Abstract
Introduction:
The prevalence of major depressive disorders is higher among persons with diabetes compared to the general population. These associations may be related to the increased risk of depressive symptoms in individuals with diabetes, increased risk of type 2 diabetes (T2DM) in individuals with depressive symptoms, or both.
Objectives:
To study the association of depression with diabetes and its complications in newly diagnosed type 2 diabetes in eastern UP.
Material and Methods:
Sixty cases and an equal number of age- and sex-matched controls were assessed for depression, diabetes complications, and a demography profile.
Results:
Depression was found in 26 (43.34%) cases, while it was present in only eight (13.33%) controls (P = 0.002). Depression correlated with the level of hyperglycemia at presentation, as measured by fasting and postprandial blood glucose (FBG and PPBG) values. The presence of diabetic nephropathy was significantly associated with depression, while the prevalence of other complications of diabetes (retinopathy and dyslipidemia), although higher among those with depression, was not statistically significant. The level of HbA1c was 8.56 ± 1.66 in the depressed versus 8.04 ± 1.88 in the non-depressed diabetics (P = 0.26).
Conclusions:
The association of depression with diabetes and its complications in newly diagnosed type 2 diabetics was highlighted in our subpopulation and emphasized the need for integrated health services. The prevalence of depression was higher among them compared to controls. The chances of becoming depressed increased as the diabetes complications worsened.
Keywords: Depression, diabetes complications, type 2 diabetes
INTRODUCTION
The prevalence of clinical depression and presence of elevated depressive symptoms are higher among persons with diabetes compared to the general population. This association may be bidirectional.
Newly diagnosed diabetics suffer not only from somatic symptoms of the disease, but also from indisposition due to lifestyle alteration, which can possibly cause depressive emotions in the initial stage of diagnosis. Negative emotions can cause stress in diabetic patients, while a series of adverse hormones increase, they reduce the sensitivity of insulin and induce insulin resistance. Negative emotions can adversely affect glucose control or the quality of life and should be detected early to be intervened.
The present study was conducted with the aim of studying the association of depression with diabetes and its complications in newly diagnosed type 2 diabetics and to compare its prevalence with age- and sex-matched healthy controls.
MATERIAL AND METHODS
This single point cross-sectional case control study was conducted at a tertiary care hospital from August 2010 to July 2011. Cases were selected as per the American Diabetes Association (ADA) 2007 Guidelines and were newly diagnosed (≤ 3 months since diagnosis) subjects who gave consent for the study.
The control group comprised of age- and sex-matched normal healthy volunteers.
Diabetic patients with other predisposing factors for depression such as other chronic diseases, disability, other major psychiatric illness, those with recent stressful and psychological causes of depression, and patients with gross cognitive deficit were excluded from the study.
Screening was done in each patient to assess the associated depression using the DSM–IV TR criteria and severity was assessed using the Beck Depression Inventory (BDI). Those having difficulty in understanding the English language were given assistance in the form of literal translation of BDI in the local language, without modifying the basic tool. A BDI score of 11 – 16 was taken as mild; 17 – 30 as moderate, and more than 30 as severe depression. The control subjects were from the same socioeconomic background, to minimize possibility of any bias. A complete physical and mental examination was done and they were assessed on the aforementioned parameters in the same way as was done for the patient group.
Cases and controls were investigated for their diabetic status; cases were also investigated for complications of diabetes and then BDI was applied. Then the data was analyzed with the appropriate statistical methods. Chi Square test and Two Sample Proportion Tests were used to calculate the P value.
RESULTS
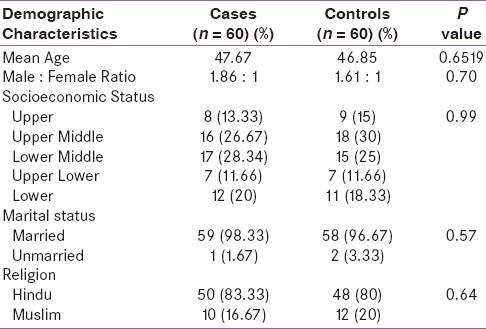
Mean age of cases was 47.67 ± 9.78 years and mean age of controls was 46.85 ± 10.08 years. Among the cases 65% were males and 35% were females. Male : female ratio was 1.86 : 1. Among the controls 61.66% were males and 38.33% were females with a male : female ratio of 1.61 : 1. On statistical analysis it was found that both groups were age- and sex-matched (P = 0.6519 for age and 0.70 for gender distribution). Similarly they were matched regarding other demographic data like socioeconomic status (P = 0.99), marital status (P = 0.57), and religion (P = 0.64) [Table 1].
Table 1.
Demographic characteristics of the study population
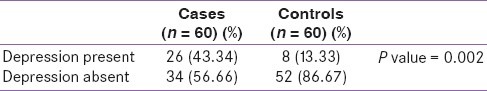
Out of the 60 newly diagnosed diabetics, depression was found in 43.34%, while it was present in only 13.33% out of 60 age- and sex-matched healthy controls (P = 0.002) [Table 2].
Table 2.
Status of depression in cases and controls
Mild-to-moderate depression was present in 69.33% of the cases and 87.5% of the controls. Severe depression was present in 30.77% of the cases and 12.5% of the controls. Among the cases, 42.85% of the females and 43.58% of the males had depression. Similarly, among the controls, 13.04% of the females and 13.51% of the males had depression. Thus, in our study there was no significant difference among the cases and controls regarding the gender distribution of depression.
The mean FPG of the diabetics was 161.76 ± 39.31 mg / dl while the mean PPBG value was 230.1 ± 47.43 mg / dl. The average HbA1c of the cases was 8.26 ± 1.79%.
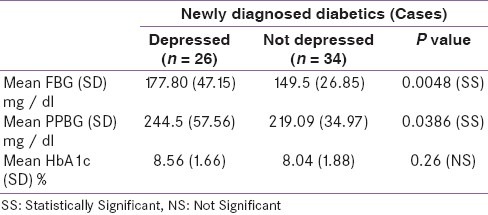
Among those diabetics who were found to be depressed, the average values of FBG, PPBG, and HbA1c were 177.80 ± 47.15 mg / dl, 244.50 ± 57.56 mg / dl, and 8.56 ± 1.66%, respectively, while among the non-depressed diabetics, the same values were 149.5 ± 26.85, 219.09 ± 34.97 mg / dl, and 8.04 ± 1.88%, respectively [Table 3]. Although the levels of all the three parameters (FBG, PPBG, and HbA1c) were higher in the depressed individuals as compared to the non-depressed individuals, the difference was significant only for FBG (P = 0.0048) and PPBG (P = 0.0386), but not for HbA1c (P = 0.26).
Table 3.
Glycemic status of newly diagnosed diabetics
The presence of diabetic complications among those with depression versus those without depression is shown in Table 4. Microalbuminuria was present in 61.66% of the newly diagnosed diabetics. Thus, a majority of diabetics had evidence of nephropathy even at diagnosis; 80.76% diabetics having depression had microalbuminuria at diagnosis, while only 47.05% of the non-depressed diabetics had microalbuminuria (P = 0.0078). Thus, positive urine microalbumin was significantly associated with depression in newly diagnosed type 2 diabetics.
Table 4.
Presence of complications in depressed versus non-depressed newly diagnosed diabetics
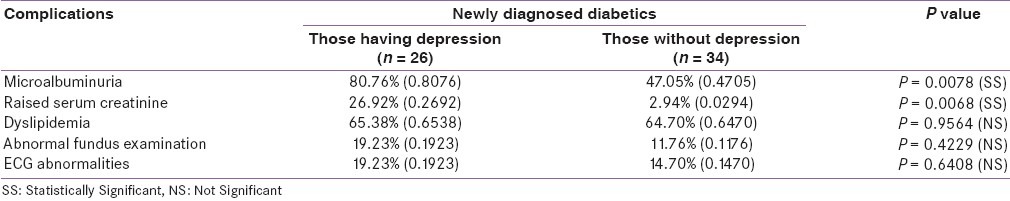
Serum creatinine was raised in 13.33% of the cases, among which 26.92% of the cases having depression had raised serum creatinine, while only 2.94% of the cases who had no depression had raised creatinine (P = 0.0068). Thus, raised serum creatinine was also significantly associated with depression in the cases.
Dyslipidemia was present in 65% of the cases; 65.38% of the cases having depression had dyslipidemia, while 64.70% of the cases who were without depression had dyslipidemia (P = 0.9564). Thus, dyslipidemia was not significantly associated with depression in the study population.
Abnormal retinal findings were present in 15% of the cases. Among the depressed diabetics 19.23% had abnormal fundus examination, while among those who did not have depression, 11.76% had abnormal fundus (P = 0.4229). Thus, diabetic retinopathy was not significantly associated with depression in newly diagnosed type 2 diabetics.
Electrocardiographic abnormalities such as ST-T changes were present in 16.67% of the cases. Among depressed diabetics, 19.23% had abnormal electrocardiograms (ECG), while among those not having depression, 14.70% had ECG abnormalities (P = 0.6408).
DISCUSSION
In the present study the prevalence of depression in newly diagnosed cases of T2DM was 43.34%, while in normal healthy controls it was 13.33%. Most studies looking for such an association have been done in diabetics, irrespective of the duration since diagnosis. Very few studies have focused on newly diagnosed diabetics. Asghar et al.[1] found evidence of depressive symptoms in 29% of the males and 30.5% of the females, with newly diagnosed diabetes. Perveen et al.[2] also found significantly higher prevalence of depression among diabetics compared to non-diabetics, while Yu et al.[3] found that 28% newly diagnosed diabetics in their study had depression. Raval et al.[4] evaluated 300 diabetic patients for depression, irrespective of the duration of diabetes, and found that 41% of the diabetics had depression. In a study by Sotiropoulos et al.[5] 33.4% type 2 diabetic subjects reported elevated depressive symptoms. Zahid et al.[6] found that depression prevalence was 14.7% among those with diabetes as opposed to 4.9% among those without diabetes, in a rural area of Pakistan. Khamseh et al.[7] conducted a hospital-based prospective study and found major depression in 71.8% of a sample of 206 Iranian patients with diabetes. Ali et al.[8] found that the prevalence of depression was significantly higher among patients with T2DM (17.6%) compared to those without diabetes (9.8%).
Various Indian studies have reported prevalence rates of depression that vary from 9 – 83% in primary care practices.[9–13] There are few population-based studies from India. Most studies have been carried out on selected groups. The Chennai Urban Rural Epidemiology Study,[14] which is the largest population-based study from India, to report on prevalence of the depression, showed that among urban south Indians, the prevalence of depression was 15.1%. The presence of depression in 13% of the healthy controls in the present study correlated with the above-mentioned studies. The prevalence of depression in 43% of the newly diagnosed diabetics correlated with the meta-analyses of several studies done by Anderson et al.[15] , who reported the prevalence of depression in diabetes ranging from 8 to 61%. Similarly all the above-mentioned studies concluded that depression was significantly associated with diabetes. However, a study by Brown and colleagues,[16] which also considered newly diagnosed diabetics in their study, did not find any relation between the two.
In the present study it was also found that the glycemic status was worse among those having depression compared to non-depressed diabetics. Similar findings were noted by Yu et al.,[3] who also found that the mean FBG and HbA1c among depressed diabetics was significantly higher than in non-depressed diabetics. Larijani et al.[17] also correlated hyperglycemia with depression. In the present study, although the level of all the three parameters FBG, PPBG, and HbA1c were higher in depressed individuals, as compared to non-depressed individuals, the difference was significant only for FBG and PPBG, but not for HbA1c. Raval et al.,[4] in their study, also showed no significant association with HbA1c.
Various studies have also noted an association between diabetic complications and depression. In the present study it was also found that among patients of newly diagnosed T2DM, the majority of those having nephropathy (screened by microalbuminuria and serum creatinine) also had significantly associated depression (P = 0.0078 for microalbuminuria and P = 0.0068 for serum creatinine). However, the relation between dyslipidemia, retinopathy, or ECG abnormalities and depression was not significant. Yu et al. also found a significant association between microalbuminuria and depression in newly diagnosed diabetics, whereas, Raval et al. found that significant risk factors associated with depression in type 2 diabetes included age, socioeconomic status, waist circumference, neuropathy, nephropathy, microvascular and macrovascular complications, diabetic foot, peripheral vascular disease (PVD), and a greater pill burden. However no significant risk was attributed to gender, HbA1c, dyslipidemia, retinopathy, blood pressure, or BMI.
One of the major strengths of our study is its matched case control design, which controlled two fundamental confounders of age and sex, at the design stage. Cases were recruited on the basis of diabetic status measured by objective laboratory values, which avoided selection biases. Both cases and controls were selected from the same source population, so they were representative of the source population with respect to depression within age- and sex-matched strata. It achieved the goal of unbiased controls. Finally, the screening tool used for depression exclusively screened out depression, thus avoiding false-positive results due to anxiety and somatic symptoms.
Limitations of the study: Because of the stringent selection criteria, the sample size was small, and hence, the results were subjected to Type II error and they could not be generalized. The study was a cross-sectional study, and to further assess the effects of the diabetic disease process over mental status, longitudinal studies were needed. In this study, the differences noted compared to the previous studies might be because of the small sample size.
CONCLUSIONS
In newly diagnosed type 2 diabetics, the prevalence of depression was significantly higher as compared to age- and sex-matched healthy controls. The presence of depression correlated with the level of hyperglycemia at presentation, as measured by the FBG and PPBG values. The presence of diabetic nephropathy was significantly associated with depression. The prevalence of other complications of diabetes (retinopathy, dyslipidemia, or ECG abnormalities) was found to be higher among those with depression. Therefore, the association between T2DM and depression was epidemiologically associated even in our subpopulation, highlighting the integrated management protocols between various specialities and psychiatric management helping the overall prognosis.
Screening for depression by a self-scored questionnaire may be easily carried out, even in a busy clinic. Treating depression with psychotherapy, medication, or a combination of these treatments may improve the patients’ well-being and ability to manage symptoms of both diseases, thus, improving the quality of their lives as well as providing disease-free longevity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Asghar S, Hussain A, Ali SM, Khan AK, Magnusson A. Prevalence of depression and diabetes: A population-based study from rural Bangladesh. Diabet Med. 2007;24:872–7. doi: 10.1111/j.1464-5491.2007.02136.x. [DOI] [PubMed] [Google Scholar]
- 2.Perveen S, Otho M, Siddiqi M, Hatcher J, Rafique G. Association of depression with newly diagnosed type 2 diabetes among adults aged between 25 to 60 years in Karachi, Pakistan. Diabetol Metab Syndr. 2010;2:17. doi: 10.1186/1758-5996-2-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yu R, Y-Hua L, Hong L. Depression in newly diagnosed type 2 diabetes. Int J Diabetes Dev Ctries. 2010;30:102–4. doi: 10.4103/0973-3930.62601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 5.Sotiropoulos A, Papazafiropoulou A, Apostolou O, Kokolaki A, Gikas A, Pappas S. Prevalence of depressive symptoms among non insulin treated Greek type 2 diabetic subjects. BMC Res Notes. 2008;1:101. doi: 10.1186/1756-0500-1-101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zahid N, Asghar S, Claussen B, Hussain A. Depression and diabetes in a rural community in Pakistan. Diabetes Res Clin Pract. 2008;79:124–7. doi: 10.1016/j.diabres.2007.07.006. [DOI] [PubMed] [Google Scholar]
- 7.Khamseh ME, Baradaran HR, Rajabali H. Depression and diabetes in Iranian patients: A comparative study. Int J Psychiatry Med. 2007;37:81–6. doi: 10.2190/FP64-82V3-1741-842V. [DOI] [PubMed] [Google Scholar]
- 8.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 9.Kishore J, Reddaiah VP, Kapoor V, Gill JS. Characteristics of mental morbidity in a rural primary health center of Haryana. Indian J Psychiatry. 1996;38:137–42. [PMC free article] [PubMed] [Google Scholar]
- 10.Amin G, Shah S, Vankar GK. The prevalence and recognition of depression in primary care. Indian J Psychiatry. 1998;40:364–9. [PMC free article] [PubMed] [Google Scholar]
- 11.Pothen M, Kuruvilla A, Philip K, Joseph A, Jacob KS. Common mental disorders among primary care attenders in Vellore, South India: Nature, prevalence and risk factors. Int J Soc Psychiatry. 2003;49:119–25. doi: 10.1177/0020764003049002005. [DOI] [PubMed] [Google Scholar]
- 12.Nambi SK, Prasad J, Singh D, Abraham V, Kuruvilla A, Jacob KS. Explanatory models and common mental disorders among patients with unexplained somatic symptoms attending a primary care facility in Tamil Nadu. Natl Med J India. 2002;15:331–5. [PubMed] [Google Scholar]
- 13.Bromet E, Andrade LH, Hwang I, Sampson NA, Alonso J, de Girolamo G, et al. Cross-national epidemiology of DSM-IV major depressive episode. BMC Med. 2011;9:90. doi: 10.1186/1741-7015-9-90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Poongothai S, Pradeepa R, Ganesan A, Mohan V. Prevalence of depression in a large urban South Indian population — The Chennai Urban Rural Epidemiology study (CURES – 70) PLoS One. 2009;4:e7185. doi: 10.1371/journal.pone.0007185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: A meta-analysis. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 16.Brown LC, Majumdar SR, Newman SC, Johnson JA. Type 2 diabetes does not increase risk of depression. CMAJ. 2006;175:42–6. doi: 10.1503/cmaj.051429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Larijani B, Bayat MK, Gorgani MK, Bandarian F, Akhondzadeh S, Sadjadi SA. Association between depression and diabetes. German J Psychiatry. 2004;7:62–5. [Google Scholar]


