Abstract
Background
Preventing sexually transmitted diseases (STD) such as Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (GC) remains a public health challenge. The U.S. Preventive Services Task Force suggests STD screening among men will likely lead to a decrease in infection rates of women. However, innovative approaches are necessary to increase the traditionally low rates of male screening. The purpose of this study is to compare the acceptability and effectiveness of home-based versus clinic-based urine screening for CT/GC in men.
Methods
We conducted a randomized clinical trial of 200 men ages 18-45 years who reside in St. Louis, Missouri. Men were enrolled via telephone and randomly assigned to receive a free urine CT/GC screening kit in-person at the research clinic or mailed to a preferred address. Participants completed questionnaires at baseline and 10-12 weeks post-enrollment. The primary outcome was whether a STD screening kit was completed.
Results
Sixty percent (120/200) completed STD screening. Men assigned to home-based screening were 60% more likely to complete screening compared to clinic-based screening (72% versus 48%, RRadj=1.6, 95% CI, 1.3, 2.00). We identified four cases of CT or GC in the home-based group compared to three cases of CT in the clinic group. Men who completed screening were significantly more likely to be white, younger, and college-educated.
Conclusions
Home-based screening for CT and GC among men is more acceptable than clinic-based screening and resulted in higher rates of screening completion. Incorporating home-based methods as adjuncts to traditional STD screening options shows promise in improving STD screening rates in men.
Keywords: Screening, sexually transmitted diseases, males, randomized clinical trial
INTRODUCTION
Chlamydia trachomatis (CT) and Neisseria gonorrhoeae (GC) are the two most common bacterial sexually transmitted diseases (STD) in the U.S.; over 1.3 million cases of CT and more than 300,000 cases of GC were reported in 2010.1-6 Nearly 90% of CT and GC infections are asymptomatic, facilitating the transmission and persistence of infections.7 Because of the serious and costly sequelae associated with CT/GC infections in women, routine screening is largely targeted at females.8
To reduce the rate of STD infections in women, we should also consider the reservoir of infected men who interact much less frequently with the health care system.9 Although the U.S. Preventive Services Task Force (USPSTF) does not recommend routine STD screening in males due to a lack of studies linking male screening to decreased transmission of infections, the USPSTF does suggest that it is nearly impossible to improve the health outcomes of women if screening programs fail to target men. Potential risks associated with male screening are minimal and studies have shown that dual male and female screening for CT is more cost-effective than screening women alone.10-11 Specifically, Blake et al. estimated that screening 2,000 men for CT will save $52,000 and eliminate 49 cases of pelvic inflammatory disease (PID) in their female partners each year compared to the absence of male screening.4 Nonetheless, many barriers such as concern regarding confidentiality, transportation to and from the clinic, and fear of painful screening procedures prohibit successful male participation in STD screening, even when the screening is free.12-13
Screening for CT and GC has become increasingly accurate and convenient with the development of nucleic acid amplification testing (NAAT) for non-invasive urine specimens.14 Although past studies have examined the role of urine-based home sampling kits for CT/GC screening in men, most were conducted in countries outside of the U.S. where there is national health care coverage, and the majority of studies were conducted only among homosexual populations or focused only on CT infections.12,15 This study was developed to compare the acceptability of home- versus clinic-based CT/GC screening. We hypothesized that men would be more likely to comply with home-based STD screening compared to clinic-based screening.
MATERIALS AND METHODS
We performed a randomized clinical trial of 200 men to compare the acceptability of CT and GC screening using non-invasive, self-collected urine specimens obtained either at home or in a traditional clinic setting. Men were invited to participate based on the following inclusion criteria: 18 to 45 years of age, English-speaking, and residing in St. Louis City or County. Recruitment strategies included study brochure distribution at low-income area health clinics and local colleges, referral through word-of-mouth, and the services of a Washington University School of Medicine community-based outreach group. The group worked within the community to inform individuals about the study and to put eligible persons in contact with study coordinators. The study protocol was approved by the Washington University in St. Louis Human Research Protection Office prior to participant recruitment.
Men interested in participating in the study called the study telephone line and were screened for eligibility over the telephone by a trained research assistant. Using a computer-generated 1:1 randomization scheme, eligible participants were randomly assigned, by random number generator function in Excel, to receive either a urine CT/GC screening kit at our research clinic or to have a CT/GC screening kit mailed to the participant's preferred address. Regardless of randomization arm, all participants received the same screening kit and self-collected their own urine sample, either at home or in the clinic setting. Due to the nature of the study, neither the investigators nor the participants were blinded to randomization assignment. Men who were randomized to home screening provided verbal consent, while those who we randomized to clinic-based screening provided both verbal and written consent. All participants completed two telephone surveys: a baseline questionnaire at the time of enrollment and a follow-up questionnaire 10 to 12 weeks post-enrollment to measure self-reported screening completion and satisfaction with the screening experience. Except for age, all questions had pre-defined response categories. Participants were given a $10 gift card at the time of study consent regardless of whether CT/GC screening was completed.
Urine collection and screening methods were the same for both experimental arms. All men were provided the following for self-sample urine collection: a sterile urine collection cup, an NAAT urine transport tube, and detailed, step-by-step instructions with photographs that explained how to collect and transfer the specimen. Each participant collected his own urine sample in the collection cup, and subsequently transferred the sample into the NAAT transport tube. A vacuum seal created between the collection cup and the NAAT tube facilitated transfer and eliminated leakage or overspill. Men randomized to home-based screening were mailed the collection kit along with written and visual instructions of how to return their urine sample in the NAAT tube with the prepaid, preaddressed mailer included, which complied with Department of Transport and U.S. Postal Service regulations. Men randomized to clinic-based screening were given the collection kit upon arrival to the clinic and returned their urine specimens in the NAAT tube to research staff. All samples were tested for CT/GC using the BDProbeTec ET instrument through DNA strand displacement amplification technology. We received clinic-based specimens the same day and home-based specimens within 4.2 (SD=2.8) days of collection on average. Upon receipt they were shipped via overnight carrier to the testing laboratory. Men who screened positive for CT or GC were provided with free treatment for themselves and their partners.
We analyzed baseline demographic and behavioral characteristics by randomization group using Student's t-tests and chi-square analyses. The primary outcome of interest was the percent of screening kits completed within each group. Multivariable logistic regression was used to determine the relative risk of STD screening by randomization group after adjusting for age, race, and education. All analyses were conducted using STATA (College Station, TX) version 10.0.
Our original sample size of 460 men was based on the following assumptions: 45% of men randomized to home-based screening would complete screening compared to 30% completion among men randomized to clinic-based screening. With an estimated relative risk of 1.5 for screening kit completion between men in the home versus clinic screening groups, we needed 230 men in each group to achieve a power of 90% at an alpha level of 0.05. We used the first 100 men enrolled as pilot data to verify our assumptions and found a higher uptake of screening completion in both groups (77% versus 54%) and therefore recalculated our sample size to 200 men, 100 in each group.
RESULTS
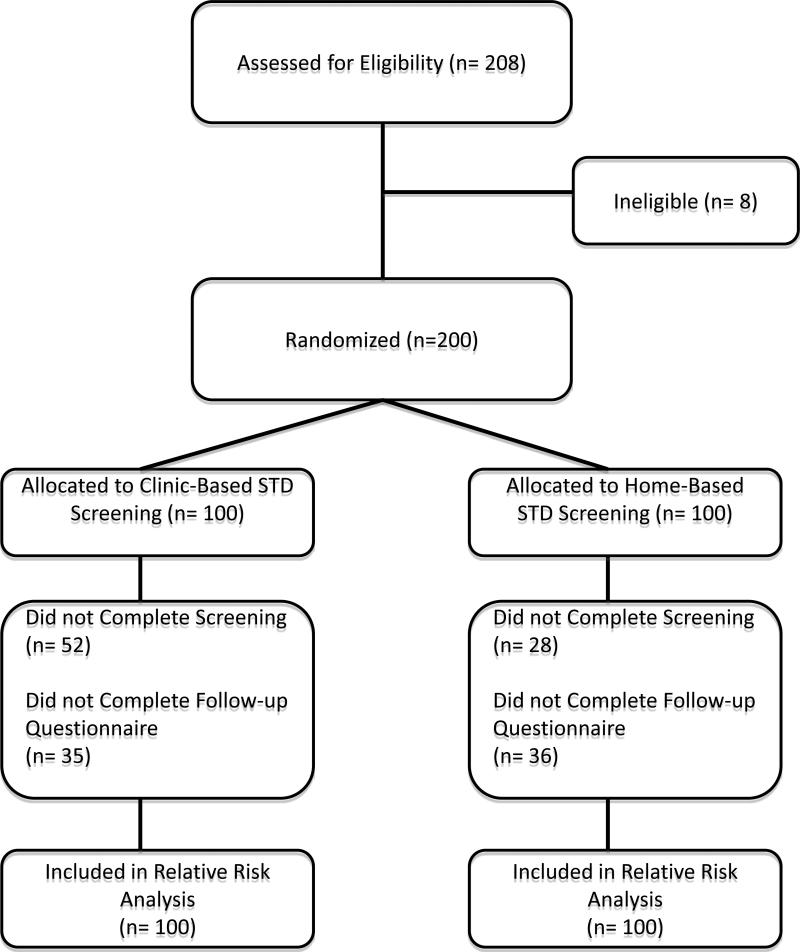
Between June 2011 and September 2011, 226 men were referred to the study through the community research collaborative; 112 (49.5%) of these men contacted the study. Between June 2010 and September 2011, 96 men were referred to the study through study brochures or word-of-mouth. In total, 208 men contacted the study and were screened for eligibility; eight men were ineligible and 200 men enrolled in the study (Figure 1).
Figure 1.
Flow diagram of study participants.
One hundred men were randomized to receive a home CT/GC screening kit and 100 men were scheduled for an in-person clinic visit to complete the CT/GC screening kit. There were no significant differences in baseline demographic and behavioral characteristics between the two groups (Table 1). The mean age among men in the home and clinic groups was 31.2 and 30.3 years, respectively. The majority of participants were single at the time of enrollment (59% for home group and 61% for clinic group). Half of participants reported their current educational attainment as “high school or less” (57% for home group and 44% for clinic group). One in five men reported two or more sexual partners in the past 30 days, and one in four reported never using condoms during sex. Nearly 40% of participants reported a lifetime history of sexually transmitted infections, of which 19% reported having the infection within the past six months.
Overall, 60% (n=120) of participants completed STD screening, regardless of group assignment (Table 2). Men were more likely to complete the screening kit if they were younger, white, had a college or graduate degree, or were assigned to receive a home kit (p<0.01). In multivariate analysis, men assigned a home kit were 60% more likely to complete screening compared to men assigned to clinic screening [adjusted relative risk (RRadj)= 1.59; 95% confidence interval (CI) 1.26, 2.00]. Screening kit completion was also associated with age (RRadj=0.98; 95% CI 0.96, 0.99]) and white race (RRadj=1.46; 95% CI 1.16, 1.84]).
Among men randomized to home-based screening, 72% completed screening and 28% did not complete screening. There were no differences in baseline demographics or behavioral characteristics between the groups that did and did not complete screening. Among men randomized to clinic-based screening, 48% completed screening and 52% did not complete screening. Men were less likely to complete clinic-based screening if they were older, black, less educated, or uninsured (Table 2).
Among the men who completed an STD screening kit, we identified four cases (3.3%) of CT and three cases (2.5%) of GC. There were three cases of GC and one case of CT in the home-based screening group compared to three cases of CT in the clinic-based screening group. Men who screened positive for CT (mean age=27 years, SD=8.0) and GC (mean age=22 years, SD=2.0) were significantly younger than other participants. All seven participants with positive screening results were treated for their infections at the study clinic.
Of the participants who completed the follow-up questionnaire (N=129 or 64.5%), 65 men were in the clinic-based screening group and 64 men were in the home-based screening group. Eighty percent of these men completed the assigned screening kit. Of those who completed the follow-up questionnaire, over 80% of men reported being “very satisfied” with their assigned screening method and thought the screening process was “very convenient;” 99% of respondents stated that they would recommend their assigned screening method to their male friends. For those assigned to clinic-based screening, 79% believed it would be “very easy” to use a urine screening kit at home. For those assigned to home-based STD screening, 95% stated it was “very easy” to follow the screening kit instructions. The number one reason men reported for completing the STD screen was the convenience of the screening kit (Table 3). Conversely, the most common reason that would prevent them from STD screening in the future is lack of health insurance (Table 3). Over 75% of men believed they were “not at all likely” to become infected with an STD in the next 6 months.
DISCUSSION
This study sought to determine the acceptability of STD screening using self-collected urine specimens among men randomized to either home- or clinic-based screening. Our findings demonstrate that men assigned to home-based screening have a higher screening completion rate (72%) compared to men assigned to a traditional clinic setting (48%). Other studies evaluating male screening in various non-traditional settings such as community or correctional centers and schools have reported screening rates of approximately 60%.14
A systematic review of STD screening among men has shown that home-based STD screening rates are slightly higher than those achieved by standard care.14 Nonetheless, the literature also demonstrates that overall acceptance of STD home screening by men is low. Previous studies have evaluated uptake and completion rates across different types of home-based screening. Also, studies have compared home-based screening to standard care, defined as traditional clinic visits.15-21 To our knowledge, no study in the U.S. has implemented a two arm interventional trial offering identical home- and clinic-based STD screening kits. Accordingly, our results demonstrate that when clinic-based and home-based urine screening are administered in a similar manner, home-based screening results in high acceptability and improved screening rates compared to clinic-based screening. These results are likely due to the removal of barriers associated with clinic-based screening, including transportation, time, financial costs, and concerns about both confidentiality and privacy.
Our results further demonstrate that men who are older, black, less educated, or uninsured are significantly less likely to complete clinic-based screening. Comparatively, there were no notable differences in the characteristics of men who did and who did not complete home-based screening. The CDC and USPSTF recognize major risk factors for acquiring STDs as black race, younger age, low socioeconomic status, history of STD, new or multiple partners, and inconsistent condom use.1-3 According to our study, home-based screening succeeds in reaching these high-risk subgroups.
Regardless of study group, convenience and free screening were reported as the top two reasons for completing the STD screen. Similar reasons were also cited as barriers to future screening, including the monetary costs associated with screening and the lack of transportation to or from a clinic. Our results suggest that the removal of financial, transportation, and time barriers are likely to increase STD screening rates among men. Interestingly, on average study participants lived within a 6.5 mile radius of our screening clinic. According to our follow-up questionnaires, over 84% of participants were willing to travel 10 miles or more to be screened. Therefore, our clinic location was likely not a major factor in the participants’ failure to complete clinic-based screening.
This study has a number of strengths. The study is an adequately powered randomized controlled trial. We recruited men through multiple methods including community-based outreach to extend participation to men with less healthcare access or utilization. Also, unlike many previous studies, both arms of our intervention involved identical screening procedures reducing the possibility of confounding factors. Additionally, our study did not send reminders to participants to complete their screening kits; this more accurately reflects clinical care compared to other research studies. Nonetheless, our study is not without limitations. There was only one clinic site available for clinic-based screening, which may not have been a convenient location for some men. We provided a small incentive to all participants regardless of whether they completed screening. This incentive may diminish real world application in which no monetary incentive would be available for screening participation. Furthermore, due to changes in participant contact information during the study period, we were unable to reach 35% of the participants to obtain follow-up information regarding their screening experience. However, participants who did not complete the follow-up questionnaire were equally distributed across the two intervention arms, reducing potential bias in the follow-up interview findings. And lastly, our study evaluated only 100 men in each intervention arm; thus, only 7 cases of CT and/or GC were identified.
This study is one of the first randomized clinical trials conducted in the U.S. to specifically evaluate home-based versus clinic-based STD screening in men. The high rate of screen completion and acceptability of home-based urine STD screening kits among our study participants demonstrate that more men would participate in STD screening if home-based screening kits were available and offered as an alternative to traditional STD screening methods. Our findings emphasize the need to encourage and implement innovative approaches such as home-based urine screening to increase male STD screening rates. Nonetheless, a better understanding of why high-risk men are less likely to complete screening is needed in order to develop screening programs that reach the population at highest risk.
SHORT SUMMARY.
Home-based nucleic acid amplification screening kits of urine specimens for Chlamydia trachomatis and Neisseria gonorrhoeae achieved higher screening rates in men compared to clinic-based screening.
Acknowledgments
Study funded by an Anonymous Foundation and Grant Numbers UL1 RR024992 and TL1 RR024995 from the Clinical and Translational Science Award (CTSA) program of the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research. This work was also supported by a grant from the Doris Duke Charitable Foundation to Washington University in St. Louis School of Medicine to fund Clinical Research Fellow Hanna Xu.
Footnotes
There are no relevant conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.U.S. Preventive Services Task Force . Ann Intern Med. Vol. 147. Agency for Healthcare Research and Quality; Rockville, MD: Jun, 2007. Screening for Chlamydial Infection: Recommendation Statement. pp. 128–133. 2007. [Google Scholar]
- 2.Centers for Disease Control and Prevention . Sexually Transmitted Diseases Surveillance, 2010. U.S. Department of Health and Human Services; Atlanta, GA: Nov. 2011. [Google Scholar]
- 3.U.S. Preventive Services Task Force . Screening for Gonorrhea: Recommendation Statement. Agency for Healthcare Research and Quality; Rockville, MD: May, 2005. AHRW Publication No. 05-0579-A. [PubMed] [Google Scholar]
- 4.Blake DR, Quinn TC, Gaydos CA. Should asymptomatic men be included in Chlamydia screening programs? Cost-effectiveness of Chlamydia screening among male and female entrants to a national job training program. Sex Transm Dis. 2008;35(1):S45–S50. doi: 10.1097/olq.0b013e31814b86f5. [DOI] [PubMed] [Google Scholar]
- 5.Fine D, Dicker L, Mosure D, et al. Increasing chlamydia positivity in women screened in family planning clinics: Do we know why? Sex Transm Dis. 2008;35:47–52. doi: 10.1097/OLQ.0b013e31813e0c26. [DOI] [PubMed] [Google Scholar]
- 6.Brunham RC, Pourbohloul B, Mak S, et al. The unexpected impact of a Chlamydia trachomatis infection control program on susceptibility to reinfection. J Infect Dis. 2005;192:1836–1844. doi: 10.1086/497341. [DOI] [PubMed] [Google Scholar]
- 7.Jones C. Urine Screening for Gonococcal and Chlamydia Infections at Community-Based Organization in a High-Morbidity Area. Sex Transm Dis. 2000;27(3):146–151. doi: 10.1097/00007435-200003000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Aral SO, Wasserheit JN. Social and behavioral correlates of pelvic inflammatory disease. Sex Transm Dis. 1998;25:378–385. doi: 10.1097/00007435-199808000-00010. [DOI] [PubMed] [Google Scholar]
- 9.Gunn RA, Poschun BS, Fitzgerald S, et al. Screening high-risk adolescent males for Chlamydia trachomatis infection. Sex Tranm Dis. 1998:49–52. doi: 10.1097/00007435-199801000-00010. [DOI] [PubMed] [Google Scholar]
- 10.Gift TL, Blake DR, Gaydos CA, et al. The cost-effectiveness of screening men for Chlamydia trachomatis: A review of the literature. Sex Transm Dis. 2008;35(11):S51–S60. doi: 10.1097/OLQ.0b013e3181723dba. [DOI] [PubMed] [Google Scholar]
- 11.Gift TL, Gaydos CA, Kent CK, et al. The program cost and cost-effectiveness of screening men for Chlamydia to prevent pelvic inflammatory disease in women. Sex Transm Dis. 2008;35:S66–S75. doi: 10.1097/OLQ.0b013e31818b64ac. [DOI] [PubMed] [Google Scholar]
- 12.Marrazzo JM, Scholes D. Acceptability of urine-based screening for Chlamydia trachomatis in asymptomatic young men: A systematic review. Sex Transm Dis. 2008;35(11):S28–S33. doi: 10.1097/OLQ.0b013e31816938ca. [DOI] [PubMed] [Google Scholar]
- 13.Scholes D, Heidrich FE, Yarbro P, et al. Population-based outreach for Chlamydia screening in men: Results from a randomized trial. Sex Transm Dis. 2007;34(11):837–839. doi: 10.1097/OLQ.0b013e31805ba860. [DOI] [PubMed] [Google Scholar]
- 14.Gaydos CA, Ferrero DV, Papp J. Laboratory aspects of screening men for Chlamydia trachomatis in the new millennium. Sex Transm Dis. 2008;35(11):S45–S50. doi: 10.1097/OLQ.0b013e31816d1f6d. [DOI] [PubMed] [Google Scholar]
- 15.Stephenson J, Carder C, Copas A, et al. Home Screening for Chlamydial Genital Infection: Is It Acceptable to Young Men and Women? Sex Transm Inf. 2000;76:25–27. doi: 10.1136/sti.76.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Andersen B, Østergaara L, Møller JK, Olesen F. Effectiveness of a mass media campaign to recruit young adults for testing of Chlamydia trachomatis. Sex Transm Inf. 2001;77:416–418. doi: 10.1136/sti.77.6.416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Domeika M, Oscarsson L, Hallén A, et al. Mailed urine samples are not an effective screening approach for Chlamydia trachomatis case finding among young men. JEADV. 2007;21:789–794. doi: 10.1111/j.1468-3083.2006.02088.x. [DOI] [PubMed] [Google Scholar]
- 18.Rogstad KE, Bates SM, Partridge S, et al. The prevalence of Chlamydia trachomatis infection in male undergraduates: A postal survey. Sex Transm Infect. 2001;77:111–113. doi: 10.1136/sti.77.2.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.van Bergen J, Gotz HM, Richardus JH, et al. Prevalence of urogenital Chlamydia trachomatis increases significantly with level of urbanization and suggests targeted screening approaches: Results from the first national population based study in the Netherlands. Sex Transm Infect. 2005;81:17–23. doi: 10.1136/sti.2004.010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gotz HM, Veldhuijzen ID, van Bergen JE, et al. Acceptability and consequences of screening for Chlamydia trachomatis by home-based urine testing. Sex Transm Dis. 2005;32:557–562. doi: 10.1097/01.olq.0000175416.15905.db. [DOI] [PubMed] [Google Scholar]
- 21.Chai SJ, Aumakhan B, Barnes M, et al. Internet-based screening for sexually transmitted infections to reach nonclinic populations in the community: risk factors for infection in men. Sex Transm Dis. 2010;37(12):756–63. doi: 10.1097/OLQ.0b013e3181e3d771. [DOI] [PMC free article] [PubMed] [Google Scholar]