Abstract
Background
Patients with repaired tetralogy of Fallot (TOF) are monitored for pulmonary regurgitation (PR), and right ventricular (RV) function. We sought to compare measures of PR and RV function on echocardiogram to those on cardiac magnetic resonance (CMR), and to develop a new tool for assessing PR by echocardiogram.
Methods and Results
Patients with repaired TOF (N=143, 12.5± 3.2 years) had an echocardiogram and CMR within three months of each other. On echocardiogram, RV function was assessed by (1) Doppler tissue imaging of the RV free wall, and (2) myocardial performance index (MPI). The ratio of diastolic and systolic time-velocity integrals (DSTVI) measured by Doppler of the main pulmonary artery was calculated. CMR variables included RV ejection fraction (EF), RV volumes, and pulmonary regurgitant fraction (RF). Pulmonary regurgitation was graded as mild (RF <20%), moderate (RF=20–40%), and severe (RF>40%). On CMR, RF was 34±17% and RV EF was 61±8%. Echocardiography had good sensitivity identifying cases with RF>20% (sensitivity 97%, 95% CI: 92–99%) but overestimated the amount of PR when RF<20% (false positive rate 36%, 95% CI: 18–57%). The DSTVI on echocardiogram showed moderate correlation with RF on CMR (R=0.60, P<0.0001). On CMR, RF of 20% and 40% corresponded with a DSTVI of 0.49 (95% CI: 0.44–0.56), and 0.72 (95% CI: 0.68–0.76), respectively. RV MPI correlated modestly with RV EF (r=−0.33, P<0.001).
Conclusions
This study suggests that the DSTVI ratio may make a modest contribution to the overall assessment of PR in patients with repaired TOF and warrants further investigation. However, echocardiography continues to have a limited ability to quantify PR and RV function as compared to CMR.
Keywords: echocardiography, regurgitation, tetralogy of Fallot
Patients with tetralogy of Fallot (TOF) following surgical repair represent a growing population with congenital heart disease as they now survive into adulthood. 1–4 Residual pulmonary regurgitation (PR) is an important determinant of outcome as it may contribute to right ventricular (RV) enlargement and dysfunction, and result in exercise intolerance, a propensity for arrhythmias and an increased risk for sudden cardiac death. 3, 5 Most studies suggest that restoration of pulmonary valve competency decreases right ventricular volumes and improves exercise capacity, though a recent meta-analysis found that pulmonary valve replacement (PVR) does not confer significant changes in RV ejection fraction (EF) nor does it change the duration of the QRS complex. 6, 7, 8 The long-term results of pulmonary valve replacement are also not well defined. Though the long term consequences of and optimal timing for such intervention remains incompletely defined, the longitudinal assessment of PR and RV function remain critical in the medical care of the patient with TOF. 6, 9–12
Cardiac magnetic resonance (CMR) is the current reference standard to evaluate RV performance and PR, thanks to its ability to quantify volumes and flow. 13, 14 However, CMR is not readily available in all institutions and not as readily accomplished in all patients as compared to echocardiography, which therefore remains the mainstay for routine assessment of the post-surgical TOF patient. Echocardiographic assessment of RV function and PR is nonetheless limited by the complex right ventricular geometric shape. To overcome these challenges, techniques such as tissue Doppler derived tricuspid annular velocities, the right ventricular myocardial performance index (MPI), and 3D calculation of volumes and function have emerged to aid in the echocardiographic assessment of RV systolic function but each method presents new challenges. 15, 16, 17, 18, 19–23 Likewise, attempts at classifying the severity of PR by echocardiogram have been made. 24, 25 However, the inability of other studies to replicate those measures raises questions as to their validity. 26
We therefore sought to compare qualitative and quantitative measures of PR and RV function on echocardiogram to those on CMR in a large cohort of post-surgical TOF patients, and to test new measurements of PR on echocardiogram. Such measurements may simplify the longitudinal clinical assessment of operated TOF patients, and may provide endpoints for long-term research studies.
Methods
This study was approved by The Children’s Hospital of Philadelphia Institutional Review Board for human research, with written informed consent and assent obtained according to the institution’s guidelines.
Patients
Patients from 8–18 years of age with surgically repaired tetralogy of Fallot were prospectively enrolled in a cross sectional study (Table 1). An echocardiogram and CMR were performed within three months of each other in each patient according to a study protocol.
Table 1.
General patient characteristics
| Variable | Value* |
|---|---|
| Age (years) | 12.5 (± 3.2) |
| Gender | |
| Female | 47 (33%) |
| Male | 96 (67%) |
| Race | |
| White | 114 (80%) |
| African American | 16 (11%) |
| Other | 13 (9%) |
| Weight (kg) | 42.9 (± 15.3) |
| Age (years) at surgical repair | 0.30 (0.10, 0.57) |
| Time elapsed (years) since surgical repair | 11.5 (9.1,14.5) |
| Original pulmonary valve | |
| Stenosis | 112 (78%) |
| Atresia | 22 (15%) |
| Absent | 9 (6%) |
| Surgical repair | |
| VSD closure only† | 19 (13%) |
| Non-transannular patch‡ | 8 (6%) |
| Transannular patch | 103 (72%) |
| RV-PA conduit§ | 13 (9%) |
Data are expressed as mean (± SD), median (interquartile range), or as number (percentage).
Ventricular septal defect closure indicating that relief of outflow tract obstruction was not necessary.
Non-transannular patch refers to relief of right ventricular outflow tract obstruction without crossing the pulmonary valve annulus.
Right ventricle to pulmonary artery.
Echocardiogram
Echocardiograms were performed using standard pediatric views 27 in a Phillips IE33 machine (Phillips, Andover, MA, USA). Images were acquired with 3–8 MHz transducers, suited for patient’s size and acoustic windows. Color, pulse wave, and continuous-wave Doppler flow data across the pulmonary valve were acquired. Myocardial velocities using tissue Doppler were acquired from the lateral annulus of the tricuspid valve. Images were digitally stored and measurements performed offline using Syngo Dynamics software (Siemens, Ann Arbor, MI, USA) by a single echocardiographer (J.R.), who was blinded to subject information and CMR results.
Qualitative assessment of RV function was classified as normal, mildly, moderately, or severely decreased.
Quantitative RV function was assessed by: (1) Doppler Tissue Imaging (DTI) of the RV free wall just beneath the tricuspid valve annulus from which the systolic s’ wave, diastolic e’ and a’ waves were measured, corresponding to systolic, early and late right ventricular filling, respectively. (2) Myocardial Performance Index (MPI), calculated from pulsed-waved Doppler interrogation of the tricuspid inflow (apical four chamber view) and main pulmonary artery flow (parasternal short axis view). The sum of the RV isovolumetric contraction time and isovolumetric relaxation time was obtained by subtracting the RV ejection time in the main pulmonary artery from the interval between cessation and onset of the tricuspid inflow velocities. The MPI index was obtained by dividing the sum of both isovolumetric intervals by the ejection time.28
The main pulmonary artery was interrogated by color, pulsed, and continuous-wave Doppler. PR was qualitatively assessed by color-flow mapping and graded as none, mild or greater than mild utilizing visual inspection of the width of the regurgitant jet in relation to the outflow tract diameter (< 25% = mild).
The pulsed-wave Doppler tracing was used to obtain the time-velocity integrals of diastolic and systolic flows (Figure 1). The calculated ratio between the regurgitant (diastolic) time-velocity integral to the antegrade (systolic) time-velocity integral was called diastolic to systolic time-velocity integral ratio, or DSTVI.
Figure 1.
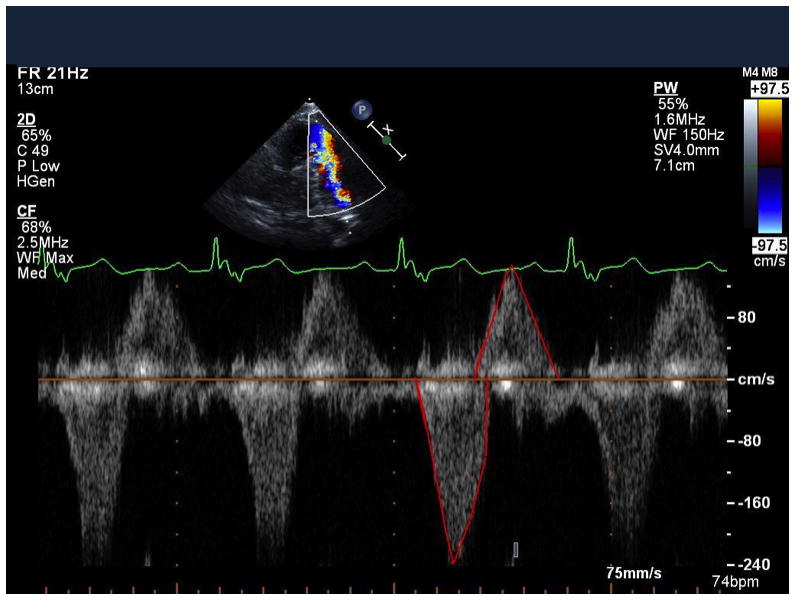
Pulsed wave Doppler in the main pulmonary artery in a patient with repaired tetralogy of Fallot and residual pulmonary regurgitation. Diastolic (above the baseline) and systolic (below the baseline) flows were traced (shown in red) to obtain the DSTVI. In this example, DSTVI= 0.612, corresponding to moderate-severe pulmonary regurgitation by CMR (RF = 47%).
Cardiac Magnetic Resonance
CMR studies were performed on a 1.5-T Avanto Whole Body Magnetic Resonance System (Siemens Medical Solutions, Erlanghen, Germany) with a 6-channel body-array coil scanner using a standard imaging protocol, which included steady-state free-precession cine CMR acquisitions in 4-chamber and long-axis planes and contiguous short-axis cine imaging from the atrioventricular junction through the cardiac apex. Sedation was used when appropriate according to patient’s age and ability to lie still for the scan. To assess end-systolic (ESV) and end-diastolic volumes (EDV) of the ventricles, a cine-MR sequence in a short-axis view was used (TE/TR 2.0/45ms, flip angle 75–90°, matrix size 196×196). The RV infundibulum was included in the RV volume up to the pulmonary annulus. All volumes were indexed to body surface area and corresponding z-scores were calculated using published normative data. 29, 30 Right ventricular EF was calculated as: stroke volume (SV) minus the EDV divided by the EDV (RVEF= SV-EDV/EDV). Phase contrast velocity mapping with a flow-sensitive gradient-echo sequence was performed in the main pulmonary artery to assess the regurgitant fraction.
CMR variables included RVEF, RV EDV and RV ESV, and pulmonary artery regurgitant fraction (RF). PR was graded as mild if the RF on CMR was less than 20%; moderate if it was between 20 and 40%, and severe if it was greater than 40%.
Statistical Analysis
Continuous variables were described using mean and standard deviation (SD) or median with inter-quartile ranges (IQR) when appropriate. Categorical variables were described using count and percentages. We calculated sensitivity and false positive rate (1-specificity) of echocardiogram (defined as mild PR or not) to grade pulmonary regurgitation using the RF found on CMR (dichotomized at 20%) as the gold standard. Pearson correlation was calculated between DSTVI on echocardiogram and RF on CMR. A linear regression of RF from CMR was fit on DSTVI from echocardiogram to identify clinically meaningful cut points of DSTVI. Measures of RV function from echocardiogram and CMR were correlated using Pearson correlation, and RV MPI was compared in patients with diminished RV systolic function and normal function. Statistical significance was reached if p-values were < 0.05 (2-sided tests). All analyses were performed using SAS statistical software version 9.2 (Cary, NC, USA).
Results
Patient characteristics
The study cohort consisted of 143 patients with TOF following surgical repair that underwent an echocardiogram and CMR within three months of each other for study purposes. Patient characteristics are detailed in Table 1. Surgical repair consisted of four approaches: (1) simple closure of ventricular septal defect when no significant RV outflow tract obstruction was present, (2) closure of the VSD with relief of RV outflow tract obstruction with a transannular patch, (3) closure of the VSD with relief of RV outflow tract obstruction with a non-transannular patch, (transannular or non-transannular), and (4) closure of the VSD with placement of an RV to pulmonary artery conduit. Most did not have a residual ventricular septal defect and few (20/135) had right ventricular outflow tract obstruction graded as > mild on CMR.
Assessment of PR and RV function
The majority of patients (85%) had greater than mild PR assessed qualitatively both by Echocardiogram and CMR. In addition, most patients had qualitatively normal RV systolic shortening by Echocardiogram and CMR (75% and 90 %, respectively). Quantitative measures of PR and RV function are detailed in Table 2 for each imaging modality. Of note, the mean regurgitant fraction by CMR in the cohort was 34.2% (±16.6%), and the mean RVEF was 60.6% (±8.2%), suggesting that the majority had at least moderate PR with preserved RV shortening.
Table 2.
Echocardiographic and CMR measures
| Echocardiogram | Value* |
|---|---|
| Pulmonary regurgitation (%)† | |
| None | 3 (2%) |
| Trivial/ mild | 17 (12%) |
| > Mild | 122 (86%) |
| RV function (%) | |
| Normal | 106 (74%) |
| Mildly decreased | 25 (17%) |
| Moderately decreased | 12 (9%) |
| RV MPI ‡ | 0.21 (± 0.16) |
| RV tricuspid peak S wave velocity (cm/sec) | 8.9 (± 2.1) |
| CMR | Value |
|---|---|
| Pulmonary regurgitation > mild § | 120 (84%) |
| Pulmonary regurgitant fraction | 34.2 (± 16.6) |
| Pulmonary regurgitation % | | | |
| None | 6 (4%) |
| Mild | 19 (13%) |
| Moderate | 53 (37%) |
| Severe | 57 (40%) |
| RV ejection fraction | 60.6 (± 8.2%) |
| RV SV (mL) | 91.3 (±35.2) |
| RV end-diastolic volume (mL) | 152.6 (± 60.9) |
| RV end-systolic volume (mL) | 61.2 (± 30.4) |
Data are expressed as mean (± SD), or number (percentage).
Not available for assessment in 1 subject
Right ventricular myocardial performance index.
Qualitative assessment on cardiac magnetic resonance.
Pulmonary regurgitation % indicates pulmonary regurgitant fraction: mild PR= RF<20 %; moderate PR: RF 20–40%; severe PR: RF>40%. Pulmonary regurgitation assessment was not possible in 8 patients.
Correlations between echocardiographic and CMR measurements
Pulmonary regurgitation
We tested the ability of echocardiography to identify patients with greater than mild PR as measured on CMR (RF >20%). Echocardiography was 97% sensitive to identify cases with RF>20% (107 in 110 patients; 95% CI: 92–99 %) qualitatively, but overestimated PR when it was mild on CMR (RF<20%), resulting in a false positive rate of 36% (9 out of 25 patients; 95% CI: 18–58%) (Table 3).
Table 3.
Echocardiographic and CMR measures
| PR on Echocardiogram* | Regurgitant Fraction on CMR† | |||
|---|---|---|---|---|
| ≤Mild | Moderate | Severe | Total | |
| ≤Mild | 16 | 3 | 0 | 19 |
| > Mild | 9 | 50 | 57 | 116 |
| Total | 19 | 53 | 57 | 135* |
PR: pulmonary regurgitation
Degree of pulmonary regurgitation: mild if regurgitant fraction <20%; moderate if 20–40%; severe if >40%.
Of the 143 subjects, 135 had measurable PR by CMR, and of the 135, 6 had regurgitant fraction= 0%, therefore total n= 129.
As an alternative measure of PR by echocardiogram, the DSTVI correlated moderately with RF on CMR (r=0.60, p<0.0001). A CMR RF of 20% and 40% (representing the boundaries between mild/moderate and moderate/severe PR) corresponded with a DSTVI of 0.49 (95% CI: 0.44–0.56), and 0.72 (95% CI: 0.68–0.76), respectively (Figure 2). DSTVI greater than 1 was present in 12 patients, all of which had RF>40% by CMR (Figure 2).
Figure 2.
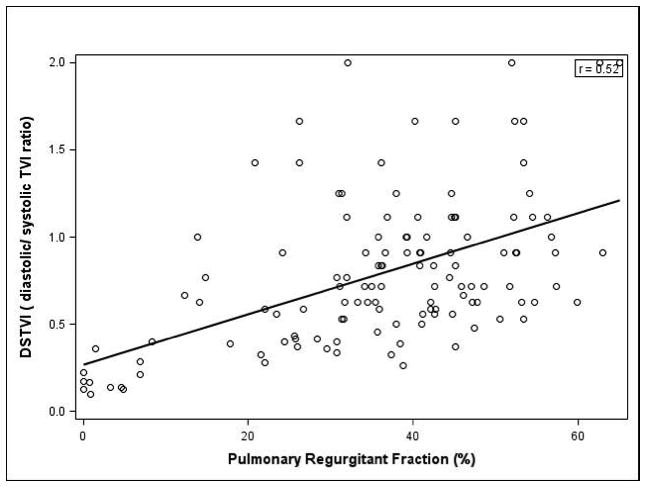
Scatter plot of diastolic-systolic time-velocity integral (DSTVI) vs. pulmonary regurgitant fraction
Regression equation: y = 0.27+0.011x; r=0.36, p<0.0001. DSTVI indicates diastolic to systolic time-velocity integral.
RV Function
Quantitative comparison of RV function by echocardiography and CMR showed a modest negative correlation between RV MPI and RV EF (r = −0.33, p<0.001), (Figure 3). RV MPI was appropriately higher (0.34 ±0.16 compared to 0.20 ±0.13; p<0.001) in those with diminished as compared to normal RV systolic function (EF ≤50% versus 50%). The systolic annular velocity of the tricuspid valve (S’) demonstrated no significant correlation with RVEF (r= 0.006, P= 0.94).
Figure 3.
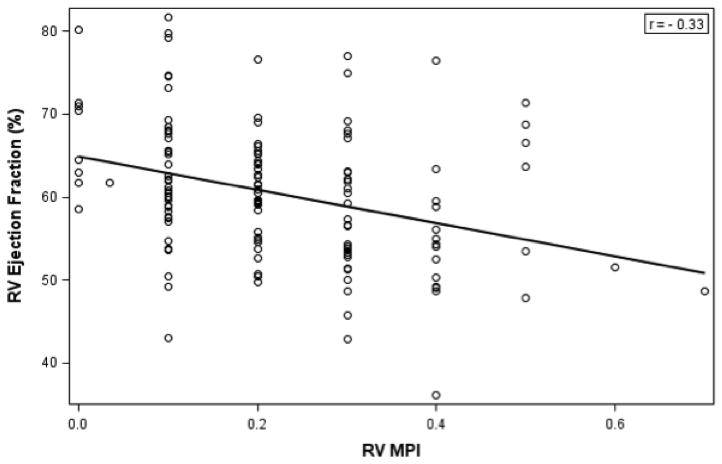
Scatter plot of right ventricular ejection fraction (%) and myocardial performance index (MPI) on echocardiogram.
Regression equation: y= 64.94 − 20.1x; r=−0.33; p < 0.001.
Discussion
Echocardiography plays an essential role in the longitudinal follow up of patients with congenital heart disease. Particularly in TOF, continued efforts have been made to use echocardiography to quantify PR and RV function, given the simplicity with which the study is performed. To date, no single echocardiographic measure of PR or RV function provides sufficient or accurate measures of hemodynamics when compared to catheterization and CMR. This study sought to further define the utility of echocardiography in the assessment of PR and RV function and to explore a new index of PR.
Comparing pulmonary regurgitation by Echocardiography and CMR
The assessment of PR by echocardiography has been largely qualitative, though multiple attempts to better quantify PR have been undertaken. 24, 25, 26, 31, 32 A number of measurements have been attempted including the Pulmonary Regurgitant Index, and in adults, the width of the vena contracta. 18, 24 However, such measurements have not proven reproducible and are not relevant to the repaired patient with TOF and a disrupted pulmonary valve. 32 As a result, echocardiographers use a number of imprecise observations to assess PR, including: Doppler patterns, the size of pulmonary arteries and right ventricle, the width of the PR regurgitant jet, and the extent of the diastolic retrograde flow. 33 Because of these limitations, we explored whether the DSTVI could better quantify PR. Our data suggest that the DSTVI correlated with RF on CMR, with higher DSTVI ratios corresponding to worse PR, as expected. While time-velocity integral (TVI) has been used for the calculation of cardiac outputs and left sided regurgitant lesions, we are not aware of its application in the quantification of pulmonary valve regurgitation. Therefore, though further validation and longitudinal studies are required to confirm its utility, it appears that the DSTVI may prove to be a helpful measure of PR. DSTVI greater than one was found in some patients with severe PR as measured by CMR; we propose that this phenomenon results from higher diastolic regurgitant velocity and dynamic changes in the pulmonary cross sectional area during the cardiac cycle in cases with severe pulmonary regurgitation. This finding merits further exploration in future studies.
Assessing Right Ventricular Function by Echocardiogram and CMR
Analysis of RV function by echocardiography is likewise challenging. We found that the MPI correlated poorly with RV ejection fraction even though the MPI was largely normal as compared to children without CHD. 34 This finding likely stems from the fact that isovolumic relaxation is not present or is shortened in a patient with severe PR whose RV is never entirely isovolumic during relaxation. In addition, the increased RV end-diastolic volume secondary to PR may increase the ejection time across the pulmonary valve, therefore lowering the MPI, a phenomenon previously called pseudonormalization. 35 When segregated by normal versus abnormal RV function on CMR, the MPI was appropriately lower in those with normal function, indicating that at least it followed the trend of ejection fraction, similar to previous studies. 16 Thus, it appears that the RV MPI may be difficult to interpret in the face of significant PR when there is essentially no isovolumic relaxation of the RV.
Our data demonstrate that the tricuspid annular systolic velocity was decreased as compared to normal values in adults without congenital heart disease in the absence of adequate normative data for children. 15, 36 Similar findings have been reported in patients with TOF. 37 Moreover, we were unable to confirm the previously reported association between the tissue Doppler derived tricuspid valve lateral annulus systolic velocity and RV EF, even though it is intuitive to compare two methods that evaluate systolic function. 15, 38 It is possible that in patients with tetralogy of Fallot and considerable ventricular dilation secondary to PR, this comparison is limited by the greater load-dependency of RVEF as compared to myocardial velocities.
Other methods with which to assess RV function have been proposed.39 We chose not to measure the RV fractional area change particularly because it was shown recently to correlate poorly with RV ejection fraction on CMR in a population with congenital heart disease. 40 In addition, it is technically difficult to delineate the endocardial border in the repaired TOF RV and this measurement does not incorporate the contribution from the RV outflow tract. The tricuspid annular plane systolic excursion (TAPSE) is another modality to assess RV function that may prove useful in TOF, but may be likewise limited by the exclusion of the RV outflow tract from the calculation. 41
In summary, our data suggest a modest correlation of DSTVI with pulmonary regurgitant fraction on CMR. Thus, the DSTVI may provide a quantitative tool to follow PR by echocardiography, although further validation and longitudinal studies are required to confirm its utility.
Limitations
Patients with severely decreased right ventricular function were not represented in our cross sectional study population, most likely given the relative youth of this cohort as compared to other studies that include adults.
While sedation may result in differences in hemodynamics if comparing a sedated CMR to a non-sedated echocardiogram, we ensured that the interval between the tests did not exceed three months in order to minimize the possibility of hemodynamic changes over time.
Finally, the cross sectional nature of this study does not allow for longitudinal inferences, where these assessments would be most helpful.
Conclusion
Even with the techniques studied, echocardiography has a limited ability to quantify PR and RV function in the TOF population. We propose that the DSTVI ratio may be a helpful quantitative tool for the assessment of PR by echocardiography in conjunction with other measures. However, further validation and longitudinal studies are required to confirm its utility.
Commentary.
Patients with tetralogy of Fallot represent a growing population of congenital heart disease. Clinicians seek to quantify pulmonary regurgitation and right ventricular function over successive appointments in patients with TOF to identify those in need of intervention or pulmonary valve replacement. To date, though echocardiography is the most valuable tool, it has fallen short in consistent quantification of pulmonary regurgitation and right ventricular function. In this study we describe an echocardiographic tool with which to assess pulmonary regurgitation in tetralogy of Fallot that only modestly correlates with measurements made by cardiac magnetic resonance. In addition, echocardiographic measures of right ventricular function showed limited performance when compared to those derived from cardiac magnetic resonance. While these echo measures still fall short of the reliability set by CMR for decision-making, these results help motivate ongoing investigative efforts to improve echocardiographic assessment of the post-operative patient with tetralogy of Fallot.
Acknowledgments
Sources of Funding
This work was supported by the National Institutes of Health [P50-HL74731].
Footnotes
Disclosures
None.
References
- 1.Murphy JG, Gersh BJ, Mair DD, Fuster V, McGoon MD, Ilstrup DM, McGoon DC, Kirklin JW, Danielson GK. Long-term outcome in patients undergoing surgical repair of tetralogy of fallot. N Engl J Med. 1993;329:593–599. doi: 10.1056/NEJM199308263290901. [DOI] [PubMed] [Google Scholar]
- 2.Nollert G, Fischlein T, Bouterwek S, Bohmer C, Klinner W, Reichart B. Long-term survival in patients with repair of tetralogy of fallot: 36-year follow-up of 490 survivors of the first year after surgical repair. J Am Coll Cardiol. 1997;30:1374–1383. doi: 10.1016/s0735-1097(97)00318-5. [DOI] [PubMed] [Google Scholar]
- 3.Hickey EJ, Veldtman G, Bradley TJ, Gengsakul A, Manlhiot C, Williams WG, Webb GD, McCrindle BW. Late risk of outcomes for adults with repaired tetralogy of fallot from an inception cohort spanning four decades. Eur J Cardiothorac Surg. 2009;35:156–164. doi: 10.1016/j.ejcts.2008.06.050. [DOI] [PubMed] [Google Scholar]
- 4.Bacha EA, Scheule AM, Zurakowski D, Erickson LC, Hung J, Lang P, Mayer JE, Jr, del Nido PJ, Jonas RA. Long-term results after early primary repair of tetralogy of fallot. J Thorac Cardiovasc Surg. 2001;122:154–161. doi: 10.1067/mtc.2001.115156. [DOI] [PubMed] [Google Scholar]
- 5.Gatzoulis MA, Balaji S, Webber SA, Siu SC, Hokanson JS, Poile C, Rosenthal M, Nakazawa M, Moller JH, Gillette PC, Webb GD, Redington AN. Risk factors for arrhythmia and sudden cardiac death late after repair of tetralogy of fallot: A multicentre study. Lancet. 2000;356:975–981. doi: 10.1016/S0140-6736(00)02714-8. [DOI] [PubMed] [Google Scholar]
- 6.Warner KG, O’Brien PK, Rhodes J, Kaur A, Robinson DA, Payne DD. Expanding the indications for pulmonary valve replacement after repair of tetralogy of fallot. Ann Thorac Surg. 2003;76:1066–1071. doi: 10.1016/s0003-4975(03)00748-3. [DOI] [PubMed] [Google Scholar]
- 7.Frigiola A, Tsang V, Bull C, Coats L, Khambadkone S, Derrick G, Mist B, Walker F, van Doorn C, Bonhoeffer P, Taylor AM. Biventricular response after pulmonary valve replacement for right ventricular outflow tract dysfunction: Is age a predictor of outcome? Circulation. 2008;118:S182–190. doi: 10.1161/CIRCULATIONAHA.107.756825. [DOI] [PubMed] [Google Scholar]
- 8.Cheung EW, Wong WH, Cheung YF. Meta-analysis of pulmonary valve replacement after operative repair of tetralogy of fallot. Am J Cardiol. 2010;106:552–557. doi: 10.1016/j.amjcard.2010.03.065. [DOI] [PubMed] [Google Scholar]
- 9.Oosterhof T, van Straten A, Vliegen HW, Meijboom FJ, van Dijk AP, Spijkerboer AM, Bouma BJ, Zwinderman AH, Hazekamp MG, de Roos A, Mulder BJ. Preoperative thresholds for pulmonary valve replacement in patients with corrected tetralogy of fallot using cardiovascular magnetic resonance. Circulation. 2007;116:545–551. doi: 10.1161/CIRCULATIONAHA.106.659664. [DOI] [PubMed] [Google Scholar]
- 10.Buechel ER, Dave HH, Kellenberger CJ, Dodge-Khatami A, Pretre R, Berger F, Bauersfeld U. Remodelling of the right ventricle after early pulmonary valve replacement in children with repaired tetralogy of fallot: Assessment by cardiovascular magnetic resonance. Eur Heart J. 2005;26:2721–2727. doi: 10.1093/eurheartj/ehi581. [DOI] [PubMed] [Google Scholar]
- 11.Dave HH, Buechel ER, Dodge-Khatami A, Kadner A, Rousson V, Bauersfeld U, Pretre R. Early insertion of a pulmonary valve for chronic regurgitation helps restoration of ventricular dimensions. Ann Thorac Surg. 2005;80:1615–1620. doi: 10.1016/j.athoracsur.2005.04.058. [DOI] [PubMed] [Google Scholar]
- 12.Therrien J, Provost Y, Merchant N, Williams W, Colman J, Webb G. Optimal timing for pulmonary valve replacement in adults after tetralogy of fallot repair. Am J Cardiol. 2005;95:779–782. doi: 10.1016/j.amjcard.2004.11.037. [DOI] [PubMed] [Google Scholar]
- 13.Geva T. Repaired tetralogy of fallot: The roles of cardiovascular magnetic resonance in evaluating pathophysiology and for pulmonary valve replacement decision support. J Cardiovasc Magn Reson. 2011;13:9. doi: 10.1186/1532-429X-13-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pennell DJ, Sechtem UP, Higgins CB, Manning WJ, Pohost GM, Rademakers FE, van Rossum AC, Shaw LJ, Yucel EK. Clinical indications for cardiovascular magnetic resonance (cmr): Consensus panel report. J Cardiovasc Magn Reson. 2004;6:727–765. doi: 10.1081/jcmr-200038581. [DOI] [PubMed] [Google Scholar]
- 15.Meluzin J, Spinarova L, Bakala J, Toman J, Krejci J, Hude P, Kara T, Soucek M. Pulsed doppler tissue imaging of the velocity of tricuspid annular systolic motion; a new, rapid, and non-invasive method of evaluating right ventricular systolic function. Eur Heart J. 2001;22:340–348. doi: 10.1053/euhj.2000.2296. [DOI] [PubMed] [Google Scholar]
- 16.Schwerzmann M, Samman AM, Salehian O, Holm J, Provost Y, Webb GD, Therrien J, Siu SC, Silversides CK. Comparison of echocardiographic and cardiac magnetic resonance imaging for assessing right ventricular function in adults with repaired tetralogy of fallot. Am J Cardiol. 2007;99:1593–1597. doi: 10.1016/j.amjcard.2007.01.035. [DOI] [PubMed] [Google Scholar]
- 17.Lancellotti P, Tribouilloy C, Hagendorff A, Moura L, Popescu BA, Agricola E, Monin JL, Pierard LA, Badano L, Zamorano JL. European association of echocardiography recommendations for the assessment of valvular regurgitation. Part 1: Aortic and pulmonary regurgitation (native valve disease) Eur J Echocardiogr. 2010;11:223–244. doi: 10.1093/ejechocard/jeq030. [DOI] [PubMed] [Google Scholar]
- 18.Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ. Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and doppler echocardiography. J Am Soc Echocardiogr. 2003;16:777–802. doi: 10.1016/S0894-7317(03)00335-3. [DOI] [PubMed] [Google Scholar]
- 19.van der Zwaan HB, Helbing WA, Boersma E, Geleijnse ML, McGhie JS, Soliman OI, Roos-Hesselink JW, Meijboom FJ. Usefulness of real-time three-dimensional echocardiography to identify right ventricular dysfunction in patients with congenital heart disease. Am J Cardiol. 2008;106:843–850. doi: 10.1016/j.amjcard.2010.05.008. [DOI] [PubMed] [Google Scholar]
- 20.van der Zwaan HB, Helbing WA, McGhie JS, Geleijnse ML, Luijnenburg SE, Roos-Hesselink JW, Meijboom FJ. Clinical value of real-time three-dimensional echocardiography for right ventricular quantification in congenital heart disease: Validation with cardiac magnetic resonance imaging. J Am Soc Echocardiogr. 2010;23:134–140. doi: 10.1016/j.echo.2009.12.001. [DOI] [PubMed] [Google Scholar]
- 21.Grewal J, Majdalany D, Syed I, Pellikka P, Warnes CA. Three-dimensional echocardiographic assessment of right ventricular volume and function in adult patients with congenital heart disease: Comparison with magnetic resonance imaging. J Am Soc Echocardiogr. 2010;23:127–133. doi: 10.1016/j.echo.2009.11.002. [DOI] [PubMed] [Google Scholar]
- 22.Leibundgut G, Rohner A, Grize L, Bernheim A, Kessel-Schaefer A, Bremerich J, Zellweger M, Buser P, Handke M. Dynamic assessment of right ventricular volumes and function by real-time three-dimensional echocardiography: A comparison study with magnetic resonance imaging in 100 adult patients. J Am Soc Echocardiogr. 2010;23:116–126. doi: 10.1016/j.echo.2009.11.016. [DOI] [PubMed] [Google Scholar]
- 23.Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, Picard MH, Roman MJ, Seward J, Shanewise JS, Solomon SD, Spencer KT, Sutton MS, Stewart WJ. Recommendations for chamber quantification: A report from the american society of echocardiography’s guidelines and standards committee and the chamber quantification writing group, developed in conjunction with the european association of echocardiography, a branch of the european society of cardiology. J Am Soc Echocardiogr. 2005;18:1440–1463. doi: 10.1016/j.echo.2005.10.005. [DOI] [PubMed] [Google Scholar]
- 24.Li W, Davlouros PA, Kilner PJ, Pennell DJ, Gibson D, Henein MY, Gatzoulis MA. Doppler-echocardiographic assessment of pulmonary regurgitation in adults with repaired tetralogy of fallot: Comparison with cardiovascular magnetic resonance imaging. Am Heart J. 2004;147:165–172. doi: 10.1016/s0002-8703(03)00527-1. [DOI] [PubMed] [Google Scholar]
- 25.Yang H, Pu M, Chambers CE, Weber HS, Myers JL, Davidson WR., Jr Quantitative assessment of pulmonary insufficiency by doppler echocardiography in patients with adult congenital heart disease. J Am Soc Echocardiogr. 2008;21:157–164. doi: 10.1016/j.echo.2007.06.003. [DOI] [PubMed] [Google Scholar]
- 26.Wald RM, Redington AN, Pereira A, Provost YL, Paul NS, Oechslin EN, Silversides CK. Refining the assessment of pulmonary regurgitation in adults after tetralogy of fallot repair: Should we be measuring regurgitant fraction or regurgitant volume? Eur Heart J. 2009;30:356–361. doi: 10.1093/eurheartj/ehn595. [DOI] [PubMed] [Google Scholar]
- 27.Lai WW, Geva T, Shirali GS, Frommelt PC, Humes RA, Brook MM, Pignatelli RH, Rychik J. Guidelines and standards for performance of a pediatric echocardiogram: A report from the task force of the pediatric council of the american society of echocardiography. J Am Soc Echocardiogr. 2006;19:1413–1430. doi: 10.1016/j.echo.2006.09.001. [DOI] [PubMed] [Google Scholar]
- 28.Ishii M, Eto G, Tei C, Tsutsumi T, Hashino K, Sugahara Y, Himeno W, Muta H, Furui J, Akagi T, Fukiyama R, Toyoda O, Kato H. Quantitation of the global right ventricular function in children with normal heart and congenital heart disease: A right ventricular myocardial performance index. Pediatr Cardiol. 2000;21:416–421. doi: 10.1007/s002460010100. [DOI] [PubMed] [Google Scholar]
- 29.Sarikouch S, Peters B, Gutberlet M, Leismann B, Kelter-Kloepping A, Koerperich H, Kuehne T, Beerbaum P. Sex-specific pediatric percentiles for ventricular size and mass as reference values for cardiac mri: Assessment by steady-state free-precession and phase-contrast mri flow. Circ Cardiovasc Imaging. 2009;3:65–76. doi: 10.1161/CIRCIMAGING.109.859074. [DOI] [PubMed] [Google Scholar]
- 30.Robbers-Visser D, Boersma E, Helbing WA. Normal biventricular function, volumes, and mass in children aged 8 to 17 years. J Magn Reson Imaging. 2009;29:552–559. doi: 10.1002/jmri.21662. [DOI] [PubMed] [Google Scholar]
- 31.Festa P, Ait-Ali L, Minichilli F, Kristo I, Deiana M, Picano E. A new simple method to estimate pulmonary regurgitation by echocardiography in operated fallot: Comparison with magnetic resonance imaging and performance test evaluation. J Am Soc Echocardiogr. 2010;23:496–503. doi: 10.1016/j.echo.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 32.Renella P, Aboulhosn J, Lohan DG, Jonnala P, Finn JP, Satou GM, Williams RJ, Child JS. Two-dimensional and doppler echocardiography reliably predict severe pulmonary regurgitation as quantified by cardiac magnetic resonance. J Am Soc Echocardiogr. 2010;23:880–886. doi: 10.1016/j.echo.2010.05.019. [DOI] [PubMed] [Google Scholar]
- 33.Redington AN. Determinants and assessment of pulmonary regurgitation in tetralogy of fallot: Practice and pitfalls. Cardiol Clin. 2006;24:631–639. vii. doi: 10.1016/j.ccl.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 34.Eidem BW, Tei C, O’Leary PW, Cetta F, Seward JB. Nongeometric quantitative assessment of right and left ventricular function: Myocardial performance index in normal children and patients with ebstein anomaly. J Am Soc Echocardiogr. 1998;11:849–856. doi: 10.1016/s0894-7317(98)70004-5. [DOI] [PubMed] [Google Scholar]
- 35.Yasuoka K, Harada K, Toyono M, Tamura M, Yamamoto F. Tei index determined by tissue doppler imaging in patients with pulmonary regurgitation after repair of tetralogy of fallot. Pediatr Cardiol. 2004;25:131–136. doi: 10.1007/s00246-003-0514-3. [DOI] [PubMed] [Google Scholar]
- 36.Roberson DA, Cui W, Chen Z, Madronero LF, Cuneo BF. Annular and septal doppler tissue imaging in children: Normal z-score tables and effects of age, heart rate, and body surface area. J Am Soc Echocardiogr. 2007;20:1276–1284. doi: 10.1016/j.echo.2007.02.023. [DOI] [PubMed] [Google Scholar]
- 37.Vogel M, Sponring J, Cullen S, Deanfield JE, Redington AN. Regional wall motion and abnormalities of electrical depolarization and repolarization in patients after surgical repair of tetralogy of fallot. Circulation. 2001;103:1669–1673. doi: 10.1161/01.cir.103.12.1669. [DOI] [PubMed] [Google Scholar]
- 38.Wahl A, Praz F, Schwerzmann M, Bonel H, Koestner SC, Hullin R, Schmid JP, Stuber T, Delacretaz E, Hess OM, Meier B, Seiler C. Assessment of right ventricular systolic function: Comparison between cardiac magnetic resonance derived ejection fraction and pulsed-wave tissue doppler imaging of the tricuspid annulus. Int J Cardiol. 2010;151:58–62. doi: 10.1016/j.ijcard.2010.04.089. [DOI] [PubMed] [Google Scholar]
- 39.Rudski LG, Lai WW, Afilalo J, Hua L, Handschumacher MD, Chandrasekaran K, Solomon SD, Louie EK, Schiller NB. Guidelines for the echocardiographic assessment of the right heart in adults: A report from the american society of echocardiography endorsed by the european association of echocardiography, a registered branch of the european society of cardiology, and the canadian society of echocardiography. J Am Soc Echocardiogr. 2010;23:685–713. doi: 10.1016/j.echo.2010.05.010. [DOI] [PubMed] [Google Scholar]
- 40.Brown DW, McElhinney DB, Araoz PA, Zahn EM, Vincent JA, Cheatham JP, Jones TK, Hellenbrand WE, O’Leary PW. Reliability and accuracy of echocardiographic right heart evaluation in the u.S. Melody valve investigational trial. J Am Soc Echocardiogr. 2012;25:383–392. doi: 10.1016/j.echo.2011.12.022. [DOI] [PubMed] [Google Scholar]
- 41.Koestenberger M, Ravekes W, Everett AD, Stueger HP, Heinzl B, Gamillscheg A, Cvirn G, Boysen A, Fandl A, Nagel B. Right ventricular function in infants, children and adolescents: Reference values of the tricuspid annular plane systolic excursion (tapse) in 640 healthy patients and calculation of z score values. J Am Soc Echocardiogr. 2009;22:715–719. doi: 10.1016/j.echo.2009.03.026. [DOI] [PubMed] [Google Scholar]


