.: the patients having an abnormal reflex when the herniated disc is present and a normal reflex when there is no pathology; we can sum up that the diagnostic power of the knee reflex is greatest followed by that of the MHR and the least being that of the ankle reflex they respectively correctly classify 86%, 79% and 67% of the patients.
In toto, the MHR is a precise neurologic test in the level diagnosis of L5 radiculopathy as its reproducibility has been demonstrated in its high intra-/inter-rater reliability. Its validity is incontestable as evidenced in its diagnostic tests characteristics with an accuracy intermediate to that of knee and ankle reflexes. The validity of these findings couldn’t have been observed by the sheer “luck of draw”, some systematic error or due to some confounding factor. This has been statistically illustrated by our adequate sampling and narrow confidence interval. The repeatability of our findings by different examiners at different times rules out any experimenter's bias. Stratified analysis fails to reveal any confounders or effect modifiers.
This valid clinical and statistical association between the L5 radiculopathy and the MHR can thus be judged as one of causality and our findings are generalizable because:
The association between the presence of an L5 radiculopathy and MHR abnormality is strong! (YI = 60%, LR = 18 and Accuracy = 79%)
There exists a sound biological credibility from the anatomical and physiological data on the reflexology of MHR.[2,5]
Our results are consistent with those of previous series[1,2,5]
Evidence of dose-response relationship was easily demonstrated by the unilaterality of an abnormal reflex to the side of the pathology.[2]
CONCLUSION
We have proven that the medial hamstring reflex is precise and accurate in predicting radiculopathy of the fifth lumbar nerve root (L5). The Medial Hamstring Reflex should thus be formally included in the routine neurologic examination of a patient with a suspected L5 radiculopathy.
Video available at www.surgicalneurologyint.com
Footnotes
Available FREE in open access from: http://www.surgicalneurologyint.com/text.asp?2012/3/1/104/100862
Contributor Information
Ignatius Ngene Esene, Email: esenengene@yahoo.co.uk.
Abdalla Meher, Email: demerdash.list@gmail.com.
Mohamed A. Elzoghby, Email: maelzoghby@yahoo.com.
Khaled El-Bahy, Email: khaledbahy@yahoo.com.
Ali Kotb, Email: alikotb@gmail.com.
Adel El-Hakim, Email: dr_a_elhakim@yahoo.com.
REFERENCES
- 1.Calmels P, Minaire P. Does asymmetric hamstring reflex indicate L5 radicular lesion? Presse Med. 1986;15:1422–3. [PubMed] [Google Scholar]
- 2.Felsenthal G, Reischer MA. Asymmetric hamstring reflexes indicative of L5 radicular lesions. Arch Phys Med Rehabil. 1982;63:377–8. [PubMed] [Google Scholar]
- 3.Hancock MJ, Koes B, Ostelo R, Peul W. Diagnostic accuracy of the clinical examination in identifying the level of herniation in patients with sciatica. Spine (Phila Pa 1976) 2011;36:E712–9. doi: 10.1097/BRS.0b013e3181ee7f78. [DOI] [PubMed] [Google Scholar]
- 4.Jensen OH. The level-diagnosis of a lower lumbar disc herniation: The value of sensibility and motor testing. Clin Rheumatol. 1987;6:564–9. doi: 10.1007/BF02330594. [DOI] [PubMed] [Google Scholar]
- 5.Jensen OH. The medial hamstring reflex in the level-diagnosis of a lumbar disc herniation. Clin Rheumatol. 1987;6:570–4. doi: 10.1007/BF02330595. [DOI] [PubMed] [Google Scholar]
- 6.Poiraudeau S, Foltz V, Drapé JL, Fermanian J, Lefèvre-Colau MM, Mayoux-Benhamou MA, et al. Value of the bell test and the hyperextension test for diagnosis in sciatica associated with disc herniation: Comparison with Lasègue's sign and the crossed Lasègue's sign. Rheumatology (Oxford) 2001;40:460–6. doi: 10.1093/rheumatology/40.4.460. [DOI] [PubMed] [Google Scholar]
- 7.Reihani-Kermani H. Correlation of clinical presentation with intra-operative level diagnosis in lower lumbar disc herniation. Ann Saudi Med. 2004;24:273–5. doi: 10.5144/0256-4947.2004.273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Van Rijn JC, Klemetso N, Reitsma JB, Majoie CB, Hulsmans FJ, Peul WC, et al. Symptomatic and asymptomatic abnormalities in patients with lumbosacral radicular syndrome: Clinical examination compared with MRI. Clin Neurol Neurosurg. 2006;108:553–7. doi: 10.1016/j.clineuro.2005.10.003. [DOI] [PubMed] [Google Scholar]
- 9.Vroomen PC, de Krom MC, Knottnerus JA. Diagnostic value of history and physical examination in patients suspected of sciatica due to disc herniation: A systematic review. J Neurol. 1999;246:899–906. doi: 10.1007/s004150050480. [DOI] [PubMed] [Google Scholar]
- 10.Wolfla CE. Principles of neurosurgery. In: Rengachary SS, Ellenbogen RG, editors. Principles of neurosurgery. Philadelphia, USA: ElsevierMosby; 2005p. pp. 752–62. [Google Scholar]
- 11.Youden WJ. Index for rating diagnostic tests. Cancer. 1950;3:32–5. doi: 10.1002/1097-0142(1950)3:1<32::aid-cncr2820030106>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


