Abstract
Brown tumors of bone are highly vascular, lytic bone lesions representing a reparative cellular process rather than a neoplastic process usually seen in patients with hyperparathyroidism. These tumors can behave aggressively and be destructive. We report a 49-year-old male patient who was admitted to our hospital with a long-term history of right shoulder and right hip pain. Multiple lytic and destructive bone lesions were found in X-ray graphy and CT images. These bone lesions mimicked multiple skeletal metastatic lesions and seemed to be those of the terminal stage of malignancy. PET scan was requested for the evaluation of FDG uptake of these lesions and to search the unknown primary tumor site. Positron emission tomography/computed tomography (PET/CT) images showed multiple hypermetabolic malignant or metastatic FDG avid bone lesions in skeletal system. However the biopsy results revealed no signs of malignancy and laboratory data showed elevated serum calcium, alkaline phosphatase, parathyroid hormone, low serum phosphate and parathyroid scintigraphy was performed. Adenoma in the left parathyroid gland was seen with Tc-99m MIBI parathyroid scintigraphy. Pathological results confirmed the diagnosis of parathyroid adenoma. Brown tumor is the potential cause of false-positive result in evaluation of a patient for unknown primary tumor or skeletal metastases with PET/CT imaging.
Keywords: Brown tumor, hyperparathyroidism, flourodeoxyglocose, positron emission tomography/computed tomography
INTRODUCTION
Brown tumors are not true tumors that arise in settings of excess osteoclast activity caused by chronic excreation of parathyroid hormone in association with primary or secondary hyperparathyroidism.[1] Clinically, brown tumors most often manifest as slowly growing, painful masses.[2] Brown tumors occur more commonly in the fifth and sixth decades of life and they can be seen in monoostotic and polyostotic forms.[3] Brown tumor can be seen in the whole skeletal system but preferentially affected sites of tumor are the metacarpals, phalanges, jaw, skull, pelvis, clavicle, ribs femur, spine, and rarely the sphenoid sinus.[4] If the brown tumors are prominent in hyperparathyroidism, skeletal abnormality may be misdiagnosed as multiple bone metastases or primary bone tumor. We report positron emission tomography/computed tomography (PET/CT) images of a 49-year-old male patient which is requested for to search the unknown primary tumor site. The present case illustrates that brown tumors can display high accumulation of FDG in PET/CT imaging and these tumors are potential cause of false-positive results in the evaluation of a patient for unknown primary tumor site or metastatic lesions.
CASE REPORT
A 49-year-old male patient was admitted to our hospital with a history of right shoulder and right hip pain. X-ray graphy and CT images were performed and multiple lytic and destructive bone lesions were found. These bone lesions mimicked multiple skeletal metastatic lesions. PET/CT imaging was requested for the evaluation of FDG uptake of these lesions and to search the possible unknown primary tumor site. F-18 FDG PET/CT whole body imaging was performed after intravenously injection of 420 MBq (11.3 mCi) 18F FDG. After 1 hour of waiting period in a silent room patient was imaged using an integrated PET/CT camera, which is consists of a 6-slice CT gantry, integrated with a LSO-based fullring PET scanner (Siemens Biograph 6, IL, Chicago, USA). PET/CT images showed multiple enhanced FDG uptake of bone lesions in skeletal system [Figure 1]. These lesions are prominent in right humerus, bilateral ribs and right iliac bone with a maximum standardized uptake value of 18.5. Firstly, these lesions were thought metastates because of their FDG uptake. However, a nodular structure inferior to the left lobe of the thyroid gland which has no increased FDG-uptake was discovered. He has no family history of hyperparathyroidism. Laboratory data showed elevated serum calcium, alkaline phosphatase, parathyroid hormone and low serum phosphate. Parathormone level was 461 pg/ ml (normal 15-65 pg/ml). DEXA was performed for right hip and showed osteopenia. The biopsy results revealed no signs of malignancy. After these findings, parathyroid adenoma and brown tumors were thought and for confirmation parathyroid scintigraphy was performed.
Figure 1.
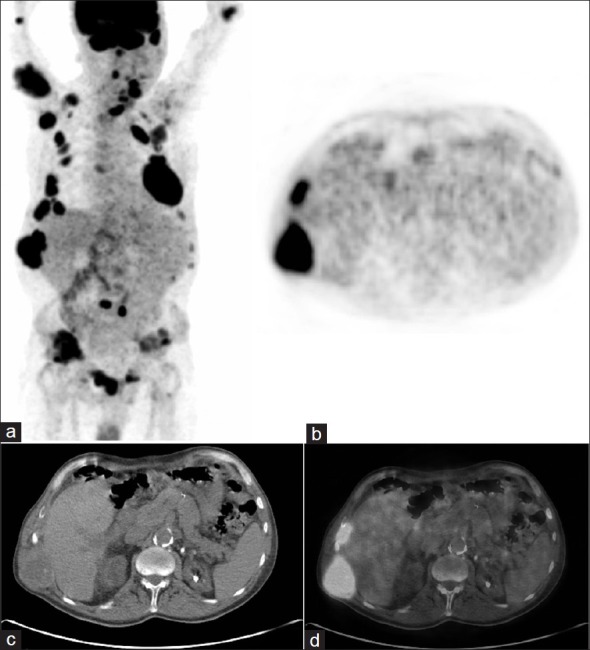
Maximum intensity projection of PET (a), axial PET (b), axial CT (c), and axial fusion (d) images showed multiple enhanced FDG uptake of bone lesions in skeletal system
Parathyroid scintigraphy with Tc-99m methoxy isobutyl isonitrile (MIBI) was performed as a dual-phase single-tracer examination with a two head gamma camera (E-cam, Diacam, Siemens, Chicago, IL, USA). Following an intravenous injection of 566.1 MBq (15.3 mCi) of 99mTc MIBI, planar static images of the anterior view of the neck and upper thorax, at a matrix size of 128 × 128, was obtained with the patient in the supine position. MIBI images revealed a parathyroid adenoma in the left thyroid lobe [Figure 2]. Parathyroidectomy was undertaken and histopathological examination revealed the presence of a parathyroid adenoma [Figure 3].
Figure 2.

Parathyroid scintigraphy with Tc-99m methoxy isobutyl isonitrile images showed intense activity accumulation in the left thyroid lobe
Figure 3.
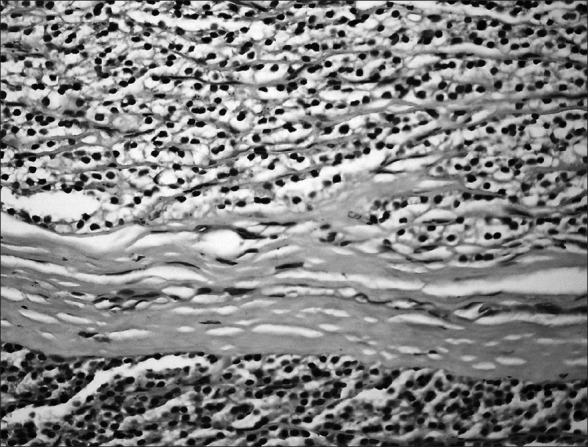
Histopathological examination revealed the presence of a parathyroid adenoma (H and E, ×200)
DISCUSSION
Brown tumors are not true tumors which are the end stage of primary or secondary hyperparathyroidism. Clinically, brown tumors most often manifest as slowly growing, painful masses and bone pain and arthralgia are the most common symptoms.[5] The incidence of brown tumor has been reported to be 3% in patients with primary hyperparathyroidism, in contrast to 1.5–1.7% in patients with secondary hyperparathyroidism.[6] Brown tumors have been reported to be detectable by bone scan and MIBI scintigraphy.[7]
FDG PET/CT imaging has been commonly used to distinguish malign lesions from benign lesions. High FDG uptake may be seen in benign conditions such as inflammation and infections. Despite their benign characteristics osteoclast-like giant cell-containing lesions, such as giant cell reparative granuloma, aneurysmal bone cyst, and giant cell tumor, show increased 18F-FDG uptake.[8] Brown tumors are benign tumors which can show high FDG uptake. High FDG uptake mechanism has been suggested to be the presence of giant cells in brown tumors on PET/CT. Another mechanism is that intracellular glucose metabolism of the macrophages may play a role for the elevated FDG uptake.[8] Kuwahara et al. showed a case of increased FDG uptake in brown tumors with primary hyperparathyroidism.[9] PET scan is used to evaluate the metabolic activity of lesions. It is known that parathyroid SESTAMIBI scan might be false negative in the detection of parathyroid condition. Santiago Chinchilla et al. showed false negative of the scintigraphy with 99mTc-sestamibi in parathyroid carcinoma with associated brown tumors in their case report.[10]
Histological findings of brown tumors may include a dense fibroblastic stroma, areas of cystic degeneration, osteoid, microfractures, hemorrhage, macrophages with hemosiderin, and multinucleated osteoclastic giant cells. Histologically, brown tumours may not be distinguishable from giant-cell tumors.
In conclusion, the diagnosis of brown tumor should be considered in patients with hyperparathyroidism with elevated calcium and alkaline phosphatase levels have multiple destructive bone lesions which are mimicking metastatic bone lesions on PET/CT images.
After resection of parathyroid adenoma, FDG PET/CT imaging can be useful to see the response to treatment and osteoblastic changes in brown tumor.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Tan G, Shiran M, Swaminathan M, Phang K, Rohaizak M. Large retrosternal parathyroid carcinoma with primary hyperparathyroidism. Asian J Surg. 2007;30:286–9. doi: 10.1016/S1015-9584(08)60041-X. [DOI] [PubMed] [Google Scholar]
- 2.Hsieh MC, Ko JY, Eng HL. Pathologic Fracture of the distal femur in osteitis Fibrosa cystica simulating metastatic disease. Arch Orthop Trauma Surg. 2004;124:498–501. doi: 10.1007/s00402-004-0697-y. [DOI] [PubMed] [Google Scholar]
- 3.Pai M, Park CH, Kim BS, Chung YS, Park HB. Multiple brown tumors in parathyroid carcinoma mimicking metastatic bone disease. Clin Nucl Med. 1997;22:691–4. doi: 10.1097/00003072-199710000-00006. [DOI] [PubMed] [Google Scholar]
- 4.Takeshita T, Tanaka H, Harasawa A, Kaminaga T, Imamura T, Furui S. Brown tumor of the sphenoid sinus in a patient with secondary hyperparathyroidism: CT and MR imaging findings. Radiat Med. 2004;22:265–8. [PubMed] [Google Scholar]
- 5.Aoki J, Watanaba H, Shinozaki T, Takagishi K, Ishijima H, Oya N, et al. FDG PET of primary benign and malignant bone tumors: Standardized uptake value in 52 lesions. Radiology. 2001;219:774–7. doi: 10.1148/radiology.219.3.r01ma08774. [DOI] [PubMed] [Google Scholar]
- 6.Nassar GM, Ayus JC. Images in clinical medicine.Brown tumor in end-stage renal disease. N Engl J Med. 1999;341:1652. doi: 10.1056/NEJM199911253412204. [DOI] [PubMed] [Google Scholar]
- 7.Treglia G, Dambra DP, Bruno I, Mulè A, Giordano A. Costal brown tumor detected by dual-phase parathyroid imaging and SPECT-CT in primary hyperparathyroidism. Clin Nucl Med. 2008;33:193–5. doi: 10.1097/RLU.0b013e318162dd89. [DOI] [PubMed] [Google Scholar]
- 8.Gamelli RL, Liu H, He LK, Hofmann CA. Augmentations of glucose uptake and glucose transporter-1 in macrophages following thermal injury and sepsis in mice. J Leukoc Biol. 1996;59:639–47. doi: 10.1002/jlb.59.5.639. [DOI] [PubMed] [Google Scholar]
- 9.Kuwahara K, Izawa S, Murabe H, Murakami N, Yokota T, Wani Y, et al. Increased 18F-fluorodeoxyglucose uptake in a brown tumor in a patient with primary hyperparathyroidism. J Clin Endocrinol Metab. 2007;92:2408–9. doi: 10.1210/jc.2007-0591. [DOI] [PubMed] [Google Scholar]
- 10.Santiago Chinchilla A, Ramos Font C, Muros de Fuentes MA, Navarro-Pelayo Láinez M, Palacios Gerona H, Moreno Caballero M, et al. False negative of the scintigraphy with 99mTc-sestamibi in parathyroid carcinoma with associated brown tumors. Contributions of the 18F-FDG-PET/CT. Rev Esp Med Nucl. 2011;30:174–9. doi: 10.1016/j.remn.2010.08.006. [DOI] [PubMed] [Google Scholar]


