Abstract
Objective. To evaluate the association between the purported risk factors for chondrocalcinosis and gout and the risk of pseudogout in the general population.
Methods. We conducted a case–control study nested within a UK general practice database (The Health Improvement Network) by identifying incident cases of pseudogout between 1986 and 2007 and up to 10 control subjects matched to each case, based on age, sex and follow-up time. We evaluated the purported risk factors for chondrocalcinosis (i.e. OA, RA, hyperparathyroidism and diuretics) and established risk factors for gout (as comparison exposures) using conditional logistic regression analysis.
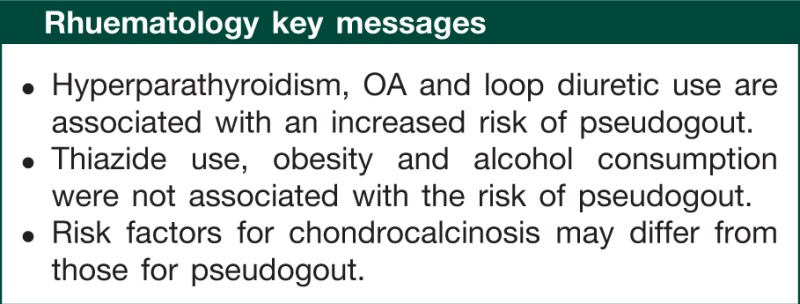
Results. We identified 795 cases of pseudogout and 7770 matched control subjects. The risk of pseudogout was associated with hyperparathyroidism [odds ratio (OR) 4.87; 95% CI 2.10, 11.3], OA (OR 2.91; 95% CI 2.48, 3.43) and loop diuretic use (OR 1.35; 95% CI 1.09, 1.67). RA, thiazide diuretic use, BMI and other gout risk factors were not associated with the risk of pseudogout, except for chronic renal failure (OR 2.29; 95% CI 1.30, 4.01).
Conclusion. This general population study based on physician-recorded pseudogout suggests that most of the previously observed associations with chondrocalcinosis are replicable with the risk of pseudogout, but there are notable differences, such as thiazide diuretics, RA and chronic renal failure, highlighting the need to study the clinical outcome, pseudogout. Avoiding loop diuretics may help individuals with recurrent pseudogout.
Keywords: pseudogout, chondrocalcinosis, CPPD, epidemiology
Introduction
Acute calcium pyrophosphate (CPP) crystal arthritis, or pseudogout, is a common inflammatory arthritis of the elderly population, and it belongs to a group of related diseases called calcium pyrophosphate deposition diseases (CPPDs), which also includes chondrocalcinosis [1]. Recent recommendations by the European League Against Rheumatism (EULAR) summarized risk factors for CPPD, such as age, OA, RA (inverse association), hyperparathyroidism and diuretics [2]. However, the source data for these risk factors are limited and are mainly derived from studies investigating chondrocalcinosis [2]. As chondrocalcinosis is often asymptomatic, its risk factors may not garner the same clinical interest as those for pseudogout. Furthermore, risk factors for pseudogout may differ with chondrocalcinosis. In this study, we sought to evaluate the relation between the purported risk factors for chondrocalcinosis and the risk of physician-recorded pseudogout in a general population context. Given its gout-like clinical presentation, we also investigated the potential impact of known risk factors for gout, such as obesity, alcohol, hypertension, diabetes, congestive heart failure and chronic kidney disease (as comparison exposures).
Methods
Study population
The Health Improvement Network (THIN) contains computerized medical records entered by general practitioners (GPs) in the UK [3]. Data on ∼7.3 million patients are systematically recorded and sent anonymously to THIN. Patients included in the database are representative of the UK population with respect to age, sex and geographical region [3]. The computerized information includes demographics, details from GP visits, diagnoses from specialist referrals and hospital admissions, results of laboratory tests and a free text section (for which information is available on request). Diagnoses are recorded using READ codes. Prescriptions issued by primary care providers are recorded automatically in the database; drugs are coded using the Multilex classification (http://www.firstdatabank.co.uk/8/multilex-drug-data-file). The validity of THIN for pharmacoepidemiological research has been demonstrated [4].
We conducted a nested case–control study using THIN data from January 1986 to June 2010. The cohort included all individuals aged ≥20 years, who had one or more years of enrolment with the GP. The start date corresponded to the date when these eligibility criteria were met. Members of the cohort were followed up until the date of one of the following end points: pseudogout detection, death or end of the study period (31 June 2010), whichever came first. The study was approved by the Boston University Institutional Review Board and Multicenter Research Ethics Committee.
Ascertainment of pseudogout and control subjects sampling
We identified all individuals with a first-ever diagnosis of pseudogout recorded by a GP using an automatic search with the READ code for pseudogout (N02.14). The date of the first occurrence of pseudogout was designated as the index date. We attempted to match up to 10 controls to each case based on year of birth, sex, enrolment date and index date. We excluded pseudogout patients, who also had a gout diagnosis (n = 310) during the cohort follow-up, to help isolate the risk factors for pseudogout without the potential influence of risk factors for gout.
Exposure assessment
We sought to evaluate the purported risk factors for CPPD that were included in the recent EULAR recommendations available in THIN [i.e. BMI, OA, RA, hyperparathyroidism and diuretic use (loop and thiazide, separately)] [2]. In addition, we evaluated associations with established risk factors for gout available in THIN [i.e. alcohol consumption, hypertension, diabetes, congestive heart failure and chronic kidney disease (defined as having a READ code of chronic renal impairment, chronic kidney disease stage 3 or higher, chronic/end-stage renal failure or having dialysis)]. We defined the presence of these medical conditions using GP-recorded diagnoses by READ codes, and thiazide and loop diuretic use by prescription drug data, as described previously, before the index date.
Statistical analysis
We estimated odds ratios (ORs) and 95% CIs for pseudogout associated with the purported risk factors for CPPD, and gout by means of conditional logistic regression analysis. As diuretics are primarily indicated for our covariate conditions, such as hypertension, heart failure and chronic kidney disease, we used a set of multivariate models that adjusted for these disease conditions separately and together with diuretic use to assess their potential impacts. The final multivariate model included all of the covariates measured. All statistical procedures were performed with SAS 9.2 (SAS Institute, Cary, NC, USA).
Results
The base cohort consisted of 4 484 066 persons followed for an average of 7 years, the mean age at cohort entry was 44.7 years, and 47.8% were male. Our study population included 795 pseudogout cases and 7770 controls; their characteristics are shown in Table 1. The mean age of individuals with pseudogout at diagnosis was 72.5 years, and 45% were male. When we assessed potential independent associations in our adjusted models, a history of hyperparathyroidism (OR 4.87; 95% CI 2.10, 11.3), OA (OR 2.91; 95% CI 2.48, 3.43) and loop diuretics (OR 1.35; 95% CI 1.09, 1.67) was associated with the risk of pseudogout (Table 1). Thiazide use was not associated with the risk of pseudogout (OR 1.02; 95% CI 0.83, 1.25). Risk factors for gout, such as BMI, heart failure, hypertension, diabetes, chronic kidney disease and alcohol consumption, were not significantly associated with the risk of pseudogout. However, when we limited the scope of chronic kidney disease to chronic renal failure (defined as READ codes including chronic kidney disease stage 5, renal failure or undergoing dialysis), it was associated with the risk of pseudogout (multivariate OR 2.29; 95% CI 1.30, 4.01). When we excluded individuals with missing BMI and alcohol consumption data, our results did not change materially.
Table 1.
Associations between purported risk factors and the risk of pseudogout
| Variable | Control (n = 7770) | Pseudogout (n = 795) | Univariate OR (95% CI) | Multivariatea OR (95% CI) | Multivariateb OR (95% CI) | Multivariatec OR (95% CI) |
|---|---|---|---|---|---|---|
| Demographic and anthropomorphic | ||||||
| Age, years | 72.2 ± 12.8 | 72.5 ± 12.8 | – | – | – | – |
| Male | 3496 (45.0) | 358 (45.0) | – | – | – | – |
| BMI, kg/m2 | ||||||
| <18.5 | 112 (1.4) | 16 (2.0) | 1.35 (0.78, 2.32) | 1.42 (0.81, 2.47) | 1.39 (0.80, 2.43) | 1.40 (0.80, 2.44) |
| 18.5–24.9 | 2366 (30.5) | 246 (30.9) | 1.00 | 1.00 | 1.00 | 1.00 |
| 25.0–29.9 | 2345 (30.2) | 262 (33.0) | 1.09 (0.91, 1.31) | 1.02 (0.84, 1.23) | 1.01 (0.84, 1.23) | 1.01 (0.84, 1.22) |
| ≥30.0 | 1165 (15) | 150 (18.9) | 1.28 (1.03, 1.60) | 1.06 (0.84, 1.33) | 1.03 (0.82, 1.30) | 1.02 (0.81, 1.29) |
| Missing | 1782 (22.9) | 121 (15.2) | 0.59 (0.46, 0.75) | 0.78 (0.58, 1.04) | 0.76 (0.57, 1.02) | 0.77 (0.58, 1.03) |
| Lifestyle | ||||||
| Alcohol consumption: | ||||||
| None | 1409 (18.1) | 148 (18.6) | 1.00 | 1.00 | 1.00 | 1.00 |
| Past | 144 (1.9) | 25 (3.1) | 1.69 (1.06, 2.69) | 1.49 (0.92, 2.42) | 1.50 (0.93, 2.43) | 1.50 (0.92, 2.43) |
| Current | 4555 (58.6) | 515 (64.8) | 1.10 (0.90, 1.34) | 1.15 (0.94, 1.41) | 1.14 (0.93, 1.40) | 1.15 (0.94, 1.41) |
| Missing | 1662 (21.4) | 107 (13.5) | 0.58 (0.44, 0.76) | 0.82 (0.59, 1.12) | 0.80 (0.59, 1.10) | 0.81 (0.59, 1.12) |
| Medical conditions | ||||||
| OA | 1844 (23.7) | 370 (46.5) | 3.14 (2.67, 3.68) | 2.93 (2.49, 3.45) | 2.92 (2.48, 3.44) | 2.91 (2.48, 3.43) |
| RA | 141 (1.8) | 24 (3.0) | 1.67 (1.07, 2.60) | 1.37 (0.87, 2.17) | 1.35 (0.86, 2.13) | 1.34 (0.85, 2.11) |
| Hyperparathyroidism | 17 (0.2) | 10 (1.3) | 6.21 (2.78, 13.9) | 4.82 (2.08, 11.2) | 5.01 (2.17, 11.6) | 4.87 (2.10, 11.3) |
| Diabetes | 678 (8.7) | 94 (11.8) | 1.42 (1.13, 1.79) | 1.20 (0.94, 1.53) | 1.21 (0.95, 1.55) | 1.16 (0.91, 1.49) |
| Hypertension | 2802 (36.1) | 335 (42.1) | 1.33 (1.13, 1.56) | 1.14 (0.96, 1.34) | – | 1.12 (0.92, 1.36) |
| Heart failure | 348 (4.5) | 56 (7.0) | 1.64 (1.21, 2.22) | 1.42 (1.04, 1.95) | – | 1.20 (0.86, 1.67) |
| Chronic kidney disease | 532 (6.9) | 78 (9.8) | 1.58 (1.20, 2.10) | 1.34 (1.00, 1.79) | – | 1.29 (0.97, 1.73) |
| Diuretic use | ||||||
| Loop diuretics | 1244 (16.0) | 182 (22.9) | 1.60 (1.32, 1.93) | – | 1.44 (1.18, 1.75) | 1.35 (1.09, 1.67) |
| Thiazides | 2268 (29.2) | 263 (33.1) | 1.23 (1.04, 1.46) | – | 1.09 (0.92, 1.29) | 1.02 (0.83, 1.25) |
The univariate model is the study population matched by age and sex. Descriptive data are presented as mean ± standard deviation or n (%).
aAdjusted for all covariates except for loop and thiazide diuretics.
bAdjusted for all covariates except for hypertension, congestive heart failure and chronic kidney disease.
cAdjusted for all of the covariates in the table.
Discussion
In this large general practice cohort representative of the UK population, we found that having a history of hyperparathyroidism, OA and loop diuretic use was associated with an increased risk of physician-recorded pseudogout. However, established risk factors for gout, such as obesity, alcohol consumption, thiazide use hypertension, diabetes and congestive heart failure, were not significantly associated with the risk of physician-recorded pseudogout. These first general population data on pseudogout suggest that most of the previously observed associations (or lack of associations) of purported factors with chondrocalcinosis are replicable with the outcome of pseudogout, but there may also be notable differences (e.g. thiazide diuretics and RA) [2].
We found that loop diuretic use was associated with the risk for pseudogout, whereas thiazide use was not, supporting the potential importance of avoiding loop diuretics among individuals with recurrent pseudogout. A previous cross-sectional study has reported that diuretic use was associated with chondrocalcinosis [5], but the study did not report the data separately for thiazide and loop diuretics. As CPP deposition is facilitated in hypomagnesaemia [6], and the main area of renal magnesium reabsorption is in the loop of Henle, the action site of loop diuretics, weaker magnesium wastage by thiazide than loop diuretics [7] may explain the potential differential effects on the risk of pseudogout between the two diuretics.
The association of hyperparathyroidism with pseudogout was consistent with previous reports on CPPD [8, 9]. It has been suggested that parathyroid hormone-induced increases in calcium or pyrophosphate concentrations may lead to CPP deposition [10]. As chronic kidney disease is a major cause of secondary hyperparathyroidism [11], there have been case reports linking chronic kidney disease and CPPD [12, 13]. Although our fully adjusted results suggested a positive trend between chronic kidney disease and pseudogout, the association became clear (multivariate OR 2.29) when we limited the exposure definition to chronic renal failure. These findings provide support for a potentially substantial association between renal failure and pseudogout, although this link was not included in the recent EULAR recommendations [2].
The magnitude of association with a history of OA was similar to that of the recent EULAR summary data [2]. Although obesity is a risk factor for OA and gout [14, 15], we found no association with the risk of pseudogout, similar to a previous report [16]. These data did not support a speculated link between obesity and chondrocalcinosis, such as mechanical loading of the joints leading to increased release of adenosine triphosphate and consequent free pyrophosphate [16, 17]. Furthermore, the absence of association between BMI and the risk of pseudogout was consistent with the lack of association with the presence of chondrocalcinosis [2, 16].
Previous studies have suggested differing directions of association between RA and CPPD. For example, although the recent EULAR summary concluded a strongly inverse association (OR 0.18) between RA and chondrocalcinosis [2], other previous studies have suggested a positive association [8] or no association [18]. We observed a non-significant positive trend between RA and pseudogout, although this may be explained by a pseudo-RA presentation of CPPD [2]. Overall, the totality of available evidence on this link seems inconclusive in our view.
Strengths and limitations of our study deserve comment. This study was conducted using a large UK general practice database; therefore findings are likely to be applicable to the general population. Previous studies had smaller numbers (the largest series had ∼100 CPPD cases) [8, 16, 19], mainly focused on chondrocalcinosis [9, 18, 20] or had a cross-sectional study design [5, 6]. Our large nested case–control study had a well-defined temporal relationship between the predictors and the outcome, and it focused on a clinical outcome, pseudogout. As in most other epidemiologic studies of CPPD [5, 6, 9, 16, 18–20], our definition of pseudogout did not require the observation of CPP crystals, and also our pseudogout cases have not been validated. Thus it is conceivable that other arthritic conditions, including other CPPD arthropathies, such as pseudo-OA or pseudo-RA [2], could have been recorded as pseudogout. However, as pseudogout is not considered one of the readily suspected arthritic diagnoses among GPs, we anticipate that GP recording is more specific for pseudogout than commonly labelled arthritic conditions (e.g. rheumatoid arthritis or gout). Any non-differential misclassification would have biased the study results toward the null. It is also noteworthy that well-established risk factors for gout in this data set [14] were not associated with the risk of pseudogout, supporting the validity of our diagnosis. Nevertheless, our data call for confirmation of our findings using validated cases of pseudogout in a prospective study context, if feasible.
In conclusion, this general population study based on physician-recorded pseudogout suggests that most of the previously observed associations (and lack thereof) between purported factors and chondrocalcinosis are replicable with the outcome of pseudogout, but also that there may be notable exceptions, such as thiazide diuretics, RA and chronic renal failure. These findings highlight the potential need to further investigate the clinical outcome of pseudogout and support the avoidance of loop diuretics among individuals with pseudogout.
Funding: This study was supported by NIH grant P60AR047785.
Disclosure statement: A.M.R. has received consultation fees from Nuoun, URL. All other authors have declared no conflicts of interest.
References
- 1.Richette P, Bardin T, Doherty M. An update on the epidemiology of calcium pyrophosphate dihydrate crystal deposition disease. Rheumatology (Oxford) 2009;48:711–15. doi: 10.1093/rheumatology/kep081. [DOI] [PubMed] [Google Scholar]
- 2.Zhang W, Doherty M, Bardin T, et al. European League Against Rheumatism recommendations for calcium pyrophosphate deposition. Part I: terminology and diagnosis. Ann Rheum Dis. 2011;70:563–70. doi: 10.1136/ard.2010.139105. [DOI] [PubMed] [Google Scholar]
- 3.Bourke A, Dattani H, Robinson M. Feasibility study and methodology to create a quality-evaluated database of primary care data. Inform Prim Care. 2004;12:171–7. doi: 10.14236/jhi.v12i3.124. [DOI] [PubMed] [Google Scholar]
- 4.Lewis JD, Schinnar R, Bilker WB, Wang X, Strom BL. Validation studies of the health improvement network (THIN) database for pharmacoepidemiology research. Pharmacoepidemiol Drug Saf. 2007;16:393–401. doi: 10.1002/pds.1335. [DOI] [PubMed] [Google Scholar]
- 5.Neame RL, Carr AJ, Muir K, Doherty M. UK community prevalence of knee chondrocalcinosis: evidence that correlation with osteoarthritis is through a shared association with osteophyte. Ann Rheum Dis. 2003;62:513–18. doi: 10.1136/ard.62.6.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Richette P, Ayoub G, Lahalle S, et al. Hypomagnesemia associated with chondrocalcinosis: a cross-sectional study. Arthritis Rheum. 2007;57:1496–501. doi: 10.1002/art.23106. [DOI] [PubMed] [Google Scholar]
- 7.Ellison DH. Divalent cation transport by the distal nephron: insights from Bartter’s and Gitelman’s syndromes. Am J Physiol Renal Physiol. 2000;279:F616–25. doi: 10.1152/ajprenal.2000.279.4.F616. [DOI] [PubMed] [Google Scholar]
- 8.Alexander GM, Dieppe PA, Doherty M, Scott DG. Pyrophosphate arthropathy: a study of metabolic associations and laboratory data. Ann Rheum Dis. 1982;41:377–81. doi: 10.1136/ard.41.4.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Yashiro T, Okamoto T, Tanaka R, et al. Prevalence of chondrocalcinosis in patients with primary hyperparathyroidism in Japan. Endocrinol Jpn. 1991;38:457–64. doi: 10.1507/endocrj1954.38.457. [DOI] [PubMed] [Google Scholar]
- 10.Doherty M. Calcium pyrophosphate dihydrate crystal-associated arthropathy. In: Hochberg MC, Silman AC, Smolen JS, Weinblatt ME, Weissman MH, editors. Rheumatology. 3rd edn. Edinburgh: Mosby; 2003. pp. 1937–50. [Google Scholar]
- 11.De Boer IH, Gorodetskaya I, Young B, Hsu CY, Chertow GM. The severity of secondary hyperparathyroidism in chronic renal insufficiency is GFR-dependent, race-dependent, and associated with cardiovascular disease. J Am Soc Nephrol. 2002;13:2762–9. doi: 10.1097/01.asn.0000034202.91413.eb. [DOI] [PubMed] [Google Scholar]
- 12.Ellman MH, Brown NL, Katzenberg CA. Acute pseudogout in chronic renal failure. Arch Intern Med. 1979;139:795–6. [PubMed] [Google Scholar]
- 13.Yildiz N, Ardic F, Ercidogan O, Coban S. Acute pseudogout arthritis in a patient with chronic renal failure: a case report. Clin Nephrol. 2008;70:424–6. doi: 10.5414/cnp70424. [DOI] [PubMed] [Google Scholar]
- 14.Cea Soriano L, Rothenbacher D, Choi HK, Garcia Rodriguez LA. Contemporary epidemiology of gout in the UK general population. Arthritis Res Ther. 2011;13:R39. doi: 10.1186/ar3272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Felson DT, Zhang Y, Hannan MT, et al. Risk factors for incident radiographic knee osteoarthritis in the elderly: the Framingham Study. Arthritis Rheum. 1997;40:728–33. doi: 10.1002/art.1780400420. [DOI] [PubMed] [Google Scholar]
- 16.Zhang W, Neame R, Doherty S, Doherty M. Relative risk of knee chondrocalcinosis in siblings of index cases with pyrophosphate arthropathy. Ann Rheum Dis. 2004;63:969–73. doi: 10.1136/ard.2003.015206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Graff RD, Lazarowski ER, Banes AJ, Lee GM. ATP release by mechanically loaded porcine chondrons in pellet culture. Arthritis Rheum. 2000;43:1571–9. doi: 10.1002/1529-0131(200007)43:7<1571::AID-ANR22>3.0.CO;2-L. [DOI] [PubMed] [Google Scholar]
- 18.Ramonda R, Musacchio E, Perissinotto E, et al. Prevalence of chondrocalcinosis in Italian subjects from northeastern Italy. The Pro.V.A. (PROgetto Veneto Anziani) study. Clin Exp Rheumatol. 2009;27:981–4. [PubMed] [Google Scholar]
- 19.Sanmarti R, Serrarols M, Galinsoga A, et al. [Diseases associated with articular chondrocalcinosis: an analysis of a series of 95 cases] Med Clin (Barc) 1993;101:294–7. [PubMed] [Google Scholar]
- 20.Felson DT, Anderson JJ, Naimark A, Kannel W, Meenan RF. The prevalence of chondrocalcinosis in the elderly and its association with knee osteoarthritis: the Framingham Study. J Rheumatol. 1989;16:1241–5. [PubMed] [Google Scholar]


