Abstract
Context:
Type 2 diabetes mellitus doubles the odds of suffering from depressive illness. Co-morbid depression is associated with poorer outcomes in diabetes mellitus in terms of glycemic control, medication adherence, quality of life, physical activity, and blood pressure control.
Aim:
The present study aims to estimate the prevalence of depression among a consecutive group of patients with type 2 diabetes and assess its impact on glycemic and blood pressure control.
Setting:
Outpatient department of the endocrinology department of a university affiliated teaching hospital in north India.
Subjects:
Consecutive adult patients (18–65 years) with type 2 diabetes mellitus of over 5-year duration with no prior history of psychiatric illnesses or intake of anti-depressants.
Materials and Methods:
A semi-structured questionnaire was used for demographic data, HbA1c was obtained to assess glycemic control, and blood pressure was recorded twice during patient interview to assess blood pressure control. Depression was assessed with the Major Depression Inventory and scores obtained were classified as consistent with mild, moderate and severe depression. Data was analyzed with SPSS v16, and multiple logistical regression test was done to compare the effect of depression on glycemic control after adjusting for age and sex.
Results:
Of the 80 patients interviewed, 31 (38.8%) had depressive symptoms. Among them 20 (25%) had mild depression, 10 (12.5%) had moderate depression, and 1 (1.3%) had severe depression.
Conclusions:
Over one third of patients with type 2 diabetes mellitus of over 5-year duration had depressive symptoms. The presence of depressive symptoms was associated with a significant worsening of glycemic control.
Keywords: Depression, glycemic control, HbA1c, type 2 diabetes mellitus
INTRODUCTION
The growing burden of non-communicable diseases (NCDs) constitutes of the major challenges facing our country in the present century. The NCD's include heart diseases, stroke, mental health disorders, diabetes mellitus, and cancers. Among these the prevalence of type 2 diabetes mellitus is steadily increasing in our country with estimates of 8–15% in urban areas.[1]
Depression has been bi-directionally associated with diabetes mellitus.[2] Subjects who are depressed are more likely to develop type 2 diabetes mellitus either because of the metabolic abnormalities caused by the drugs used to treat depression or because of poor food choices and lack of physical activity that may accompany major depressive episode.[3] Among the anti-depressants, the ones that have non-adrenergic activity are the ones with the highest potential to cause metabolic abnormalities.[4]
Patients suffering from diabetes mellitus are also at a higher risk of being diagnosed with depression compared to normal population. This prevalence of depression among subjects with diabetes mellitus ranges from 12% to 28% in various studies.[5–7] A large meta-analysis by Andersen et al. in 2001 incorporating data from 42 studies concluded that the presence of diabetes doubles the odds of having co-morbid depression.[8]
In addition to the morbidity associated with the disease itself, the presence of depression complicates outcomes in the management of diabetes mellitus. Patients with co-morbid depression are more likely to have poor control of hyperglycemia in both type 1 and 2 diabetes mellitus.[9] Depression is also associated with poor adherence to diabetic medications and dietary regimes. There is also lesser physical activity, reduced quality of life, and increased heath care expenditure in patients with diabetes and depression.[10–14]
The purpose of this study was to assess the prevalence of depression among patients with type 2 diabetes mellitus of at least 5-year duration attending the diabetic outpatient clinic in the tertiary hospital. Depression was correlated the glycemic and blood pressure control.
MATERIAL AND METHODS
Setting
The study was done in the Endocrinology out-patient clinic of a tertiary care, university affiliated teaching hospital in North India.
Subjects
Consecutive adult patients (18–65 years) with type 2 diabetes mellitus of at least 5-year duration attending the endocrine-diabetes outpatient clinics of a tertiary hospital were recruited for the study. Patients with self-reported preexisting psychiatric illness or currently taking anti-depressants were excluded. Informed consent was obtained before study-related procedures.
Clinical evaluation
Anthropometric examination was made and demographic data of the patient was collected on a semi-structured questionnaire. Glycosylated hemoglobin (HPLC, Bio-rad) was noted from the charts. Blood pressure was measured on the day of the interview on two occasions once before the interview and once after 15 min apart with a mercury sphygmomanometer.
Glycemic control was optimal if the HbA1c was ≤7% and suboptimal if it was between 7.1% and 8.0% and considered poor if the HbA1c was greater than 8.1%.
Assessment of blood pressure was based on American Diabetes Association guidelines for optimal blood pressure treatment goals in patients with Diabetes.[15]
Depression assessment
The major depression inventory (MDI) was used to assess depression. The score obtained was used for the diagnosis and classification into mild, moderate, and severe depression.[16] This tool is reported to be as valid as the more common self-reported instruments like Becks Depressive Inventory.[17] The items on this inventory are measured in frequency using the past 2 weeks as the time frame. Each item is scored on the Likert scale from 0 to 5. The scores are interpreted and can be used as a diagnostic instrument as per the Diagnostic and Statistical Manual of Mental Disorders IV ed. 2000 (DSM-IV).
Statistical analysis
Data was analyzed using the statistical software SPSS version 16. Continuous variables were expressed as means and standard deviation. Univariate analysis was done to compare the effects of depression on glycemic control (HbA1c) and blood pressure. Multiple linear regression was used to compare the effect of depression on glycemic control after adjusting for age and sex. A P-value ≤0.05 was considered statistically significant.
The Ethics committee of the Institution approved the study protocol prior to any study-related procedures.
RESULTS
Eighty patients were enrolled for the study from the clinic. The mean age of the subjects was 54.8 (SD 10.3) years. There were 32 (47.5%) men and 42 (52.5%) women. All of them had diabetes mellitus for a minimum of 5 years.
The mean HbA1c among all the patients was 9.5% (SD ± 1.80). Only 5% (n = 4) of patients among the 80 achieving the HbA1c targets of ≤ 7%. Another 17.5% (n = 14) had suboptimal control and the remaining 77.5% (n = 62) had poor control of glycemia at the time of the study interview.
Thirty-one (38.8%) out of 80 subjects recruited had some degree of depression to suggest a diagnosis based on scores obtained from the MDI. Among them 20 (25%) had mild depression, 10 (12.5%) had moderate depression, and 1 (1.3%) had severe depression.
The clinical data among the patients with depression and those without are summarized in Table 1.
Table 1.
The clinical data among the patients with depression and those without depression
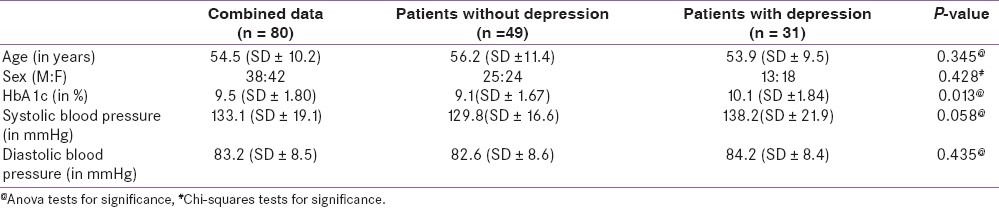
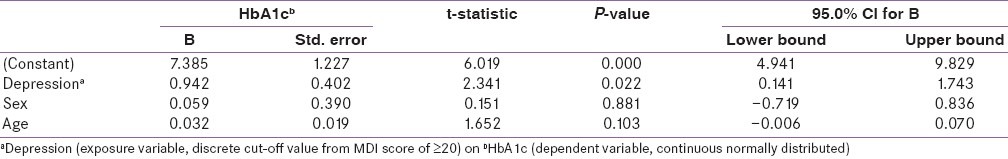
Table 2 shows the multiple linear regression model of the effect of depression on glycemic control (HbA1c) after controlling for age and sex. The multiple linear regression models showed that the presence of depression increased HbA1c by an average of 0.94% after adjusting for age and sex. This increase was statistically significant (P = 0.022).
Table 2.
Multiple linear regression model of the effect of depression on glycemic control (HbA1c) after controlling for age and sex
DISCUSSION
The study which included 80 patients with type 2 diabetes mellitus of over 5-year duration attending an Indian tertiary hospital in North India showed a prevalence of depression in over one third (39%) of the patients interviewed. Although a majority of those with depressive symptoms had only mild depression, the presence of these symptoms was significantly associated with higher HbA1c at the time of interview.
The prevalence of depression in our study was much higher than what was observed in other western studies primarily because we have only included patients with at least 5-year duration of disease. A recent study from north India by Blahara et al. found only 16% of patients with type 2 diabetes had depression as measured by the hospital anxiety depression score (HADS). This study included all patients with type 2 diabetes, regardless of the duration of the disease.[18] However our study is consistent with results seen in another study done in India by Raval et al. in which 41% of patients were diagnosed to have depression again in a similar setting in North India.[19] A much higher prevalence of depression (44%) was seen among type 2 diabetic patients in Pakistan in a recent study by Khawja et al. in 2010.[20]
The prevalence figure of depressive illness among patients with diabetes is relatively lower in western studies. This could in turn be related to recruitment of patients from primary practices in western studies while most of the studies done in India have recruited patients from clinics in tertiary hospital who would be suffering from more co-morbidity and more complications related to diabetes.[21–23]
One of the primary endpoints of the present study was to determine the co-relation of depression with metabolic control. Good metabolic control was defined as per the standards given by the American Diabetes Association in 2011.[17] However, the majority of patients recruited for the study did not meet the glycemic target of HbA1c <7%. Hence, there was no statistically significant difference between the percentages of patients achieving optimal glycemic control in the two groups of patients. However, when we analyzed the data with regards to the actual HbA1c values there were statistically significant differences between the patients exhibiting depressive symptoms and those that did not. There was average difference of HbA1c of 1% (9.1% vs. 10.1%, P = 0.013) between the two groups. This difference was maintained when logistical regression was done for the possible confounding effects of age and sex.
This was consistent with findings in other studies were authors have found an impact of co-morbid depression on glycemic control in diabetes. Skaff et al. after evaluating 206 patients showed that mood changes were acutely associated with higher blood glucose value. In their study, a daily negative mood was associated with high fasting blood glucose values the very next day (r = 0.17; P < 0.05).[24] A prospective study done by Eren et al. on the clinical impact of depressive episodes on glycemic control showed that the number of depressive episodes correlated with a higher HbA1c in a group of 104 Turkish patients with type 2 diabetes mellitus.[25] Another longitudinal study done among American veterans by Richardson et al., the authors observed a higher HbA1c among patients with depression at all time points compared to patients without depression.[26] The difference between the two groups was however small (0.13%, 95% CI [0.03–0.22] P < 0.05) compared to our study were the difference was much larger. This larger difference would be explained by the fact that patients at baseline had poorer blood glucose control irrespective of the presence of depressive symptoms.
Our study showed slightly higher values of systolic and diastolic blood pressure among patients who were depressed compared to those who were not depressed. Both these clinical outcomes were not statistically significant. This is consistent with the a large community-based study of over 3700 patients were there was no difference in systolic blood pressure and cholesterol levels in patients with diabetes in the presence of depression.[27]
The main limitation of this study is the small numbers of patients studied and the large number of patients who at baseline did not have good sugar control. Despite the small number, there are clearly a third of patients who suffer from depressive symptoms and in turn this significantly impacts their glycemic control.
Studies have shown that intervention in this group of patients with pharmacotherapy for depression in the either the primary care or hospital-based settings improved the likelihood of depressed patients reaching glycemic targets.[28,29] Even in a primary care setting, a minimal intervention requiring three visits and pharmacotherapy of depression by the primary care physician rather than by hospital-based specialists resulted in significant improvements in glycemic control (HbA1c <7%. 60.9% vs. 35.7% in usual care) and improved medication adherence. This is in addition to the improvement in quality of life because of decrease in depressive symptoms.[30]
CONCLUSIONS
This study adds to the data about the prevalence of depression among patients with type 2 diabetes mellitus. It affects over one third of patients with duration of disease more than 5 years. Co-morbid depression is significantly associated with higher HbA1c. Early diagnosis of depression and intervention in patients with type 2 diabetes mellitus makes metabolic control easier and more likely.
Footnotes
Source of Support: The first author received an ICMR- Short Term Studentship Award to complete this work
Conflict of Interest: None declared.
REFERENCES
- 1.Gupta R, Misra A. Type 2 Diabetes in India: Regional Disparities. Br J Diab Vasc Dis. 2007;7:12–6. [Google Scholar]
- 2.Golden SH, Lazo M, Carnethon M, Bertoni AG, Schreiner PJ, Diez Roux AV, et al. Examining a bidirectional association between depressive symptoms and diabetes. JAMA. 2008;299:2751–9. doi: 10.1001/jama.299.23.2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knol MJ, Twisk JW, Beekman AT, Heine RJ, Snoek FJ, Pouwer F. Depression as a risk factor for the onset of type 2 diabetes mellitus. A meta-analysis. Diabetologia. 2006;49:837–45. doi: 10.1007/s00125-006-0159-x. [DOI] [PubMed] [Google Scholar]
- 4.Medved V, Jovanović N, Knapić VP. ‘The comorbidity of diabetes mellitus and psychiatric disorders’. Psychiatr Danub. 2009;21:585–8. [PubMed] [Google Scholar]
- 5.Ali S, Stone MA, Peters JL, Davies MJ, Khunti K. The prevalence of co-morbid depression in adults with Type 2 diabetes: A systematic review and meta-analysis. Diabet Med. 2006;23:1165–73. doi: 10.1111/j.1464-5491.2006.01943.x. [DOI] [PubMed] [Google Scholar]
- 6.Hermanns N, Scheff C, Kulzer B, Weyers P, Pauli P, Kubiak T, et al. Association of glucose levels and glucose variability with mood in Type 1 diabetic patients. Diabetologia. 2007;50:930–3. doi: 10.1007/s00125-007-0643-y. [DOI] [PubMed] [Google Scholar]
- 7.Shaban MC, Fosbury J, Kerr D, Cavan DA. The prevalence of depression and anxiety in adults with Type 1 diabetes. Diabet Med. 2006;23:1381–4. doi: 10.1111/j.1464-5491.2006.02012.x. [DOI] [PubMed] [Google Scholar]
- 8.Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes. Diabetes Care. 2001;24:1069–78. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- 9.Lustman PJ, Clouse RE. Depression in diabetic patients: The relationship between mood and glycemic control. J Diabetes Complications. 2005;19:113–22. doi: 10.1016/j.jdiacomp.2004.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Simon GE, Katon WJ, Lin EH, Rutter C, Manning WG, Von Korff M, et al. Cost-effectiveness of systematic depression treatment among people with diabetes mellitus. Arch Gen Psychiatry. 2007;64:65–72. doi: 10.1001/archpsyc.64.1.65. [DOI] [PubMed] [Google Scholar]
- 11.Gonzalez JS, Peyrot M, McCarl LA, Collins EM, Serpa L, Mimiaga MJ, et al. Depression and diabetes treatment nonadherence: A meta- analysis. Diabetes Care. 2008;31:2398–403. doi: 10.2337/dc08-1341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Von Korff M, Katon W, Lin EH, Simon G, Ludman E, Oliver M, et al. Potentially modifiable factors associated with disability among people with diabetes. Psychosom Med. 2005;67:233–40. doi: 10.1097/01.psy.0000155662.82621.50. [DOI] [PubMed] [Google Scholar]
- 13.Schram MT, Baan CA, Pouwer F. Depression and quality of life in patients with diabetes: A systematic review from the European depression in diabetes (EDID) research consortium. Curr Diabetes Rev. 2009;5:112–9. doi: 10.2174/157339909788166828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koopmans B, Pouwer F, de Bie RA, van Rooij ES, Leusink GL, Pop VJ. Depressive symptoms are associated with physical inactivity in patients with type 2 diabetes.The DIAZOB Primary Care Diabetes study. Fam Pract. 2009;26:171–3. doi: 10.1093/fampra/cmp016. [DOI] [PubMed] [Google Scholar]
- 15.American Diabetes Association. Clinical Practice Recommendations. Diabetes Care. 2010;1:S1–103. [PubMed] [Google Scholar]
- 16.Cuijpers P, Dekker J, Noteboom A, Smits N, Peen J. Sensitivity and specificity of the Major Depression Inventory in outpatients. BMC Psychiatry. 2007;7:39. doi: 10.1186/1471-244X-7-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Konstantinidis A, Martiny K, Bech P, Kasper S. A comparison of the major depression inventory (MDI) and the beck depression inventory (BDI) in severely depressed patients. Int J Psychiatry Clin Pract. 2011;15:56–61. doi: 10.3109/13651501.2010.507870. [DOI] [PubMed] [Google Scholar]
- 18.Balhara Y, Sagar R. Correlates of anxiety and depression among patients with type 2 diabetes mellitus. Indian J Endocr Metab. 2011;15:50–4. doi: 10.4103/2230-8210.83057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Raval A, Dhanaraj E, Bhansali A, Grover S, Tiwari P. Prevalence and determinants of depression in type 2 diabetes patients in a tertiary care centre. Indian J Med Res. 2010;132:195–200. [PubMed] [Google Scholar]
- 20.Khuwaja AK, Lalani S, Dhanani R, Azam IS, Rafique G, White F. Anxiety and depression among outpatients with type 2 diabetes: A multi-centre study of prevalence and associated factors. Diabetol Metab Syndr. 2010;2:72. doi: 10.1186/1758-5996-2-72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Aina Y, Susman JL. Understanding comorbidity with depression and anxiety disorders. J Am Osteopath Assoc. 2006;106(5 Suppl 2):S9–14. [PubMed] [Google Scholar]
- 22.Bouwman V, Adriaanse MC, van’t Riet E, Snoek FJ, Dekker JM, Nijpels G. Depression, anxiety and glucose metabolism in the general Dutch population: The new Hoorn study. PloS One. 2010;5:e9971. doi: 10.1371/journal.pone.0009971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Collins MM, Corcorant P, Perry IJ. Anxiety and depression symptoms in patients with diabetes. Diabet Med. 2009;26:153–61. doi: 10.1111/j.1464-5491.2008.02648.x. [DOI] [PubMed] [Google Scholar]
- 24.Skaff MM, Mullan JT, Almeida DM, Hoffman L, Masharani U, Fisher L. Daily negative mood affects fasting glucose in type 2 diabetes. Health Psychol. 2009;28:265–72. doi: 10.1037/a0014429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Eren I, Erdi O, Ozcankaya R. Relationship between blood glucose control and psychiatric disorders in type II diabetic patients. Turk Psikiyatri Derg. 2003;14:184–91. [PubMed] [Google Scholar]
- 26.Richardson LK, Egede LE, Mueller M, Echols CL, Gebregziabher M. Longitudinal effects of depression on glycemic control in veterans with Type 2 diabetes. Gen Hosp Psychiatry. 2008;30:509–14. doi: 10.1016/j.genhosppsych.2008.07.001. [DOI] [PubMed] [Google Scholar]
- 27.Heckbert SR, Rutter CM, Oliver M, Williams LH, Ciechanowski P, Lin EH, et al. Depression in relation to long-term control of glycemia, blood pressure, and lipids in patients with diabetes. J Gen Intern Med. 2010;25:524–9. doi: 10.1007/s11606-010-1272-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Petrak F, Herpertz S. Treatment of depression in diabetes: An update. Curr Opin Psychiatry. 2009;22:211–7. doi: 10.1097/YCO.0b013e3283207b45. [DOI] [PubMed] [Google Scholar]
- 29.Katon WJ, Lin EH, Von Korff M, Ciechanowski P, Ludman EJ, Young B, et al. Collaborative care for patients with depression and chronic illnesses. N Engl J Med. 2010;363:2611–20. doi: 10.1056/NEJMoa1003955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bogner HR, Morales KH, de Vries HF, Cappola AR. Integrated management of type 2 diabetes mellitus and depression treatment to improve medication adherence: A randomized controlled trial. Ann Fam Med. 2012;10:15–22. doi: 10.1370/afm.1344. [DOI] [PMC free article] [PubMed] [Google Scholar]


